Abstract
Background
Sexual contact has been shown to be a major mode of HIV transmission among people who inject drugs (PWID). This study examined gender and racial differences among PWID' sexual risk behaviors from the perspective of sexual scripts.
Methods
696 PWID enrolled from Philadelphia on HPTN 037 were classified as engaging in high-risk sex behaviors if they reported having sex in the past 30 days and condomless sex with a non-primary partner, giving/receiving sex for money, or multiple partners. A multivariable logistic regression model was used to assess associations between demographic factors and high risk sex.
Results
Findings of the multivariable regression analysis demonstrated that being White (OR=0.52, p<0.001) and male (OR=0.59, p=0.002) were protective of high risk sex, while homelessness (OR=1.7, p=0.005), and being single (OR=1.83, p=0.006) were positively associated with high risk sex. African American (AA) women were 1.7 times more likely to report high-risk sex than AA men (p=0.002), 3.28 times more likely than White men (p<0.001), and 1.93 times more likely than White women (p<0.001).
Conclusions
Since AA women report high-risk sex behaviors more than other demographic groups, behavioral interventions for HIV risk reduction among PWID may benefit from focusing on sex-risk reduction among AA women.
Keywords: injection drug use, high risk sex, African American, gender, race
1.0 Introduction
Injection drug use (IDU) continues to be an important risk behavior in the HIV epidemic in the US (Spiller et al., 2015). New HIV cases transmitted by IDU have decreased significantly in the last decade. However, IDU continues to be a source of HIV transmission in the US ((CDC), 2012; CDC, 2014). In 2015, 6% (2,392) of HIV diagnoses in the US were attributed to IDU ((CDC), 2015a). Of those new HIV infections, 41% (980) of persons who inject drugs (PWID) were women and 23% (539) were African American (AA) ((CDC), 2015a).
Historically, HIV prevention interventions for injection drug-using populations have shown efficacy at decreasing injection risk behavior, sharing needles/syringes, sharing injecting paraphernalia, and to a lesser extent unprotected sex (Meader et al., 2013). Targeted strategies to decrease injection drug use risks and sexual risks among PWID have been successful among diverse groups; however, the literature is missing data on strategies tailored to subgroups within vulnerable populations. Although HIV prevention strategies have targeted sexual risk, they may have been underestimated sexual risk as an HIV transmission route for PWID. A behavioral analysis in 2012 among 9,425 PWID found that 30% engaged in receptive syringe sharing, 70% reported condomless vaginal sex, 25% of heterosexuals had engaged in condomless anal sex, and 5% reported condomless sex among male-to-male sexual contact (Spiller et al., 2015). These findings and other research findings suggest that sexual transmission may be an important source of HIV infections among PWID (Kral et al., 2001; Semaan et al., 2006; Strathdee et al., 2001).
Given the positive link between high risk sex and HIV transmission among PWID, specific factors that lead to high risk sex should be explored. Reports of a main sex partner has demonstrated a protective effect against HIV risks (Kral et al., 2001). Some research suggests that among women who inject drugs, IDU behaviors may be less influential in HIV seroconversion as compared to high risk sex behaviors (Strathdee et al., 2001). Given the influence of high risk sex on HIV transmission among women, a more in-depth understanding of factors that contribute to decisions to engage in high risk sex is warranted.
1.1 Theoretical Framework
The relevance of sexual/gender theoretical frameworks were substantiated through their use in public health research aimed at better understanding sexual risk behaviors in the context of HIV and related public health issues (Bowleg et al., 2015; Eaton and Stephens, 2016; Horley, 2016; Stephens, 2017). A theoretical framework built on both the Sexual Script Theory (SST) and the Theory of Gender and Power (TGP) highlights the influence of gender roles on sexual behaviors of women. Through presentation of gender as a social construct that organizes social relationships, this theoretical framework provides social context to sexual interactions between women and men (Farmer, 1996; Mantell et al., 2006; Schoepf, 1992). Research findings report that some men find it easy to initiate sexual activity (McLellan-Lemal et al., 2013) and express comfort with the role as the initiator when compared to women (Hickman, 1999; Vannier and O'Sullivan, 2011). Comparatively, women described an ideal sexual scenario as a situation whereby the male partner is the initiator (Bowleg, 2004; Morgan, 2007; Ortiz-Torres, 2003). Women have acknowledged maintenance of relationships with men who they perceive to engage in ‘high-risk’ sex behaviors (multiple partners, sex while under the influence of drugs/alcohol, sex with both men and women, concurrent partnerships) (Farmer, 1996; Mantell et al., 2006; Schoepf, 1992; Semaan et al., 2002). However, few researchers have evaluated the impact of gender roles on ‘high-risk’ sexual acts (Wagstaff et al., 1995). Both the SST and TGP help to explain how the relationship between gender and sexual risk has relevance for injection drug-using populations (Hill et al., 2016). In particular, SST describes the process whereby sexual experiences establishes ‘normal sex’ scripts.
1.2 Sexual Script Theory
Sexual scripts are influenced by complex emotions (Jones, 2006; Slovic, 1999). The SST focuses on the ways culture shapes perception and expression of appropriate and socially acceptable sexual behavior (Bowleg, 2004; Gagnon, 1973; Holman and Sillars, 2012; Jones, 2006; McLellan-Lemal et al., 2013). In regards to sexual risk, women have high risk of HIV acquisition from sexual encounters that involve a transaction of sex for drugs that do not include condom use, and/or occur with numerous partners concurrently or in succession (Booth et al., 2000). Women are at higher risk of HIV and other STI acquisition from unprotected sex, as well as pregnancy during heterosexual sexual intercourse ((Miller et al., 2004; Blythe et al., 2006). The traditional sexual script of condomless sex offers men more sexual autonomy, opportunities for sexual satisfaction, and well-being than it does women (Amaro, 2001; Masters et al., 2013). Scripts provide widely shared gender and culture-specific guides for sexual behaviors (Bowleg et al., 2015; Hill et al., 2017). They also offer a blueprint of predictable responses to sexual cues and dictate how men and women behave sexually (Hill et al., 2016; McLellan-Lemal et al., 2013; Roye et al., 2013;).
Stephens and Phillips (2005) led the focus of females' sexual script development research on AA women. Qualitative research has found that within sexual scripts among AA women, the power in the heterosexual relationship favors the man (McLellan-Lemal et al., 2013), supporting a dynamic where women may be vulnerable to the decisions made by her male partner (Hill, et al., 2017; Hill et al., 2016; Martyn and Hutchinson, 2001; McLellan-Lemal et al., 2013). This illustrates the intersectionality of the SST and TGP. Like the SST, the TGP is a sound theory to help clinicians and interventionists better understand sexual risk behaviors in the context of HIV for an exceptionally vulnerable population, AA women who inject drugs.
1.3 Theory of Gender and Power
The TGP compliments the SST in addressing vulnerability of the woman to the man. Culture and societal norms reinforce value systems giving decision power to men, including sexual decisions. As a result, risk reduction practices that could be effectively led by women are impeded (Jones, 2006; Slovic, 1999). In circumstances where a conflict occurs between a woman's relationship health and her own sexual health, the sexual script provides a roadmap to the sexual decision. When the decision is led by traditional sexual scripts wherein the decision making power belongs to the man, the decision made may introduce HIV risks. TGP discusses the influence of gender-based inequalities at the societal level where men are supported in controlling sexual decision making (Pulerwitz, 2006; Pulerwitz et al., 2002). Societal support moves beyond sexual decision making and permeates the type and frequency of sex (Dixon-Mueller, 1993). It also influences relationship dynamics, permeating the way people manage conflict, power, communication (Bowleg, 2004) and norms by better understanding gender-based inequalities in society. Gina Wingood applied TGP to powerlessness of AA women in sexual decision making (Wingood and DiClemente, 1992, 1998, 2000; Wingood et al., 2003; Wingood et al., 2000). She found that encouraging men to use a condom raised concern of perceived infidelity by the women. TGP offers an explanation of the influential power of gender on sexual risk.
1.4 Link between Theories and High Risk Sex Behaviors
Few research agendas have explored demographic correlates of high risk sex behavior with a hypothesis that stems from a theoretical framework comprised of the SST and TGP (Hill and Andrews, 2017; Hill et al., 2017; Hill et al., 2016). In a study where 44 heterosexually active men and women aged 18-25 years were interviewed, men preferred recreational sex, valued sex over relationships, and sought out multiple sex partners, while women preferred sex in the context of commitment and monogamy and sought emotional intimacy and trust with sex (Masters et al., 2013). Justification of multiple partners among women entailed conforming to traditional gender roles of being desired, but not desiring sex. The sexual script of women enrolled in a study of 30 substance-using, AA women ages 18-25 years involved use of sex as a partner pleasing tool to elicit a stronger emotional response (i.e., like, love) from the male partner and to fulfill what they perceived as their obligation in the relationship (Hill and Andrews, 2017; Hill et al., 2017). In addition, sexual scripts here condomless sex is normative were associated with a defined phase within a long-term relationship where women deemed their partner trustworthy (Hill and Andrews, 2017).
In a British study, 3,395 men and 4,980 women ages 16-44 years were sexually-active substance users (Paquette et al., 2017). Men and women reported 5 or more partners (AOR= 5.03 and 4.15 respectively), men and women reported 2 or more sexual partners without a condom (AOR=5.50 and 5.24), and men who traded money for sex in the past year (AOR=2.47) were more likely to report recent illicit drug use when compared to referent others based on sociodemographic, health related factors, and sexual behaviors. Study findings of US and British studies collectively illustrate a correlation between high risk sexual behaviors and illicit drug use that appears to be moderated by gender; thus, this illustration warrants the need to examine established relationships among PWID through relevant theoretical frameworks.
The SST and TGP provide a theoretical framework to examine associations between gender, race, and HIV risks driven by high risk sex behaviors. Although the HIV Prevention Trials Network (HPTN) 037 study was not developed with a SST and TGP as its theoretical framework, application of these theories to correlations between gender, race, and sexual risk informs our research question assessing whether there is an association between gender and/or race and ‘high risk’ sexual behaviors among an injection drug-using population. We hypothesized that due to power differences and racial differences in sexual scripts, there would be more high-risk sexual behavior, including condomless sex, among AA women compared to Whites and men.
2.0 Methods
This is a secondary analysis of HPTN 037, a phase III randomized study to evaluate the efficacy of a network-oriented peer educator intervention for the prevention of HIV transmission among injection drug users and their network members at two study sites in Philadelphia and Thailand. HPTN 037 screened 1249 potential participants in Philadelphia, and enrolled 232 index members and 464 network members (Total N=696) (Latkin et al., 2009). This secondary analyses of 696 participants enrolled in Philadelphia only focused on a subset of the HPTN 037′ variables, specifically self-reported data on sexual risk variables (n=649).
HPTN 037 involved training participants to diffuse behavior change to their network members. Further details on the methods used for the HPTN 037 study are provided in earlier publications (59, 60). Variables chosen to address the research question of this secondary analysis are described in the ‘measures’ section below. Specific variables related to sexual risk were evaluated at baseline for all individuals enrolled.
2.1 Measures
Participants were classified into sex risk categories (high and low) using self-reported responses provided during the baseline enrollment visit. A detailed account of high risk behaviors assessed, the specified HPTN 037′ survey question, and the response format is provided (Figure 1). The main outcome variable for this secondary analysis had four parts, one primary and three secondary. The primary factor was a report of vaginal or anal sexual activity in the last month. Individuals who reported this primary factor without any reports of the three high risk sexual behaviors were stratified to the ‘low risk for HIV’ group. Conversely, individuals who reported at least one of three high risk sexual behaviors, in addition to a report of sexual activity, were stratified to the ‘high risk for HIV’ group. The three high risk sexual behaviors were condomless sex with their non-primary partner (DePadilla et al., 2011), transactional sex (giving or receiving goods for sex) (Doherty et al., 2000; Dunkle et al., 2010), and multiple sex partners (Strathdee et al., 2001; Amaro et al., 2001). The response format for the primary factor was yes/no and were continuous numerical values for the three high risk sex behaviors. A secondary assessment to quantify high risk sex related to condomless sex was measured based on a weekly account of sexual encounters with primary and/or casual sex partners. Transactional sex was measured and quantified in both directions to account for giving and/or receiving money or drugs in exchange for sex. Lastly, multiple sex partners were measured using numerical values accounting for the number of different male and/or female partners in the last month.
Figure 1. Detailed description of outcome variables in the HPTN 037′ secondary analysis Figure 1.
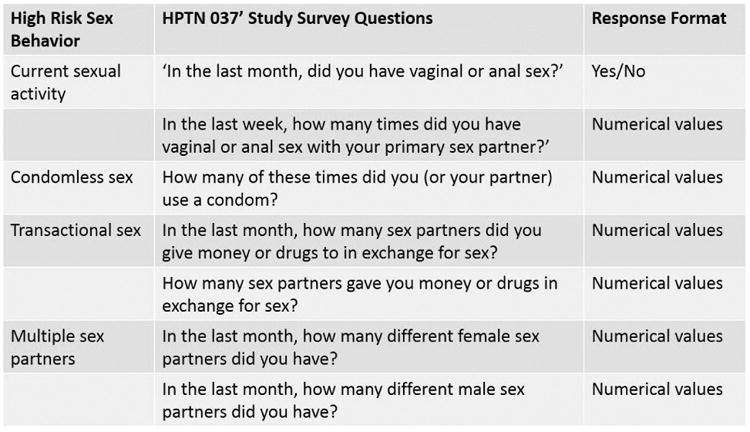
* Responses of <1 were included.
The study assessed demographics including age, race, and gender. Participants' recent history of jail time in the last 6 months prior to enrollment was assessed. Participants were classified as having been ‘recently homeless’ if they reported living on the street, in a car, or in an abandoned building in the six months previous to enrollment. Participants were classified as married if they reported being married or reported currently living with a partner.
2.2 Data Analysis
We assessed bivariate associations between sociodemographic characteristics of participants and both race and gender. In a subgroup analysis, we also assessed associations between sociodemographic characteristics and race among only female participants. All bivariate analyses were conducted using frequencies and Fisher's exact tests.
We used a multivariable logistic regression model to examine the associations between both race and gender and reporting high risk sex. We used a stepwise approach to select covariates for inclusion into the model. Initial potential confounders assessed for inclusion included age, race, gender, jail time, homelessness, marital status, and education. To explore the possibility of interaction effects between race and gender on the reporting of high risk sex, an interaction term between race and gender was also included as a covariate to be assessed for inclusion in the initial full model. The final reduced model was selected in terms of minimum AIC by stepwise procedure. Linear combinations of the coefficients in the final adjusted model were used to compare race and gender subgroups. Models were run in R version 3.3.2.
3.0 Results
The demographic assessment of the study population revealed differences by gender and race. Men tended to be older than women (41 versus 39 years old) (Table 1). A significant number of men were 50 and older (24.2%) while few women were in this age group (11.5%). Half of the men were AA (50.1%), while only 41.9% of the women were AA. Homelessness was noted among 27.8% of men and 17.5% of women. The majority of study participants were single (61.5%), reported some secondary education or more (98.2%), were unemployed (81%), and did not report prior arrests (82.9%).
Table I. Demographics Count and Percent by Gender and Race, N (%).
| Gender | Race | |||||
|---|---|---|---|---|---|---|
| Female (n = 217) | Male (n = 479) | White (n = 318) | AA (n = 331) | Other (n = 47) | Total (n = 696) | |
| Age | ||||||
| Mean (SD) | 38.97 (8.68) | 41.25 (10.3) | 36.51 (10.02) | 45.1 (7.85) | 35.68 (7.27) | 40.54 (9.87) |
| P-Value | 0.003 | < .001 | 0.49 | |||
| Age Categories | ||||||
| 18 - 29 | 35 (16.1) | 78 (16.3) | 98 (30.8) | 6 (1.8) | 9 (19.1) | 113 (16.2) |
| 30 - 39 | 77 (35.5) | 123 (25.7) | 94 (29.6) | 83 (25.1) | 23 (48.9) | 200 (28.7) |
| 40 - 49 | 80 (36.9) | 162 (33.8) | 92 (28.9) | 136 (41.1) | 14 (29.8) | 242 (34.8) |
| 50+ | 25 (11.5) | 116 (24.2) | 34 (10.7) | 106 (32) | 1 (2.1) | 141 (20.3) |
| Gender | ||||||
| Female | 217 (100) | 0 (0) | 111 (34.9) | 91 (27.5) | 15 (31.9) | 217 (31.2) |
| Male | 0 (0) | 479 (100) | 207 (65.1) | 240 (72.5) | 32 (68.1) | 479 (68.8) |
| Race/Ethnicity | ||||||
| White | 111 (51.2) | 207 (43.2) | 318 (100) | 0 (0) | 0 (0) | 318 (45.7) |
| African American | 91 (41.9) | 240 (50.1) | 0 (0) | 331 (100) | 0 (0) | 331 (47.6) |
| Other | 15 (6.9) | 32 (6.7) | 0 (0) | 0 (0) | 47 (100) | 47 (6.8) |
| Marital Status | ||||||
| single | 114 (52.5) | 314 (65.6) | 194 (61) | 204 (61.6) | 30 (63.8) | 428 (61.5) |
| married | 27 (12.4) | 43 (9) | 28 (8.8) | 39 (11.8) | 3 (6.4) | 70 (10.1) |
| living with partner/not married | 26 (12) | 31 (6.5) | 20 (6) | 28 (8.5) | 9 (19.1) | 57 (8.2) |
| separated/married but separate | 21 (9.7) | 36 (7.5) | 26 (8.2) | 30 (9.1) | 1 (2.1) | 57 (8.2) |
| divorced | 20 (9.2) | 40 (8.4) | 35 (11) | 22 (6.6) | 3 (6.4) | 60 (8.6) |
| widowed | 9 (4.1) | 15 (3.1) | 15 (4.7) | 8 (2.4) | 1 (2.1) | 24 (3.4) |
| Education | ||||||
| no schooling | 1 (0.5) | 0 (0) | 1 (0.3) | 0 (0) | 0 (0) | 1 (0.1) |
| primary | 4 (1.8) | 8 (1.7) | 4 (1.3) | 7 (2.1) | 1 (2.1) | 12 (1.7) |
| some secondary | 81 (37.3) | 141 (29.4) | 104 (32.7) | 99 (29.9) | 19 (40.4) | 222 (31.9) |
| completed secondary | 83 (38.2) | 231 (48.2) | 139 (43.7) | 155 (46.8) | 20 (42.6) | 314 (45.1) |
| vocational | 4 (1.8) | 10 (2.1) | 7 (2.2) | 7 (2.1) | 0 (0) | 14 (2) |
| some university | 35 (16.1) | 70 (14.6) | 47 (14.8) | 53 (16) | 5 (10.6) | 105 (15.1) |
| completed university | 8 (3.7) | 18 (3.8) | 14 (4.4) | 10 (3) | 2 (4.3) | 26 (3.7) |
| graduate school | 1 (0.5) | 1 (0.2) | 2 (0.6) | 0 (0) | 0 (0) | 2 (0.3) |
| Employment | ||||||
| full time | 12 (5.5) | 48 (10) | 28 (8.8) | 30 (9.1) | 2 (4.3) | 60 (8.6) |
| part time | 7 (3.2) | 29 (6.1) | 14 (4.4) | 20 (6) | 2 (4.3) | 36 (5.2) |
| occasional | 3 (1.4) | 33 (6.9) | 15 (4.7) | 17 (5.1) | 4 (8.5) | 3 6 (5.2) |
| Unemployed* | 195 (89.9) | 369 (77) | 261 (82.1) | 264 (79.8) | 39 (83) | 564 (81) |
| Social Challenges | ||||||
| Arrested/ had trouble with legal system* | 39 (18) | 80 (16.7) | 74 (23.3) | 38 (11.5) | 7 (14.9) | 119 (17.1) |
| Trouble getting or keeping housing* | 38 (17.5) | 133 (27.8) | 95 (29.9) | 62 (18.7) | 14 (29.8) | 171 (24.6) |
Legend:
-only represents individuals who responded yes to survey questions. Respondents who responded ‘no’ are excluded from this table.
High risk sex behaviors were significantly more common among women (50.5%) than among men (40%) (p=0.01) (Table 2). The reports of sexual risk behaviors are non-significantly different between African Americans and Whites (46.8% vs 39.6%, p=0.07).
Table II. Count and Percent Summary of Risk Related to Sexual Behaviors by Gender and Race, N (%).
| Gender | Race | ||||||
|---|---|---|---|---|---|---|---|
| Female (n = 202) | Male (n = 447) | -Value | White (n = 318) | African American (n = 331) | -Value | Total (n = 649) | |
| Risk Type | |||||||
| Sex Risk | |||||||
| Low | 100 (49.5) | 268 (60) | .01 | 192 (60.4) | 176 (53.2) | .07 | 368 (56.7) |
| High | 102 (50.5) | 179 (40) | 126 (39.6) | 155 (46.8) | 281 (43.3) | ||
| Individual Behaviors | |||||||
| Multiple male partners | 96 (47.5) | 9 (2) | .001 | 51 (16) | 54 (16.3) | 105 (16.2) | |
| Multiple female partners | 13 (6.4) | 158 (35.3) | .001 | 68 (21.4) | 103 (31.1) | .006 | 171 (26.3) |
| Received goods for sex | 75 (37.1) | 41 (9.2) | .001 | 47 (14.8) | 69 (20.8) | .05 | 116 (17.9) |
| Gave goods for sex | 8 (4) | 96 (21.5) | .001 | 32 (10.1) | 72 (21.8) | .001 | 104 (16) |
| Condomless sex with non-primary partner | 44 (21.8) | 67 (15) | .04 | 053 (16.7) | 58 (17.5) | .83 | 111 (17.1) |
In addition to demographic differences, there were differences in high risk sex behaviors by gender and race. Women reported multiple male partners, receiving goods for sex, and condomless sex with a non-primary partner more frequently than men; whereas, men reported multiple female partners and giving goods for sex more frequently than women (p≤0.001, Table 2). African Americans reported multiple female partners, receiving goods for sex, and giving goods for sex more frequently than Whites (p≤0.001, Table 2). A sub-analysis of high risk sex behaviors among women demonstrated a statistically nonsignificant racial difference of 12.1% (p=0.09, 95% CI: 0.9%-25.2%). Self –reported high risk behaviors among AA women was higher (57.1%) than White women (45%) (Table 3).
Table III. Count and Percent Summary of Risk Related to Sexual Behaviors by Race for Women and Men, N (%).
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| White (n = 111) | African American (n = 91) | -Value | Total (n = 202) | White (n = 207) | African American (n = 240) | -Value | Total (n = 447) | |
| Risk Type | ||||||||
| Sex Risk | ||||||||
| Low | 61 (55) | 39 (42.9) | .09 | 100 (49.5) | 131 (63.3) | 137 (57.1) | .21 | 268 (60) |
| High | 50 (45) | 52 (57.1) | 102 (50.5) | 76 (36.7) | 103 (42.9) | 179 (40) | ||
| Individual Behaviors | ||||||||
| Multiple male partners | 47 (42.3) | 49 (53.8) | .12 | 096 (47.5) | 4 (1.9) | 5 (2.1) | 91 (2) | |
| Multiple female partners | 6 (5.4) | 7 (7.7) | .57 | 13 (6.4) | 62 (30) | 96 (40) | .03 | 158 (35.3) |
| Received goods for sex | 33 (29.7) | 42 (46.2) | .02 | 75 (37.1) | 14 (6.8) | 27 (11.2) | .14 | 41 (9.2) |
| Gave goods for sex | 1 (0.9) | 7 (7.7) | .02 | 8 (4) | 31 (15) | 65 (27.1) | .002 | 96 (21.5) |
| Condomless sex with non-primary partner | 26 (23.4) | 18 (19.8) | .61 | 044 (21.8) | 27 (13) | 40 (16.7) | .29 | 67 (15) |
The stepwise modeling process resulted in a final adjusted model including age, race, gender, marital status, and homelessness. There was no significant interaction between race and gender (Table 4). However, the adjusted model suggests that being younger, single, homeless, and female are all significantly associated with more self-reporting of high risk behaviors. In particular, women have 1.7 (p=0.002) times the odds of self-reported high risk behaviors as compared to men. AA women have 3.28 (p<0.001) and 1.93 (p<0.001) times the odds of self-reported high risk behavior than White men and White women, (Tables 5) respectively.
Table IV. Multivariate Logistic Regression Results Showing the Adjusted Association Between Demographic Factors and High-Risk Sex Behaviors.
| Confounder in Stepwise Selected Model | Odds Ratio (95% CI) | P-Value |
|---|---|---|
| (Intercept) | 0.66 (0.29, 1.50) | 0.327 |
| Age* | 0.78 (0.65, 0.93) | 0.007 |
| Race: African American | 1.93 (1.34, 2.77) | < 0.001 |
| Race: Other | 2.27 (1.20, 4.29) | 0.012 |
| Race: White | 1 | (n/a) |
| Gender: Female | 1.70 (1.21, 2.39) | 0.002 |
| Homeless: Yes | 1.70 (1.18, 2.45) | 0.005 |
| Marital Status: Single | 1.83 (1.19, 2.80) | 0.006 |
| Race/Gender Subgroup Comparisons | ||
| African American women vs White men | 3.28 (1.96, 5.51) | < 0.001 |
| White women vs African American men | 0.88 (0.55, 1.42) | 0.607 |
Legend:
Odds ratio for 10-year differences in age.
Note: this table includes the final adjusted model selected by the stepwise procedure.
Table V. Adjusted Odds Ratios Comparing the Likelihood of High-Risk Sex Behaviors by Race and Gender Subgroups.
| Contrast | Odds Ratio (95% CI) | P-Value |
|---|---|---|
| African American women vs African American men | 1.70 (1.21, 2.39) | 0.002 |
| African American women vs White men | 3.28 (1.96, 5.51) | < 0.001 |
| African American women vs White women | 1.93 (1.34, 2.77) | < 0.001 |
| White women vs African American men | 0.88 (0.55, 1.42) | 0.607 |
| White women vs White men | 1.70 (1.21, 2.39) | 0.002 |
4.0 Discussion
The study contributes to our understanding of demographic differences in high risk sexual behaviors among PWID, which perhaps has important implications for HIV prevention efforts. The prevalence of high risk sex behaviors was much higher among women than men. In addition, the study found that AA women were more likely to self-report high risk sex behavior than White men and women. These results reflect recent CDC findings depicting trends in HIV diagnoses between 2005 and 2014 (CDC, 2016). Even though HIV rates are declining overall, the disproportionate burden of new HIV diagnoses to AA women compared to other women remain alarming. Findings of this analysis have potential to validate gender differences in risk factors for HIV seroconversion among injection drug users discerned nearly twenty years ago (Strathdee et al., 2001).
4.1 Gender, Race, and Transactional Sex Among PWID
Among PWID that reported transactional sex, women more often received goods and men gave goods in exchange for sex. When assessed by race, we found that AA women engaged in transactional sex significantly more than White women. These findings may be rooted in perceptions of and experiences with gender-based power imbalances coupled with immediate economic and social circumstances, as perceived and experienced by AA women in previous research (Adimora et al., 2006a; Adimora et al., 2001; Hill and Andrews, 2017; Hill et al., 2017). Sexual scripts for AA women may be reinforced by a combination of distal causes (legacy of slavery, exploitation, etc.) and proximal causes related to contemporary gender norms [powerlessness, meekness (DePadilla et al., 2011; Roye et al., 2013; Sanchez et al., 2012)]. The legacy of slavery manifests differently among AA men and women; whereby, AA men are subject to the school-to-prison pipeline (Kim, 2010) and are subsequently less available to AA women due to incarceration. Conversely, studies of sexuality among AA women found that the legacy of slavery influences sexual scripts where women are manipulated, exploited, and controlled by dominant others (Bowleg, 2004; Hussen et al., 2012; Whitehead, 1997). In some instances, power dynamics of master/slave girl are adopted as norms of AA husband/wife (Robinson et al., 2002; Stephens, 2005). Today, the intersection of the distal (legacy of slavery) and proximal (societal gender norms) causes manifest as socioeconomic disparities that influence racial health disparities) that include HIV ((CDC, 2016; Bowleg, 2004; Hussen et al., 2012; Whitehead, 1997). Stephens and Phillips suggested that this intersection challenges the development of healthy sexual scripts among AA women (Stephens, 2007). This perspective is supported by research findings among substance-using AA women where associations between transactional sex and emotional wounds stemming from a history of abuse, rape, abandonment, and/or feelings of low self-worth were demonstrated (Hill et al., 2017; Hill and Andrews, 2017). Concerted efforts to overcome barriers to adoption of healthy sexual scripts are warranted.
Future interventions that are tailored to AA women would benefit from adaptations that include strategies aimed at challenging unhealthy sexual scripts. Interventional adaptations are needed to encourage women to behave in ways that are in direct conflict with scripts by which they have grown accustomed (Mallory and Stern, 2000; Semaan et al., 2010), such as engaging in transactional sex and multiple sex partners, are imperative to reducing HIV risk (Hill et al., 2016).
4.2 Race and Multiple Sex Partners among PWID
Comprehensive HIV prevention strategies would benefit from addressing HIV risk associated with multiple sex partners as a direct complement to risks related to transactional sex. The indirect HIV risk to AA women as result of AA men in this study sample of PWID is worth mentioning. Based on data extrapolated from Tables 2 and 3, AA men reported multiple female sex partners more than their White counterparts. This finding supports a previous study where 22% of 671 predominantly single, young AA women living in low-income housing developments had an exclusive partner who either had other sexual partners in the past year or had a history of injection drug use (Wagstaff et al., 1995). In one study that enrolled 30 AA women who reported substance use and high risk sex behaviors, AA women in monogamous relationships acknowledged that they are committed to men who they know or suspect routinely have sex with other partners (Hill et al., 2017). This particular direction of HIV risk from the AA man to the AA woman is seemingly supported within the AA culture whereby relationship maintenance appears to be prioritized above the expectation of men to be monogamous (Adimora et al., 2006b; Hotton et al., 2015; Lane et al., 2004). Although AA women do not report multiple male partners significantly more than White women in this sample, their HIV risk remains high. The rationale for the disproportionate burden of risk is because sexual networks of AA women are usually racially homogenous and have a much higher prevalence of HIV when compared to White counterparts (Adimora and Schoenbach, 2002; Adimora et al., 2002; Adimora et al., 2006a). As a result, AA women are likely participant to ‘pass through’ risk of their male sex partners. Thus, an individual who is low risk, but is in a monogamous relationship with a high-risk partner who has other partners, becomes high risk (Hill et al., 2016; Wagstaff et al., 1995).
4.3 Race and Condomless Sex among PWID
An important HIV risk to transactional sex and multiple sex partners is condomless sex with any sexual partner. Condomless sex is an established primary route of HIV transmission among AA women in the US, as two out of three AA women contracted HIV from condomless sex with a man ((CDC), 2015b). Condomless sex as a behavior may be an indication of intimacy and is associated with sex with a main partner (Marshall et al., 2016). It is also associated with tolerance of infidelity as a cultural norm (Santo, 2015). These factors work together to increase HIV risk for this vulnerable population. AA women who tolerate infidelity as a part of sexual relationships with male partners may, in part, underestimate the severity of HIV risk that stem from their male partner's sexual behaviors (Jones, 2006; King, 2004; Montgomery et al., 2003). AA women who partner with AA men who have sex with both men and women are linked to sexual networks that include AA MSM, the subgroup at highest risk for HIV in the US (CDC, 2016). Within some AA communities there is also a social norm where women are encouraged to ignore behaviors of their partners and focus on benefits of the relationship (i.e., stability, finances, and family) (Gardner, 2016). The risk of losing a male partner for refusing to engage in condomless sex may be perceived as more imminent than the ‘real’ risk of contracting HIV. This value system illustrates cultural and social influences on sexual decision making that cause AA women, who have a double minority status based on race and gender, to be at especially high risk for HIV through behaviors that align with high risk sexual scripts and gender-power imbalances.
4.4 Limitations
The study population for HPTN 037 was selected with the goal to recruit high risk individuals. A study limitation is that results from this convenience sample may not generalize to high risk drug users more broadly, regardless of treatment. However, most drug users are not in treatment and this is a sample of difficult to recruit individuals. There is also the limitation of self-reports.
4.5 Future Research
Future research efforts would benefit from intervention strategies designed to re-write sexual scripts in a way to encourage willingness of women to negotiate and communicate the desire to adopt a comprehensive HIV prevention strategy, including PrEP and consistent condom use among minority women (Hill et al., 2016; Wingood and DiClemente, 1998). A qualitative research study utilizing both focus groups and individual in-depth interviews were facilitated among low-income AA young women (Martyn and Hutchinson, 2001). The women who were recipients of negative social-psychological scripts were engaged in an exercise to rewrite these scripts through recognition of negativity, aims to be different, and to create better lives for themselves. Through use of grounded theory methods, the women disclosed beliefs in self-responsibility, self-protection, education, and financial independence. Health promotion strategies and recommendations from this study support the theory of rewriting negative scripts (Martyn and Hutchinson, 2001). Identifying strategies to rewrite sexual scripts is a key step toward interrupting patterns that support ‘high risk’ sex behaviors (McLellan-Lemal et al., 2013).
Efforts to reduce ‘high-risk’ sex behaviors among women should include four phases: 1) recognizing negative scripts, 2), being disappointed with negative scripts, 3) determining to be different, and 4) creating a different life (Berne, 1964; Martyn and Hutchinson, 2001). These phases do not require chronology, but instead can occur simultaneously. Studies addressing the development of sexual scripts of women are limited (Stephens, 2005). Strategies to re-write sexual scripts must involve relating new scripts with more familiar scripts (i.e., default scripts) (Stacy et al., 2000). Although it has not been assessed yet, qualitative researchers suggest that relating high-power scripts, which are scripts of women who perceived themselves as ‘strong-minded’, ‘steadfast in their decisions’, and ‘solid with sticking to what [they wanted]’, with healthy relationship dynamics and health-promoting behaviors coalesced with normative sex scripts is a strategy at-risk women may readily embrace (Jones, 2006; Martyn and Hutchinson, 2001).
5.0 Conclusion
The findings of this secondary analysis support the need to address gender and race related factors through HIV prevention efforts. Tailoring interventions with an aim to reduce high risk sex behaviors among PWID, based on gender and race, is a needed HIV prevention strategy. More specifically, targeting AA women who report high risk sex behaviors for HIV prevention is an essential strategy to minimize the disparity in new HIV diagnoses among women in the US (Crepaz et al., 2009).
Addressing AA women through HIV intervention requires sensitivity to AA culture and content relevance (Crepaz et al., 2009; Hill et al., 2016). Adapting evidence based interventions with proven effectiveness at reducing HIV risks among populations at risk for HIV with an added culturally relevant theoretical framework to address gender and race, based on the TGP and SST, will lead to sustainable changes in sexual behavioral patterns among populations at risk for HIV, particularly AA women (Hill et al., 2016; Latkin et al., 2013).
Highlights.
There were differences in high risk sex behaviors by gender and race.
High risk sex with a casual partner was more common among women than men.
African American women had more risky sex than other women who inject drugs.
Acknowledgments
Role of Funding Source: This research was supported by funding from the National Institute of Allergy and Infectious Diseases to the HIV Prevention Trials Network (PIs: Drs. Darrell Wheeler and Steve Vermund) with a supplement to Mandy J. Hill as an HPTN Scholar (UM1AI068619).
Footnotes
Author Disclosures: Contributors: Dr. Mandy Hill developed the research question and led the writing of the manuscript. Michael Holt and Zhe Wang executed the analytic plan and results section and made tables. Dr. Brett Hanscom oversaw and guided the analytic plan, and provide revisions for the text. Dr. Marylou Cardenas-Turanzas supported the data analysis and contributed to the writing of the manuscript and editing of the tables. Dr. Carl Latkin mentored Dr. Hill in the development of the research question, guided the analysis, and provided revisions to the manuscript. All authors have approved the final article.
Conflict of Interest: No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adimora AA, Schoenbach VJ. Contextual factors and the black-white disparity in heterosexual HIV transmission. Epidemiology. 2002;13:707–712. doi: 10.1097/00001648-200211000-00016. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Schoenbach VJ, Bonas DM, Martinson FE, Donaldson KH, Stancil TR. Concurrent sexual partnerships among women in the United States. Epidemiology. 2002;13:320–327. doi: 10.1097/00001648-200205000-00013. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Schoenbach VJ, Doherty IA. HIV and African Americans in the southern United States: Sexual networks and social context. Sex Transm Dis. 2006a;33:S39–45. doi: 10.1097/01.olq.0000228298.07826.68. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Schoenbach VJ, Martinson FE, Coyne-Beasley T, Doherty I, Stancil TR, Fullilove RE. Heterosexually transmitted HIV infection among African Americans in North Carolina. J Acquir Immune Defic Syndr. 2006b;41:616–623. doi: 10.1097/01.qai.0000191382.62070.a5. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Schoenbach VJ, Martinson FE, Donaldson KH, Fullilove RE, Aral SO. Social context of sexual relationships among rural African Americans. Sex Transm Dis. 2001;28:69–76. doi: 10.1097/00007435-200102000-00002. [DOI] [PubMed] [Google Scholar]
- Amaro H, Raj A, Reed E. Women's Sexual health: The need for feminist analyses in public health in the decade of behavior. Psychol Women Q. 2001;25:324–334. [Google Scholar]
- Berne E. Games people play: The psychology of human relationships. Grove; New York: 1964. [Google Scholar]
- Blythe MJ, Fortenberry JD, Temkit M, Tu W, Orr DP. Incidence and correlates of unwanted sex in relationships of middle and late adolescent women. Arch Pediatr Adolesc Med. 2006;160:591–595. doi: 10.1001/archpedi.160.6.591. [DOI] [PubMed] [Google Scholar]
- Booth RE, Kwiatkowski CF, Chitwood DD. Sex related HIV risk behaviors: Differential risks among injection drug users, crack smokers, and injection drug users who smoke crack. Drug Alcohol Depend. 2000;58:219–226. doi: 10.1016/s0376-8716(99)00094-0. [DOI] [PubMed] [Google Scholar]
- Bowleg L, Burkholder GJ, Noar SM, Teti M, Malebranche DJ, Tschann JM. Sexual scripts and sexual risk behaviors among Black heterosexual men: Development of the Sexual Scripts Scale. Arch Sex Behav. 2015;44:639–654. doi: 10.1007/s10508-013-0193-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, Lucas KJ, Tschann JM. “The ball was always in his court”: An exploratory analysis of relationship scripts, sexual scripts, and condom use among african american women. Psychol Women Q. 2004;28:70–82. [Google Scholar]
- Center for Disease Control and Prevention (CDC) HIV Surveillance Supplemental Report. Atlanta, GA: 2012. Estimated HIV incidence among adults and adolescents in the United States, 2007-2010. [Google Scholar]
- Center for Disease Control and Prevention (CDC) Diagnoses of HIV infection in the United States and dependent areas, 2015. [Accessed January 3 2017];2015a https://www.cdc.gov/hiv/statistics/overview/ataglance.html.
- Center for Disease Control and Prevention (CDC) HIV and African American women. [Accessed June 9 2017];2015b https://www.cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/hivwomen.html.
- Crepaz N, Marshall KJ, Aupont LW, Jacobs ED, Mizuno Y, Kay LS, Jones P, McCree DH, O'Leary A. The efficacy of HIV/STI behavioral interventions for African American females in the United States: A meta-analysis. Am J Public Health. 2009;99:2069–2078. doi: 10.2105/AJPH.2008.139519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePadilla L, Windle M, Wingood G, Cooper H, DiClemente R. Condom use among young women: Modeling the theory of gender and power. Health Psychol. 2011;30:310–319. doi: 10.1037/a0022871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon-Mueller R. The sexuality connection in reproductive health. Stud Fam Plann. 1993;24:269–282. [PubMed] [Google Scholar]
- Doherty MC, Garfein RS, Monterroso E, Brown D, Vlahov D. Correlates of HIV infection among young adult short-term injection drug users. AIDS. 2000;14:717–726. doi: 10.1097/00002030-200004140-00011. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Wingood GM, Camp CM, DiClemente RJ. Economically motivated relationships and transactional sex among unmarried African American and white women: Results from a U.S. national telephone survey. Public Health Rep. 2010;125:90–100. doi: 10.1177/00333549101250S413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton AA, Stephens DP. Using the theory of planned behavior to examine beliefs about verbal sexual coercion among urban black adolescents. J Interpers Violence. 2016 doi: 10.1177/0886260516659653. [DOI] [PubMed] [Google Scholar]
- Farmer P, Connors M, Simmons J. Women, poverty, and AIDS: Sex, drugs, and structural violence. Common Courage Press; Monroe: 1996. [Google Scholar]
- Gagnon JH, Simon W. Sexual conduct: The social sources of human sexuality. Aldine; Chicago, IL: 1973. [Google Scholar]
- Gardner AJ. Exploring risky sexual behaviors of southern African American men and their readiness for barbershop-based HIV prevention programs. The University of Alabama; 2016. [Google Scholar]
- Hickman SE, Muehlenhard CL. “By the semi-mystical appearance of a condom”: How young women and men communicate sexual consent in heterosexual situations. J Sex Res. 1999;35:258–272. [Google Scholar]
- Hill M, Andrews S. Evolution of the DECISION: Pilot study findings reveal a logic model to sexual decision making. J Gen Emerg Med. 2017;3:1–15. [Google Scholar]
- Hill M, Granado M, Stotts A. Theoretical implications of gender, power, and sexual scripts for HIV prevention programs aimed at young, substance-using African American women. J Racial Ethn Health Disparities. 2016;4:1175–80. doi: 10.1007/s40615-016-0323-z. [DOI] [PubMed] [Google Scholar]
- Hill M, Granado M, Villarreal Y, Fuega J, Robinson D, Stotts A. Predictors of sexual scripts among young, sexually-active, substance-using African American women. J AIDS Clin Res. 2017;8:655. [Google Scholar]
- Holman A, Sillars A. Talk about “hooking up”: The influence of college student social networks on nonrelationship sex. Health Commun. 2012;27:205–216. doi: 10.1080/10410236.2011.575540. [DOI] [PubMed] [Google Scholar]
- Horley J, Clarke J. Experience, meaning, and identity in sexuality: A psychosocial theory of sexual stability and change. Springer; 2016. [Google Scholar]
- Hotton AL, French AL, Hosek SG, Kendrick SR, Lemos D, Brothers J, Kincaid SL, Mehta SD. Relationship dynamics and sexual risk reduction strategies among heterosexual young adults: A qualitative study of sexually transmitted infection clinic attendees at an Urban Chicago Health Center. AIDS Patient Care STDS. 2015;29:668–674. doi: 10.1089/apc.2015.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussen SA, Bowleg L, Sangaramoorthy T, Malebranche DJ. Parents, peers and pornography: The influence of formative sexual scripts on adult HIV sexual risk behaviour among Black men in the USA. Cult Health Sex. 2012;14:863–877. doi: 10.1080/13691058.2012.703327. [DOI] [PubMed] [Google Scholar]
- Jones R. Sex scripts and power: A framework to explain urban women's HIV sexual risk with male partners. Nurs Clin North Am. 2006;41:425–436, vii. doi: 10.1016/j.cnur.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Kim CY, Hewit DT, Losen DJ. The School-to-Prison Pipeline: Structuring Legal Reform. New York University Press; New York and London: 2010. [Google Scholar]
- King JL. On the down low: A journey into the lives of “straight” Black men who sleep with men. Broadway Books; 2004. [Google Scholar]
- Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: Risk-factor analysis. Lancet. 2001;357:1397–1401. doi: 10.1016/S0140-6736(00)04562-1. [DOI] [PubMed] [Google Scholar]
- Lane SD, Keefe RH, Rubinstein RA, Levandowski BA, Freedman M, Rosenthal A, Cibula DA, Czerwinski M. Marriage promotion and missing men: African American women in a demographic double bind. Med Anthropol Q. 2004;18:405–428. doi: 10.1525/maq.2004.18.4.405. [DOI] [PubMed] [Google Scholar]
- Latkin C, Donnell D, Liu TY, Davey-Rothwell M, Celentano D, Metzger D. The dynamic relationship between social norms and behaviors: The results of an HIV prevention network intervention for injection drug users. Addiction. 2013;108:934–943. doi: 10.1111/add.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Donnell D, Metzger D, Sherman S, Aramrattna A, Davis-Vogel A, Quan VM, Gandham S, Vongchak T, Perdue T, Celentano DD. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc Sci Med. 2009;68:740–748. doi: 10.1016/j.socscimed.2008.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallory C, Stern PN. Awakening as a change process among women at risk for HIV who engage in survival sex. Qual Health Res. 2000;10:581–594. doi: 10.1177/104973200129118660. [DOI] [PubMed] [Google Scholar]
- Mantell JE, Dworkin SL, Exner TM, Hoffman S, Smit JA, Susser I. The promises and limitations of female-initiated methods of HIV/STI protection. Soc Sci Med. 2006;63:1998–2009. doi: 10.1016/j.socscimed.2006.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall BD, Perez-Brumer AG, MacCarthy S, Mena L, Chan PA, Towey C, Barnett N, Parker S, Barnes A, Brinkley-Rubinstein L, Rose JS, Nunn AS. Individual and partner-level factors associated with condom non-use among African American STI clinic attendees in the deep south: An event-level analysis. AIDS Behav. 2016;20:1334–1342. doi: 10.1007/s10461-015-1266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martyn KK, Hutchinson SA. Low-income African American adolescents who avoid pregnancy: Tough girls who rewrite negative scripts. Qual Health Res. 2001;11:238–256. doi: 10.1177/104973201129119073. [DOI] [PubMed] [Google Scholar]
- Masters NT, Casey E, Wells EA, Morrison DM. Sexual scripts among young heterosexually active men and women: continuity and change. J Sex Res. 2013;50:409–420. doi: 10.1080/00224499.2012.661102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan-Lemal E, Toledo L, O'Daniels C, Villar-Loubet O, Simpson C, Adimora AA, Marks G. “A man's gonna do what a man wants to do”: African American and Hispanic women's perceptions about heterosexual relationships: A qualitative study. BMC Womens Health. 2013;13:27. doi: 10.1186/1472-6874-13-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meader N, Semaan S, Halton M, Bhatti H, Chan M, Llewellyn A, Des Jarlais DC. An international systematic review and meta-analysis of multisession psychosocial interventions compared with educational or minimal interventions on the HIV sex risk behaviors of people who use drugs. AIDS Behav. 2013;17:1963–1978. doi: 10.1007/s10461-012-0403-y. [DOI] [PubMed] [Google Scholar]
- Miller WC, Ford CA, Morris M, Handcock MS, Schmitz JL, Hobbs MM, Cohen MS, Harris KM, Udry JR. Prevalence of chlamydial and gonococcal infections among young adults in the United States. JAMA. 2004;291:2229–2236. doi: 10.1001/jama.291.18.2229. [DOI] [PubMed] [Google Scholar]
- Montgomery JP, Mokotoff ED, Gentry AC, Blair JM. The extent of bisexual behaviour in HIV-infected men and implications for transmission to their female sex partners. AIDS Care. 2003;15:829–837. doi: 10.1080/09540120310001618676. [DOI] [PubMed] [Google Scholar]
- Morgan EM, Z EL. Wanting sex and wanting to wait: Young adults' account of sexual messages from first significant dating partners. Fem Psychol. 2007;17:515–541. [Google Scholar]
- Ortiz-Torres B, Williams SP, Ehrardt A. Urban women's gender scripts: Implications for HIV. Cult Health Sex. 2003;5:1–17. [Google Scholar]
- Paquette R, Tanton C, Burns F, Prah P, Shahmanesh M, Field N, Macdowall W, Gravningen K, Sonnenberg P, Mercer CH. Illicit drug use and its association with key sexual risk behaviours and outcomes: Findings from Britain's third National Survey of Sexual Attitudes and Lifestyles (Natsal-3) PLoS One. 2017;12:e0177922. doi: 10.1371/journal.pone.0177922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevention, C.f.D.C.a. Diagnoses of HIV Infection in the United States and Dependent Areas, 2014, HIV Surveillance Report. Center for Disease Control and Prevention; Atlanta, GA: 2014. p. 123. [Google Scholar]
- National Center for HIV/AIDS, V.H., STD, and TB Prevention, editor. Center for Disease Control and Prevention (CDC) CDC Fact Sheet: Trends in U S HIV Diagnoses, 2005-2014. Center for Disease Control and Prevention; Atlanta, GA: 2016. p. 5. [Google Scholar]
- Pulerwitz J, Amaro H, De Jong W, Gortmaker SL, Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14:789–800. doi: 10.1080/0954012021000031868. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J, Barker G, Segundo M, Nasciemento M. Promoting more gender-equitable norms and behaviors among young men as an HIV/AIDS-prevention strategy. In: Council P, editor. Horizons Research Summary. 2006. [Google Scholar]
- Roye CF, Tolman DL, Snowden F. Heterosexual anal intercourse among Black and Latino adolescents and young adults: a poorly understood high-risk behavior. J Sex Res. 2013;50:715–722. doi: 10.1080/00224499.2012.719170. [DOI] [PubMed] [Google Scholar]
- Sanchez DT, Fetterolf JC, Rudman LA. Eroticizing inequality in the United States: The consequences and determinants of traditional gender role adherence in intimate relationships. J Sex Res. 2012;49:168–183. doi: 10.1080/00224499.2011.653699. [DOI] [PubMed] [Google Scholar]
- Santo SD. Why THIS Secret Twist On The 80/20 Rule Makes Relationships Happier. [Accessed October 14 2016];2015 http://www.yourtango.com/experts/sue-de-santo/new-twist-8020-rule-relationships-and-dating.
- Schoepf BG. Gender relations and development: Political economgy and culture. In: Anang SF, editor. Twenty-first century Africa: Towards a new vision of sustainable development. African World Press; Trenton: 1992. [Google Scholar]
- Semaan S, Des Jarlais DC, Malow R. Behavior change and health-related interventions for heterosexual risk reduction among drug users. Subst Use Misuse. 2006;41:1349–1378. doi: 10.1080/10826080600838018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semaan S, Des Jarlais DC, Sogolow E, Johnson WD, Hedges LV, Ramirez G, Flores SA, Norman L, Sweat MD, Needle R. A meta-analysis of the effect of HIV prevention interventions on the sex behaviors of drug users in the United States. J Acquir Immune Defic Syndr. 2002;30:S73–93. [PubMed] [Google Scholar]
- Semaan S, Neumann MS, Hutchins K, D'Anna LH, Kamb ML, Project RSG. Brief counseling for reducing sexual risk and bacterial STIs among drug users--results from project RESPECT. Drug Alcohol Depend. 2010;106:7–15. doi: 10.1016/j.drugalcdep.2009.07.015. [DOI] [PubMed] [Google Scholar]
- Singer JL, Salovey P. Organized knowledge structure and personality: Person schemas, self schemas, prototypes, and scripts. In: Press, U.o.C, editor. Person schemas and maladaptive interpersonal patterns. Horwitz; MJ, Chicago: 1991. pp. 33–79. [Google Scholar]
- Slovic P. Trust, emotion, sex, politics, and science: Surveying the risk-assessment battlefield. Risk Anal. 1999;19:689–701. doi: 10.1023/a:1007041821623. [DOI] [PubMed] [Google Scholar]
- Spiller MW, Broz D, Wejnert C, Nerlander L, Paz-Bailey G Centers for DiseaseControl and Prevention, National HIV Behavioral Surveillance System Study. HIV infection and HIV-associated behaviors among persons who inject drugs--20 cities, United States, 2012. MMWR Morb Mortal Wkly Rep. 2015;64:270–275. [PMC free article] [PubMed] [Google Scholar]
- Stacy AW, Newcomb MD, Ames SL. Implicit cognition and HIV risk behavior. J Behav Med. 2000;23:475–499. doi: 10.1023/a:1005577132666. [DOI] [PubMed] [Google Scholar]
- Stephens D, Few A. The effects of images of African American women in hip hop on early adolescents' attitudes toward physical attractiveness and interpersonal relationships. Sex Roles. 2007;56:251–264. [Google Scholar]
- Stephens DP, Phillips L. Freaks, Gold Diggers, Divas, and Dykes: The socio-historical development of adolescent African American women's sexual scripts. Sex Cult. 2003;11:3–49. [Google Scholar]
- Stephens DP, Phillips L. Integrating Black feminist thought into conceptual frameworks of African American adolescent women's sexual scripting processes. Sexual Evol Gender. 2005;7:27–55. [Google Scholar]
- Stephens DP, Eaton AA, Boyd B. Hispanic college men's perceptions of appropriate strategies for initiating sexual intercourse with women. Sex Roles. 2017;77:239–253. [Google Scholar]
- Strathdee SA, Galai N, Safaiean M, Celentano DD, Vlahov D, Johnson L, Nelson KE. Sex differences in risk factors for HIV seroconversion among injection drug users: A 10-year perspective. Arch Intern Med. 2001;161:1281–1288. doi: 10.1001/archinte.161.10.1281. [DOI] [PubMed] [Google Scholar]
- Vannier SA, O'Sullivan LF. Communicating interest in sex: Verbal and nonverbal initiation of sexual activity in young adults' romantic dating relationships. Arch Sex Behav. 2011;40:961–969. doi: 10.1007/s10508-010-9663-7. [DOI] [PubMed] [Google Scholar]
- Wagstaff DA, Kelly JA, Perry MJ, Sikkema KJ, Solomon LJ, Heckman TG, Anderson ES. Multiple partners, risky partners and HIV risk among low-income urban women. Fam Plann Perspect. 1995;27:241–245. [PubMed] [Google Scholar]
- Whitehead TL. Urban low-income African American men, HIV/AIDS, and gender identity. Med Anthropol Q. 1997;11:411–447. doi: 10.1525/maq.1997.11.4.411. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Cultural, gender, and psychosocial influences on HIV-related behavior of African-American female adolescents: Implications for the development of tailored prevention programs. Ethn Dis. 1992;2:381–388. [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Partner influences and gender-related factors associated with noncondom use among young adult African American women. Am J Community Psychol. 1998;26:29–51. doi: 10.1023/a:1021830023545. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000;27:539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, Bernhardt JM, Harrington K, Davies SL, Robillard A, Hook EW., 3rd A prospective study of exposure to rap music videos and African American female adolescents' health. Am J Public Health. 2003;93:437–439. doi: 10.2105/ajph.93.3.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, Scd, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000;27:539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]


