Abstract
To date, good experimental animal models of renal anemia are not available. Therefore, the purpose of this study was to establish a novel approach to induce chronic kidney disease (CKD) with severe anemia by oral administration of adenine in rodents. Adenine was administered to 6-week-old male C57BL/6 mice (25 and 50 mg/kg body weight) by oral gavage daily for 28 days. Serum creatinine and BUN as well as hematocrit, hemoglobin (Hb) and plasma erythropoietin (EPO) levels were monitored to assess renal function and anemia, respectively. Adenine at 25 mg/kg for 28 days slightly increased plasma creatinine levels, but did not induce anemia. In contrast, 50 mg/kg of adenine daily for 28 days showed severe renal dysfunction (plasma creatinine 1.9 ± 0.10 mg/dL) and anemia (hematocrit 36.5 ± 1.0% and EPO 28 ± 2.4 pg/mL) as compared with vehicle-treated mice (0.4 ± 0.02 mg/dL, 49.6 ± 1.6% and 61 ± 4.0 pg/mL, respectively). At the end of experiment, level of Hb also significantly reduced in 50 mg/kg adenine administration group. Remarkable histological changes of kidney tissues characterized by interstitial fibrosis and cystic appearance in tubules were observed in 50 mg/kg of adenine treatment group. These results have demonstrated that oral dosing with adenine at 50 mg/kg for 28 days is suitable to induce a stable anemia associated with CKD in mice.
Introduction
Anemia is a common hallmark of chronic kidney disease (CKD) which is associated with reduced quality of life and increased cardiovascular disease (CVD), hospitalizations, cognitive impairment and mortality [1]. It has also been shown that anemia is an independent predictor for ischemic cardiac events [2]. Therefore, anemia plays an important role in adding a further layer of complexity to the relationship between CKD and CVD [3]. Anemia management through recombinant human erythropoietin (rhEPO) or erythropoiesis stimulating agents (ESAs) greatly benefits patients with CKD by improving their debilitating symptoms, and relieving them from dependence on blood transfusions [4]. However, the current management and therapeutic approach for patients with renal anemia is controversial due to increased morbidity and mortality [5–7]. Therefore, there is a desperate need for studies to determine the precise mechanism of renal anemia in order to develop novel therapies or therapeutic strategies.
Animal models of CKD are important means of enabling translational research for investigating the pathophysiology of renal anemia and providing opportunities to assess the screening of potential novel therapies [8]. A number of animal models are available for induction of progressive renal failure including 5/6 nephrectomy (subtotal nephrectomy) and unilateral ureteral obstruction (UUO). However, these surgical induction of CKD in animals have numerous limitations such as a significant mortality rate and less anemia [9]. The adenine-induced CKD animal model has gained attention due to its relative ease of implementation without surgery and encouraging outcomes. Orally administered adenine metabolizes to 2,8-dihydroxyadenine, which forms crystal in the proximal tubular epithelia leading to inflammation and subsequent tubulointerstitial fibrosis [10, 11] as well as anemia [12]. In rodents, a number of studies have modified the original protocol developed by Yokozawa et al. [13] by changing the concentration of adenine in feed and/or the duration of administration to mimic renal anemia in humans [14–18]. However, administration of dietary adenine has a limitation: food intake is decreased significantly after mixing adenine with chow [19]. Therefore, food intake was not equal among the animals, and variability in the induction of CKD and/or anemia was obvious [18, 20].
The purpose of the present study is to establish a novel method of adenine administration in rodents to stably induce renal anemia. To avoid the variability of the effect of adenine, we measured the body weight of mice daily and administered the calculated amount of adenine accurately by oral gavage. There are few reports that have examined the effects of oral gavage of adenine in rats; however, no information is available regarding anemia [21]. Accordingly, we also followed a previous report [21] to induce CKD in rats and investigated the subsequent anemia.
Materials and methods
Animals
All experimental procedures in this study involving animals were carried out according to the ethical standards of Kagawa University, Japan and the principles of the Declaration of Helsinki (S1 File). The protocol of this study was reviewed and approved by the local institutional committee at Kagawa University, Japan. Five-week-old C57BL/6 mice and Wistar rats were purchased from Japan SLC Inc. (Shizuoka, Japan). Male rodents were preferred in this study because female rodents are resistant to kidney injury [22, 23] and less likely to develop adenine-induced CKD [24]. Animals were housed in specific-pathogen-free animal facilities under controlled temperature (24 ± 2°C) and humidity (55 ± 5%) conditions with a 12-hour light-dark cycle, and were given standard chow and had access to water ad libitum.
Drugs
Adenine was purchased from Sigma-Aldrich, Inc. (Saint Louis, MO, USA). Carboxymethyl cellulose (CMC) was purchased from Wako Pure Chemical Industries Ltd. (Osaka, Japan).
Experimental protocols
Following one week of acclimatization, 6-week-old C57BL/6 mice and Wistar rats were divided into three groups each (S1 Fig) based on the baseline plasma levels of creatinine and hematocrit data. In the control group, 0.5% CMC was administered by oral gavage to both mice (0.2 mL per 20 g body weight; n = 20) and rats (2 mL per 200 g body weight, n = 20). Adenine was administered to mice at 25 (n = 30) and 50 (n = 30) mg/kg body weight in 0.5% CMC by oral gavage (because mice were reluctant to consume adenine-containing chow) daily for 28 days. Furthermore, in rats, adenine at 200 (n = 30) and 600 (n = 30) mg/kg body weight in 0.5% CMC was administered by oral gavage daily for 10 days. During the observation period, at each time point 5–6 animals were euthanized with sevoflurane via precision vaporizer to measure renal function and anemia related parameters and the remaining animals were euthanized at the end of the observation period. In addition, to confirm this adenine-induced renal injury model is suitable to study renal anemia, rhEPO (5 IU) was injected subcutaneously every 2 days for 35 days in mice, after 28 days oral administration of 50 mg/kg adenine with an additional 7 days of recovery.
Sample collection
Blood samples were collected from the tail vein to measure hematological parameters both in mice and rats. We collected blood samples after the end of adenine administration, as well as at various time points during the observation period (S1 Fig).
Biochemical and hematological parameters
Plasma creatinine was measured by a commercially available kit (LabAssay Creatinine, Wako Pure Chemical Industries Ltd., Osaka, Japan). For hematocrit measurement, blood was collected in hematocrit tubes followed microhematocrit centrifugation. The length of the column of packed red cells was measured, divided by the length of the column of whole blood and multiplied by 100%. Levels of plasma BUN and hemoglobin (Hb), as well as total protein in urine were measured by an automated analyzer (7020-Automatic Analyzer; Hitachi High-Technologies, Tokyo, Japan). Plasma erythropoietin (EPO) level was measured in both mice and rats by ELISA (Epo Mouse ELISA Kit, Cat. No. KA1998, Abnova, Tapei City, Taiwan; Legend Max Rat Erythropoietin ELISA Kit, Cat. No. 442807, BioLegend, San Diego, CA, USA, respectively) in accordance with the manufacturers’ instruction. Levels of ferritin and gamma glutamyltransferase (γ-GT) were also measured in rat plasma by commercially available ELISA kits (Ferritin (Rat) ELISA kit, Cat. No. KA1949, Abnova; Rat γ-GT1 ELISA Kit, Cat. No. E-EL-RO404, Elabscience, Wuhan, China, respectively).
Histological analysis
Following euthanasia of the mice and rats, kidneys were collected and perfused with 0.9% saline and then pieces of kidney were fixed in 10% neutral-buffered formalin, dehydrated in a concentration gradient of ethanol, cleared with xylene and embedded in paraffin. Tissue samples were cut into 5-μm-thick sections and stained with azan, as described previously [25].
Gene expression in renal tissue
RNA was isolated from renal cortical tissues of rats by the phenol–chloroform extraction method and cDNA prepared as described previously [26]. The mRNA expression of α-smooth muscle actin (Sma) and fibroblast growth factor (Fgf) 23 was analyzed by real-time PCR using an ABI Prism 7000 system with Power SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA, USA). The oligonucleotide primers for rats used were as follows (forward and reverse, respectively): 5′-ACGGCGGCTTCGTCTT CT-3′ and 5′-CCAGCTGACTCCATGCCAAT-3′ for α-Sma [27]; 5′-TTGGATCGTATC ACTTCAGC-3′ and 5′-TGCTTCGGTGACAGGTAG-3′ for Fgf23 [28]; 5′-CCCTG GCTCCTAGCACCAT-3′, and 5′-CCTGCTTGCTGATCCACAT CT-3′ for β-Actin [27]. The abundance of target genes were normalized to β-Actin (as internal control) and analyzed by the 2−ΔΔCt method as described previously [29].
Statistical analysis
Data are the mean ± SEM. One-way analysis of variance followed by Dunnett’s multiple comparison test was used for all cross sectional one-factor data (plasma BUN, Hb, ferritin, γ-GT, urine protein, mRNA expression). Longitudinal (body weight, plasma creatinine, hematocrit and EPO) data were analyzed by two-way analysis of variance followed by the Bonferroni post-hoc test to determine differences between groups, except for mouse plasma creatinine and EPO data (one-way analysis of variance followed by Bonferroni post-hoc test). Data of the adenine administered rats and mice were compared with that of the respective vehicle-treated group. A P-value of P < 0.05 was considered statistically significant. Data were analyzed by GraphPad Prism 7 (GraphPad Software, Inc., CA, USA).
Results
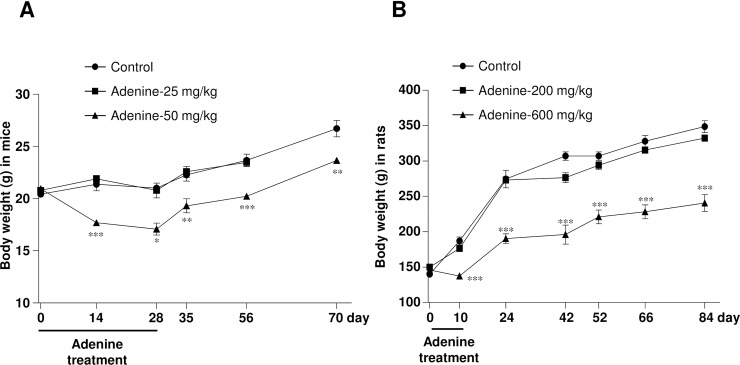
High dose adenine treatment by oral gavage reduces body weight
In C57BL/6 mice, the gradual increase in body weight in the vehicle-treated group signified a normal growth curve (Fig 1A). However, adenine at 25 mg/kg did not affect the body weight during or after administration as compared with vehicle-treated animals. In contrast, oral administration of adenine at 50 mg/kg reduced body weight significantly during and after 28 days of treatment.
Fig 1. High dose of adenine by oral gavage reduces body weight in mice and rats.
Changes of body weight during adenine administration and the observation period in (A) mice and (B) rats. * P < 0.05, ** P < 0.01, *** P < 0.001 vs. vehicle-treated mice or rats, respectively.
In Wistar rats, adenine at 200 mg/kg did not affect body weight, while adenine at 600 mg/kg body weight for 10 days significantly decreased the body weight (Fig 1B). Food intake tended to increase at the end of experiments in both mice and rats (Table 1). Increase in body weight was accompanied by an increase in food intake during the observation period, up to 70 days in mice and 84 days in rats, respectively. However, body weight remained significantly lower in adenine-treated groups as compared with the respective vehicle-treated control animals.
Table 1. Plasma biochemical, hematological, metabolic and urinary parameters in rodents with adenine-induced renal injury.
| Parameters | Mice | Rats | ||||||
|---|---|---|---|---|---|---|---|---|
| Day | Vehicle | 25 mg/kg | 50 mg/kg | Day | Vehicle | 200 mg/kg | 600 mg/kg | |
| Plasma Creatinine (mg/dL) | 28 | 0.3 ± 0.01 | 0.8 ± 0.1 | 1.8 ± 0.1*** | 10 | 0.5 ± 0.04 | 1.1 ± 0.1 | 3.02 ± 0.02*** |
| 70 | 0.2 ± 0.03 | - | 1.2± 0.1** | 84 | 0.7 ± 0.02 | 1.0 ± 0.06 | 2.3 ± 0.3*** | |
| Plasma BUN (mg/dL) | 70 | 36.6 ± 1.1 | - | 73 ± 3.7*** | 66 | 24 ± 0.9 | 56 ± 2.2* | 142 ± 1.9*** |
| Hematocrit (%) | 28 | 49.6 ± 1.6 | 48.6 ± 0.9 | 36.5 ± 1.0*** | 10 | 43.5 ± 2.2 | 41.7 ± 1.0 | 40.1 ± 1.2 |
| 70 | 49.5 ± 0.7 | - | 33.9 ± 1.1*** | 84 | 43.4 ± 1.5 | 44.1 ± 1.7 | 30.1 ± 1.0*** | |
| Hemoglobin (g/dl) | 70 | 16.8 ± 0.2 | - | 12.9 ± 0.2*** | 66 | 17.0 ± 0.1 | 14.2 ± 0.5 | 11.9 ± 0.5*** |
| Total RBC (x104/ μL) | - | - | - | - | 763 | 763 ± 4.9 | 642 ± 20.3 | - |
| Plasma EPO (pg/mL) | 28 | 60.9 ± 4.0 | 44.8 ± 2.5 | 27.8 ± 2.3*** | 10 | 28.4 ± 3.7 | 7.5 ± 1.6*** | 2.0 ± 0.8*** |
| 70 | - | - | 16.6 ± 4.7††† | 84 | 28.6 ± 2.6 | 23.2 ± 3.4 | 13.1 ± 2.5** | |
| Plasma ferritin (ng/mL) | - | - | - | - | 66 | 238 ± 36 | 388± 29* | 404 ± 42* |
| Plasma γ-GT (U/L) | - | - | - | - | 66 | 3.4 ± 0.2 | 3.8 ± 0.1 | 4.3 ± 0.2 |
| Food intake (mL) | 4.8 ± 0.3 | - | 4.9 ± 0.2 | 66 | 13.0 ± 0.7 | 15.9 ± 0.6 | 14.3 ± 1.1 | |
| Water intake (mL) | 5.9 ± 0.2 | - | 13 ± 0.4*** | 66 | 19.0 ± 1.1 | 38.8 ± 2.0 | 62.7 ± 4.1*** | |
| Urine volume (mL) | 70 | 2.0 ± 0.2 | - | 7.9 ± 0.5*** | 66 | 11.7 ± 0.8 | 26 ± 2.1* | 47 ± 3.5*** |
| Urine protein (mg/day) | 70 | 5.6 ± 0.5 | - | 9.7 ± 1.4* | 66 | 5.7 ± 0.6 | 6.7 ± 1.0 | 24 ± 6.0*** |
Data are mean ± SE.
* P < 0.01
** P < 0.01
*** P < 0.001 vs. vehicle-treated mice or rats (corresponding time points) respectively
††† P < 0.001 vs. vehicle-treated mice at 28 days.
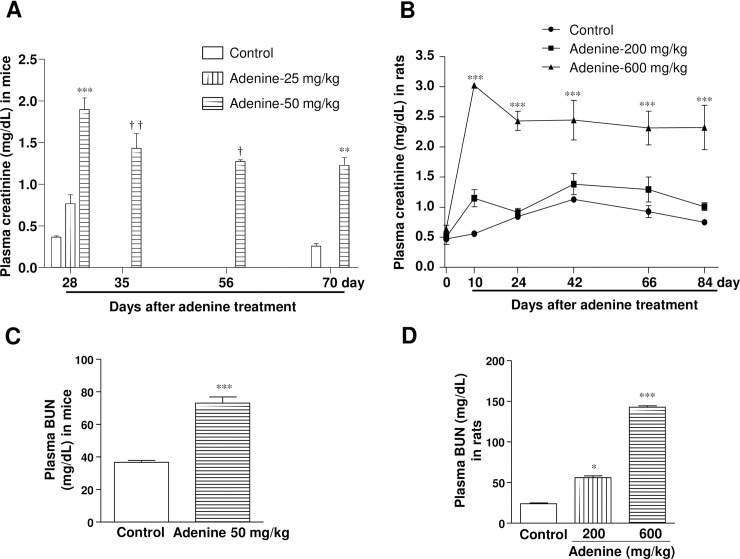
Adenine administration by oral gavage decreases renal function and manifests pathological features like CKD
In mice, oral administration of adenine at 25 mg/kg slightly, but significantly, increased plasma creatinine (0.8 ± 0.10 mg/dL) levels at day 28 (Fig 2A). In contrast, 50 mg/kg of adenine caused an approximately 5-fold increase in plasma creatinine levels (1.9 ± 0.10 mg/dL) as compared with the vehicle-treated mice (0.4 ± 0.02 mg/dL). During the observation period, levels of plasma creatinine tended to be decreased, but remained significantly higher in the 50 mg/kg adenine treatment group in comparison with the vehicle-treated mice at day 28. Consistently, BUN level in plasma also significantly higher in mice treated with adenine at 50 mg/kg at day 70 (Fig 2C).
Fig 2. Administration of adenine by oral gavage decreases renal function.
Changes in plasma creatinine levels after adenine administration and during the observation period in (A) mice and (B) rats. Levels of plasma BUN in (C) mice and (D) rats at day 70 and 66, respectively. * P < 0.05, ** P < 0.01, *** P < 0.001 vs. vehicle-treated mice or rats (corresponding time points) respectively; † P < 0.05, †† P < 0.01 vs. vehicle-treated mice at 28 days.
In rats, adenine at 200 mg/kg caused a significant increase in plasma creatinine level (1.2 ± 0.14 mg/dL) compared with vehicle-treated rats (0.6 ± 0.05 mg/dL) (Fig 2B). However, the plasma creatinine level was elevated 5-fold (3.0 ± 0.02 mg/dL) in 600 mg/kg adenine-treated rats during the administration period. At day 24, plasma creatinine levels were approximately 4-fold higher and remained constant during the remainder of the observation period. Levels of plasma BUN levels in rats also significantly higher following administration of adenine at either 200 or 600 mg/kg at day 66 (Fig 2D).
Adenine administration at 50 mg/kg in mice and 600 mg/kg in rats caused a significant increase in urine protein excretion (Table 1), suggesting high doses of adenine induces proteinuria which is a pathological manifestation in patients with CKD. Moreover, plasma levels of γ-GT were significantly increased by adenine administration at 600 mg/kg in rats, indicating systemic toxicity and liver damage (Table 1).
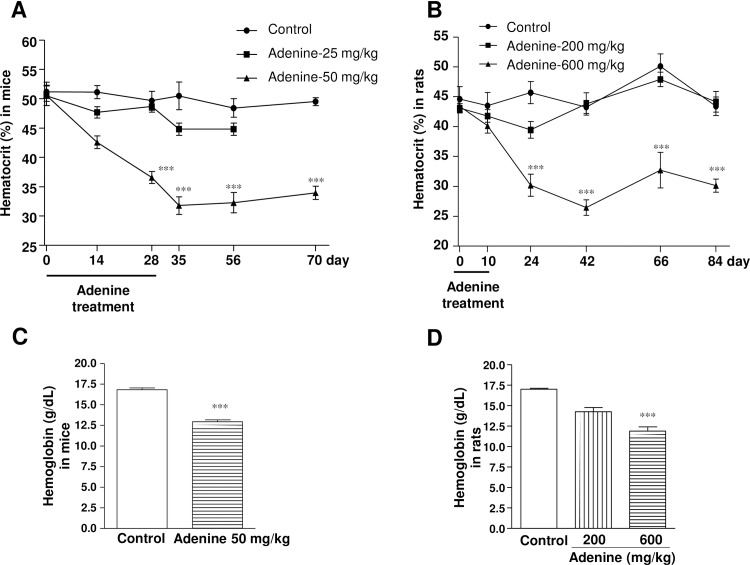
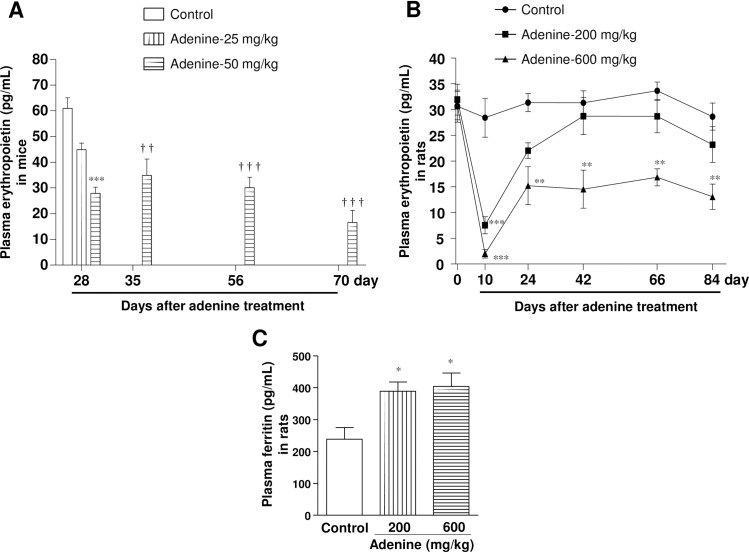
Adenine administration by oral gavage induces anemia
To observe anemia in CKD, hematocrit and plasma EPO levels were measured during and after the end of adenine administration in both C57BL/6 mice and Wistar rats (Figs 3 and 4). Adenine at 25 mg/kg in mice did not change the hematocrit (48.7 ± 0.9%) and EPO (45 ± 2.0 pg/mL) levels. However, adenine at 50 mg/kg administered for 28 days caused a significant reduction in hematocrit level (36.5 ± 1.0%) as compared with vehicle-treated mice (49.6 ± 1.6%), which remained significantly lower during the observation period (Fig 3A). Furthermore, plasma Hb levels were also significantly reduced in mice (16.8 ± 0.2 vs. 12.9 ± 0.2 g/dL) by oral administration of adenine at 50 mg/kg at day 70 (Fig 3C). Consistently, plasma EPO level was significantly reduced following adenine administration at 50 mg/kg for 28 days (28 ± 2 pg/mL vs. 61 ± 4 pg/mL), which also remained significantly lower upto the end of the experimental period (Fig 4A).
Fig 3. Administration of adenine by oral gavage reduces hematocrit and Hb levels.
Changes in hematocrit levels after adenine administration and during the observation period in (A) mice and (B) rats. Levels of plasma Hb in (C) mice and (D) rats at day 70 and 66, respectively. ***P < 0.001 vs. vehicle-treated mice or rats (corresponding time points) respectively.
Fig 4. Administration of adenine by oral gavage impacts on plasma erythropoietin and ferritin levels.
Changes in plasma erythropoietin (EPO) levels after adenine administration and during the observation period in (A) mice and (B) rats. Levels of plasma ferritin in (c) rats at day 66. * P < 0.05, ** P < 0.01, *** P < 0.001 vs. vehicle-treated mice or rats (corresponding time points) respectively; †† P < 0.01, ††† P < 0.001 vs. vehicle-treated mice at 28 days.
In rats, hematocrit level did not change during or after adenine administration at 200 mg/kg (Fig 3B). In contrast, adenine at 600 mg/kg caused a significant reduction in hematocrit level (30.2 ± 1.9%) at day 24 as compared with vehicle-treated rats (45.7 ± 1.7%), which remained significantly lower during the observation period. Consistently, plasma hemoglobin levels were significantly reduced (16.7 ± 0.1 vs.12.8 ± 0.6 g/dL) in rats following adenine administration at 600 mg/kg at day 66 (Fig 3D). Moreover, rat plasma EPO levels were significantly decreased by adenine administration at 200 or 600 mg/kg at day 10. However, in later period plasma EPO levels turned back to the normal range in 200 mg/kg adenine-treated rats, but remained significantly lower at 600 mg/kg adenine-treated group (Fig 4B). Plasma ferritin levels were significantly increased by oral administration of adenine at either 200 or 600 mg/kg in rats, which is a typical feature of CKD (Fig 4C).
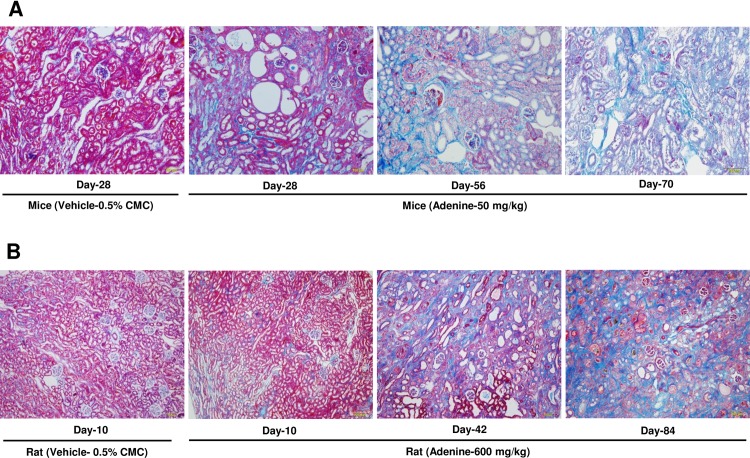
Adenine treatment changes the gross morphology of the kidney and induces damage and fibrosis to renal tissue
In mice, swelling, discoloration and deformity of the kidney were more obvious after treatment with 50 mg/kg of adenine (S2A Fig). Azan staining of histological sections of mouse kidney tissue revealed severe tubulointerstitial fibrosis and cyst formation in kidneys after administration of adenine at 50 mg/kg during the observation period at days 56 and 70 (Fig 5A).
Fig 5. Adenine treatment via oral gavage induces tubulointerstitial fibrosis.
Representative photomicrograph of azan staining of cortical sections of kidney tissues to demonstrate tubulointerstitial fibrosis in (A) mice and (B) rats after treatment with vehicle or adenine (50 mg/kg for mice and 600 mg/kg for rat) at different time points. Photomicrographs taken at 100× magnification.
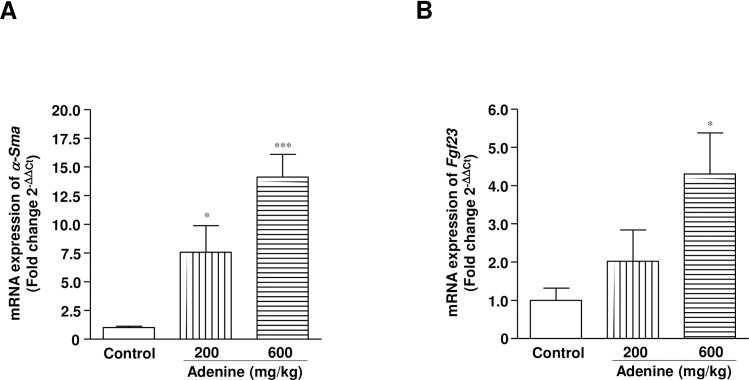
In rats, these gross morphological changes in the kidneys were also obvious in the 600 mg/kg adenine treatment group (S2B Fig). Severe tubulointerstitial fibrosis accompanied with cyst formation and tubular damage was obvious 42 and 84 days after oral administration of adenine at 600 mg/kg in rats (Fig 5B). Consistently, mRNA expression level of α-Sma (a critical mediator of fibrosis) was increased dramatically in cortical kidney tissues at day 84 (Fig 6A). Furthermore, Fgf23 mRNA was expressed highly in the kidney tissues of rats treated with adenine at 600 mg/kg because it predicted CKD progression by interfering with bone remodeling (Fig 6B).
Fig 6. Oral administration of adenine increases the gene expression related to fibrosis and bone regeneration.
Relative changes of mRNA expression of (A) α-Sma and (B) Fgf23 in the renal cortical tissues of rats at day 84. * P < 0.05, *** P < 0.001 vs. vehicle-treated rats.
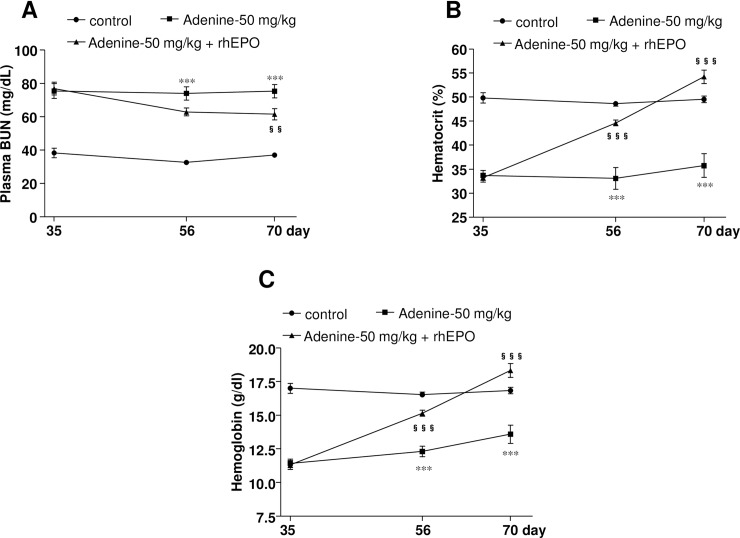
Erythropoietin treatment improves adenine-induced CKD associated anemia in mice
rhEPO treatment for 35 days caused a significant reduction in the plasma levels of BUN (Fig 7A) in mice. In contrast, levels of hematocrit (Fig 7B) and Hb (Fig 7C) gradually increased just after starting rhEPO treatment and significantly increased within 21 days of treatment and remained significantly higher at the end of the experiment. These data suggest that the adenine-induced renal injury model of rodents is a convenient tool to study anemia associated with CKD.
Fig 7. Erythropoietin treatment improves renal anemia in adenine-induced renal injury model.
Plasma levels of (A) BUN, (B) hematocrit, and (C) Hb following subcutaneous injections of rhEPO (5IU) every 2 days interval for 5 weeks in mice with adenine-induced renal injury (50 mg/kg adenine for 4 weeks). *** P < 0.001 vs. vehicle-treated mice; §§ P < 0.01, §§§ P < 0.001 vs. adenine-treated (50 mg/kg) mice.
Discussion and conclusions
To date, good experimental mouse models of renal anemia are not available. Here, we have established stable renal anemia in mice. We showed that adenine at 50 mg/kg administered through oral gavage for 28 days is enough to induce CKD with severe anemia in mice. Our data also demonstrate that biological variation among the animals in the adenine treated groups is less in comparison with the previously reported models of dietary administration of adenine [10, 20, 30].
In the initial report of adenine-induced CKD, adenine was given to rats mixed with feed at a concentration of 0.75% (w/w) for 4 weeks [11]. Many studies have followed the same protocol [23, 24] or modified the concentration of adenine in feed, e.g. 0.25% [14] and 0.5% [14, 16]. Duration of adenine administration has also been changed to obtain varying degrees of CKD with targeted pathophysiological conditions [30]. Dietary adenine administration at the concentration of 0.15–0.3% for 6–8 weeks has been reported to induce severe renal injury in C57BL/6 mice [17, 18, 31]. However, there is no available information regarding the anemia status in mice following adenine administration. We showed that adenine at 25 mg/kg did not change the hematocrit or plasma EPO levels after 28 days of oral administration, while these levels tended to decrease during the observation period. In contrast, 50 mg/kg oral administration of adenine for 28 days caused a significant reduction in hematocrit and plasma EPO levels as compared with the vehicle-treated mice, which remained significantly lower during the observation period of up to 70 days. In agreement with this, Hb levels also significantly reduced in mice at day 70. We also found that adenine at 100 mg/kg body weight was lethal for mice (data not shown). Recent studies have demonstrated that EPO treatment significantly reduced the BUN levels in renal ischemic reperfusion in rats [32] and 5/6 nephrectomy in mice [32, 33]. In the present study, we observed that rhEPO (5 IU) administration significantly decreased the plasma level of BUN, and increased the hematocrit and hemoglobin levels in adenine (50 mg/kg)-induced anemic mice, suggesting an improvement of renal function and anemia in these animals. Thus, our data revealed that adenine at 50 mg/kg induces severe anemia in mice, which mimics clinical renal anemia in humans, and this model is also suitable to study the pathophysiology and treatment of renal anemia.
Studies have shown that in Wistar rats, 0.75% (w/w) adenine diet for 4 weeks and an additional 4 weeks observation caused a severe anemia with hemoglobin levels of 7.6 ± 1.7 g/dL [30], and a hematocrit of 32.6±1.2% [34] (13.8±1.2 g/dL and 51.0±0.6% in control rats, respectively). However, Terai et al. [21] demonstrated the induction of renal disease by oral dosing of rats with 600 mg/kg adenine, although there was no reported information regarding anemia. In the present study, we showed that oral administration of adenine at 600 mg/kg for 10 days with an additional 14 days observation caused a significant reduction in hematocrit as well as plasma EPO levels, which remained at significantly lower levels than the controls for the 84 day observation period. A significantly lower level of Hb also confirmed the anemia in rats after administration of 600 mg/kg adenine. We also found that 200 mg/kg of adenine tended to decrease hematocrit and plasma EPO levels at day 24, but they soon returned to the normal level. In the present study, at day 10, both 200 and 600 mg/kg adenine caused a significant reduction in plasma levels of EPO in rats. Clinical studies have shown that acute renal injury stimulates EPO production at the beginning of the disease with a strong tendency to decrease just after the course of injury [35]. Similarly, renal HIF-1 was upregulated within 2 hours following acute renal injury and totally diminished within 24 hours [36]. This study also suggests that HIF induction is maximal with moderate hypoxia and declines with the increasing severity of hypoxia. In contrast, a recent study showed that 100 mg/kg adenine for 7 days caused severe renal cellular hypoxia in rats [37]. Collectively, a dramatic fall of EPO concentration at day 10 might be due to the reduction of expression of HIF-1α in adenine-induced severe cellular hypoxic kidneys in rats. Moreover, a recent clinical study has shown that renal anemia is caused by relative EPO deficiency [38], which is a consequence of injury and fibrosis as well as accumulation of myofibroblasts in the kidney [12]. In the present study, adenine administration in mice (50 mg/kg) and rats (600 mg/kg) induced severe tubulointerstitial fibrosis in the kidneys that was evident from the histomorphological changes by azan staining as well as increased mRNA level of α-Sma expression in cortical tissues. Consistently, Zhang et al. have demonstrated that adenine (200 mg/kg) given for 3 weeks in rats upregulated the expression of pro-fibrotic proteins such as α-Sma, collagen I, fibronectin, plasminogen activator inhibitor-1, and transforming growth factor-β1 significantly [39]. Expression of fibrotic proteins was not evaluated in the present study, but a similar level of kidney injury was observed in rats after adenine administration at 600 mg/kg for 10 days. Recently, it has demonstrated that the bone-derived hormone, FGF23 regulates systemic phosphate homeostasis, vitamin D metabolism and α-Klotho expression through a novel bone-kidney axis [40]. However, FGF23 levels increase gradually along with kidney injury, leading to reductions in 1,25(OH)2D levels and secondary hyperparathyroidism in individuals with CKD [41]. Interestingly, our results revealed that adenine administration at 600 mg/kg, but not 200 mg/kg caused significantly high expression of Fgf23 mRNA that mimics the clinical condition of CKD. Therefore, all of these data have documented that 10 days of treatment with adenine at 200 mg/kg does not induce severe renal injury and anemia, while at 600 mg/kg caused a severe state of anemia in rats.
A number of studies have already shown changes in renal functional parameters in adenine-treated mice and rats [11, 15, 17, 18, 30, 42]. In mice, plasma creatinine was elevated by 1.5-fold in comparison with vehicle-treated mice following 0.2% dietary administration of adenine for 4 weeks [17]. However, our data revealed that plasma creatinine levels were increased by 5-fold following 50 mg/kg oral administration of adenine for 28 days in mice, which remained significantly higher during the observation period of up to 70 days. Consistent with previous data shown by Terai et al. [21], we also documented that 10 days of oral administration of adenine at 600 mg/kg body weight causes a significant increase in plasma creatinine levels in rats, which remained elevated during the observation period. Previous studies showed that 4 weeks adenine (0.75% w/w) administration through feed resulted in a significant increase in plasma creatinine [30] and decrease in creatinine clearance [15] in rats. Moreover, in the present study, plasma levels of BUN and protein excretion in urine were significantly increased in rats treated with oral administration of adenine at 600 mg/kg, suggesting an impairment of renal function. Furthermore, the mortality rate was 20% in the rats treated with 600 mg/kg adenine at the end of the experiment and the pathological manifestations were severe, which mimics the clinical features of CKD. We also showed that 200 mg/kg of adenine caused a transient increase in plasma creatinine during oral administration of adenine. However, these levels were not significantly different in comparison to the vehicle-treated rats after day 24. Importantly, increases in plasma creatinine levels in adenine-treated mice and rats were associated with renal tissue injury.
Previous studies have shown that dietary adenine administration (for 8 weeks in mice [43]; and for 3 weeks in rats [44]) induces renal injury, which is associated with a reduction in reticulocyte count, suggesting a hyporegenerative anemia. In the present study, the novel approach of adenine administration by oral gavage shortens the duration of renal injury induction (to 4 weeks in mice and 10 days in rats). However, the extent of renal injury and anemia are similar among both current and previous studies. These data suggest that adenine administration through oral gavage and diet induces renal anemia which is associated with hyporegenerative anemia. Water balance data indicated that water retention was significantly increased by adenine administration either at 600 mg/kg in rats or 50 mg/kg in mice, compared with the respective vehicle-treated animals [data not shown], suggesting that adenine-induced renal injury caused impairment in the excretion of water through urine. This water retention is also evident from hematocrit data, which is a characteristic feature of CKD [45]. We also observed that adenine at 600 mg/kg significantly increased plasma γ-GT in rats, consistent with a previous report of dietary adenine administration [15]. In contrast, 200 mg/kg adenine induced a significant reduction in the total RBC count without changing plasma γ-GT levels [Table 1]. Taken together, these data suggest that adenine-induced anemia is not predominantly induced by its toxic effect on erythropoiesis. Eryptosis, a dramatic loss of erythrocytes due to death of suicidal erythrocytes, is one of the important underlying mechanism of anemia in CKD as well as in end stage renal disease (ESRD) [46]. In clinical studies, it has been demonstrated that anemia is aggravated in CKD by eryptosis [47, 48] which is triggered by increased cytosolic Ca2+ concentration, oxidative stress and ceramide. Therefore, the severe anemia induced by adenine in rodents might also be associated with eryptosis.
Thus the present study has demonstrated that oral administration of adenine at 50 mg/kg for 28 days in mice or at 600 mg/kg for 10 days in rats induces a significant anemia, which is accompanied by renal tissue injury and dysfunction. In conclusion, we have established a novel approach to renal anemic models in both mice and rats. These animal models would be important and useful tools for translational research on renal anemia in humans.
Supporting information
Oral administration of adenine at (A) 25 or 50 mg/kg body weight for 28 days in mice or (B) 200 or 600 mg/kg body weight for 10 days in rats. In mice the observation period was up to 70 days while in rats it was up to 84 days. Arrows (↑) indicate the blood collection time points.
(TIF)
Changes in size and color of kidney during the observation period in (A) mice and (B) rats after treatment with vehicle (0.5% CMC) or adenine (50 mg/kg for mice and 600 mg/kg for rat) at different time points.
(TIF)
(DOCX)
Acknowledgments
We would like to thank Yumi Sakane for her excellent technical assistance.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Japan Society for the Promotion of Science (JSPS) Grants-in-Aid for Scientific Research (KAKENHI) (26460343 to Akira Nishiyama) and the Hoansha Foundation (to Akira Nishiyama). However, the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kdoqi, National Kidney F. KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Anemia in Chronic Kidney Disease. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2006;47(5 Suppl 3):S11–145. doi: 10.1053/j.ajkd.2006.03.010 . [DOI] [PubMed] [Google Scholar]
- 2.Wang X, Qiu M, Li J, Wang H, Qi J, Wang G, et al. Impacts of anemia on 3-year ischemic events in patients undergoing percutaneous coronary intervention: a propensity-matched study. Journal of thoracic disease. 2015;7(11):1951–9. doi: 10.3978/j.issn.2072-1439.2015.10.66 ; PubMed Central PMCID: PMC4669295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Virani SA, Khosla A, Levin A. Chronic kidney disease, heart failure and anemia. The Canadian journal of cardiology. 2008;24 Suppl B:22B–4B. ; PubMed Central PMCID: PMC2794442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, et al. Correction of anemia with epoetin alfa in chronic kidney disease. The New England journal of medicine. 2006;355(20):2085–98. doi: 10.1056/NEJMoa065485 . [DOI] [PubMed] [Google Scholar]
- 5.Pfeffer MA, Burdmann EA, Chen CY, Cooper ME, de Zeeuw D, Eckardt KU, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. The New England journal of medicine. 2009;361(21):2019–32. doi: 10.1056/NEJMoa0907845 . [DOI] [PubMed] [Google Scholar]
- 6.Macdougall IC, Provenzano R, Sharma A, Spinowitz BS, Schmidt RJ, Pergola PE, et al. Peginesatide for anemia in patients with chronic kidney disease not receiving dialysis. The New England journal of medicine. 2013;368(4):320–32. doi: 10.1056/NEJMoa1203166 . [DOI] [PubMed] [Google Scholar]
- 7.Igarashi T, Ito S, Sako M, Saitoh A, Hataya H, Mizuguchi M, et al. Guidelines for the management and investigation of hemolytic uremic syndrome. Clinical and experimental nephrology. 2014;18(4):525–57. doi: 10.1007/s10157-014-0995-9 . [DOI] [PubMed] [Google Scholar]
- 8.Becker GJ, Hewitson TD. Animal models of chronic kidney disease: useful but not perfect. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association—European Renal Association. 2013;28(10):2432–8. doi: 10.1093/ndt/gft071 . [DOI] [PubMed] [Google Scholar]
- 9.Shobeiri N, Adams MA, Holden RM. Vascular calcification in animal models of CKD: A review. American journal of nephrology. 2010;31(6):471–81. doi: 10.1159/000299794 . [DOI] [PubMed] [Google Scholar]
- 10.Yokozawa T, Oura H, Koizumi F. 2,8-Dihydroxyadenine urolithiasis induced by dietary adenine in rats. Nihon Jinzo Gakkai shi. 1985;27(3):371–8. . [PubMed] [Google Scholar]
- 11.Yokozawa T, Zheng PD, Oura H. Biochemical features induced by adenine feeding in rats. Polyuria, electrolyte disorders, and 2,8-dihydroxyadenine deposits. Journal of nutritional science and vitaminology. 1984;30(3):245–54. . [DOI] [PubMed] [Google Scholar]
- 12.Asada N, Takase M, Nakamura J, Oguchi A, Asada M, Suzuki N, et al. Dysfunction of fibroblasts of extrarenal origin underlies renal fibrosis and renal anemia in mice. The Journal of clinical investigation. 2011;121(10):3981–90. doi: 10.1172/JCI57301 ; PubMed Central PMCID: PMC3195468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yokozawa T, Zheng PD, Oura H, Koizumi F. Animal model of adenine-induced chronic renal failure in rats. Nephron. 1986;44(3):230–4. . [DOI] [PubMed] [Google Scholar]
- 14.Diwan V, Mistry A, Gobe G, Brown L. Adenine-induced chronic kidney and cardiovascular damage in rats. Journal of pharmacological and toxicological methods. 2013;68(2):197–207. doi: 10.1016/j.vascn.2013.05.006 . [DOI] [PubMed] [Google Scholar]
- 15.Ali BH, Al Za'abi M, Ramkumar A, Yasin J, Nemmar A. Anemia in adenine-induced chronic renal failure and the influence of treatment with gum acacia thereon. Physiological research / Academia Scientiarum Bohemoslovaca. 2014;63(3):351–8. . [DOI] [PubMed] [Google Scholar]
- 16.Claramunt D, Gil-Pena H, Fuente R, Garcia-Lopez E, Loredo V, Hernandez-Frias O, et al. Chronic kidney disease induced by adenine: a suitable model of growth retardation in uremia. American journal of physiology Renal physiology. 2015;309(1):F57–62. doi: 10.1152/ajprenal.00051.2015 . [DOI] [PubMed] [Google Scholar]
- 17.Ali BH, Al-Salam S, Al Za'abi M, Waly MI, Ramkumar A, Beegam S, et al. New model for adenine-induced chronic renal failure in mice, and the effect of gum acacia treatment thereon: comparison with rats. Journal of pharmacological and toxicological methods. 2013;68(3):384–93. doi: 10.1016/j.vascn.2013.05.001 . [DOI] [PubMed] [Google Scholar]
- 18.Jia T, Olauson H, Lindberg K, Amin R, Edvardsson K, Lindholm B, et al. A novel model of adenine-induced tubulointerstitial nephropathy in mice. BMC nephrology. 2013;14:116 doi: 10.1186/1471-2369-14-116 ; PubMed Central PMCID: PMC3682934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang C, Liu C, Zhou Q, Xie YC, Qiu XM, Feng X. Effect of atracylodes rhizome polysaccharide in rats with adenine-induced chronic renal failure. Indian journal of pharmaceutical sciences. 2015;77(1):103–7. ; PubMed Central PMCID: PMC4355872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neven E, D'Haese PC. Vascular calcification in chronic renal failure: what have we learned from animal studies? Circulation research. 2011;108(2):249–64. doi: 10.1161/CIRCRESAHA.110.225904 . [DOI] [PubMed] [Google Scholar]
- 21.Terai K, Nara H, Takakura K, Mizukami K, Sanagi M, Fukushima S, et al. Vascular calcification and secondary hyperparathyroidism of severe chronic kidney disease and its relation to serum phosphate and calcium levels. British journal of pharmacology. 2009;156(8):1267–78. doi: 10.1111/j.1476-5381.2008.00108.x ; PubMed Central PMCID: PMC2697742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hodeify R, Megyesi J, Tarcsafalvi A, Mustafa HI, Hti Lar Seng NS, Price PM. Gender differences control the susceptibility to ER stress-induced acute kidney injury. American journal of physiology Renal physiology. 2013;304(7):F875–82. doi: 10.1152/ajprenal.00590.2012 ; PubMed Central PMCID: PMC3625845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kang KP, Lee JE, Lee AS, Jung YJ, Kim D, Lee S, et al. Effect of gender differences on the regulation of renal ischemia-reperfusion-induced inflammation in mice. Molecular medicine reports. 2014;9(6):2061–8. doi: 10.3892/mmr.2014.2089 ; PubMed Central PMCID: PMC4055478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diwan V, Small D, Kauter K, Gobe GC, Brown L. Gender differences in adenine-induced chronic kidney disease and cardiovascular complications in rats. American journal of physiology Renal physiology. 2014;307(11):F1169–78. doi: 10.1152/ajprenal.00676.2013 . [DOI] [PubMed] [Google Scholar]
- 25.Nishioka S, Nakano D, Kitada K, Sofue T, Ohsaki H, Moriwaki K, et al. The cyclin-dependent kinase inhibitor p21 is essential for the beneficial effects of renal ischemic preconditioning on renal ischemia/reperfusion injury in mice. Kidney international. 2014;85(4):871–9. doi: 10.1038/ki.2013.496 . [DOI] [PubMed] [Google Scholar]
- 26.Rahman A, Kittikulsuth W, Fujisawa Y, Sufiun A, Rafiq K, Hitomi H, et al. Effects of diuretics on sodium-dependent glucose cotransporter 2 inhibitor-induced changes in blood pressure in obese rats suffering from the metabolic syndrome. Journal of hypertension. 2016;34(5):893–906. doi: 10.1097/HJH.0000000000000871 . [DOI] [PubMed] [Google Scholar]
- 27.Rafiq K, Nakano D, Ihara G, Hitomi H, Fujisawa Y, Ohashi N, et al. Effects of mineralocorticoid receptor blockade on glucocorticoid-induced renal injury in adrenalectomized rats. Journal of hypertension. 2011;29(2):290–8. ; PubMed Central PMCID: PMC3034279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lavi-Moshayoff V, Wasserman G, Meir T, Silver J, Naveh-Many T. PTH increases FGF23 gene expression and mediates the high-FGF23 levels of experimental kidney failure: a bone parathyroid feedback loop. American journal of physiology Renal physiology. 2010;299(4):F882–9. doi: 10.1152/ajprenal.00360.2010 . [DOI] [PubMed] [Google Scholar]
- 29.Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nature protocols. 2008;3(6):1101–8. . [DOI] [PubMed] [Google Scholar]
- 30.Hideto Okada YK, Takiko Yawata, Hideto Uyama, Seiichiro Ozono, Yoshihiro Motomiya and Yoshihiko Hirao. Reversibility of adenine-induced renal failure in rats Clinical Experimental Nephrology. 1999;3(2):82–8. [Google Scholar]
- 31.Tanaka T, Doi K, Maeda-Mamiya R, Negishi K, Portilla D, Sugaya T, et al. Urinary L-type fatty acid-binding protein can reflect renal tubulointerstitial injury. The American journal of pathology. 2009;174(4):1203–11. doi: 10.2353/ajpath.2009.080511 ; PubMed Central PMCID: PMC2671353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hussien NI, Emam HT. The potential protective effects of erythropoietin and estrogen on renal ischemia reperfusion injury in ovariectomized rats. Alexandria Journal of Medicine. 2016;52(4):325–35. https://doi.org/10.1016/j.ajme.2015.12.001. [Google Scholar]
- 33.Ogino A, Takemura G, Kawasaki M, Tsujimoto A, Kanamori H, Li L, et al. Erythropoietin receptor signaling mitigates renal dysfunction-associated heart failure by mechanisms unrelated to relief of anemia. Journal of the American College of Cardiology. 2010;56(23):1949–58. doi: 10.1016/j.jacc.2010.04.068 . [DOI] [PubMed] [Google Scholar]
- 34.Ataka K, Maruyama H, Neichi T, Miyazaki J, Gejyo F. Effects of erythropoietin-gene electrotransfer in rats with adenine-induced renal failure. American journal of nephrology. 2003;23(5):315–23. doi: 72913. doi: 10.1159/000072913 . [DOI] [PubMed] [Google Scholar]
- 35.Morgera S, Heering P, Szentandrasi T, Niederau C, Grabensee B. Erythropoietin in patients with acute renal failure and continuous veno-venous haemofiltration. International urology and nephrology. 1997;29(2):245–50. . [DOI] [PubMed] [Google Scholar]
- 36.Rosenberger C, Heyman SN, Rosen S, Shina A, Goldfarb M, Griethe W, et al. Up-regulation of HIF in experimental acute renal failure: evidence for a protective transcriptional response to hypoxia. Kidney international. 2005;67(2):531–42. doi: 10.1111/j.1523-1755.2005.67110.x . [DOI] [PubMed] [Google Scholar]
- 37.Fong D, Ullah MM, Lal JG, Abdelkader A, Ow CP, Hilliard LM, et al. Renal cellular hypoxia in adenine-induced chronic kidney disease. Clinical and experimental pharmacology & physiology. 2016;43(10):896–905. doi: 10.1111/1440-1681.12621 . [DOI] [PubMed] [Google Scholar]
- 38.Artunc F, Risler T. Serum erythropoietin concentrations and responses to anaemia in patients with or without chronic kidney disease. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association—European Renal Association. 2007;22(10):2900–8. doi: 10.1093/ndt/gfm316 . [DOI] [PubMed] [Google Scholar]
- 39.Zhang ZH, Vaziri ND, Wei F, Cheng XL, Bai X, Zhao YY. An integrated lipidomics and metabolomics reveal nephroprotective effect and biochemical mechanism of Rheum officinale in chronic renal failure. Sci Rep. 2016;6:22151 doi: 10.1038/srep22151 ; PubMed Central PMCID: PMC4763304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Quarles LD. Role of FGF23 in vitamin D and phosphate metabolism: implications in chronic kidney disease. Experimental cell research. 2012;318(9):1040–8. doi: 10.1016/j.yexcr.2012.02.027 ; PubMed Central PMCID: PMC3336874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gutierrez O, Isakova T, Rhee E, Shah A, Holmes J, Collerone G, et al. Fibroblast growth factor-23 mitigates hyperphosphatemia but accentuates calcitriol deficiency in chronic kidney disease. Journal of the American Society of Nephrology: JASN. 2005;16(7):2205–15. doi: 10.1681/ASN.2005010052 . [DOI] [PubMed] [Google Scholar]
- 42.Hideto Okada YM, Yoshiteru Kaneko, katsumori Yoshida, Seiichiro Ozono, Yoshihiko Hirao, Kayoko Furukawa and Takiko Yawata. Branched chain amino acid in adenine-induced uremic rats treated with rHuEPO. Clinical Experimental Nephrology. 2001;5(1):28–32. doi: 10.1007/s101570170028 [Google Scholar]
- 43.Akchurin O, Sureshbabu A, Doty SB, Zhu YS, Patino E, Cunningham-Rundles S, et al. Lack of hepcidin ameliorates anemia and improves growth in an adenine-induced mouse model of chronic kidney disease. American journal of physiology Renal physiology. 2016;311(5):F877–F89. doi: 10.1152/ajprenal.00089.2016 ; PubMed Central PMCID: PMC5130453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun CC, Vaja V, Chen S, Theurl I, Stepanek A, Brown DE, et al. A hepcidin lowering agent mobilizes iron for incorporation into red blood cells in an adenine-induced kidney disease model of anemia in rats. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association—European Renal Association. 2013;28(7):1733–43. doi: 10.1093/ndt/gfs584 ; PubMed Central PMCID: PMC3707526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hung SC, Kuo KL, Peng CH, Wu CH, Wang YC, Tarng DC. Association of fluid retention with anemia and clinical outcomes among patients with chronic kidney disease. Journal of the American Heart Association. 2015;4(1):e001480 doi: 10.1161/JAHA.114.001480 ; PubMed Central PMCID: PMC4330071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lang F, Bissinger R, Abed M, Artunc F. Eryptosis—the Neglected Cause of Anemia in End Stage Renal Disease. Kidney & blood pressure research. 2017;42(4):749–60. doi: 10.1159/000484215 . [DOI] [PubMed] [Google Scholar]
- 47.Abed M, Artunc F, Alzoubi K, Honisch S, Baumann D, Foller M, et al. Suicidal erythrocyte death in end-stage renal disease. Journal of molecular medicine. 2014;92(8):871–9. doi: 10.1007/s00109-014-1151-4 . [DOI] [PubMed] [Google Scholar]
- 48.Bissinger R, Artunc F, Qadri SM, Lang F. Reduced Erythrocyte Survival in Uremic Patients Under Hemodialysis or Peritoneal Dialysis. Kidney & blood pressure research. 2016;41(6):966–77. doi: 10.1159/000452600 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Oral administration of adenine at (A) 25 or 50 mg/kg body weight for 28 days in mice or (B) 200 or 600 mg/kg body weight for 10 days in rats. In mice the observation period was up to 70 days while in rats it was up to 84 days. Arrows (↑) indicate the blood collection time points.
(TIF)
Changes in size and color of kidney during the observation period in (A) mice and (B) rats after treatment with vehicle (0.5% CMC) or adenine (50 mg/kg for mice and 600 mg/kg for rat) at different time points.
(TIF)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.