Abstract
Background
The relationship between driver blood alcohol concentration (BAC) and crash involvement is well understood. However, the role of alcohol use disorders (AUDs) (i.e., dependence or abuse) in crash occurrence, as distinguished from non-clinical heavy alcohol consumption, has not been adequately explored.
Methods
Data from the 2010–2011 Crash Risk Study conducted in Virginia Beach, VA, were used in this study. Drivers involved in crashes were compared with control drivers, and four drinker groups were examined: alcohol dependent, alcohol abusers, heavy drinkers, and all other current (i.e., normative) drinkers. Logistic regression analyses were conducted on two outcomes: having a moderate BAC (≥ .05 g/dl), and crash involvement.
Results
Overall, 2,411 crash-involved and 5,514 control drivers provided useable data, 52.4% of which were men and 70.8% Whites. The prevalence of drivers with AUDs was lower for the crash-involved drivers (8.7%) than for the control drivers (12.7%). Only heavy drinkers, but not abusive or dependent drinkers, were over four times more likely to drive with moderate BACs at nighttime. More important, at nighttime, the odds of crash involvement for dependent drinkers were only one third of those for normative drinkers. Daytime crashes, however, were more likely to involve normative drinkers than any of the other three drinker types.
Conclusions
Drivers with AUDs are not more likely than normative drinkers to drive with moderate BACs at night. After accounting for the influence of BAC, dependent drinkers have a lower risk of being involved in a crash, at any time of the day.
Keywords: alcohol use disorder, heavy drinking, crash involvement
1. Introduction
It is well known that alcohol impairs driving skills and endangers drivers in motor vehicle crashes across the world. Prior studies have proved that higher blood alcohol concentrations (BACs) can significantly elevate drivers’ likelihood of crashing (e.g., Blomberg et al., 2009; Borkenstein et al., 1974; Moskowitz and Fiorentino, 2000; Zador et al., 1999). For drivers under the influence of alcohol (DUI) and thus at a higher risk of crash involvement, their drinking characteristics have been the focus of an ongoing debate among researchers and policy makers, i.e., whether drivers with drinking problems contribute more to crash occurrence than other types of drinkers. The answer to this question is critical for DUI policy decisions regarding the allocation of increasingly scarce resources, either to programs on “problem drinkers”, or to general deterrence programs aimed at the much larger number of drivers in the general drinking public, or both.
Among US drivers arrested for DUI, many of them were found to have alcohol-related problems (Cavaiola and Wuth, 2002; Fell et al., 2010; Jones and Lacey, 2002; Lapham et al., 2004; Robertson et al., 2008). As measured in different ways across studies, such “problem drinkers” could have characteristics like heavy and frequent alcohol consumption, life problems related to drinking, or even diagnoses of alcohol use disorders (AUDs) (i.e., alcohol abuse or dependence meeting the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition [DSM-IV] criteria). Research evidence from other countries also supports that about a third or more of the first-time DUI offenders have drinking problems including AUDs (Bergman et al., 2005; Okamura et al., 2014; Wickens et al., 2016; Zhao et al., 2017). The proportion is even higher among repeat offenders (Jones and Lacey, 2000; Perrine, 1990). Meanwhile, problem drinking was also prevalent among alcohol-impaired drivers in fatal crashes (Baker and Chen, 2001; Baker et al., 2002; Voas et al., 2006; Wundersitz and Raftery, 2017). For example, Baker et al. (2002) found that 21% to 61% of drivers in fatal crashes were “problem drinkers” among those with blood alcohol concentrations (BACs) ⩾ .15 g/dl.
In comparison, the prevalence of alcohol problems (particularly AUDs) among the general driving public is much lower. A recent study on a national sample of weekend nighttime drivers on U.S. roads found that 14% of all current drinkers who drive could be classified as either alcohol dependent or abusive (Furr-Holden et al., 2011). Findings from studies in other countries are also similar, or suggest even lower proportions (Faller et al., 2012; Hubicka et al., 2007; Peltzer et al., 2010; Rio et al., 2001).
Therefore, drivers with problem drinking may seem to have a higher crash risk than normative social drinkers, as some researchers believed (Cavaiola and Wuth, 2002; Simpson et al., 1996). Other authors (e.g., Hedlund and Fell, 1995; Jones and Lacey, 2000, 1998), however, argued that “problem drinkers” only accounted for a small proportion of all fatal crashes. Largely, the lack of progress in this debate is caused by incomplete data on drinking characteristics of both drivers in crashes and not involved in crashes. To date, the risk of crash involvement for drivers with drinking problems has not been assessed through a theoretically sound study design, such as a case-control design employed in famous studies on alcohol-related crash risks (Blomberg et al., 2009; Borkenstein et al., 1974).
In order to conduct such needed research, it is first necessary to categorize drivers into different drinker types based on sound instruments. As mentioned earlier, many existing studies of drivers examined “problem drinkers” as one group, which could include drivers with heavy alcohol consumption only and those with clinical signs of AUDs instead. Such within-group variation made it impossible to distinguish the contribution to crashes of those who cannot control their drinking, from that of those with manageable heavy drinking. In fact, aggregate analyses at the state level by Voas et al. (2006) have shown an association between a state’s population of heavy drinkers or abusive drinkers (but not dependent drinkers) and the ratio of drivers in fatal crashes with high BACs (⩾ .15 g/dl). Furr-Holden et al. (2011) also found that only heavy drinking, but not alcohol abuse or dependence, were related to the presence of an illegal BAC (⩾ .08 g/dl). Therefore, it is necessary to separate drivers with AUDs from heavy drinkers, both of whom to be compared against normative drinking drivers.
Another limitation in prior research is the lack of data on drivers in non-fatal crashes. Given the challenge of making diagnoses of AUDs on fatal drivers, current understanding about drivers with AUDs will benefit from studies of drivers in crashes of all severity levels. In addition, more information on drivers at risk for crashes, matched with crash-involved drivers, is also needed for crash risk estimation. The Furr-Holden et al. study (2011) was the first one to collect AUD and heavy drinking data as well as actual BACs from drivers on the road (but not involved in crashes), followed by a similar roadside study in Brazil (Faller et al., 2012). Such detailed drinker characteristics data must be gathered from both crash-involved drivers and their comparisons, in order to quantify the relationship between drinker type and crash involvement.
1.1. Objectives
This study took advantage of the case-control alcohol and drug crash risk study in Virginia Beach, VA, sponsored by the National Highway Traffic Safety Administration (NHTSA) and the National Institute on Alcohol Abuse and Alcoholism. It examined the BACs and crash involvement of different drinker types among drivers, as measured by the same valid and reliable instrument adopted in the Furr-Holden et al. study (2011). The first research objective was to compare the relationship between driver BACs on the road and drinker types— drinkers with alcohol dependence, drinkers with alcohol abuse, heavy drinkers, and all other current (i.e., normative) drinkers. Crash-involved and non-crash-involved drivers were examined separately. The second objective was to understand the relative crash risks of drivers with AUDs, as compared to heavy drinkers and normative drinkers, taking into account the influence of BAC.
2. Methods
2.1. The Crash Risk Study Procedures
The crash risk study collected data from more than 3,000 crash-involved drivers and 6,000 control drivers (i.e., drivers not involved in a crash) in Virginia Beach, VA, over a 20-month period (2010–2011). A more detailed description of the methodology is available from NHTSA (Compton and Berning, 2015; Lacey et al., 2016). Research teams responded 24 hours a day, 7 days a week to crashes that were reported to the police. They traveled to crash sites to interview and collect biological samples (i.e., breath, oral fluid, or blood samples) from crash-involved drivers. Procedures were also developed for collecting data from drivers who were more seriously injured or who died and were transported to a hospital or morgue and those who were arrested for DUI and taken to a police station, as well as hit-and-runs. Overall, 33.6% of the crashes involved an injury (N = 886) or fatality (N = 15). Distributions of drivers in hospitals, fatalities, in jail/arrested, and hit-and-runs are displayed in Table 1. For comparison with each crash-involved driver who provided data for the study, the team returned to the crash site one week after each crash to randomly select and interview two non-crash-involved drivers on the same day of the week, at the same time of day, and in the same direction of travel as the original crash. Breath samples were used for measuring BACs for most of the drivers. BACs of those who did not provide breath samples were determined by oral fluid and/or blood samples, if provided. The procedures for the study were approved by the Pacific Institute for Research and Evaluation’s Institutional Review Board.
Table 1.
Attempts to collect data from crash-involved drivers in hospitals, fatalities, in jail/arrested, and hit-and-runs.
| Crash-Involved Drivers | ||
|---|---|---|
| Drivers transported to hospital | 729 | |
| Eligible | 393 | |
| Consented (percentage of eligible) | 362 | 92.1% |
| Fatalities | 18 | |
| Drivers transported to jail/arrested | 205 | |
| Eligible | 120 | |
| Consented (percentage of eligible) | 109 | 90.8% |
| Hit and run | 84 | |
| Hit and run (caught) | 42 | |
| Eligible | 27 | |
| Consented (percentage of eligible) | 24 | 88.9% |
2.2. Administration of the AUD Survey
Respondents who completed a general survey questionnaire were offered a $10 incentive to provide an oral fluid sample, and an additional $5 incentive to complete the 15-item AUD questionnaire while the oral fluid sample was collected. Only participants who were current drinkers and reported consuming alcohol in the past year were eligible for the AUD survey. The instrument combined the Alcohol Use Disorders Identification Test (AUDIT) consumption scale that measures heavy alcohol consumption, and the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS) instrument that diagnoses alcohol abuse and dependence. It should be noted that we used the AUDIT only to screen for non-clinical heavy drinking but not clinical AUDs, the latter being diagnosed by the AUDADIS instead. Both instruments have been proven to have high construct and criterion validity and test-retest reliability (Allen et al., 1997; Babor et al., 1992; Üstün et al., 1997). The details of the scales and categorization of drinkers are borrowed from the Furr-Holden et al. (2011) article as in Table 2 and explained below.
Table 2.
Fifteen-item version of the standard Alcohol Use Disorder and Associated Disabilities Interview Schedule diagnostic instrument used in 2007 National Roadside Survey (NRS)a
| AUDIT-C consumption items for measuring heavy drinking questions | ||||
| 1. In the past year, how often did you have a drink containing alcohol? | ||||
| Never (0) | monthly or less (1) | 2–4 times/month (2) | 2–3 times/week (3) | 4 or more times/week (4) |
| 2. In the past year, how many drinks containing alcohol did you have on a typical day when you were drinking? | ||||
| 1 or 2 (0) | 2–4 (1) | 5 or 6 (2) | 7–9 (3) | 10 or more (4) |
| 3. In the past year, how often did you have six (five for a woman) or more drinks on one occasion? | ||||
| Never (0) | less than monthly (1) | monthly (2) | weekly (3) | daily/almost daily (4) |
| AUDADIS alcohol abuse questionsa | ||||
| 4. Did your drinking often interfere with taking care of your home or family or cause you problems at work or school? | ||||
| 5. Did you more than once get into a situation while drinking or after drinking that increased your chances of getting hurt—like driving a car or other vehicle or using heavy machinery—after having had too much to drink? | ||||
| 6. Did you get arrested, held at a police station or have legal problems because of your drinking? | ||||
| 7. Did you continue to drink even though it was causing you trouble with your family of friends? | ||||
| AUDADIS dependence questionsa | ||||
| 8. Have you found that you have to drink more than you once did to get the effect you want? | ||||
| 9. Did you find that your usual number of drinks had less effect on you than it once did? | ||||
| 10. Did you more than once want to try to stop or cut down on your drinking, but you couldn’t do it? | ||||
| 11. Did you end up drinking more or drinking for a longer period than you intended? | ||||
| 12. Did you give up or cut down on activities that were important to you or gave you pleasure in order to drink | ||||
| 13. When the effects of alcohol were wearing off, did you experience some of the bad aftereffects of drinking—like trouble sleeping, feeling nervous, restless, anxious, sweating or shaking, or did you have seizures or sense things that weren’t really there? | ||||
| 14. Did you spend a lot of time drinking or getting over the bad aftereffects of drinking? | ||||
| 15. Did you continue to drink even though it was causing you to feel depressed or anxious or causing a health problem or making one worse? | ||||
All items prefaced with ‘In the last year’. AUDIT-C: Alcohol Use Disorder Identification Test-consumption. (Furr-Holden et al., 2011)
2.2.1. The AUDIT
The 10-item AUDIT has a brief three-item consumption scale (AUDIT-C) that is approximately equal in accuracy to the full AUDIT (Reinert and Allen, 2007).
2.2.1.1. Heavy Drinkers
The first three items on our survey instrument were derived from the AUDIT-C, each of which is scored on a scale from 0 to 4 (see Table 2). We used the standard scoring system which specifies that a score of 6 or more is the criterion for heavy drinking for men and a score of 5 or more is the criterion for women.
2.2.2. The AUDADIS
The AUDADIS is a comprehensive, fully structured diagnostic tool for alcohol abuse and dependence, supported by algorithms that generate International Classification of Disease–10th version (ICD-10) and DSM-IV AUDs. It has good correlations with the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) and with the Diagnostic Interview Schedule (DIS).
2.2.2.1. Abusive Drinkers
Items 4–7 on our survey were derived from the AUDADIS, which is constructed to have one item per DSM-IV symptom (see Table 2). A positive response to one or more of these items was the criterion for alcohol abuse in this study.
2.2.2.2. Dependent Drinkers
Items 8–15 were also taken from the AUDADIS (see Table 2). Three ‘yes’ responses to any of the seven symptoms of dependence (items 8 and 9 counting as one item which both relate to the domain of tolerance) were the criteria for alcohol dependence. If responses to four or more of the items were not provided, the case was scored as missing unless the three other available responses were ‘yes’.
In addition, some people might qualify for all three drinker types depending on their answers to the AUD survey; therefore, each category was created to be independent of the others based on the hierarchy: Dependent Drinkers > Abusive Drinkers > Heavy Drinkers. For example, individuals who qualify for both the dependence and abuse categories are classified as dependent and not included in the abuse classification.
2.2.2.3. Normative Drinkers
Respondents who qualified as current-year drinkers but who did not provide a response to the AUD survey that placed them in one of the three drinker categories were classified as normative drinkers. They served as a comparison group for the other drinking categories.
2.3. Data Analysis
We first examined the distribution of drinker types among all drivers, drivers who had a zero BAC, a moderate BAC (.05 g/dl or above), or an illegal BAC (.08 g/dl or above). Next, two sets of logistic regression analyses were conducted on two outcome variables separately: (1) having a moderate BAC and (2) being involved in a crash. We were able to calculate odds ratios (ORs) of each drinker type compared with normative drinkers and their 95% confidence intervals (CIs). Since the crash risk study collected data at any time of day, we added time of day as an independent variable, defining nighttime as the period between 9:00 p.m. and 3:00 a.m. This allowed for comparison with the nighttime sample of drivers from the 2007 National Roadside Survey (Furr-Holden et al., 2011). In both models, key demographic variables comparable to those in Furr-Holden et al.—including gender, age, race/ethnicity, employment status, and educational attainment—were adjusted for their influences. We also tested for interaction effects that were important for crash risk estimation.
It should be noted that our initial logistic regression modeling of the driver BAC outcome focused on an illegal BAC (.08 g/dl or above), for the purpose of direct comparison with the same model in the Furr-Holden et al. study (2011). Although results were generally reasonable with some anomaly, we were concerned about the very low numbers of drivers with an illegal BAC in our sample, particularly among control drivers (i.e., 5 dependent drinkers, 1 abusive drinkers, and 7 heavy drinkers), which could affect accuracy and reliability of model estimates. Therefore, we decided to run logistic regression analyses on the outcome of having a moderate BAC (.05 g/dl or above) instead.
2.3.1. Dependent Variable
Model 1: Having a moderate BAC (.05 g/dl or above) or not was the dependent measure.
Model 2: Being involved in a crash or not was the dependent measure.
2.3.2. Independent Variables
Model 1: Independent variables included drinker type, nighttime, crash involvement (i.e., crash-involved versus controls), gender, age, race/ethnicity, employment status, and educational attainment. Two significant interaction effects were kept in the final model, which were between drinker type and nighttime, and between drinker type and crash involvement.
Model 2: Independent variables included drinker type, driver BAC, nighttime, gender, age, race/ethnicity, employment status, and educational attainment. The interaction effect between drinker type and nighttime was significant and kept in the final model.
3. Results
3.1. Participation
As noted earlier, only participants who were current drinkers and reported consuming alcohol in the past year were eligible for the AUD survey (crash: 72.4%, control: 81.2%), leaving 2,411 crash-involved and 5,514 control drivers who provided useable data for this study (i.e., valid responses to the AUD questionnaire and BAC test results). Note that the final sample we analyzed is different from that reported by NHTSA (Compton and Berning, 2015), the latter based on the 1:2 case-control matching from oral fluid samples and the total number of 9,285 drivers instead. Table 3 shows the distribution of drinker types among crash-involved and control drivers. The proportion of drivers with AUDs was lower for the crash-involved drivers (8.7%) than for the control drivers (12.7%). An additional 6.9% of crash-involved drivers and 10.4% of control drivers displayed signs of heavy drinking.
Table 3.
Percentage of AUD, heavy, and normative drinkers among all current drinkers in relation to BACs
| Type of drinker | All current drinkers | Current drinkers with BAC = .00 | Current drinkers with BAC ≥ .05 | Current drinkers with BAC ≥ .08 |
|---|---|---|---|---|
| Crash drivers | (n = 2,411) | (n = 2,234) | (n = 123) | (n = 101) |
| Dependent (n = 77) | 3.2 | 2.6 | 12.2* | 13.9* |
| Abusive (n = 133) | 5.5 | 4.2 | 29.3* | 32.7* |
| Heavy (n = 167) | 6.9 | 6.5 | 10.6 | 9.9 |
| Normative (n = 2,034) | 84.4 | 86.7 | 48.0* | 43.6* |
| Control drivers | (n = 5,514) | (n = 5,320) | (n = 56) | (n = 27) |
| Dependent (n = 323) | 5.9 | 5.7 | 10.7 | 18.5* |
| Abusive (n = 376) | 6.8 | 6.6 | 10.7 | 3.7 |
| Heavy (n = 573) | 10.4 | 10.1 | 21.4* | 25.9* |
| Normative (n = 4,242) | 76.9 | 77.6 | 57.1* | 51.9* |
Note: Non-current-drinkers: crash drivers n = 965, control drivers n = 1329
Significant at α = 0.05, when compared with the rest of the current drinkers
3.2. Relationship between Drinker Categories and Driver BACs
Table 3 also relates the proportions of each drinker category to ascending BAC levels. As BAC increased, the proportions of drivers with non-normative drinking (i.e., with alcohol abuse, alcohol dependence, or heavy drinking) increased, but the patterns were different for crash-involved and control drivers. Drinkers with AUDs became overrepresented among crash-involved drivers with higher BACs (e.g., 12.2% were alcohol-dependent and 29.3% were alcohol-abusive among drivers with BACs at or above .05 g/dl), whereas there were significantly more heavy drinkers among control drivers with higher BACs (i.e., 21.4%).
After adjusting for the influences of covariates in the logistic regression model (i.e., Model 1) in Table 4, the odds ratios of having a moderate BAC are presented in Table 4a for each drinker category compared with normative drinkers. The results are similar to those from the BAC .08 model we initially ran. All three non-normative drinker categories—heavy, abusive, and dependent drinkers—were overrepresented among crash-involved drivers with a moderate BAC, regardless of time of day (except heavy drinkers in the daytime). In comparison, among nighttime control drivers on the road, only heavy drinkers, but not abusive or dependent drinkers, were more likely to have moderate BACs (OR = 4.28, 95% CI = [1.86, 9.81]). Dependent drinkers among daytime control drivers, on the other hand, were more likely to have moderate BACs (OR = 3.31, 95% CI = [1.18, 9.29]). In addition, demographic variables such as gender and age were statistically significant. For example, female drivers were less likely to have moderate BACs (OR = 0.62, 95% CI= [0.44, 0.89]).
Table 4.
Logistic regression results for analysis of AUD and moderating variables relationships to drivers with BACs ≥ .05
| Total n = 7,804 | OR for BAC ≥ .05 | 95% CI for OR | |
|---|---|---|---|
| Crash driver (n = 2,373) | See Table 4a | ||
| Reference: Control driver (n = 5,431) | |||
| Nighttime (n = 838) | See Table 4a | ||
| Reference: Daytime (n = 6,966) | |||
| Women (n = 3,711) | 0.62* | 0.44 | 0.89 |
| Reference: Men (n = 4,093) | |||
| Age group (years) | |||
| 21–34 years (n = 3230) | 2.10* | 1.14 | 3.87 |
| 35–44 years (n = 1482) | 0.79 | 0.35 | 1.82 |
| 45+ years (n = 2481) | 1.27 | 0.64 | 2.54 |
| Reference: <21 years (n = 611) | |||
| Race/ethnicity | |||
| Black or African American (n = 1,290) | 1.24 | 0.78 | 1.97 |
| Hispanic (n = 443) | 1.01 | 0.53 | 1.93 |
| Other (n = 545) | 1.18 | 0.66 | 2.11 |
| Reference: White (n = 5,526) | |||
| Education level | |||
| Did not graduate high school (n = 336) | 0.33* | 0.12 | 0.92 |
| Some college/college degree (n = 5,682) | 0.74 | 0.51 | 1.07 |
| Reference: High school graduate (n = 1,786) | |||
| Employment status | |||
| Unemployed (n = 655) | 0.998 | 0.54 | 1.85 |
| Other (n = 581) | 1.33 | 0.61 | 2.90 |
| Reference: Employed (n = 6,568) | |||
| AUD category | |||
| Dependent (n = 391) | See Table 4a | ||
| Abusive (n = 503) | |||
| Heavy (n = 734) | |||
| Reference: Normative (n = 6,176) | |||
| Interaction** | |||
| Case × Dependent | 1.16* | N/A | |
| Case × Abusive | 1.79* | ||
| Case × Heavy | −0.38 | ||
| Nighttime × Dependent | −1.12* | ||
| Nighttime × Abusive | 0.33 | ||
| Nighttime × Heavy | 0.96 | ||
Significant at α = 0.05
Parameter estimates were shown for interaction effects, since odds ratios were not applicable. CI = Confidence Interval; OR = Odds Ratio
Table 4a.
Odds ratios for BAC >= 0.05 for each drinker category.
| Crash | Control | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nighttime (n = 262) | Daytime (n = 2,111) | Nighttime (n = 576) | Daytime (n = 4,855) | |||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| Dependent | 3.45* | 1.22 | 9.73 | 10.60* | 4.88 | 23.03 | 1.08 | 0.36 | 3.23 | 3.31* | 1.18 | 9.29 |
| Abusive | 13.98* | 6.01 | 32.51 | 10.05* | 5.20 | 19.42 | 2.34 | 0.87 | 6.30 | 1.68 | 0.57 | 4.99 |
| Heavy | 2.94* | 1.30 | 6.65 | 1.13 | 0.41 | 3.11 | 4.28* | 1.86 | 9.81 | 1.64 | 0.60 | 4.52 |
| Reference: Normative | ||||||||||||
Significant at α = 0.05
CI = Confidence Interval; OR = Odds Ratio
3.3. Crash Risks of Each Drinker Category
The relative risks of crash involvement for each drinker category were estimated by the logistic regression model in Table 5 (i.e., Model 2), when BAC and other factors were held constant. Not surprisingly, crash risk increased significantly as driver BAC increased, and drivers younger than 21 years had the highest crash risk among all age groups. A key result is that drinker type also made a significant contribution to drivers’ likelihood of crashing, after the influences of BAC and other covariates were accounted for. According to Table 5a, the three non-normative drinker types had different odds of crash involvement, which also varied from day to night. The odds of being involved in a nighttime crash were essentially the same for abusive and heavy drinkers compared to normative drinkers, but dependent drinkers demonstrated a much lower crash risk than normative drinkers (OR = 0.37, 95% CI = [0.18, 0.77]). On the other hand, all three non-normative drinker types were less likely to crash during the daytime, with significant odds ratios all lower than 1 (i.e., 0.36, 0.52, and 0.50 respectively for dependent, abusive and heavy drinkers).
Table 5.
AUD and Crash Involvement
| Total n = 7,804 | OR for Crash | 95% CI for OR | ||
|---|---|---|---|---|
| AUD category | See Table 5a | |||
| Dependent (n = 391) | ||||
| Abusive (n = 503) | ||||
| Heavy (n = 734) | ||||
| Reference: Normative (n = 6,176) | ||||
| Nighttime (n = 838) | ||||
| Reference: Daytime (n = 6,966) | ||||
| Interaction*** | ||||
| Nighttime × Dependent | 0.03 | N/A | ||
| Nighttime × Abusive | 0.49 | |||
| Nighttime × Heavy | 0.60* | |||
| BAC | ** | ** | ** | |
| Women (n = 3,711) | 1.00 | 0.91 | 1.11 | |
| Reference: Men (n = 4,093) | ||||
| Age group (years) | ||||
| 21–34 years (n = 3,230) | 0.64* | 0.53 | 0.77 | |
| 35–44 years (n = 1,482) | 0.43* | 0.35 | 0.53 | |
| 45+ years (n = 2,481) | 0.46* | 0.38 | 0.56 | |
| Reference: <21 years (n = 611) | ||||
| Education level | ||||
| Did not graduate high school (n = 336) | 1.35* | 1.04 | 1.73 | |
| Some college/college degree (n = 5,682) | 1.01 | 0.89 | 1.14 | |
| Reference: High school graduate (n = 1,786) | ||||
| Employment status | ||||
| Unemployed (n = 655) | 1.19 | 0.99 | 1.41 | |
| Other (n = 581) | 0.99 | 0.82 | 1.21 | |
| Reference: Employed (n = 6,568) | ||||
| Race/ethnicity | ||||
| Black or African American (n = 1,290) | 0.73* | 0.63 | 0.84 | |
| Hispanic (n = 443) | 0.95 | 0.76 | 1.18 | |
| Other (n = 545) | 1.26* | 1.04 | 1.52 | |
| Reference: White (n = 5,526) | ||||
Significant at α = 0.05
BAC is modeled as a continuous variable and significant, but the odds ratio for each 1 unit of increase is extremely high and therefore not shown in the table.
Parameter estimates were shown for interaction effects, since odds ratios were not applicable. CI = Confidence Interval; OR = Odds Ratio
Table 5a.
Odds ratios for crash for each drinker category.
| Nighttime (n = 838) | Daytime (n = 6,966) | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Dependent | 0.37* | 0.18 | 0.77 | 0.36* | 0.27 | 0.49 |
| Abusive | 0.84 | 0.47 | 1.53 | 0.52* | 0.41 | 0.66 |
| Heavy | 0.90 | 0.52 | 1.57 | 0.50* | 0.41 | 0.61 |
| Reference: Normative | ||||||
Significant at α = 0.05
CI = Confidence Interval; OR = Odds Ratio
In addition, separate regression models (using different drinker categories as the reference level) found the odds of being involved in a nighttime crash to be significantly lower for dependent drinkers than heavy drinkers (OR = 0.41, 95% CI = [0.17, 0.98]). This is consistent with earlier results, in which heavy drinkers with moderate or high BACs were more likely to be on the road at nighttime than dependent drinkers. Heavy drinkers in the daytime, on the other hand, tended to have lower BACs and thus a lower likelihood of crashing. A closer look at the proportions of drinker types among crashes by time clearly indicates this day-night difference among heavy drinkers (Figure 1). The percentage of heavy drinkers among crashes witnessed a very high rise during the late evening period (9:00 p.m. to 3:00 a.m.) when alcohol impairment plays a large role (National Highway Traffic and Safety Administration, 2016). By contrast, normative drinkers were more likely to crash during the daytime, particularly during rush hours, when traffic volume is a significant contributor to crash involvement. Percentages of normative drinkers among crashes remained stable throughout the day and then dropped at night.
Figure 1.
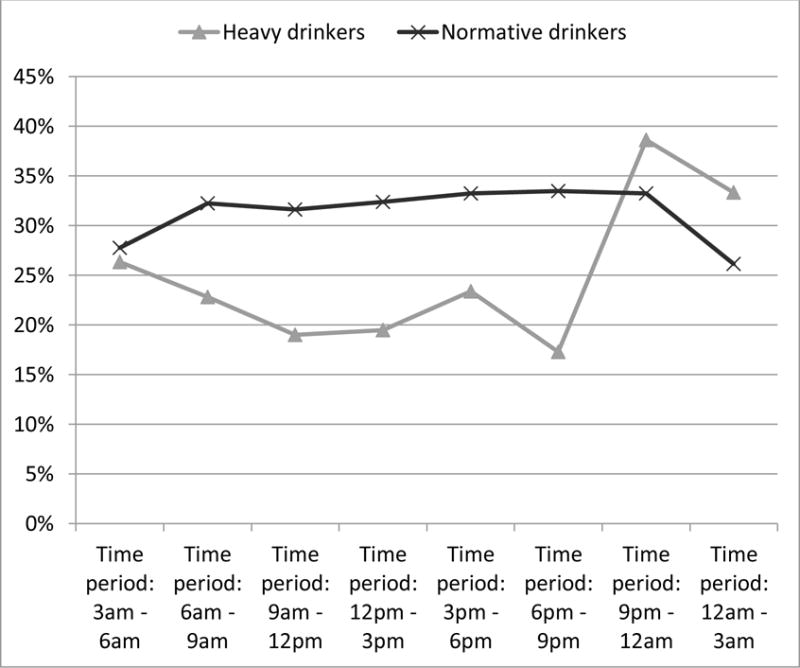
Comparison of proportions of heavy drinkers and normative drinkers by time of crash.
4. Discussion
This study took advantage of the four available driver samples with BAC data—daytime crash-involved drivers, nighttime crash-involved drivers, daytime control drivers, and nighttime control drivers, which allowed for analysis of the relationship between driver BAC and drinker type and for direct comparisons with different groups in previous studies. Consistent with prior research on drivers in fatal crashes (Baker and Chen, 2001; Baker et al., 2002), drivers in nonfatal crashes with signs of problem drinking—heavy, abusive, or dependent drinkers—are also found more likely to have moderate to high BACs. The only exception is heavy drinkers in daytime crashes, who are not different from normative drinking drivers in terms of alcohol prevalence. Regarding drivers not involved in crashes, findings of this study were similar to those of Furr-Holden et al. (2011), which found that one in four current drinkers could be classified as a non-normative drinker; this study reported 23%. More important, both studies found that nighttime drivers with higher BACs do not necessarily display signs of alcohol abuse or dependence, but tend to be heavy drinkers that have not yet met clinical criteria for an AUD.
An important finding related to the second research objective is that, when BAC was controlled, dependent drinkers had significantly lower odds of being involved in a crash than normative drinkers, regardless of time of day. This is probably due to the lower likelihood of dependent drivers on the road, given other alcohol-related problems they tend to have (e.g., unemployment, loss of a driver’s license, limited social life) (Joutsenniemi et al., 2007; Pilowsky et al., 2013; Zemore et al., 2017). On the other hand, heavy drinkers in the daytime were less likely to crash than normative drinkers, but as their drinking activities increased notably at night, particularly late at night, their likelihood of crash involvement would elevate (shown in Figure 1).
It should be noted that as a result of having research teams on the road 24/7, two thirds (66.4%) of crashes covered in the study were property-damage-only crashes, which are typical under congested driving conditions in the daytime and tend to be unrelated to alcohol. At most, 13% of the crashes (n = 159) in this study could be classified as alcohol-related (defined as a crash that involved at least one driver with a positive BAC). If BAC .05 g/dl or .08 g/dl was used as the cutoff criterion, the percentage of alcohol-related crashes became even lower (10% and 8%, respectively). Therefore, daytime, rush hours, and other crowded road conditions may have played a large role in the crashes studied, where alcohol is typically less likely to be a factor for low-severity, property-damage-only crashes. It is then not surprising to see that both drivers with AUDs and those who reported heavy drinking were less likely to be involved in a daytime crash than normative drinkers.
This study is the first empirical study to determine the relative crash risks of drivers with AUDs using a case-control design, the most theoretically sound study design for crash risk estimation (Houwing et al., 2012). It suggests that drivers with AUDs are not necessarily more likely to be involved in a crash, and the risk of crash involvement for alcohol-dependent drivers might indeed be lower than normative drinkers. Meanwhile, drivers with heavy drinking who have not met the DSM-IV criteria of alcohol abuse and dependence are more at risk for driving with high BACs at nighttime, which can greatly increase their chances of being involved in alcohol-related crashes.
This study provides empirical evidence that may further illuminate the debate on different approaches to the drinking and driving problem, i.e., whether to allocate resources to targeted programs aimed at clinically significant cases, or to the much larger number of normative and heavy drinkers in the general public, or both. This study suggests that the contribution of drivers with AUDs to crash occurrence might have been overstated, and further research is needed that focuses on alcohol-related crashes with injuries rather than small crashes leading to property damage only.
4.1. Limitations
In addition to an inadequate number of alcohol-related crashes examined, another limitation of this study is bias from self-reported answers, particularly when private or sensitive information is collected. Given the contexts at the crash site and possible concerns about legal consequences related to alcohol misuse, some drivers with alcohol problems could have provided dishonest answers to the AUD instrument, although the extent of this bias is hard to assess. In fact, the unexpected lower odds of crash involvement for drivers with AUDs and heavy drinkers in the daytime might be partly related to the fact that crash-involved drivers could have under-reported their alcohol use problems. We tried to minimize response bias through stringent research protocols, but more work is needed to ensure honest and accurate answers (e.g., Loughran et al., 2014).
This study was limited to drivers who were current drinkers in one US city. Therefore, the findings might not be representative of the US national driving population, and regional variation might exist. Such concerns are partially addressed by comparing with the national sample of drivers in Furr-Holden et al. (2011) and achieving similar results. The sample used in this study was also comparable to samples in prior studies on alcohol-related crash risk, as NHTSA (Compton and Berning, 2015) compared the relative crash risks by BAC level with the relative risk curve from the study in Blomberg et al. (2009) and found no significant difference between the studies. In addition, other limitations of the study might include inadequate information on injury severity of drivers, leaving out one or more significant factors affecting crash likelihood such as exposure (i.e., vehicle miles travelled), diagnostic accuracy of the AUDADIS instrument on the roadside instead of in clinical settings, and so on. Future research that addresses such concerns will help refine the crash risk estimates for drivers with AUDs.
Highlights.
Blood Alcohol Content (BAC) and crash involvement were influenced by drinking characteristics of drivers.
Heavy drinkers were more likely to drive at night with higher BACs.
Alcohol-dependent drinkers were less likely to be involved in a nighttime crash.
Daytime crashes were more likely to involve normative drinkers.
Acknowledgments
Role of Funding
This study was funded by the National Institute on Alcohol Abuse and Alcoholism (R01 AA018352) and made possible by the cooperation of the National Highway Traffic Safety Administration in the collection of data during its study: Drug and Alcohol Crash Risk: A Case-Control Study (DOT HS 812 355).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Jie Yao, Ph.D., was responsible for the management of the data system and the data analysis and was the principle author of the paper. Robert B. Voas, Ph.D., was the Principal Investigator for the grant and developed the research plan and a secondary author of the article. John H. Lacey, M.P.H., was project director for the companion relative risk study funded by NHTSA that was responsible for the collection of the data. All authors on this paper have approved of the final manuscript before submission.
Conflict of Interest
None.
References
- Allen JP, Litten RZ, Fertig JB, Babor T. A review of research on the Alcohol Use Disorders Identification Test (AUDIT) Alcohol Clin Exp Res. 1997;21:613–619. [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. World Health Organization; Geneva: 1992. [Google Scholar]
- Baker SP, Braver ER, Chen LH, Li G, Williams AF. Drinking histories of fatally injured drivers. Inj Prev. 2002;8:221–226. doi: 10.1136/ip.8.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker SP, Chen LH. DOT HS 809 380. U.S. Department of Transportation, National Highway Traffic Safety Administration; Washington, DC: 2001. Determination of Characteristics of Fatally Injured Drivers. Available from http://ntl.bts.gov/lib/18000/18800/18856/PB2002102279.pdf. [Google Scholar]
- Bergman H, Hubicka B, Laurell H. Alcohol problems and blood alcohol concentration among Swedish drivers suspected of driving under the influence. Contemp Drug Prob. 2005;32:387–404. [Google Scholar]
- Blomberg RD, Peck RC, Moskowitz H, Burns M, Fiorentino D. The Long Beach/Fort Lauderdale relative risk study. J Saf Res. 2009;40:285–292. doi: 10.1016/j.jsr.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Borkenstein RF, Crowther RF, Shumate RP, Ziel WB, Zylman R. The role of the drinking driver in traffic accidents. Blutalkohol. 1974;11:1–132. [Google Scholar]
- Cavaiola AA, Wuth C. Assessment and Treatment of the DWI Offender. Haworth Press; New York: 2002. [Google Scholar]
- Compton RP, Berning A. Traffic Safety Facts Research Note DOT HS 812 117. National Highway Traffic Safety Administration; Washington, DC: 2015. Drug and Alcohol Crash Risk. [Google Scholar]
- Faller S, Webster JM, Leukefeld CG, Bumaguin DB, Duarte PV, Boni RD, Pechansky F. Psychiatric disorders among individuals who drive after the recent use of alcohol and drugs. Revista Brasileira De Psiquiatria. 2012;34:314–320. doi: 10.1016/j.rbp.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Fell JC. Update: Repeat DWI offenders involvement in fatal crashes in 2010. Traff Inj Prev. 2014;15:431–433. doi: 10.1080/15389588.2013.838230. [DOI] [PubMed] [Google Scholar]
- Fell JC, Tippetts S, Voas R. Drinking characteristics of drivers arrested for driving while intoxicated in two police jurisdictions. Traff Inj Prev. 2010;11:443–452. doi: 10.1080/15389588.2010.488274. [DOI] [PubMed] [Google Scholar]
- Furr-Holden CD, Voas RB, Lacey J, Romano E, Jones K. The prevalence of alcohol use disorders among night-time weekend drivers. Addiction. 2011;106:1251–1260. doi: 10.1111/j.1360-0443.2011.03408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedlund J, Fell J. Persistent drinking drivers in the U.S. Ann Adv Automotive Med. 1995;39:1–12. [Google Scholar]
- Houwing S, Mathijssen R, Brookhuis K. In search of a standard for assessing the crash risk of driving under the influence of drugs other than alcohol: Results of a questionnaire survey among researchers. Traff Inj Prev. 2012;13:554–565. doi: 10.1080/15389588.2012.663118. [DOI] [PubMed] [Google Scholar]
- Hubicka B, Bergman H, Laurell H. Alcohol problems among Swedish drunk drivers: Differences related to mode of detection and geographical region. Traff Inj Prev. 2007;8:224–231. doi: 10.1080/15389580701426322. [DOI] [PubMed] [Google Scholar]
- Jones RK, Lacey JH. DOT HS 809 383. National Highway Traffic Safety Administration; Washington, DC: 2002. Alcohol and Highway Safety 2001: A Review of the State of Knowledge. [Google Scholar]
- Jones RK, Lacey JH. DOT HS 809 027. National Highway Traffic Safety Administration; Washington, DC: 2000. State of Knowledge of Alcohol-impaired Driving: Research on Repeat DWI Offenders. [Google Scholar]
- Joutsenniemi K, Martelin T, Kestilä L, Martikainen P, Pirkola S, Koskinen S. Living arrangements, heavy drinking and alcohol dependence. Alcohol Alcohol. 2007;42:480. doi: 10.1093/alcalc/agm011. [DOI] [PubMed] [Google Scholar]
- Lacey JH, Kelley-Baker T, Berning A, Romano E, Ramirez A, Yao J, Moore C, Brainard K, Carr K, Pell K, Compton R. DOT HS 812 355. National Highway Traffic Safety Administration; Washington, DC: 2016. Drug and Alcohol Crash Risk: A Case-control Study. [Google Scholar]
- Lapham SC, C’de Baca J, McMillan G, Hunt WC. Accuracy of alcohol diagnosis among DWI offenders referred for screening. Drug Alcohol Depend. 2004;76:135–141. doi: 10.1016/j.drugalcdep.2004.04.020. [DOI] [PubMed] [Google Scholar]
- Loughran TA, Paternoster R, Thomas KJ. Incentivizing responses to self-report questions in perceptual deterrence studies: An investigation of the validity of deterrence theory using bayesian truth serum. J Quant Criminol. 2014;30:677–707. [Google Scholar]
- Moskowitz H, Fiorentino D. DOT HS 809 208. National Highway Traffic Safety Administration; Washington, DC: 2000. A Review of the Literature on the Effects of Low Doses of Alcohol on Driving Related Skills. [Google Scholar]
- National Highway Traffic and Safety Administration. DOT HS 812 350. Department of Transportation; Washington, DC: 2016. Traffic Safety Fact Sheet - Alcohol Impaired Driving. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. National epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2004;74:223–234. [Google Scholar]
- Okamura K, Kosuge R, Kihira M, Fujita G. Typology of driving-under-the-influence (DUI) offenders revisited: Inclusion of DUI-specific attitudes. Addict Behav. 2014;39:1779–1783. doi: 10.1016/j.addbeh.2014.07.007. [DOI] [PubMed] [Google Scholar]
- Peltzer R, Cremonte M, Ubeda C, Ledesma R. Drinking and driving, and alcohol drinking patterns in Argentinean drivers. Inj Prev. 2010;16:A126. [Google Scholar]
- Perrine MW. Who are the drinking drivers? The spectrum of drinking drivers revisited. Alcohol Health Res World. 1990;14:26–35. [Google Scholar]
- Pilowsky DJ, Keyes KM, Geier TJ, Grant BF, Hasin DS. Stressful life events and relapse among formerly alcohol dependent adults. Soc Work Ment Health. 2013;11:184–197. doi: 10.1080/15332985.2012.711278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test: An update of research findings. Alcohol Clin Exp Res. 2007;31:185–199. doi: 10.1111/j.1530-0277.2006.00295.x. [DOI] [PubMed] [Google Scholar]
- Rio MC, Gonzalez-Luque JC, Alvarez FJ. Alcohol-related problems and fitness to drive. Alcohol Alcohol. 2001;36:256–261. doi: 10.1093/alcalc/36.3.256. [DOI] [PubMed] [Google Scholar]
- Robertson R, Simpson H, Parsons P. Screening, Assessment and Treatment of DWI Offenders: A Guide for Justice Professionals and Policy Makers. Traffic Injury Research Foundation; Ottawa, Ontario: 2008. Available from http://www.alcoholandcrime.org/images/uploads/pdf_research/screening_tirf_2008.pdf. [Google Scholar]
- Simpson HM, Mayhew DR, Beirness DJ. Dealing with the hard core drinking driver. Traffic Injury Research Foundation; Ottawa, Canada: 1996. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD: 2008. [Google Scholar]
- Üstün B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Gogus A, Mavreas V, Peters L, Pull C, Saunders J, Smeets R, Stipec MR, Vrasti R, Hasin D, Room R, Van den Brink W, Regier D, Blaine J, Grant BF, Sartorius N. WHO study on the reliability and validity of the alcohol and drug use disorder instruments: Overview of methods and results. Drug Alcohol Depend. 1997;47:161–169. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- Voas RB, Romano EO, Tippetts AS, Furr-Holden CDM. Drinking status and fatal crashes: Which drinkers contribute most to the problem? J Stud Alcohol. 2006;67:722–729. doi: 10.15288/jsa.2006.67.722. [DOI] [PubMed] [Google Scholar]
- Wickens CM, Flam-Zalcman R, Mann RE, Stoduto G, Docherty C, Thomas RK. Characteristics and predictors of recidivist drink-drivers. Traff Inj Prev. 2016;17:564–572. doi: 10.1080/15389588.2015.1125477. [DOI] [PubMed] [Google Scholar]
- Williams AF, McCartt AT, Ferguson SA. Hardcore drinking drivers and other contributors to the alcohol-impaired driving problem: Need for a comprehensive approach. Traff Inj Prev. 2007;8:1–10. doi: 10.1080/15389580600992895. [DOI] [PubMed] [Google Scholar]
- Wundersitz L, Raftery S. Understanding the context of alcohol impaired driving for fatal crash-involved drivers: A descriptive case analysis. Traff Inj Prev. 2017:1–7. doi: 10.1080/15389588.2017.1322696. https://doi.org/10.1080/15389588.2017.1322696. [DOI] [PubMed]
- Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: An update using 1996 data. J Stud Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Mulia N, Williams E, Gilbert PA. Job loss and alcohol dependence among Blacks and Whites in a National Longitudinal Survey. J Ethn Subst Abuse. 2017;16:314–327. doi: 10.1080/15332640.2016.1209144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao R, Sun W, Zhang L, Bao Y, Huang L, Dong P, Zhou S, Wang Z, Kosten T, Sun H. Psychopathology and personality traits associated with driving while intoxicated in Beijing, China: Implications for interventions. Am J Addict. 2017;26:374–378. doi: 10.1111/ajad.12536. [DOI] [PubMed] [Google Scholar]


