Abstract
Background
Aggressive management of patients prior to and after determination of death by neurologic criteria (DNC) is necessary to optimize organ recovery, transplantation, and increase the number of organs transplanted per donor (OTPD). The effects of time management are understudied but potentially pivotal component. The objective of this study was to analyze specific time points (time to DNC, time to procurement) and the time intervals between them to better characterize the optimal timeline of organ donation.
Methods
Using data over a 5-year time period (2011–2015) from the largest US OPO, all patients with catastrophic brain injury and donated transplantable organs were retrospectively reviewed. Active smokers were excluded. Maximum donor potential was seven organs (heart, lungs [2], kidneys [2], liver, and pancreas). Time from admission to declaration of DNC and donation was calculated. Mean time points stratified by specific organ procurement rates and overall OTPD were compared using unpaired t-test.
Results
Of 1719 Declaration of Death by Neurologic Criteria organ donors, 381 were secondary to head trauma. Smokers and organs recovered but not transplanted were excluded leaving 297 patients. Males comprised 78.8%, the mean age was 36.0 (±16.8) years, and 87.6% were treated at a trauma center. Higher donor potential (>4 OTPD) was associated with shorter average times from admission to brain death; 66.6 versus 82.2 hours, P = 0.04. Lung donors were also associated with shorter average times from admission to brain death; 61.6 versus 83.6 hours, P = 0.004. The time interval from DNC to donation varied minimally among groups and did not affect donation rates.
Conclusions
A shorter time interval between admission and declaration of DNC was associated with increased OTPD, especially lungs. Further research to identify what role timing plays in the management of the potential organ donor and how that relates to donor management goals is needed.
Keywords: Transplant donor pool, Organ donor management, Donor management guidelines, Lung transplantation, Brain death declaration
Introduction
Expanding the donor pool and increasing the number of transplantable organs is essential to counter the growing list of transplant candidates. A major target in increasing the donor pool is the critical care management of the patient who progresses to death by neurologic criteria (DNC). Donor management goals (DMGs) and catastrophic brain injury guidelines (CBIGs) have been developed to optimize the potential organ donor to increase the number of organs transplanted per donor (OTPD).1–4 Studies have shown that a higher compliance with DMGs and CBIGs results in a higher number of OTPD.5–10
An area not commonly addressed or included in CBIGs, when considering the management of a DNC donor, is the optimal timing of organ procurement. At time of DNC, a systemic change occurs affecting all organ systems, including cardiovascular, pulmonary, and endocrine.11 As a result, cardiopulmonary death can occur prior to procurement resulting in a reported loss of 25% of potential donors.12 Therefore, prevailing logic has been that organ procurement should occur as closely to DNC as possible to avoid complications related to these systemic changes.
However, emerging literature has put this dogma into question, with evidence to suggest that instituting a period of organ optimization prior to procurement may increase OTPD.13–16 Malinoski et al. showed that although few patients met DMGs at the time of consent for donation, a higher number were met at time of procurement, which led to an increased number of OTPD.17
The purpose of this study was to study the effect of time on organ donation to better characterize an optimal timeline for organ donation. Our aim was to determine whether procurement should be delayed to allow time to meet more DMGs or if prolongation would place undue risk to the potential organs for donation with an increased risk of somatic death occurring prior to procurement, resulting in a loss of donor potential. We hypothesized that potential donors would benefit from a longer time interval from injury to procurement, allowing for critical care management and optimization of transplantable organs.
Methods
Institutional review board approval was obtained for this study. This was a retrospective review using the Gift of Life (GOL) database. GOL is one of the largest organ procurement organizations (OPO) in the nation. A nonprofit organization, it serves the eastern half of Pennsylvania, southern New Jersey, and Delaware. GOL has a recovery facility, but it was not used clinically during the study period; all organs were recovered at the treating acute care hospital. Within the GOL catchment area, there are 15 transplant centers.
Data were reviewed for all nonsmoking adult organ donors from 2011–2015, who suffered head trauma that progressed to DNC. Seven organs were considered in the data collection: heart, two lungs, two kidneys, liver, and pancreas. Smokers were actively excluded so as not to bias the data against lung transplantation specifically due to tobacco use. Pediatric donors were excluded as the pathophysiology of their injuries and their donor management physiology were likely very different than that of an adult. We also excluded small bowel transplantation from our study because its use is extremely rare in our OPO. Only one patient donated small bowel during our study period.
In 2015, the Society of Critical Care Medicine, the American College of Chest Physicians, and the Association of Organ Procurement Organizations published recommendations for organ donor management.2 On the basis of these recommendations, and other prospective studies validating critical care endpoints as DMGs,6,17 seven DMGs were chosen (vasopressor use ≤ 1, mean arterial blood pressure > 60, ejection fraction > 45%, sodium < 155 mEq/L, glucose < 150 mg/dL, PaO2:FiO2 ratio > 300, and average urine output (UOP) of 0.05–3 mL/kg/h), in addition to the use of hormonal therapy at any time point (T4, steroids, and insulin), serum creatinine, and ventilator settings at time of procurement, as a measure of donor optimization during their time in intensive care. Additional variables obtained from the GOL database included demographics, treatment facilities, and comorbidities of each potential donor.
Different time points (time of patient admission, declaration of DNC, and procurement) were obtained from the GOL database. These time points were used to calculate time from admission to declaration of DNC (AtoD), time from declaration of DNC to procurement (DtoP), and the overall time from admission to procurement (AtoP).
The Health Resources and Science Administration set the national goal for organ donation to be 3.75 organs transplanted per donor. Therefore, the primary outcome measure was having greater than four organs transplanted per donor. We did not capture data on organs that were recovered but never transplanted.
The study populations were compared based on the number of organs transplanted per donor, > 4 and ≤ 4, and by individual organ. Continuous variables were compared using Student’s t-test, whereas dichotomous variables were compared using chi-square or Fisher’s exact test, as appropriate. Values are reported as mean ± standard deviation (SD) for continuous variables and as percentages for categorical variables. All statistical analysis was performed using Statistical Package for Social Sciences (SPSS), version 24.0.
Results
Over the 5-year period, 1719 DNC organ donors were identified. Three hundred eighty-one were declared secondary to head trauma. Excluding smokers and patients who had non-transplantable organs recovered, 297 patients remained for analysis. The majority of donors were treated at trauma (n = 26, 87.9%) and transplant (n = 154, 51.9%) centers. The average age was 36.0 ± 16.9 years, 79.1% (n = 235) were male. When comparing the populations of those who donated greater or less than four organs, the two populations were equivalent in respect to demographics, mechanism of injury, treatment facilities, and hormonal use. Donors who had more than four organs transplanted were younger (28.6 ± 10.1 years) than those who donated less than four organs (41.3 ± 18.6 years, P < 0.001). Description of all patient baseline characteristics can be seen in Table 1. A small proportion of donors met all seven DMGs (n = 12, 4.0%), and there was no difference between the >4 and ≤4 OTPD groups (4, 3.3% versus 8, 4.6%; P = 0.13). A complete comparison of donor management and DMGs met were shown in Table 2.
Table 1.
Donor demographics and baseline characteristics.
| Variable | Overall (n = 297) | OTPD > 4 (n = 123) | OTPD ≤ 4 (n = 174) | P value |
|---|---|---|---|---|
| Male | 235 (79.1%) | 100 (81.3%) | 135 (77.6%) | 0.47 |
| Age | 36.0 ± 16.9 | 28.6 ± 10.1 | 41.3 ± 18.6 | <0.001 |
| Body mass index (BMI) | 27.3 ± 5.7 | 25.9 ± 5.3 | 28.3 ± 5.8 | <0.001 |
| Transplant center | 154 (51.9%) | 65 (52.8%) | 89 (51.1%) | 0.81 |
| Trauma center | 261 (87.9%) | 107 (87%) | 154 (88.5%) | 0.72 |
| Penetrating mechanism | 83 (27.9%) | 41 (33.3%) | 42 (24.1%) | 0.09 |
| Race | ||||
| Black | 59 (19.9%) | 27 (22.0%) | 32 (18.4%) | 0.46 |
| White | 205 (69%) | 77 (62.6%) | 128 (73.6%) | 0.06 |
| Comorbidities | ||||
| DM | 15 (5.05%) | 2 (1.6%) | 13 (7.5%) | 0.03 |
| HTN | 45 (15.2%) | 8 (6.5%) | 29 (22%) | <0.001 |
Bold values indicate statistical significance at P < 0.05.
Table 2.
Critical care management and DMGs.
| Variable | Overall (n = 297) | OTPD > 4 (n = 123) | OTPD ≤ 4 (n = 174) | P value |
|---|---|---|---|---|
| Hormonal therapy | 295 (99.3%) | 121 (98.4%) | 174 (100%) | 0.17 |
| Creatinine | 1.27 ± 1.04 | 1.15 ± 0.65 | 1.36 ± 1.2 | 0.09 |
| TV/Kg | 8.89 ± 1.63 | 9.0 ± 1.5 | 8.8 ± 1.7 | 0.17 |
| DMGs met | ||||
| ≤1 vasopressor used | 236 (79.5%) | 104 (84.6%) | 132 (75.9%) | 0.08 |
| MAP > 60-mm Hg | 264 (88.89%) | 110 (89.4%) | 154 (88.5%) | 0.85 |
| Ejection fraction > 45% | 226/250 (90.4%) | 112 (91.1%) | 114 (65.5%) | 0.52 |
| Sodium < 155 mEq/L | 266 (89.6%) | 107 (87.0%) | 159 (91.4%) | 0.25 |
| Glucose < 150 mg/dL | 77 (25.9%) | 31 (25.2%) | 46 (26.4%) | 0.89 |
| Average urine output (0.05–3 mL/kg/h) | 182 (61.3%) | 66 (53.7%) | 116 (66.7%) | 0.03 |
| PaO2:FiO2 ratio > 300 | 161 (54.2%) | 98 (79.7%) | 63 (36.2%) | <0.001 |
MAP = mean arterial blood pressure; TV/Kg = tidal volume per kilogram.
Bold values indicate statistical significance at P < 0.05.
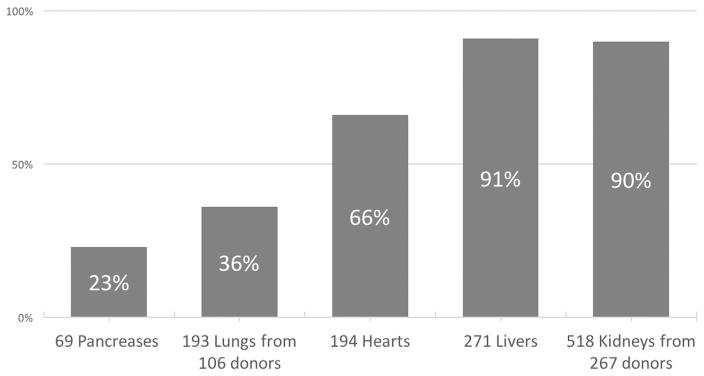
Overall, 1245 organs were transplanted from 297 donors. The most frequently transplanted organs were liver and kidney, followed by heart, lungs, and pancreas. The mean number of OTPD was 4.21 ± 1.66 and 41.4% (n = 123) donated > 4 organs. A full description of numbers of donors donating individual organs is displayed in Figure 1, and the distribution of donated organs between OTPD groups is shown in Table 3. Almost all donors (n = 267, 97%) donated transplantable kidneys; however, only 36% (n = 106) had lungs procured for transplantation. There was a disproportionate distribution of specific organs transplanted between the two cohorts. Donors with >4 OTPD donated 91.7% (n = 177, P < 0.001) of all lungs transplanted. Likewise, significantly, more pancreases were transplanted from donors with OTPD > 4 than those with ≤4 OTPD, 69 (91.3%) and 6 (8.7%, P < 0.001) respectively.
Fig. 1.
Percentage of organ donors, by specific organ. Total: 1245 organs from 297 donors.
Table 3.
Distribution of transplanted organs.
| Organs transplanted | OTPD > 4 (n, %) | OTPD ≤ 4 (n, %) | P value |
|---|---|---|---|
| Heart (n = 194) | 110 (56.7) | 84 (43.3) | <0.001 |
| Lung (n = 193) | 177 (91.7) | 16 (8.3) | <0.001 |
| Liver (n = 271) | 119 (43.9) | 152 (56.0) | 0.006 |
| Pancreas (n = 69) | 69 (91.3) | 6 (8.7) | <0.001 |
| Kidneys (n = 518) | 244 (47.1) | 274 (52.8) | <0.001 |
Bold values indicate statistical significance at P < 0.05.
Average times covered a wide range in the time periods measured. The average time from AtoP was 75.73 ± 63.55 hours, the largest variation in time spans was in the AtoD period, averaging 45.42 ± 63.00 hours. Conversely, there was minimal variation in the average time from DtoP, 30.32 ± 10.89 hours. Donors with >4 OTPD had shorter times from AtoP (66.62 ± 45.12 hours) than patients who donated ≤4 (82.18 ± 73.30 hours, P = 0.04). AtoD times were shorter in donors with >4 OTPD (34.98 ± 44.20 hours versus 52.79 ± 72.68 hours, P = 0.02). However, there was no significant difference between the time from DtoP between the groups.
Comparison of the 3 time periods by organ donated is shown in Table 4. Those who donated lungs had shorter AtoD (29.93 ± 37.45 hours) and AtoP (61.55 ± 38.53 hours) lengths of time than those who did not donate lungs (AtoD: 54.01 ± 72.12, P = 0.002 and AtoP: 83.61 ± 72.78, P = 0.004). A different trend was seen in those who donated hearts and kidneys. A longer AtoP time was associated with increased donation of heart and kidneys. There was no difference between any of the time periods and the donation of livers or pancreases.
Table 4.
Temporal relationship to organs donated.
| Variable | Admit to DDNC (hours) | P value | DDNC to procurement (hours) | P value | Admit to procurement (hours) | P value |
|---|---|---|---|---|---|---|
| Overall mean | 45.42 ± 63.00 | 30.32 ± 10.89 | 75.73 ± 63.55 | |||
| >4 OTPD | 34.98 ± 44.20 | 0.02 | 31.63 ± 9.62 | 0.08 | 66.62 ± 45.12 | 0.04 |
| ≤4 OTPD | 52.79 ± 72.68 | 29.39 ± 11.65 | 82.18 ± 73.30 | |||
| Heart | 49.45 ± 68.69 | 0.13 | 31.75 ± 10.04 | 0.002 | 81.20 ± 68.41 | 0.04 |
| No heart | 37.82 ± 50.02 | 27.62 ± 11.93 | 65.44 ± 51.97 | |||
| Lung | 29.93 ± 37.45 | 0.002 | 31.61 ± 9.92 | 0.11 | 61.55 ± 38.53 | 0.004 |
| No lung | 54.01 ± 72.12 | 29.6 ± 11.36 | 83.61 ± 72.78 | |||
| Liver | 46.38 ± 64.36 | 0.28 | 30.52 ± 10.687 | 0.39 | 76.89 ± 64.50 | 0.24 |
| No liver | 35.42 ± 46.37 | 28.23 ± 12.90 | 63.65 ± 52.14 | |||
| Pancreas | 35.67 ± 44.40 | 0.14 | 31.67 ± 8.622 | 0.24 | 67.33 ± 45.34 | 0.21 |
| No pancreas | 48.37 ± 67.44 | 29.91 ± 11.48 | 78.28 ± 67.99 | |||
| Kidneys | 47.91 ± 65.27 | 0.04 | 30.73 ± 10.81 | 0.06 | 78.65 ± 65.71 | 0.02 |
| No kidneys | 23.20 ± 29.48 | 26.60 ± 11.12 | 49.80 ± 29.09 |
DDNC = Declaration of Death by Neurologic Criteria.
Bold values indicate statistical significance at P < 0.05.
Discussion
To combat the growing list of patients waiting for transplants, there is a significant need to increase the number of potential donors and number of transplantable organs per donor. Early, aggressive management of potential donors has been shown to increase OTPD.18 Therefore, DMGs and CBIGs have been developed to guide the care of the potential organ donor. The optimal timeline to procurement, though, has yet to be well-defined. Somatic survival after brain death is relatively short, supporting the concept that procurement should occur quickly after declaration to prevent loss of donor potential.19 However, Lytle et al. showed that organ failure scores did not significantly progress during the intensive care unit course of organ donors, implying that prolonged periods of time to organ retrieval were not as detrimental.15
The purpose of our study was to more closely evaluate the time intervals related to DNC and organ procurement to define a relationship between time and organ donor potential to help guide the management of the potential organ donor. Our study demonstrated a significant relationship between the timing of DNC and the number of organs procured and transplanted. Patients who donated greater than four organs were declared earlier than patients, on average 17.81 hours earlier, than those who donated less than or equal to four organs.
The differences between the time periods and the two groups are better explained when looking at specific organs procured. Timing played a critical role for lung donation. More lungs were transplanted from donors who had shorter AtoD times; on average, a difference of 24.1 hours earlier. Further evaluation of the data reveals there was an uneven distribution of organs procured between the two groups. Hearts, kidneys, and livers were almost evenly distributed between the two groups (hearts 56% versus 43%; liver 43% versus 56%, and kidney 47% versus 52%). However, lungs and pancreases were overwhelmingly more likely to be transplanted from organ donors who donated >4 OTPD. Ninety-two percent of the patients who donated lungs donated >4 organs, whereas only 8.3% of patients who donated ≤4 had lungs procured.
Conversely, the earlier time advantage was not seen for hearts or kidneys. In fact, the opposite appeared true, with a prolonged AtoD time, donors were more likely to donate hearts and kidneys, on average 11.6 hours and 25 hours, respectively. These findings are consistent with studies demonstrating longer time periods resulted in improved organ function and increased the number of transplantable organs. Kunzendorf et al. found that kidney grafts from donors with a longer time to procurement had better graft survival than those with a shorter duration.13 In addition, a recent study demonstrated that a prolonged donor management after declaration of brain death using frequent transthoracic echocardiograms to monitor and optimize cardiac function resulted in transplantation of 53% of initially considered marginal donor hearts.16 The concept of organ optimization, in theory, can be adopted for any organ if the donor management efforts are directed toward optimization of that specific organ.
Why early declaration of DNC seemingly benefited lung procurement and not numbers of hearts or kidneys transplanted may reflect current critical care management and DMGs. Delaying procurement for resuscitation and critical care management of the donor may result in a higher organ yield. To combat the drop in systemic vascular resistance that occurs as a result of the autonomic storm in DNC, donors require aggressive resuscitation. To meet DMGs, interventions, including reduction of vasopressors and increased volume resuscitation to increase mean arterial pressures and UOP are required.2 In exchange for meeting DMGs targeted to improve systemic vascular resistance and UOP, pulmonary edema can result, leading to a decrease in transplantable lungs.11
Unlike AtoD time, DtoP time had minimal variation. This is likely a reflection of patient management being assumed by the OPO, Gift of Life, which aims to allocate and procure patients within an expedient, consistent time frame. In comparison to Lytle et al., our median time to declaration was much longer, 11.8 hours versus 45.4 hours.15 This may be a reflection of single-center data being compared to multi-center data. As each institution has its own declaration of DNC protocols, required waiting periods and staff availability, AtoD times can be dramatically affected. As we did not see significant differences between groups in the DtoP time period, we do not suspect organ allocation differences led to our findings.
A key limitation of this retrospective study is the inability to assess from the data, the cause for the time differences. Is the difference in times and numbers of organs transplanted attributable to a physiologic, systemic process that occurs at time of DNC or does current critical care management favor one organ system over another? Further research is required to determine if current resuscitation goals disproportionately affect certain organs and whether modifying goals to target-specific organ optimization could result in a higher yield of the less frequently donated organs. Another unanswered question by our data is whether the time differences are reflections of preventable delays, for example, systems issues, family requests, lack of training, or center variation in declaration protocols? Given the time-related relationship identified in this study, further efforts to create standardized declaration of DNC exams and CBIGs across the nation need to be undertaken. In addition, to keep a more homogeneous population, this study was only conducted on patients who died from catastrophic head injury. Further studies should be conducted to determine if the temporal trends defined in the traumatic brain injury population hold true in other medical and nontraumatic populations. The results of this study raise many questions pertinent to the management of potential organ donors. Further research should be targeted at identifying potential delays related to DNC and procurement to better understand what role time plays in organ donation and ultimately to determine whether time should be incorporated into CBIGs.
Conclusions
A shorter time interval between admission and declaration of DNC was associated with increased OTPD, especially lungs. However, more kidneys and hearts were transplanted when time to procurement was longer. Further research to identify what role timing plays in the management of the potential organ donor and how that relates to DMGs is needed.
Acknowledgments
Authors’ contributions: All authors participated in the conception and design of the study. S.R. and N.D.M. participated in the acquisition of data. S.R, N.D.M, and D.H. participated in the analysis of the data. All authors participated in the interpretation of the data results. S.R. and N.D.M were principally responsible for the drafting the article. All authors participated in critical revisions and made final approval of the version being submitted. All authors agree to be accountable for all aspects of the work.
Footnotes
Presented at 12th Annual Meeting of the Academic Surgical Congress, quickshot presentation, Las Vegas, NV, February 2017.
Disclosure
This work was supported by grant funding from The Transplant Foundation, a charitable foundation supporting the mission of the Gift of Life Donor Program.
References
- 1.Salim A, Martin M, Brown C, Rhee P, Demetriades D, Belzberg H. The effect of a protocol of aggressive donor management: implications for the national organ donor shortage. J Trauma. 2006;61:429–435. doi: 10.1097/01.ta.0000228968.63652.c1. [DOI] [PubMed] [Google Scholar]
- 2.Kotloff RM, Blosser S, Fulda GJ, et al. Management of the potential organ donor in the ICU. Crit Care Med. 2015;43:1291–1325. doi: 10.1097/CCM.0000000000000958. [DOI] [PubMed] [Google Scholar]
- 3.Westphal GA, Filho MC, Fiorelli A, et al. Guidelines for maintenance of adult patients with brain death and potential for multiple organ donations: the task force of the Brazilian association of intensive medicine the Brazilian association of organs transplantation, and the transplantation center of Santa Catarina. Transplant Proc. 2012;44:2260–2267. doi: 10.1016/j.transproceed.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 4.Shemie SD. Organ donor management in Canada: recommendations of the forum on medical management to optimize donor organ potential. Can Med Assoc J. 2006;174:S13–S30. doi: 10.1503/cmaj.045131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malinoski DJ, Daly MC, Patel MS, Oley-Graybill C, Foster CE, III, Salim A. Achieving donor management goals before deceased donor procurement is associated with more organs transplanted per donor. J Trauma. 2011;71:990–996. doi: 10.1097/TA.0b013e31822779e5. [DOI] [PubMed] [Google Scholar]
- 6.Patel MS, Zatarain J, La Cruz De S, et al. The impact of meeting donor management goals on the number of organs transplanted per expanded criteria donor: a prospective study from the UNOS Region 5 Donor Management Goals Workgroup. JAMA Surg. 2014;149:969–975. doi: 10.1001/jamasurg.2014.967. [DOI] [PubMed] [Google Scholar]
- 7.Bloom MB, Raza S, Bhakta A, et al. Impact of deceased organ donor demographics and critical care end points on liver transplantation and graft survival rates. J Am Coll Surg. 2015;220:38–47. doi: 10.1016/j.jamcollsurg.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 8.Franklin GA, Santos AP, Smith JW, Galbraith S, Harbrecht BG, Garrison RN. Optimization of donor management goals yields increased organ use. Am Surg. 2010;76:587–594. doi: 10.1177/000313481007600621. [DOI] [PubMed] [Google Scholar]
- 9.Malinoski DJ, Patel MS, Lush S, et al. Impact of compliance with the American College of Surgeons trauma center verification requirements on organ donation-related outcomes. J Am Coll Surg. 2012;215:186–192. doi: 10.1016/j.jamcollsurg.2012.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinn L, McTague W, Orlowski JP. Impact of catastrophic brain injury guidelines on donor management goals at a level I trauma center. Transplant Proc. 2012;44:2190–2192. doi: 10.1016/j.transproceed.2012.07.112. [DOI] [PubMed] [Google Scholar]
- 11.Smith M. Physiologic changes during brain stem death—lessons for management of the organ donor. J Heart Lung Transplant. 2004;23:S217–S222. doi: 10.1016/j.healun.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 12.Mackersie RC, Bronsther OL, Shackford SR. Organ procurement in patients with fatal head injuries. The fate of the potential donor. Ann Surg. 1991;213:143–150. doi: 10.1097/00000658-199102000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kunzendorf U, Hohenstein B, Oberbarnscheid M, et al. Duration of donor brain death and its influence on kidney graft function. Am J Transplant. 2002;2:292–294. doi: 10.1034/j.1600-6143.2002.20316.x. [DOI] [PubMed] [Google Scholar]
- 14.Avlonitis VS, Wigfield CH, Golledge HDR, Kirby JA, Dark JH. Early hemodynamic injury during donor brain death determines the severity of primary graft dysfunction after lung transplantation. Am J Transplant. 2007;7:83–90. doi: 10.1111/j.1600-6143.2006.01593.x. [DOI] [PubMed] [Google Scholar]
- 15.Lytle FT, Afessa B, Keegan MT. Progression of organ failure in patients approaching brain stem death. Am J Transplant. 2009;9:1446–1450. doi: 10.1111/j.1600-6143.2009.02575.x. [DOI] [PubMed] [Google Scholar]
- 16.Borbely XI, Krishnamoorthy V, Modi S, et al. Temporal changes in left ventricular systolic function and use of echocardiography in adult heart donors. Neurocrit Care. 2015;23:66–71. doi: 10.1007/s12028-014-0101-x. [DOI] [PubMed] [Google Scholar]
- 17.Malinoski DJ, Patel MS, Daly MC, Oley-Graybill C, Salim A UNOS Region 5 DMG Workgroup. The impact of meeting donor management goals on the number of organs transplanted per donor: results from the United Network for Organ Sharing Region 5 prospective donor management goals study. Crit Care Med. 2012;40:2773–2780. doi: 10.1097/CCM.0b013e31825b252a. [DOI] [PubMed] [Google Scholar]
- 18.DuBose J, Salim A. Aggressive organ donor management protocol. J Intensive Care Med. 2008;23:367–375. doi: 10.1177/0885066608324208. [DOI] [PubMed] [Google Scholar]
- 19.George S, Thomas M, Ibrahim WH, et al. Somatic survival and organ donation among brain-dead patients in the state of Qatar. BMC Neurol. 2016;16:207. doi: 10.1186/s12883-016-0719-8. [DOI] [PMC free article] [PubMed] [Google Scholar]