Abstract
Background
Poor performance on Drug Stroop tasks, which could indicate attentional bias to drug-related cues, craving, poor cognitive control (including poor response inhibition), has been associated with substance use severity, treatment retention and substance use treatment outcomes. Cognitive Behavioral Therapy (CBT) focuses on training in appraisal and coping strategies, including strategies to minimize the negative impact of triggers and coping with drug-cue-induced craving. One mechanism of action of CBT may be the strengthening of cognitive control processes and reduction of attentional bias to drug-related stimuli.
Methods
Methadone-maintained individuals with cocaine-use disorders, participating in a randomized controlled trial of treatment as usual (TAU) versus TAU plus access to computer-based CBT (CBT4CBT), completed a computerized Drug Stroop task at pre- and post-treatment. Analyses determined whether attentional bias toward drug-related stimuli changed differentially by treatment group or cocaine use outcomes across the treatment period and whether engagement in components of CBT4CBT or TAU treatment related to changes in attentional bias toward drug-related stimuli at post- versus pre-treatment.
Results
Participants achieving a longer duration of cocaine abstinence during treatment (3+ weeks) showed greater reductions in Drug Stroop Effect than those with shorter maximum continuous abstinence. Reductions in Drug Stroop Effect across treatment were associated with greater engagement with CBT4CBT-specific treatment components, but not TAU-specific treatment components.
Conclusions
Reduction in attentional bias to drug-related cues and craving and/or improved executive cognitive control and response inhibition may contribute to the mechanism of action of CBT4CBT.
Keywords: cocaine, cognitive behavioral therapy (CBT), Drug Stroop, Emotional Stroop, cognitive control, attentional bias, psychotherapy
1. Introduction
Cognitive Behavioral Therapy (CBT) and computer-based CBT (CBT4CBT) (Carroll et al., 2008; Carroll et al., 2009; Carroll et al., 2014b) are efficacious treatments for cocaine use disorder. CBT4CBT modules focus on strategies to minimize the vulnerability to triggers (e.g., drug-related stimuli), such as avoiding situations likely to involve triggers, recognizing and changing drug-related thoughts, and temporizing behavior. Since CBT contains training in appraisal and coping strategies, one mechanism of action of CBT (and CBT4CBT) may be the strengthening of executive cognitive-control processes and reduction of attentional bias toward drug-related stimuli and reduced craving, which may reduce the vulnerability to drug use.
The Stroop Effect (from the Color-Word Stroop Task) is a measure of executive cognitive control requiring the individual to override the dominant tendency to read the word instead of naming the color of the ink in which the word is printed, for example, the word “red” printed in blue ink with the correct response being “blue” (Stroop, 1935). Drug Stroop tasks compare response times (e.g., indicate the color of the word) in trials with drug-related word versus neutral words. The Drug Stroop effect (i.e., slowed responding to drug, relative to neutral, stimuli) could indicate attention bias to drug-related cues, cue-induced craving, poor cognitive control and poor response inhibition, and has been proposed to be of clinical relevance in substance using populations (Field and Cox, 2008; Field et al., 2014; Smith and Ersche, 2014). The Drug Stroop effect has been demonstrated in substance-using populations and associated with severity of dependence (Ersche et al., 2010). A larger Drug Stroop Effect has been associated with poorer within-treatment cocaine-use outcomes and treatment retention in individuals with cocaine-use disorder (Carpenter et al., 2006). Drug Stroop Effect increased prior to and during periods of reported temptation to use cocaine or heroin (Waters et al., 2012), increased prior to relapse and was associated with higher likelihood of subsequent relapse (Marhe et al., 2013b; Kennedy et al., 2014). Greater drug-cue-induced craving is associated with likelihood of subsequent relapse on longer time-scales (Li et al., 2014). Pre-treatment self-reported craving and Drug Stroop Effect-related neural activity predicted cocaine use in the months following treatment in cocaine users (Marhe et al., 2013a). Drug Stroop Effect with heroin-related stimuli at pre-treatment predicted relapse in months following treatment, even after controlling for pre-treatment craving, and Drug Stroop Effect was reduced following cue-exposure therapy in heroin users (Marissen et al., 2006).
Here, analyses are presented of a secondary outcome measure (Drug Stroop task) from a randomized controlled trial (RCT) in methadone-maintained individuals with cocaine-use disorder, randomized to receive treatment as usual (TAU) or TAU plus access to CBT4CBT (CBT4CBT+TAU). We assessed whether Drug Stroop Effect changed across treatment differentially by treatment group or cocaine-use outcomes and whether it related to engagement in CBT4CBT or TAU treatment components. Given CBT4CBT’s focus on recognizing triggers and coping with craving, we hypothesized a greater reduction in Drug Stroop Effect at post-versus pre-treatment in CBT4CBT+TAU versus TAU groups, and in those with better versus poorer cocaine abstinence outcomes. Furthermore, we hypothesized that greater engagement with CBT4CBT, but not TAU, treatment components will be associated with lower Drug Stroop Effect at post-treatment and greater reduction in Drug Stroop Effect at post- versus pre-treatment.
2. Methods
2.1 Participants
Participants in a RCT evaluating the efficacy of CBT4CBT for cocaine-use disorders (Carroll et al., 2014b) were eligible for the RCT if they were stabilized in methadone maintenance, met criteria for current cocaine dependence (past 30 days) (DSM-IV; American Psychiatric Association, 1994), English-speaking, had a reading-level ≥6th grade, and no untreated or unstable psychotic disorders. Drug Stroop task data were available on a subset of the individuals participating in the parent RCT. Only those with Drug Stroop data at pre-treatment and post-treatment time points were included in the analyses. Within the RCT sample (N=101), N=22 were missing Drug Stroop data at pre- or post-treatment, leaving a final randomized sample of N=79 with pre- and post-treatment Drug Stroop data. Of the RCT participants who completed treatment (N=69), N=8 were missing Drug Stroop data at pre- or post-treatment, leaving a final completer sample of N=61 with pre- and post-treatment Drug Stroop data. Drug Stroop data were missing due to the task being added after the start of the RCT.
2.2 Treatments
During the 8-week treatment trial, the standard treatment at the outpatient clinic was offered as a platform treatment. ‘Treatment as usual’ (TAU) consisted of daily methadone-maintenance and weekly counseling sessions. The CBT4CBT+TAU group received access to CBT4CBT over the 8 weeks in addition to TAU. The CBT4CBT program, described in detail elsewhere (Carroll et al., 2008; Carroll et al., 2014b), is a user-friendly computer-based program designed to teach CBT tools in an interactive and engaging environment. The CBT4CBT program consists of seven, 45-minute ‘modules’ which cover: (1) understanding and changing patterns of drug use, (2) coping with craving, (3) refusing offers of drugs and alcohol, (4) problem-solving skills, (5) challenging thoughts about drug use, (6) improving decision-making skills, and (7) HIV-risk reduction skills. Each module includes a brief check-in and agenda, introduction to skill topic, videos of characters experiencing a common risky situation and demonstrating how to use the targeted skill successfully, interactive exercises, and introduction to the practice assignment (i.e., homework). For CBT4CBT, privacy and confidentiality were protected by using a dedicated computer with a login and password system, located in a private room at the clinic. No protected health information (PHI) is collected by the program. Computerized urn randomization balanced TAU and CBT4CBT+TAU groups on gender, race/ethnicity, education level, and cocaine use at baseline (# days of use in past month).
2.3 Assessments
Research assistants assessed participants at baseline, twice-weekly during treatment and at the 8-week treatment termination point. Detailed day-by-day self-reports of drug and alcohol use were collected with the Timeline Followback method (Robinson et al., 2014) for the 28-day period prior to randomization and throughout treatment. Measures of longest duration of abstinence during treatment were based on these self-report measures. Urine toxicology screens for cocaine, marijuana, benzodiazepines, opiates, methamphetamine were collected at each research visit. Other assessments are described in detail in the main study report (Carroll et al., 2014b). Assessments were completed at the clinic, after participants had received their methadone dose. Cognitive assessments (e.g., Drug Stroop task) were completed last, after all other assessment components were done.
2.3.1 Drug Stroop task
A computerized ‘Drug Stroop’ task (Reeves et al., 1991; Reeves et al., 2002) was completed at pre- and post-treatment (week 8). The task consisted of a practice and a task condition. During the practice, a series of letters were displayed on the screen in different colored font. Participants were asked to press quickly and accurately on buttons corresponding with different colored fonts, to teach color-button pairings. During the task, which required the participants to override the dominant tendency to word read, participants were shown words on the screen, written in different colored fonts and asked to press as quickly accurately as possible on buttons corresponding with the different colored font (button-color combinations were consistent with the practice condition). Words were either cocaine-related ‘drug’ (e.g., cocaine) or ‘neutral’ (e.g., chair) words.
2.4 Statistical analyses
Data presented are from a subset of parent RCT participants who were randomized to a treatment condition and performed the Drug Stroop task at pre-treatment and post-treatment (randomized N=79; treatment completer N=61). Treatment groups were compared with chi-square and ANOVAs to assess for baseline differences, as well as primary clinical outcomes, as defined in the parent RCT (Carroll et al., 2014b). Repeated measures ANOVAs were run and included trial type (drug-related versus neutral words) and time-point (pre- versus post-treatment) as within-subject factors to assess whether attentional bias toward drug-related stimuli changes across treatment, and whether this occurs differentially across treatment group or cocaine abstinence outcomes. Treatment group (CBT4CBT+TAU, TAU) or longest duration of cocaine-abstinence during treatment (greater or less than 3 weeks) were included as between-subject factors in separate ANOVAs. The 3-week cut-off for abstinence was based on prior work supporting this measure as a meaningful cocaine outcome (Carroll et al., 2014a). These analyses focused on the completer sample (N=61) because sufficient treatment exposure and duration of treatment retention (results for the randomized sample reported in Supplemental Table 1) was needed to examine treatment mechanisms. The primary outcome measure for the Drug Stroop task was mean response time (RT) for correct responses by trial-type (drug, neutral trials). Trials with response times <100ms were excluded (n=4 trials excluded) from the calculation of participants’ mean correct response times, since <100ms is considered insufficient time to visually process and respond to the stimulus. A secondary outcome measure was percent correct responses by trial-type. Generalized eta squared (η2G) effect sizes were calculated for the ANOVA analyses (Bakeman, 2005). Kendall’s rank correlation (i.e., Kendall’s tau (T)) assessed the relationship between the Drug Stroop ‘Effect’ (average correct response time for drug trials-average correct response time for all neutral trials) at pre-treatment, post-treatment, and change (post-pre-treatment), and indicators of treatment engagement that were TAU-related (present in both groups: number of group sessions, methadone dose), CBT4CBT-related (present in CBT4CBT condition only: number of CBT4CBT sessions, number of CBT4CBT homework assignments done); and overall days in treatment protocol. Correlations were carried out within each treatment group separately within the randomized sample (N=79), since continuous measures of exposure were used, making the restriction to treatment completers unnecessary. Correlations reported as significant survived Bonferroni corrections for multiple comparisons within each treatment group (e.g., 15 correlations within CBT4CBT+TAU; pcorrected=0.05/15=0.0033).
3. Results
3.1 Baseline demographics
There were no significant differences in demographics, baseline substance use, treatment engagement or treatment outcomes between treatment groups in completer (N=61) or randomized (N=79) samples, except baseline cigarette-smoking (CBT4CBT+TAU>TAU; randomized sample) (Table 1).
Table 1.
Baseline demographic, psychiatric, and substance-use characteristics by treatment group
| COMPLETER SAMPLE | RANDOMIZED SAMPLE | |||||||
|---|---|---|---|---|---|---|---|---|
| Total Complete rs (n=61) |
CBT4CBT+T AU (n=29) |
TAU (n=3 2) |
Statistics by Treatme nt Group |
Total Randomiz ed (n=79) |
CBT4CBT+T AU (n=38) |
TAU (n=41) |
Statistics by Treatme nt Group |
|
| Demographics | F(p) or X2 (p) | F(p) or X2 (p) | ||||||
| Sex, N (%) Female | 34 (55.7) | 16 (55.2) | 18 (56.3) | 0.01 (0.93) | 46 (58.2) | 23 (60.5) | 23 (56.1) | 0.16 (0.69) |
| Age | 43.1 (9.2) | 44.3 (8.6) | 42.0 (9.8) | 0.93 (0.34) | 42.2 (9.6) | 43.0 (9.3) | 41.5 (9.9) | 0.46 (0.50) |
| High School Graduate or Higher, N (%) | 44 (72.1) | 21 (72.4) | 23 (71.9) | 0.002 (0.96) | 55 (69.6) | 25 (65.8) | 30 (73.2) | 0.51 (0.48) |
| Race, N (%) | 1.5 (0.68) | 1.81 (0.61) | ||||||
| Caucasian | 35 (57.4) | 16 (55.2) | 19 (59.4) | 50 (63.3) | 24 (63.2) | 26 (63.4) | ||
| African-American | 20 (32.8) | 11 (37.9) | 9 (28.1) | 22 (27.8) | 12 (31.6) | 10 (24.4) | ||
| Hispanic | 5 (8.2) | 2 (6.9) | 3 (9.4) | 6 (7.6) | 2 (5.3) | 4 (9.8) | ||
| Multiracial/Other | 1 (1.6) | 0 (0.0) | 1 (3.1) | 1 (1.3) | 0 (0) | 1 (2.4) | ||
| Estimated IQ (SILS) | 88.2 (12.6) | 88.7 (12.0) | 87.8 (12.8) | 0.08 (0.77) | 87.5 (13.1) | 88.4 (13.1) | 86.6 (13.3) | 0.35 (0.56) |
| Number of months incarcerated, lifetime | 41.2 (64.8) | 34.8 (55.3) | 47.0 (72.8) | 0.53 (0.47) | 36.9 (60.5) | 32.7 (49.3) | 40.9 (69.8) | 0.35 (0.56) |
| On probation or parole, N (%) | 8 (13.1) | 2 (6.9) | 6 (18.8) | 1.9 (0.17) | 12 (15.2) | 5 (13.2) | 7 (17.1) | 0.24 (0.63) |
| Current Substance Use Measures | ||||||||
| Route of Cocaine Administration, N (%) | 0.69 (0.71) | 0.35 (0.84) | ||||||
| Smoke | 50 (82.0) | 25 (86.2) | 25 (78.1) | 67 (84.8) | 33 (86.8) | 34 (82.9) | ||
| Snort | 8 (13.1) | 3 (10.3) | 5 (15.6) | 9 (11.4) | 4 (10.5) | 5 (12.2) | ||
| Intravenous | 3 (4.9) | 1 (3.4) | 2 (6.3) | 3 (3.8) | 1 (2.6) | 2 (4.9) | ||
| Methadone Dose | 82.1 (27.1) | 83.8 (28.7) | 80.6 (25.9) | 0.21 (0.65) | 83.1 (26.8) | 84.1 (28.2) | 82.2 (25.8) | 0.10 (0.76) |
| Age first used Cocaine | 19.6 (5.0) | 20.2 (5.5) | 19.0 (4.5) | 0.98 (0.33) | 19.7 (4.9) | 19.9 (5.3) | 19.5 (4.6) | 0.10 (0.75) |
| Other Lifetime Psychiatric Diagnoses, N(%) | ||||||||
| Alcohol-Use Disorder | 49 (80.3) | 25 (86.2) | 24 (75.0) | 1.21 (0.27) | 61 (78.2) | 30 (81.1) | 31 (75.6) | 0.34 (0.56) |
| Sedative-Use Disorder | 20 (33.3) | 10 (34.5) | 10 (32.3) | 0.03 (0.86) | 26 (33.3) | 12 (31.6) | 14 (35.0) | 0.10 (0.75) |
| Cannabis-Use Disorder | 42 (71.2) | 22 (75.9) | 20 (66.7) | 0.61 (0.44) | 56 (73.7) | 29 (76.3) | 27 (71.1) | 0.27 (0.60) |
| Hallucinogen-Use Disorder | 9 (14.8) | 4 (13.8) | 5 (15.6) | 0.04 (0.84) | 14 (17.7) | 7 (18.4) | 7 (17.1) | 0.03 (0.88) |
| Major Depression | 20 (32.8) | 10 (34.5) | 10 (31.3) | 0.07 (0.79) | 24 (30.4) | 13 (34.2) | 11 (26.8) | 0.51 (0.48) |
| Anxiety Disorder | 17 (27.9) | 10 (34.5) | 7 (21.9) | 1.20 (0.27) | 23 (29.1) | 13 (34.2) | 10 (24.4) | 0.92 (0.34) |
| Panic Disorder | 8 (13.1) | 6 (20.7) | 2 (6.3) | 2.78 (0.10) | 12 (15.2) | 8 (21.1) | 4 (9.8) | 1.95 (0.16) |
| Antisocial-Personality Disorder | 5 (8.2) | 3 (10.3) | 2 (6.3) | 0.34 (0.56) | 7 (8.9) | 5 (13.2) | 2 (4.9) | 1.67 (0.20) |
| Post-Traumatic Stress Disorder | 10 (16.7) | 6 (20.7) | 4 (12.9) | 0.65 (0.42) | 12 (15.4) | 6 (15.8) | 6 (15.0) | 0.01 (0.92) |
| Days of Use in Month Prior to Treatment1 | ||||||||
| Cocaine | 14.2 (9.0) | 14.6 (8.7) | 13.9 (9.4) | 0.10 (0.76) | 14.8 (9.3) | 16.2 (9.5) | 13.5 (9.1) | 1.6 (0.20) |
| Heroin | 1.8 (5.3) | 1.4 (5.2) | 2.1 (5.5 | 0.22 (0.64) | 1.7 (5.2) | 1.2 (4.6) | 2.2 (5.7) | 0.67 (0.42) |
| Alcohol | 0.4 (0.5) | 0.4 (0.5) | 0.3 (0.5) | 0.66 (0.42) | 0.4 (0.5) | 0.4 (0.5) | 0.3 (0.5) | 0.92 (0.34) |
| Cannabis | 3.0 (6.9) | 2.6 (6.6) | 3.4 (7.3) | 0.18 (0.68) | 2.7 (6.5) | 2.1 (5.8) | 3.2 (7.1) | 0.63 (0.43) |
| Cigarettes | 26.4 (6.1) | 27.4 (3.0) | 25.5 (7.8) | 1.54 (0.22) | 25.7 (7.3) | 27.6 (2.6) | 23.9 (9.5) | 5.23 (0.03) |
| Lifetime Years of Regular Use | ||||||||
| Cocaine | 11.6 (8.5) | 12.0 (6.5) | 11.3 (10.1) | 0.13 (0.72) | 11.7 (8.4) | 12.4 (6.7) | 11.0 (9.7) | 0.55 (0.46) |
| Opiate | 10.2 (8.3) | 9.8 (7.0) | 10.6 (9.4) | 0.14 (0.71) | 10.8 (8.7) | 10.5 (7.6) | 11.0 (9.7) | 0.08 (0.78) |
| Alcohol | 8.0 (8.8) | 7.6 (8.6) | 8.4 (9.0) | 0.13 (0.72) | 8.2 (9.5) | 8.9 (10.4) | 7.5 (8.7) | 0.40 (0.53) |
| Cannabis | 8.3 (9.3) | 6.7 (7.5) | 9.8 (10.6) | 1.74 (0.19) | 8.0 (9.5) | 6.9 (8.1) | 9.0 (10.6) | 0.91 (0.34) |
| Treatment Engagement | ||||||||
| Days in Treatment (out of 56) | 56.0 (0.0) | 56.0 (0.0) | 56.0 (0.0) | 0.00 (1.00) | 47.7 (17.6) | 47.6 (17.1) | 47.9 (18.2) | 0.01 (0.94) |
| Number of CBT4CBT Sessions Attended | n/a | 6.2 (1.4) | n/a | n/a | n/a | 5.1 (2.5) | n/a | n/a |
| Number of CBT4CBT Homework Assignments Done | n/a | 3.5 (2.1) | n/a | n/a | n/a | 2.8 (2.2) | n/a | n/a |
| Number of Group TAU Sessions Attended | 8.3 (13.7) | 6.4 (9.5) | 9.8 (16.4) | 0.92 (0.34) | 8.34 (13.2) | 6.4 (9.0) | 10.0 (15.8) | 1.18 (0.28) |
| Treatment Outcome Measures | ||||||||
| % Urines Negative for Cocaine Within Treatment Period | 24.4 (29.7) | 29.8 (33.5) | 19.5 (25.2) | 1.87 (0.18) | 22.8 (31.1) | 25.4 (34.0) | 20.1 (27.9) | 0.53 (0.47) |
| % Days Self-reported Abstinence Within Treatment Period | 62.7 (27.9) | 65.6 (27.8) | 60.0 (28.1) | 0.60 (0.44) | 59.3 (30.1) | 59.6 (31.5) | 59.0 (29.2) | 0.01 (0.93) |
| Longest Duration Continuous Abstinence Within Treatment Period (Days) | 12.4 (12.9) | 14.1 (14.3) | 11.0 (11.6) | 0.87 (0.35) | 11.0 (12.5) | 11.3 (13.5) | 10.6 (11.6) | 0.06 (0.82) |
| 3+ Weeks Continuous Abstinence, (N (%)) | 11 (18.0) | 8 (27.6) | 3 (9.4) | 3.4 (0.07) | 12 (15.2) | 8 (21.1) | 4 (9.8) | 1.95 (0.16) |
Days of use in month prior to treatment was out of a possible total of 28 days (i.e., past four weeks) Results are reported as mean (SD) unless otherwise noted, in which case it is reported as N (percent)
SILS=Shipley Institute of Living Scale; RT= response time; ms =milliseconds
3.2 Changes in Drug Stroop task performance by treatment group and abstinence status
Changes in Drug Stroop task performance results are presented in full in Table 2.
Table 2.
Drug Stroop Task Performance
| I. Drug Stroop Behavior: Means, SD | Completers (N=61) | |||||
|
|
||||||
| Total (n=61) | CBT4CBT+TAU (n=29) | TAU (n=32) | ||||
|
|
||||||
| Ii. Pre-Treatment | Mean | SD | Mean | SD | Mean | SD |
| Drug Trials: Mean Correct RT (ms) | 817.02 | 204.75 | 824.00 | 217.03 | 810.69 | 196.23 |
| Neutral Trials: Mean Correct RT (ms) | 778.15 | 171.26 | 784.38 | 156.51 | 772.50 | 185.94 |
| Drug Trials: Proportion Correct | 0.97 | 0.04 | 0.96 | 0.05 | 0.98 | 0.04 |
| Neutral Trials: Proportion Correct | 0.97 | 0.03 | 0.97 | 0.03 | 0.97 | 0.03 |
| Iii. Post-Treatment | ||||||
| Drug Trials: Mean Correct RT (ms) | 745.22 | 168.77 | 699.76 | 129.60 | 786.43 | 190.46 |
| Neutral Trials: Mean Correct RT (ms) | 739.54 | 145.08 | 722.10 | 133.62 | 755.35 | 155.13 |
| Drug Trials: Proportion Correct | 0.94 | 0.14 | 0.94 | 0.11 | 0.94 | 0.17 |
| Neutral Trials: Proportion Correct | 0.95 | 0.07 | 0.95 | 0.05 | 0.95 | 0.08 |
|
| ||||||
| II. Drug Stroop Statistics | Completers (N=61) | |||||
|
|
||||||
| Mean Correct RT | Percent Correct | |||||
|
|
||||||
| IIi. Between Subject Factor: Treatment Group | F (df=1,59) | p | η2G | F (df=1,59) | p | η2G |
|
|
||||||
| Trial Type (Drug, Neutral) | 5.75 | 0.02 | 0.004 | 1.86 | 0.18 | 0.003 |
| Time Point (Pre-, Post-Treatment) | 11.60 | 0.001 | 0.027 | 2.90 | 0.09 | 0.018 |
| Treatment Group (CBT4CBT+TAU; TAU) | 0.36 | 0.55 | 0.005 | 0.14 | 0.07 | 0.001 |
| Trial type × time point | 4.51 | 0.04 | 0.003 | 1.00 | 0.32 | 0.001 |
| Time point × treatment group | 4.70 | 0.03 | 0.011 | 0.14 | 0.713 | 0.001 |
| Trial type × treatment group | 2.07 | 0.16 | 0.035 | 0.53 | 0.47 | 0.084 |
| Trial type × time point × treatment group | 2.85 | 0.097 | 0.002 | 0.36 | 0.55 | 0.001 |
|
|
||||||
| IIii. Between Subject Factor: Abstinence Outcome | F (df=1,59) | p | η2G | F (df=1,59) | p | η2G |
|
|
||||||
| Trial Type (Drug, Neutral) | 3.93 | 0.05 | 0.003 | 1.98 | 0.17 | 0.003 |
| Time Point (Pre-, Post-Treatment) | 11.78 | 0.001 | 0.028 | 1.21 | 0.28 | 0.008 |
| Abstinence Outcome (</>3 weeks abstinence) | 0.12 | 0.73 | 0.002 | 0.26 | 0.61 | 0.002 |
| Trial type × time point | 10.8 | 0.002 | 0.006 | 0.001 | 0.98 | 0.000 |
| Time point × abstinence outcome | 2.18 | 0.15 | 0.005 | 0.13 | 0.72 | 0.001 |
| Trial type × abstinence outcome | 0.03 | 0.86 | 0.032 | 0.37 | 0.55 | 0.082 |
| Trial type × time point × abstinence outcome | 6.79 | 0.01 | 0.004 | 1.46 | 0.23 | 0.002 |
CBT4CBT=computer based cognitive behavioral therapy; TAU=treatment as usual; ms=milliseconds. Statistics in bold are significant (p<.05) and in bold italics are trend
η2G= Generalized Eta Squared
In the analysis comparing treatment groups, within the completer sample, a trend (p<0.1) time-point-by-trial-type-by-group interaction, and significant time-point-by-group and trial-type-by-time-point interactions reflected greater reduction in RT to the drug-related (versus neutral) trials at post- versus pre-treatment in the CBT4CBT+TAU versus TAU group. This pattern indicates more reduction in Drug Stroop Effect in the CBT4CBT+TAU versus TAU group. In addition, there were significant effects on mean correct RT for time-point (pre>post-treatment; with no significant change in percent accuracy) reflecting faster RT at post- relative to pre-treatment, and trial-type (drug>neutral) indicating the expected Drug Stroop Effect (slower responding to drug versus neutral stimuli).
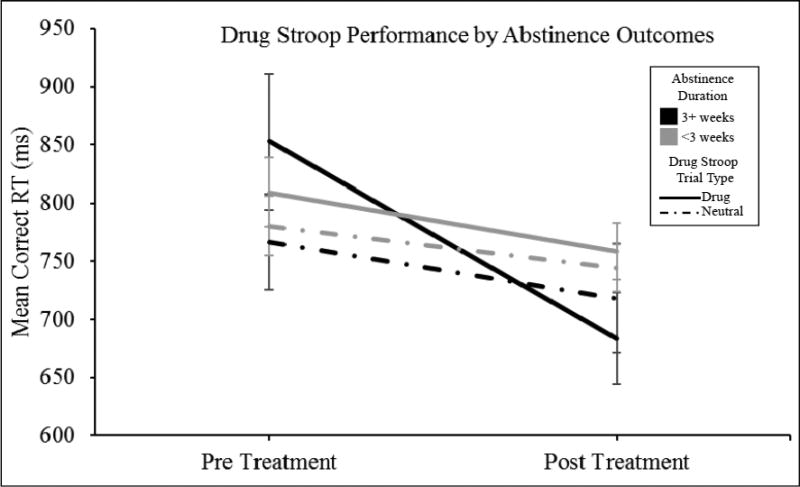
In the analysis comparing abstinence outcomes, within the completer sample, there was a time-point-by-trial-type-by-abstinence interaction showed greater reduction Drug Stroop Effect in the group that achieved longer (3+ weeks) abstinence during treatment, relative to the group with shorter abstinence duration. Furthermore, a time-point-by-trial-type-interaction and a main effect on mean correct RT of time-point (pre-treatment>post-treatment) indicated less slowing to drug-related stimuli at post- versus pre-treatment (Figure 1).
Figure 1. Changes in Drug Stroop Performance across Treatment Period by Abstinence Outcome.
Within the completer sample (N=61), a significant time point (pre-, post-treatment) by trial type (drug, neutral) by longest duration of abstinence during treatment (3+ weeks; <3 weeks) reflected greater improvement in Drug Stroop performance (reduced slowing to drug-related stimuli relative to neutral stimuli) in the group that achieved longer (3+ weeks) abstinence during treatment, relative to the group with shorter abstinence duration. Color indicates abstinence outcome (black=3+ weeks continuous abstinence during treatment; gray=<3 weeks continuous abstinence during treatment). Line type indicates Drug Stroop trial type (solid=Drug trials; dotted=Neutral trials). RT= response time (in milliseconds).
Within the completer sample, there were no significant main or interactive effects on the secondary outcome of proportion correct responses when analyzed by treatment group or abstinence outcome.
3.3 Associations between Drug Stroop task performance and treatment engagement
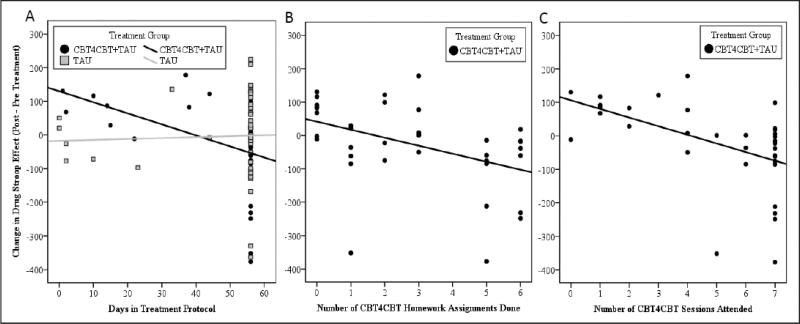
Correlation results are reported in full in Table 3. Correlations between treatment engagement indicators and Drug Stroop Effect performance assessed whether this measure at pre-treatment, post-treatment or change (post-pre-treatment) was associated with treatment engagement and retention. Larger ‘Drug Stroop Effect’ scores reflect greater response time slowing to drug-related stimuli versus neutral stimuli (mean correct RT for drug - neutral trials). Change in Drug Stroop Effect scores at post- vs. pre-treatment were negatively correlated with CBT4CBT treatment engagement indicators (number of CBT4CBT Sessions, CBT4CBT Homework Assignments Done, and Days in Treatment Protocol (CBT4CBT+TAU group; Figure 2a–c). These associations were not observed at pre- or post-treatment for CBT4CBT+TAU-related treatment components and were not observed or for TAU-related treatment components in either the CBT4CBT+TAU group or the TAU group at any time-point. Therefore, more engagement with CBT4CBT, but not TAU, treatment components were associated with a greater reduction in Drug Stroop Effect at post- relative to pre-treatment.
Table 3.
Associations between Drug Stroop Effect and Indicators of Treatment Engagement
| TREATMENT ENGAGEMENT INDICATORS |
CBT4CBT +TAU Treatment Group | TAU Treatment Group | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre- Treatment |
Post- Treatment |
Change (PostTx - PreTx) |
Pre- Treatment |
Post- Treatment |
Change (PostTx - PreTx) |
|||
| TAU Treatment Components | ||||||||
| # Group TAU Sessions During Active Treatment | T | −0.061 | −0.171 | −0.044 | 0.085 | 0.041 | 0.002 | |
| p | 0.664 | 0.221 | 0.752 | 0.494 | 0.738 | 0.988 | ||
| N | 29 | 29 | 29 | 35 | 35 | 35 | ||
| Methadone dose | T | 0.08 | 0.101 | −0.01 | 0.1 | −0.045 | −0.076 | |
| p | 0.487 | 0.384 | 0.93 | 0.38 | 0.69 | 0.501 | ||
| N | 38 | 38 | 38 | 41 | 41 | 41 | ||
| CBT4CBT Treatment Components | ||||||||
| # Computerized CBT (CBT4CBT) Sessions Attended | T | 0.215 | −0.229 | −0.463 | . | . | . | |
| p | 0.083 | 0.065 | 0.0002 | . | . | . | ||
| N | 38 | 38 | 38 | . | . | . | ||
| # CBT Homework Assignments Done | T | 0.199 | −0.162 | −0.363 | . | . | . | |
| p | 0.099 | 0.179 | 0.0026 | . | . | . | ||
| N | 38 | 38 | 38 | . | . | . | ||
| Overall Study Treatment Duration | ||||||||
| Days in treatment protocol | T | 0.199 | −0.265 | −0.488 | −0.004 | 0.016 | 0.037 | |
| p | 0.123 | 0.04 | 0.0002 | 0.974 | 0.896 | 0.769 | ||
| N | 38 | 38 | 38 | 41 | 41 | 41 | ||
Correlations betwen Drug Stroop Effect (mean correct RT for drug trials - mean correct RT for neutral trials; at pre-treatment, post-treatment and change (Post- Pre Treatment)) and measures of treatment engagement were run within the randomized sample (N=79), split by treatment group (CBT4CBT+TAU=38; TAU=41). CBT= cognitive behavioral therapy; TAU=treatment as usual; Tx=treatment; T;= tau= Kendall’s rank correlation coefficient. CBT homework was assigned at CBT4CBT sessions, and the correlation between these two variables was T=0.59 (p<.001). Fifteen correlations were run within the CBT4CBT+TAU group. A Bonferroni-corrected p-value for these multiple comparisons would be pcorrected=0.05/15=0.0033. Therefore, the associations between change in Drug Stroop and number of CBT4CBT sessions, number of CBT homework assignments done, and number of days in treatment protocol within the CBT4CBT+TAU group remain significant following Bonferroni correction (indicated with gray highlights).
Figure 2. Associations between change in Drug Stroop Effect at post- relative to pre-treatment and indicators of CBT4CBT treatment engagement.
Drug Stroop Effect indicates slower responding to drug (cocaine) cues relative to neutral cues (mean correct RT for drug trials – mean correct RT for neutral trials). Therefore, a negative change score, showing lower Drug Stroop Effect at post-treatment relative to pre-treatment, reflects an improvement on this task. Greater reduction in Drug Stroop Effect was associated with (A) more ‘days in the treatment protocol’ within the CBT4CBT+TAU group but not in the TAU only group; (B) more CBT4CBT homework assignments completed in the CBT4CBT+TAU group; and (C) more CBT4CBT sessions attended in the CBT4CBT group. For full correlation matrix, including non-significant associations between TAU treatment components and Drug Stroop measures, see Table 3.
4. Discussion
First, reduction in Drug Stroop Effect (cocaine-related cues) at post- relative to pre-treatment was affected by treatment assignment: participants assigned to CBT4CBT+TAU showed a trend towards greater reduction in Drug Stroop Effect across treatment relative to those receiving TAU. Second, individuals who achieved three or more weeks of continuous cocaine abstinence during treatment showed significantly greater reduction in Drug Stroop Effect relative to those who did not. Third, greater engagement with CBT4CBT-specific treatment components (e.g., CBT4CBT sessions, homework, days in treatment protocol within the CBT4CBT+TAU group) was associated with greater reduction in Drug Stroop Effect across treatment, despite no association with pre-treatment Drug Stroop Effect. Conversely, engagement with TAU-specific components of treatment (e.g., TAU sessions, methadone dose, days in treatment protocol within the TAU only group) did not correlate with Drug Stroop Effect at any time-point or change in Drug Stroop Effect.
Attentional bias toward drug-related cues, which could enhance the Stroop effect and interfere with executive cognitive control, is thought to relate to drug use and treatment outcomes in part due to its association with cue-induced craving as well as possible general effects on cognitive resources (e.g., (Field and Cox, 2008)). Drug Stroop Effect for cocaine related cues is associated with severity of cocaine craving (Copersino et al., 2004). Cocaine users display poorer response inhibition in response to cocaine-related cues relative to neutral cues (Pike et al., 2013). Poorer cognitive-control in response to cocaine-related cues has been found in cocaine users, compared to healthy non-substance users (Dias et al., 2015) and is associated with more cocaine-cue-induced craving (DiGirolamo et al., 2015). Poor attentional control under increased cognitive load further worsened in the presence of cocaine-related stimuli in cocaine users (Hester and Garavan, 2009). Therefore, our findings of an association between better Drug Stroop task performance and longer abstinence and may reflect improved cognitive control in presence of drug cues, which may either arise from or result in improved ability to resist use. Greater reduction in Drug Stroop Effect in those with longer abstinence supports the clinical relevance of this measure.
Using data from a well-characterized RCT sample is a strength. A limitation of the study is that it is possible that methadone could impact cognitive task performance. All cognitive testing occurred after methadone daily dosing (so subjects should not have been in acute withdrawal) and following all other assessments. However, the time between dosing and cognitive testing could have varied somewhat across individuals, which could, theoretically, have had an impact on task performance. All subjects were stabilized on their methadone doses for at least two months prior to beginning the study and were maintained on this stable dose, which provided the benefit of minimizing methadone-related variability across test days. Furthermore, any possible variability in cognitive performance arising from this slight variation in timing between dosing and testing would mirror what would happen in clinical practice as patients meet with clinicians or participate in groups following methadone dosing. While test-retest reliability of Drug Stroop tasks may be higher than other tasks designed to measure attentional bias (e.g., visual probe), a subset of studies have found it to have acceptable test-retest reliability (Cronbach’s α>0.7), while others have not (for review; (Ataya et al., 2012)). Test-retest reliability of the task may be lower in individuals with lower dependence on the substance used in the cues (e.g., in cigarette smokers responding to smoking cues; Spiegelhalder et al., 2011). This limitation was partially mitigated by all participants in this study meeting criteria for cocaine dependence. While the classic color-word Stroop task and emotional Stroop tasks showed high reliability when response times are directly analyzed, difference scores showed lower test-retest reliability in healthy young adults (Strauss et al., 2005). Diminished test-retest reliability could reduce power to detect treatment related effects. Nevertheless, this is the first clinical trial to indicate differential reduction in attentional bias to drug-related cues by treatment condition, in this case standard methadone maintenance versus computer-based CBT. If replicated, this suggests reduction in attentional bias may be one mechanism of action of CBT4CBT, consistent with the treatment’s focus on recognizing triggers and coping with craving.
Supplementary Material
Highlights.
Computer based cognitive behavioral therapy (CBT4CBT) versus treatment as usual Randomized Controlled Trial (RCT)
Participants were methadone-maintained, seeking treatment for cocaine-use disorders
Reduced (i.e., improved) Drug Stroop effect observed at post- versus pre-treatment
Greater reductions in Drug Stroop effect correlated with more CBT4CBT engagement
More reduction in Drug Stroop effect with longer within-treatment cocaine abstinence
Acknowledgments
Role of Funding Source
This work was supported by National Institute on Drug Abuse grants R37-DA015969 and P50-DA09241. The funding source did not contribute to the analysis or decision to publish this work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Elise DeVito performed the data analysis and wrote the initial draft of the manuscript. Brian Kiluk contributed to completion of the parent RCT. Charla Nich oversaw the clinical data management and consulted on data analyses. Maria Mouratidis consulted on the design of the parent RCT, including the choice of task presented in this manuscript. Kathleen Carroll led the design and oversight of the parent RCT and consulted on the analytic approach. All authors provided feedback on the manuscript and approved the submission of the final version.
Conflict of Interest
Kathleen Carroll is a consultant to CBT4CBT LLC, which makes CBT4CBT available to qualified clinical providers and organizations on a commercial basis. Dr. Carroll works with Yale University to manage any potential conflicts of interest. The other authors report no financial relationships with commercial interests or other potential conflicts of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth. APA Press; Washington DC: 1994. [Google Scholar]
- Ataya AF, Adams S, Mullings E, Cooper RM, Attwood AS, Munafo MR. Internal reliability of measures of substance-related cognitive bias. Drug Alcohol Depend. 2012;121:148–151. doi: 10.1016/j.drugalcdep.2011.08.023. [DOI] [PubMed] [Google Scholar]
- Bakeman R. Recommended effect size statistics for repeated measures designs. Behav. Res. Methods. 2005;37:379–384. doi: 10.3758/bf03192707. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Schreiber E, Church S, McDowell D. Drug Stroop performance: Relationships with primary substance of use and treatment outcome in a drug-dependent outpatient sample. Addict. Behav. 2006;31:174–181. doi: 10.1016/j.addbeh.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, Gordon MA, Portnoy GA, Rounsaville BJ. Computer-assisted delivery of cognitive-behavioral therapy for addiction: A randomized trial of CBT4CBT. Am. J. Psychiatry. 2008;165:881–888. doi: 10.1176/appi.ajp.2008.07111835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: A 6-month follow-up of CBT4CBT. Drug Alcohol Depend. 2009;100:178–181. doi: 10.1016/j.drugalcdep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD, Nich C, DeVito EE, Decker S, LaPaglia D, Duffey D, Babuscio TA, Ball SA. Toward empirical identification of a clinically meaningful indicator of treatment outcome: Features of candidate indicators and evaluation of sensitivity to treatment effects and relationship to one year follow up cocaine use outcomes. Drug Alcohol Depend. 2014a;137:3–19. doi: 10.1016/j.drugalcdep.2014.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD, Nich C, Gordon MA, Portnoy GA, Marino DR, Ball SA. Computer-assisted delivery of cognitive-behavioral therapy: Efficacy and durability of CBT4CBT among cocaine-dependent individuals maintained on methadone. Am. J. Psychiatry. 2014b;171:436–444. doi: 10.1176/appi.ajp.2013.13070987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copersino ML, Serper MR, Vadhan N, Goldberg BR, Richarme D, Chou JC, Stitzer M, Cancro R. Cocaine craving and attentional bias in cocaine-dependent schizophrenic patients. Psychiatry Res. 2004;128:209–218. doi: 10.1016/j.psychres.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Dias NR, Schmitz JM, Rathnayaka N, Red SD, Sereno AB, Moeller FG, Lane SD. Anti-saccade error rates as a measure of attentional bias in cocaine dependent subjects. Behav. Brain Res. 2015;292:493–499. doi: 10.1016/j.bbr.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGirolamo GJ, Smelson D, Guevremont N. Cue-induced craving in patients with cocaine use disorder predicts cognitive control deficits toward cocaine cues. Addict. Behav. 2015;47:86–90. doi: 10.1016/j.addbeh.2015.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ersche KD, Bullmore ET, Craig KJ, Shabbir SS, Abbott S, Muller U, Ooi C, Suckling J, Barnes A, Sahakian BJ, Merlo-Pich EV, Robbins TW. Influence of compulsivity of drug abuse on dopaminergic modulation of attentional bias in stimulant dependence. Arch. Gen. Psychiatry. 2010;67:632–644. doi: 10.1001/archgenpsychiatry.2010.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field M, Cox WM. Attentional bias in addictive behaviors: A review of its development, causes, and consequences. Drug Alcohol Depend. 2008;97:1–20. doi: 10.1016/j.drugalcdep.2008.03.030. [DOI] [PubMed] [Google Scholar]
- Field M, Marhe R, Franken IH. The clinical relevance of attentional bias in substance use disorders. CNS Spectr. 2014;19:225–230. doi: 10.1017/S1092852913000321. [DOI] [PubMed] [Google Scholar]
- Hester R, Garavan H. Neural mechanisms underlying drug-related cue distraction in active cocaine users. Pharmacol. Biochem. Behav. 2009;93:270–277. doi: 10.1016/j.pbb.2008.12.009. [DOI] [PubMed] [Google Scholar]
- Kennedy AP, Gross RE, Ely T, Drexler KP, Kilts CD. Clinical correlates of attentional bias to drug cues associated with cocaine dependence. Am. J. Addict. 2014;23:478–484. doi: 10.1111/j.1521-0391.2014.12134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Li W, Wang H, Wang Y, Zhang Y, Zhu J, Zheng Y, Zhang D, Wang L, Li Y, Yan X, Chang H, Fan M, Li Z, Tian J, Gold MS, Wang W, Liu Y. Predicting subsequent relapse by drug-related cue-induced brain activation in heroin addiction: An event-related functional magnetic resonance imaging study. Addict. Biol. 2014;20:968–78. doi: 10.1111/adb.12182. [DOI] [PubMed] [Google Scholar]
- Marhe R, Luijten M, van de Wetering BJ, Smits M, Franken IH. Individual differences in anterior cingulate activation associated with attentional bias predict cocaine use after treatment. Neuropsychopharmacology. 2013a;38:1085–1093. doi: 10.1038/npp.2013.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marhe R, Waters AJ, van de Wetering BJ, Franken IH. Implicit and explicit drug-related cognitions during detoxification treatment are associated with drug relapse: An ecological momentary assessment study. J Consult. Clin. Psychol. 2013b;81:1–12. doi: 10.1037/a0030754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marissen MA, Franken IH, Waters AJ, Blanken P, van den Brink W, Hendriks VM. Attentional bias predicts heroin relapse following treatment. Addiction. 2006;101:1306–1312. doi: 10.1111/j.1360-0443.2006.01498.x. [DOI] [PubMed] [Google Scholar]
- Pike E, Stoops WW, Fillmore MT, Rush CR. Drug-related stimuli impair inhibitory control in cocaine abusers. Drug Alcohol Depend. 2013;133:768–771. doi: 10.1016/j.drugalcdep.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves D, Schlege R, Gilliland K. The UTCPAB and the NATO AGARD STRES Battery: Results from standardization studies. Medical Defense Biosciences Review 1991 [Google Scholar]
- Reeves D, Winter K, Kane R, Elsmore T, Bleiberg J. ANAM 2001’s User’s Manual. National Cognitive Recovery Foundation 2002 [Google Scholar]
- Robinson SM, Sobell LC, Sobell MB, Leo GI. Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychol. Addict. Behav. 2014;28:154–162. doi: 10.1037/a0030992. [DOI] [PubMed] [Google Scholar]
- Smith DG, Ersche KD. Using a drug-word Stroop task to differentiate recreational from dependent drug use. CNS Spectr. 2014;19:247–255. doi: 10.1017/S1092852914000133. [DOI] [PubMed] [Google Scholar]
- Spiegelhalder K, Jahne A, Kyle SD, Beil M, Doll C, Feige B, Riemann D. Is smoking-related attentional bias a useful marker for treatment effects? Behav. Med. 2011;37:26–34. doi: 10.1080/08964289.2010.543195. [DOI] [PubMed] [Google Scholar]
- Strauss GP, Allen DN, Jorgensen ML, Cramer SL. Test-retest reliability of standard and emotional stroop tasks: An investigation of color-word and picture-word versions. Assessment. 2005;12:330–337. doi: 10.1177/1073191105276375. [DOI] [PubMed] [Google Scholar]
- Stroop JR. Studies of interference in serial verbal reactions. J. Exp. Psychol. 1935;18:642–662. [Google Scholar]
- Waters AJ, Marhe R, Franken IH. Attentional bias to drug cues is elevated before and during temptations to use heroin and cocaine. Psychopharmacol. (Berl.) 2012;219:909–921. doi: 10.1007/s00213-011-2424-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.