Relevance of glioblastoma stem cells (GSCs)
Glioblastoma (GBM) is the most frequent, malignant and lethal brain tumor in adults, with an associated 5-year survival of 5% and a median survival of 15 months (1). Current standard treatment includes surgery followed by radiotherapy and chemotherapy with temozolomide (TMZ). However, despite the initial tumor regression, therapy resistance frequently occurs leading to tumor recurrence and death. The presence of a subpopulation of undifferentiated cancer cells, called GSCs, is one of the most critical circumstances promoting the failure of the therapies in GBM. GSCs are quiescent cells that exhibit the stem cell properties of unlimited self-renewal and multilineage differentiation potential, and also resistance to therapies, characteristics that make them responsible for tumor formation and maintenance, as well as recurrence after therapy (2). Since conventional therapies are directed against proliferative cells, do not target quiescent cells as GSCs. Therefore, the identification of specific GSC biomarkers and regulators for their use as molecular targets is a prominent need that has become a priority for therapeutic development.
Integrin α7 functions and implications in cancer
Integrin α7 (ITGA7) belongs to the integrin family of adhesion molecules, which participates in relevant cell-cell and cell-extracellular matrix interactions in a broad range of cellular processes. Integrins are heterodimers consisting of an alpha and a beta subunit. Both subunits are single-pass type I membrane proteins with a large extracellular domain that interacts with extracellular matrix proteins and a short cytoplasmic domain that interacts with cytoskeletal components. The alpha-7 subunit is expressed mainly in skeletal and cardiac muscle and together with integrin beta 1 (ITGB1) conforms a specific cellular receptor for laminins in the basement membrane (3). ITGA7/ITGB1 is involved in the maintenance of the myofibers organization and functionality. The heterodimer also links Schwann cells to laminin and is essential for peripheral nerve development and function (4). In vascular smooth muscle cells (VSMCs) ITGA7/ITGB1 sustains the differentiated contractile phenotype (5). Regarding the implications of ITGA7 in cancer, it acts as a tumor suppressor in melanoma (6), prostate cancer (7,8), leiomyosarcoma (8) and mesothelioma (9). In contrast, ITGA7 is associated with adverse clinicopathological features in oesophageal squamous cell carcinomas, wherein it is involved in the regulation of the subpopulation of cancer stem cells (CSCs) (10). Until now, the participation of ITGA7 in the activity of GSCs and in glioblastoma was unknown.
In an elegant study Haas and collaborators have identified ITGA7 as a specific marker of GSCs and have described in detail its role in this relevant subpopulation of cells (11). Their research, published in Cell Stem Cell, followed an unbiased and unsupervised approach with the purpose of identifying specific surface markers of GSCs. In order to reach this aim, the authors generated a hybridoma library using as immunogen a previously characterized culture of neurospheres derived from a human GBM (GSC1) (12). Through a high-throughput screening based in flow cytometry, they analyzed the ability of the monoclonal antibodies (mAbs) generated to bind GSC1, and also the corresponding isogenic differentiated cells and non-tumoral cells [peripheral blood leucocytes (PBLs)]. They selected those antibodies that presented no affinity for PBLs and a binding ratio of 1.8-fold for GSCs respect to the correspondent differentiated cells. After validating the binding properties of the selected antibodies in additional independent primary GSC cultures, the authors selected those able to bind GSCs also in monolayer culture conditions. After certifying that these antibodies did not bind to different commercial brain tumor cell lines, they focused on the antibody exhibiting the most robust binding properties in a panel of different primary GBM lines, the mAb named 1.4A12 (Figure 1) (11). Then, the authors validated the binding of 1.4A12 to GSCs and human GBM samples by immunofluorescence analysis, noticing a low binding to differentiated GSCs and an enrichment in the perivascular areas of GBMs. After that, the phenotype of GBM cells exhibiting high or low 1.4A12 binding was compared. For that, they used tumor cells freshly dissociated from xenograft tumors generated with primary spheroid GBM cultures established from GBM patients. They performed fluorescence activated cell sorting (FACS) based on the binding of 1.4A12 and found that, in vitro, cells exhibiting high 1.4A12 binding were more proliferative, contained a higher number of clonogenic cells and exhibited an enhanced sphere formation capacity respect to cells presenting low binding. This aggressive phenotype was accompanied by high expression of genes involved in proliferation and CSC biology, and low expression of genes driving neuronal differentiation. Accordingly, high 1.4A12 binding cells were more tumorigenic when they were orthotopically implanted in mice and formed tumors that grew faster, reducing significantly the survival of mice respect to mice developing tumors from low 1.4A12 binding cells (Figure 1) (11). Thereby, through experiments of immunoprecipitation using 1.4A12 in biotinylated GSC1 cells, followed by mass spectrometry procedures, they deciphered that the selected antibody recognized ITGA7 and/or its partner ITGB1. Finally, through transduction and knockdown approaches in cell lines, followed by the evaluation of the 1.4A12 binding, the authors concluded that the direct antigen of 1.4A12 was ITGA7 (11), a marker never before analyzed in GSCs.
Figure 1.
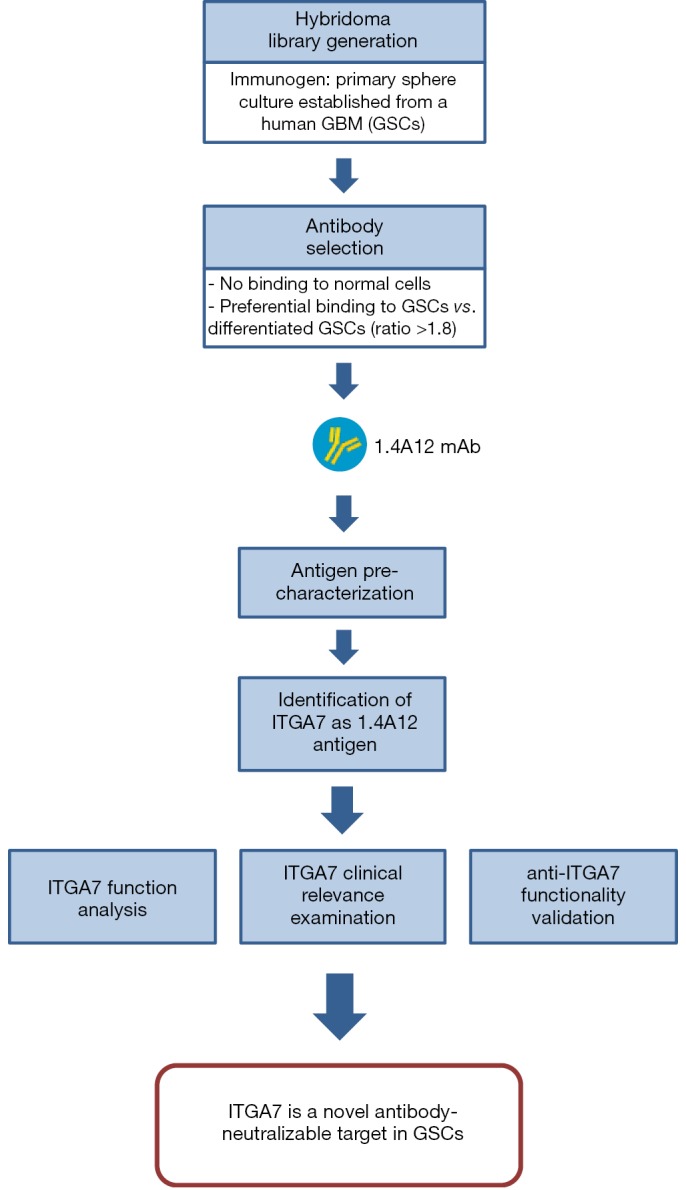
Methodological strategy used to identify ITGA7 as a novel functional marker of GSCs associated with poor prognosis of GBM patients. GSCs, glioblastoma stem cells; GBM, glioblastoma.
To unravel more deeply the oncogenic function of ITGA7, the authors performed several functional studies and analyzed different available clinical datasets (Figure 1). Thus, through reverse-phase protein arrays (RPPA) in GSCs derived from patients and submitted to ITGA7 silencing by shRNA, they found consistent changes affecting cell cycle-regulating proteins, the oncogenic transcription factor FoxM1, as well as the phosphorylation status of p38 MAPK and members of the PI3K/AKT pathway. The effect on p38 and AKT was confirmed by Western blot and reproduced, albeit modestly, in response to the anti-ITGA7 antibody. Reduced levels of FoxM1 with ITGA7 knockdown were also confirmed and diminished phosphorylation of its regulator FOXO3a was reported. Consistently, the expression of FoxM1 target genes was reduced in ITGA7-silenced GSCs. The study of cycle-regulating proteins such us p27, Skp2 or cyclin B by Western blot in ITGA7-silenced cells revealed a molecular context against the entry into the S phase of the cell cycle, effect that was parallelled by a cellular arrest in G0/1 phase in cell cycle analysis. Moreover, the authors found that ITGB1 silencing provoked the same effect on the analyzed cell cycle-regulating proteins, attributing the observed phenotype to the ITGA7/β1 dimer (11). They showed that ITG7 and also ITGB1 silencing reduced the proliferation and the clonogenic survival of GSC cells. Furthermore, pharmacological inhibition of AKT, but not p38, reproduced the growth impairment, showing the relevance of AKT in the ITGA7-mediated proliferation. Interestingly, ITGA7 silencing reduced the tumorigenicity of GSCs in heterotopic and orthotopic xenografts, having a significant impact in tumor growth and mice survival (11). Since the ITGA7/β1 dimer is involved in muscle cell motility (13), Haas and collaborators analyzed this aspect and revealed that ITG7A silencing decreased the spreading of the GSCs into matrigel and their invasion in laminin, being the effect on invasion reproduced by ITGB1 knockdown. ITGA7 knockdown abolished the phosphorylation of Src and FAK kinases induced by laminin, suggesting that ITG7A is critical in the signaling initiated by components of the extracellular matrix. The authors also showed that the pharmacological inhibition of p38, but not AKT, reduced the invasive capacity of GSCs, suggesting that the phenotype may rely on the effect on p38. However, they proved that 1.4A12 was able to inhibit the spreading of GSCs into matrigel and their invasion in laminin without affecting phospho-p38 levels and having a marked impact on laminin-induced Src and FAK phosphorylation (11). Then, the authors went a step forward to assess the clinical relevance of ITGA7 (Figure 1). Thus, after certifying the positive correlation between ITGA7 protein and mRNA expression levels in different GSCs and conventional cell lines, they analyzed the Repository of Molecular Brain Neoplasia Data (REMBRADT) datasets (14) and the microarray data obtained in an independent study with glioma patients (GEO accession number GSE4290) (15), and found ITGA7 overexpression in human glioma samples in a progressively increasing manner from grade II to grade IV. Using REMBRADT and TCGA datasets they also determined an association of ITGA7 high expression with lower overall survival in low-grade gliomas and also in GBM, this finding being extrapolated to three other independent cohorts of GBM patients. TCGA data revealed the lowest ITGA7 expression for the proneural subtype of GBMs, wherein ITGA7 expression was heterogenous and a robust prognostic marker (11). Furthermore, underlining the potential of ITG7A as a molecular target, they determined by flow cytometry that the expression of this marker was much lower in the surface of human neural progenitor cells (NHNPs) respect to GSC lines. Haas and collaborators determined that other α integrins partners of ITGB1 such as ITGA3 or ITGA6 were present in the surface of GSCs, yet their expression was less abundant and their prognostic value in patients was weaker. Considering all the implications of ITG7A in the biology of the GSCs and its clinical relevance, the authors evaluated the capabilities of the antibody generated in their study (Figure 1). Thus, through in vitro experiments with cell lines they showed that 1.4A12 not only marked ITGA7+ cells, but also interfered the binding of ITGA7 to laminin. In vivo, anti-ITGA7 treatment suppressed tumor growth in subcutaneous xenografts and its effect on FAK and AKT activation was confirmed in formed tumors. Furthermore, having shown the ability of the antibody to reduce the invasion of GSCs in vitro, the authors demonstrated its effectiveness also in intracranial xenografts, showing very limited brain invasion in anti-ITGA7-treated mice respect to control mice, which reached larger tumor volumes, exhibited a significant shorter survival and presented a higher number of tumor cells infiltrating diverse brain regions (11).
In summary, the work of Haas and collaborators brings valuable new information in the field of GBM treatment, for the targeting of GSCs in particular. Spheres derived from GBM samples represent valid models to study GSC markers, yet their analysis commonly has followed supervised approaches and has not been systematic, providing conflicting results (16). So far, no studies had displayed a hybridoma screening method for the search of surface markers in GSCs. In this way, the authors have identified ITGA7 as a novel functional marker of GSCs involved in their proliferation and invasion through the activation of FAK, AKT and Src. Furthermore, while the clinical relevance of other putative GSC markers is null or not robustly demonstrated, Haas et al. have determined that high ITGA7 expression in GBM is associated with reduced survival in five independent cohorts of GBM patients. From a translational point of view, it is remarkable that ITGA7 expression is much lower in normal human neural progenitor cells respect to GSCs, fact that raises the possibility of a specific GSC targeting. The study also demonstrates the effectiveness of the antibody-based ITGA7 neutralization in vitro and in vivo, so it provides evidence that could be sufficient to foster the implementation of therapeutic strategies aimed at ITGA7 targeting in GBM.
Acknowledgements
Funding: J Auzmendi-Iriarte is a recipient of predoctoral fellowship from the University of the Basque Country. The laboratory of A Matheu is supported by grants from the Instituto Salud Carlos III and FEDER funds (PI13/02277, CP16/00039, PI16/01580, DTS16/0184), Industry and Health Departments of the Basque Government, Diputacion Gipuzkoa and the European Union (Marie Curie CIG 2012/712404).
Provenance: This is an invited Editorial commissioned by Editor-in-Chief Zhizhuang Joe Zhao (Pathology Graduate Program, University of Oklahoma Health Sciences Center, Oklahoma City, USA).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Ostrom QT, Bauchet L, Davis FG, et al. The epidemiology of glioma in adults: a "state of the science" review. Neuro Oncol 2014;16:896-913. 10.1093/neuonc/nou087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen J, Li Y, Yu TS, et al. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature 2012;488:522-6. 10.1038/nature11287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.von der Mark H, Williams I, Wendler O, et al. Alternative splice variants of alpha 7 beta 1 integrin selectively recognize different laminin isoforms. J Biol Chem 2002;277:6012-6. 10.1074/jbc.M102188200 [DOI] [PubMed] [Google Scholar]
- 4.Chernousov MA, Kaufman SJ, Stahl RC, et al. Alpha7beta1 integrin is a receptor for laminin-2 on Schwann cells. Glia 2007;55:1134-44. 10.1002/glia.20536 [DOI] [PubMed] [Google Scholar]
- 5.Wang L, Zheng J, Du Y, et al. Cartilage oligomeric matrix protein maintains the contractile phenotype of vascular smooth muscle cells by interacting with alpha(7)beta(1) integrin. Circ Res 2010;106:514-25. 10.1161/CIRCRESAHA.109.202762 [DOI] [PubMed] [Google Scholar]
- 6.Ziober BL, Chen YQ, Ramos DM, et al. Expression of the alpha7beta1 laminin receptor suppresses melanoma growth and metastatic potential. Cell Growth Differ 1999;10:479-90. [PubMed] [Google Scholar]
- 7.Tan LZ, Song Y, Nelson J, et al. Integrin alpha7 binds tissue inhibitor of metalloproteinase 3 to suppress growth of prostate cancer cells. Am J Pathol 2013;183:831-40. 10.1016/j.ajpath.2013.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ren B, Yu YP, Tseng GC, et al. Analysis of integrin alpha7 mutations in prostate cancer, liver cancer, glioblastoma multiforme, and leiomyosarcoma. J Natl Cancer Inst 2007;99:868-80. 10.1093/jnci/djk199 [DOI] [PubMed] [Google Scholar]
- 9.Burkin DJ, Fontelonga TM. Mesothelioma cells breaking bad: loss of integrin alpha7 promotes cell motility and poor clinical outcomes in patients. J Pathol 2015;237:282-4. 10.1002/path.4587 [DOI] [PubMed] [Google Scholar]
- 10.Ming XY, Fu L, Zhang LY, et al. Integrin alpha7 is a functional cancer stem cell surface marker in oesophageal squamous cell carcinoma. Nat Commun 2016;7:13568. 10.1038/ncomms13568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haas TL, Sciuto MR, Brunetto L, et al. Integrin alpha7 Is a functional marker and potential therapeutic target in glioblastoma. Cell Stem Cell 2017;21:35-50.e9. 10.1016/j.stem.2017.04.009 [DOI] [PubMed] [Google Scholar]
- 12.Ricci-Vitiani L, Pallini R, Larocca LM, et al. Mesenchymal differentiation of glioblastoma stem cells. Cell Death Differ 2008;15:1491-8. 10.1038/cdd.2008.72 [DOI] [PubMed] [Google Scholar]
- 13.Yao CC, Ziober BL, Squillace RM, et al. Alpha7 integrin mediates cell adhesion and migration on specific laminin isoforms. J Biol Chem 1996;271:25598-603. 10.1074/jbc.271.41.25598 [DOI] [PubMed] [Google Scholar]
- 14.Madhavan S, Zenklusen JC, Kotliarov Y, et al. Rembrandt: helping personalized medicine become a reality through integrative translational research. Mol Cancer Res 2009;7:157-67. 10.1158/1541-7786.MCR-08-0435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun L, Hui AM, Su Q, et al. Neuronal and glioma-derived stem cell factor induces angiogenesis within the brain. Cancer Cell 2006;9:287-300. 10.1016/j.ccr.2006.03.003 [DOI] [PubMed] [Google Scholar]
- 16.Carrasco-Garcia E, Sampron N, Aldaz P, et al. Therapeutic strategies targeting glioblastoma stem cells. Recent Pat Anticancer Drug Discov 2013;8:216-27. 10.2174/15748928113089990002 [DOI] [PubMed] [Google Scholar]


