Abstract
Minimally invasive surgical techniques are important in surgical management of thymic pathologies. Traditional access techniques are being replaced with minimally invasive techniques using multiportal or uniportal approach. Adoption of minimally invasive techniques for thymic malignancies has been slow due to long term recurrence concerns. Recent studies show that minimally invasive video-assisted thoracoscopic surgery (VATS) or robotic approach to early stage thymic malignancies are associated with less intraoperative bleeding, lower rate of respiratory complications, shorter chest tube duration and shorter hospital stay. Oncologic outcomes are at least equivalent to open approach. Minimally invasive approach for benign pathologies is widely applied. There are significant variations in VATS approaches for thymus, showing a multinational interest in the issue of minimizing trauma during thymectomy. Use of robotic technology is also popular, as the retrosternal area is a narrow anatomic space to manipulate conventional instruments. The evolution of minimally invasive surgery for thymus has been possible with contribution from centers all around the world. In the current practice, various approaches are being adopted and every surgeon should prefer a technique depending on surgical preference and experience.
Keywords: Video-assisted thoracoscopic surgery (VATS), thymectomy, thymomectomy, subxiphoid
Minimally invasive surgical techniques play a very important role in the contemporary surgical management of intrathoracic pathologies. Thymic surgery has also evolved in the last two decades with minimally invasive surgical techniques becoming the preferred approach. Traditional access to the anterior mediastinum for thymic surgery required a median sternotomy, however due to morbidity of sternotomy, transcervical access to anterior mediastinum was also popular in many centers (1). Minimally invasive visualization and techniques enabled surgeons to have access to the anterior mediastinum through right and/or left chest and recently through subxiphoid area using multiportal or uniportal approach (2-4).
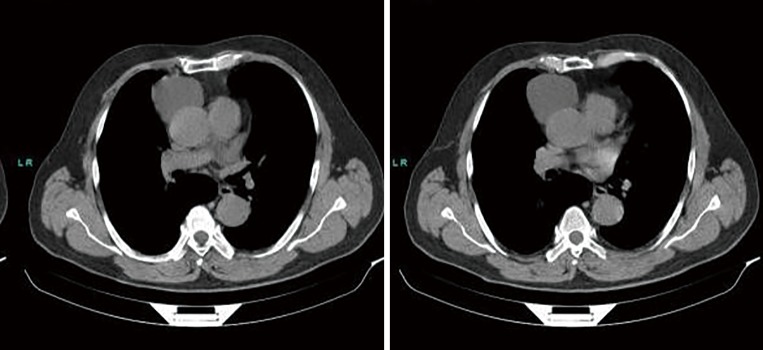
The adoption of minimally invasive techniques in benign thymic pathologies (Figure 1) has been fast, however it was slow for thymic malignancies, mainly due to the concerns of increased manipulation of the tumor, capsular disruption, pleuropericardial seeding, incomplete resections and thus an increased incidence of locoregional recurrence (5). Open resection of early stage thymoma results in excellent long term survival (90%) and very low rate (<5%) of recurrence (5). However recent studies show that minimally invasive video-assisted thoracoscopic surgery (VATS) or robotic approach to early stage thymic malignancies are associated with less intraoperative bleeding, lower rate of respiratory complications, shorter chest tube duration and shorter hospital stay (6). Conversion rates of minimally invasive techniques for thymic tumors are in single digit numbers. Oncologic outcomes are at least equivalent to open approach.
Figure 1.
A case of anterior mediastinal thymic cyst in a 52-year-old male patient. It was removed using a right uniportal VATS technique. VATS, video-assisted thoracoscopic surgery.
For thymomas, principles of minimally invasive resection were published by International Thymic Malignancy Interest Group (7). These principles were:
No rib spreading or sternal cutting with an intent for complete resection with visualization on a video monitor (Figure 2);
Resection of thymoma, thymus and mediastinal fat (Figure 3);
Dissection and visualization of innominate vein and both phrenic nerves (Figure 4);
Conversion to open surgery should be performed if oncologic principles are not followed such as disruption of the capsule, incomplete resection, risk of a discontinuous (not en bloc) resection or disruption of the tissues exposing the tumor;
Incision for retrieval should be large enough to prevent specimen disruption;
Exploration of pleura should be done if the thymoma invades the mediastinal pleura;
Always remove the specimen in the bag;
Examine removed specimen for completeness of the resection;
Communicate with pathologist for suspicious areas, analysis and orientation of the specimen.
Figure 2.
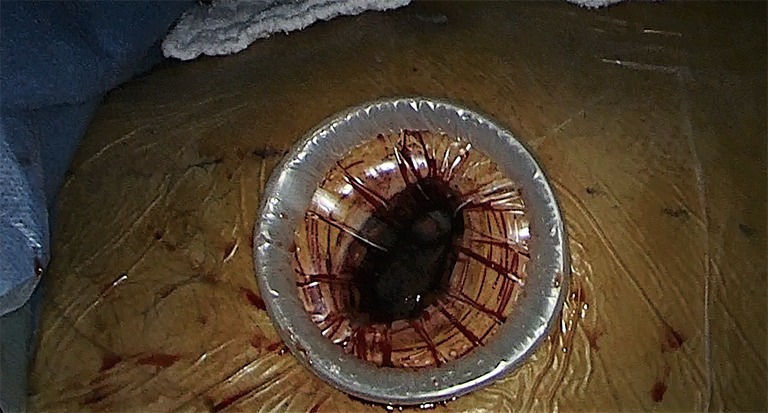
Uniportal incision for anterior mediastinal access on the 5th intercostal space between anterior and posterior axillary line.
Figure 3.
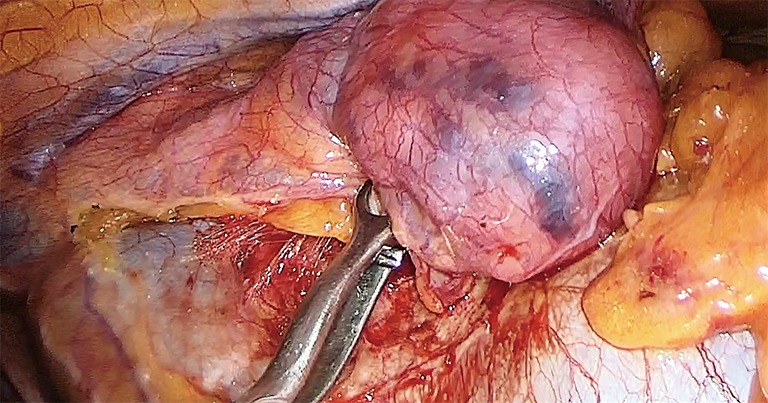
A 5-cm thymoma is seen which was elevated from the pericardium and vena cava.
Figure 4.
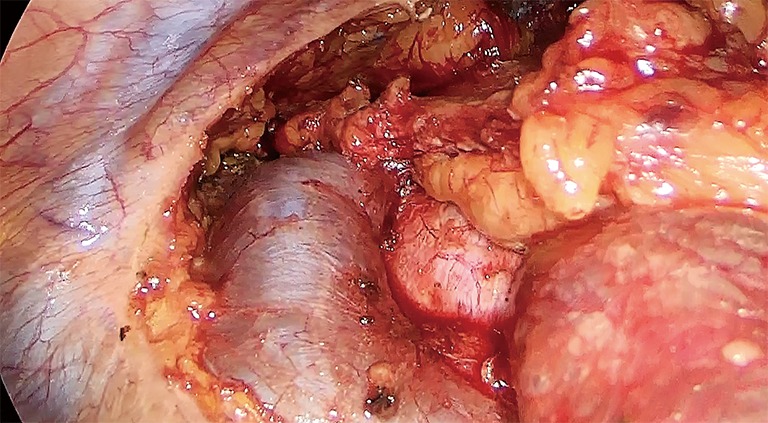
Innominate vein can be dissected under direct vision and with good access to the superior and inferior sides.
Minimally invasive extended thymectomy is currently the primary surgical technique for myasthenia gravis. It results in lower rate of respiratory complications and need for postoperative ventilator support, less pain and shorter hospital stay (8).
The use of minimally invasive approach for other benign pathologies (mainly cysts and benign tumors such as teratomas) of the thymus is straightforward and tailored according to the location and size of the lesion.
Technical approaches across the globe
There are significant variations in VATS approaches for thymus. In the early times of VATS, triportal right sided approach was the most widely adopted technique and it is still commonly practiced by many centers across the globe. However, the technique has limitations when the lesion extends to the left side and for clear visualization of left phrenic nerve. Thus approaches through the left chest and/or subxiphoid area were either added or performed solely depending on the localization of the lesion and preference of the surgical team. Uniportal, multiportal and robotic assisted subxiphoid thymectomy technique was developed in Poland, Japan and China showing a multinational interest in the issue of minimizing trauma during thymectomy (2,3,9). In the beginning, subxiphoid approach was combined with right thoracoscopy and even a cervical incision to perform maximal thymectomy. It was later refined to multi- or uniportal approach from the subxiphoid region. Subxiphoid approach allows the surgeon to see both phrenic nerves very clearly and reach high into the anterior mediastinum under direct vision. The difficulty arises when patient has a large pericardial fat pad and the recommendation is to remove part of pericardial fat pad for better visualization before proceeding to thymectomy. In one report subxiphoid thymectomy was found to have a shorter operating time and cause less bleeding compared with the VATS approach (10).
Use of robotic technology in thymic surgery also became popular, as the retrosternal area is a narrow anatomic space to manipulate instruments intra- and extracorporeally, especially in females with large breasts. Robotic arms are more stable with better dexterity in such difficult to reach areas. Robotic thymectomy was routinely performed by specialized centers in Germany and Turkey and several papers were published about the technique and results (11,12). German group showed that robotic thymectomy resulted in higher remission rates than thoracoscopic thymectomy (39% to 20% respectively). This was attributed to a higher rate of complete thymectomy especially in anatomically difficult cases (11).
A uniportal approach from the 4th or 5th intercostal space, anterior axillary line has been described for resection of thymic lesions. Twenty-nine patients were operated with 13 thymectomies (8 extended) (2). There was no mortality or morbidity.
In conclusion, the evolution of minimally invasive surgery for thymus has been possible with contribution from centers all around the world. In the current practice, various approaches are being adopted and every surgeon should prefer their technique depending on surgical preference and experience.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- 1.Shrager JB, Nathan D, Brinster CJ, et al. Outcomes after 151 extended transcervical thymectomies for myasthenia gravis. Ann Thorac Surg 2006;82:1863-9. 10.1016/j.athoracsur.2006.05.110 [DOI] [PubMed] [Google Scholar]
- 2.Wu CF, Gonzalez-Rivas D, Wen CT, et al. Single-port video-assisted thoracoscopic mediastinal tumour resection. Interact Cardiovasc Thorac Surg 2015;21:644-9. 10.1093/icvts/ivv224 [DOI] [PubMed] [Google Scholar]
- 3.Zieliński M, Rybak M, Wilkojc M, et al. Subxiphoid video-assisted thorascopic thymectomy for thymoma. Ann Cardiothorac Surg 2015;4:564-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yim AP, Izzat MB, Lee TW, et al. Video-assisted thoracoscopic thymectomy. Ann Thorac Cardiovasc Surg 1999;5:18-20. [PubMed] [Google Scholar]
- 5.Friedant AJ, Handorf EA, Su S, et al. Minimally Invasive versus Open Thymectomy for Thymic Malignancies: Systematic Review and Meta-Analysis. J Thorac Oncol 2016;11:30-8. 10.1016/j.jtho.2015.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Batirel HF. Early stage thymoma: is VATS the new standard of care? J Thorac Dis 2016;8:1431-3. 10.21037/jtd.2016.05.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toker A, Sonett J, Zielinski M, et al. Standard terms, definitions, and policies for minimally invasive resection of thymoma. J Thorac Oncol 2011;6:S1739-42. 10.1097/JTO.0b013e31821ea553 [DOI] [PubMed] [Google Scholar]
- 8.Jurado J, Javidfar J, Newmark A, et al. Minimally invasive thymectomy and open thymectomy: outcome analysis of 263 patients. Ann Thorac Surg 2012;94:974-81; discussion 981-2. 10.1016/j.athoracsur.2012.04.097 [DOI] [PubMed] [Google Scholar]
- 9.Wang H, Gu Z, Ding J, et al. Perioperative outcomes and long-term survival in clinically early-stage thymic malignancies: video-assisted thoracoscopic thymectomy versus open approaches. J Thorac Dis 2016;8:673-9. 10.21037/jtd.2016.03.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yano M, Moriyama S, Haneda H, et al. The Subxiphoid Approach Leads to Less Invasive Thoracoscopic Thymectomy Than the Lateral Approach. World J Surg 2017;41:763-70. 10.1007/s00268-016-3783-8 [DOI] [PubMed] [Google Scholar]
- 11.Rückert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg 2011;141:673-7. 10.1016/j.jtcvs.2010.11.042 [DOI] [PubMed] [Google Scholar]
- 12.Kaba E, Cosgun T, Ayalp K, et al. Robotic thymectomy-a new approach for thymus. J Vis Surg 2017;3:67. 10.21037/jovs.2017.03.28 [DOI] [PMC free article] [PubMed] [Google Scholar]