Abstract
Background
By 2030, numbers and proportions of older adults with substance-use problems are expected to increase. While risk factors for problem drinking in late life have been identified, it remains unknown whether these factors drive daily drinking among older problem drinkers. This study examined the daily drivers of drinking among problem drinkers, moderated by age, utilizing ecological momentary assessment (EMA).
Method
Participants (N=139), ages 20–73, received daily EMA online surveys completed via a smartphone prior to initiation of treatment. Multilevel modeling tested the moderating impact of age on within- and between-person relationships between drinking and focal predictors (mood, loneliness, boredom, stress, poor sleep, social factors, alcohol salience, commitment and confidence not to drink heavily).
Results
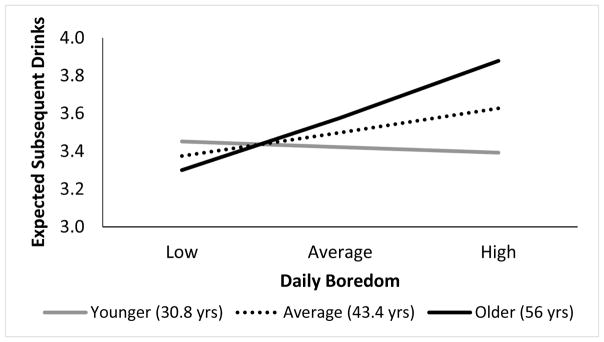
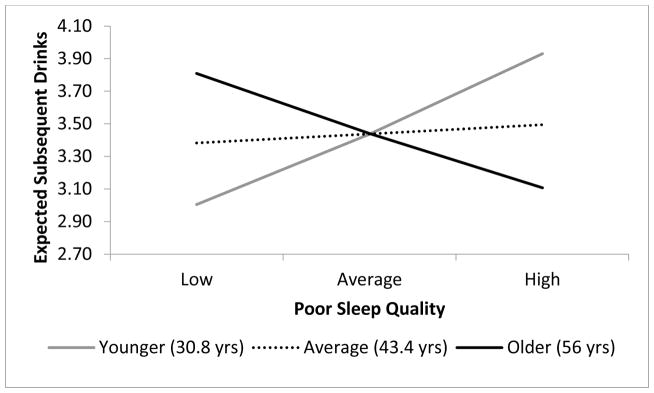
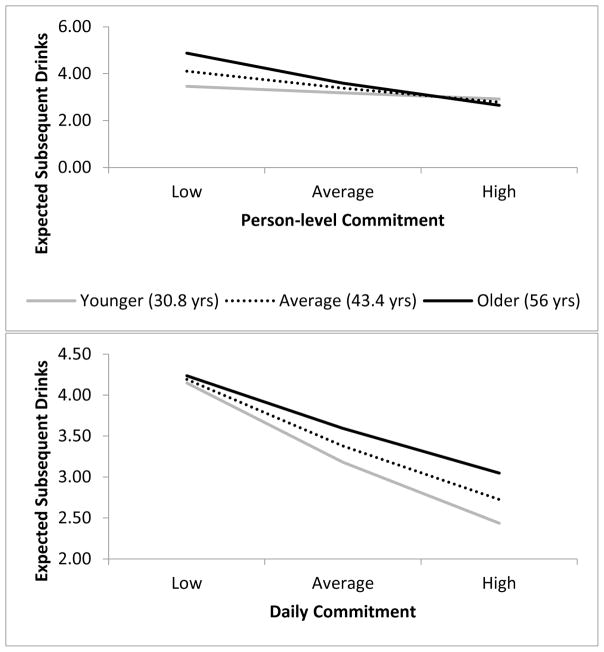
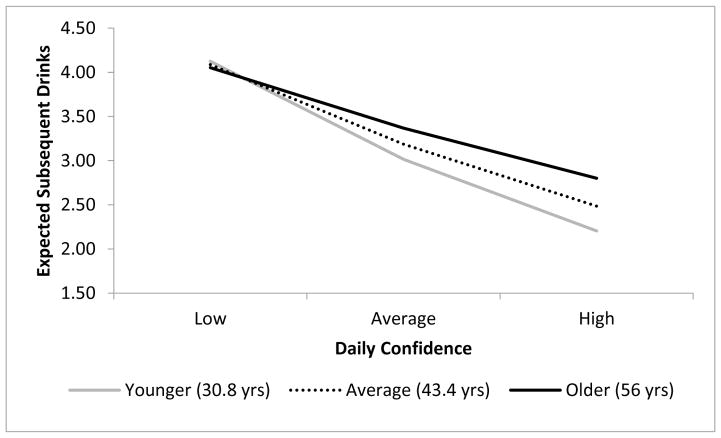
Older adults reported greater alcohol consumption when daily boredom levels were higher. Heavier drinking among younger adults was associated with poorer sleep quality. Greater daily confidence, daily commitment and daily alcohol salience did not impact drinking to the same extent for older adults as for younger adults. Greater person-level commitment predicted reduced drinking equivalently across age, but low person-level commitment predicted greater drinking among older adults compared to their younger counterparts.
Conclusion
Older adults may have unique daily drivers of drinking that are not fully realized in current research and intervention efforts. Addressing the growing substance-use treatment needs among this population will require identifying the unique drivers of drinking among older adults, such as boredom, when compared to younger adults.
Keywords: older adults, ecological momentary assessment, problem drinking, risk factors, self-efficacy, motivation
1. Introduction
As Baby Boomers (born 1946–1964) age, the number of older adults in the United States will almost double between 2010 and 2030 (Institute of Medicine, 2012). In this context, both numbers and proportions of older adults with substance use problems are expected to increase (Han et al., 2009). Unlike preceding generations, prevalence rates of substance use remain high among Baby Boomers as they age (Moore et al., 2009; Substance Abuse and Mental Health Services Administration, 2013). Thus, there is a growing public health challenge of how to better identify, assess, and treat alcohol and substance use and abuse among this population (Institute of Medicine, 2008, 2012).
Alcohol remains the most commonly used substance among middle-aged and older adults (Arndt et al., 2011; Moore et al., 2009). Middle-aged and older adults who drink more than the recommended guidelines for healthy alcohol consumption (e.g., males < 65: < 14 standard drinks per week, < 4 on one occasion; for males > 65 and females: < 7 standard drinks, < 3 on one occasion (National Institute on Alcohol Abuse and Alcoholism, 2013) are quite prevalent. Among adults 50 and older who completed the 2014 National Survey on Drug Use and Health, 14.9% reported drinking more than these recommended amounts, and 3.7% endorsed criteria for alcohol use disorder (AUD)—a significant increase from 12.5% and 3.0%, respectively, in 2005 (Han et al., 2017).
Aging-related biological changes in the body and brain that start around age 50 can increase one’s vulnerability to the deleterious effects of alcohol (Hanson, 2011; Oslin and Mavandadi, 2009). As one ages, there is an increased health risk of drinking with both medical conditions (e.g., hypertension, depression) and associated prescription medications, for which alcohol may be contraindicated (Moore et al., 2007). These risk factors can lead to loss of independence, increased falls, increased hospitalizations and reduced length and quality of life for these individuals (Moore et al., 2007; Sacco et al., 2015b). Thus, there is growing urgency to better understand potentially unique aspects of substance use and misuse among those 50 and older compared to their younger counterparts in order to best prevent and treat those at risk for harm (Institute of Medicine, 2008, 2012) among this group.
1.1 Factors Associated with Older Adult Problem Drinking
Life events and social transitions common in late life are thought to be risk factors for hazardous (greater than recommended guidelines) drinking and AUD in later life (Moore et al., 2017). For example, bereavement, ill health, loneliness, caregiving for an ill spouse, forced changes in living arrangements, retirement or loss of occupation are associated with hazardous alcohol use among middle-aged and older adults (Brennan et al., 1999; Center for Substance Abuse Treatment, 1998; Myers and Harper, 2004). The few treatment-based studies of middle-aged and older adults found continued and/or relapse to hazardous drinking was associated with: depressed mood, loneliness, boredom, stress, sleep problems, and social pressure (Blow et al., 2000b; Carstensen et al., 1985; Dupree et al., 1984; Schonfeld et al., 2000). Epidemiological studies recruiting from the community or primary care also found that depressed mood, loneliness, boredom, stress, sleep problems, and social factors were predictors or correlates of problem drinking in middle to late life (Adlaf and Smart, 1995; Blow et al., 2000a; Borok et al., 2013; Brennan et al., 1999; Christopherson et al., 1984; Kuerbis and Sacco, 2012; Moos et al., 1990; Moos et al., 2010a, b; Schonfeld et al., 2010).
While these existing studies provide important foundational knowledge, study limitations prevent generalization to today’s middle-aged and older adult population. A majority of studies were not implemented with Baby Boomers, a cohort known to have distinct, more permissive attitudes toward substance use compared to previous generations; and a majority of the treatment study samples were all male (e.g., Blow et al., 2000b). In addition, all studies excluded constructs central to theories of behavior change and treatment: motivation, self-efficacy (Kuerbis et al., 2013; Morgenstern et al., 2016), and alcohol salience, defined as the prominence of alcohol cues and/or availability (Witteman et al., 2015). Given that older hazardous drinkers are suspected to have long entrenched patterns of alcohol use, older adults are thought to have lower motivation, lower self-efficacy, and a lower threshold for responding to alcohol salience (e.g., exposure to drinking contexts) compared to younger counterparts with presumably shorter relationships with alcohol (Center for Substance Abuse Treatment, 1998; Sjoerds et al., 2014). Past failures among older adults to change behavior may cause differentially low self-efficacy to change patterns of drinking and may then impact motivation to implement behavior change.
Finally, all of the aforementioned studies evaluated risk factors in aggregate—how overall levels of risk factors influence overall levels of drinking. Virtually nothing is known about the day-to-day influences on drinking among middle-aged and older adults. For example, while drinkers aged 50+ with higher levels of depression or loneliness may drink more regularly or heavily, they may be less apt to drink on days when feeling particularly depressed or lonely. Understanding what drives daily drinking for middle-aged and older adults compared to younger adults is important for optimal prevention and intervention.
1.2 Use of Ecological Momentary Assessment with Middle-aged and Older Adults
One way to better understand daily predictors of drinking is to utilize ecological momentary assessment (EMA) to study dynamic patterns of behavior over time. EMA is a methodology defined as “repeated collection of real-time data on subjects’ behavior and experience in their natural environment” (Shiffman et al., 2008), in which constructs are assessed daily (or more frequently). While studies using EMA with older adults exist (e.g., Sacco et al., 2015a; Steptoe and Wardle, 2011), EMA has not been widely used among middle-aged and older adults in relation to alcohol use. Older adults are often excluded from studies focusing on AUD that use EMA due to age-related exclusion criterion or persistent stereotypes that older adults are unwilling or unable to engage with mobile technology (Kuerbis et al., 2017).
1.3 The Current Study
This study used secondary data analysis to test whether age moderated relationships between daily- and person-level focal predictors (specifically, mood, loneliness, boredom, stress, poor sleep, social factors, commitment not to drink heavily, confidence not to drink heavily, and alcohol salience) and drinking among problem drinkers aged 20 to 73. It was hypothesized that age would significantly moderate the previously identified risk factors for drinking in later life—such that older age would interact with lower mood, greater loneliness, more boredom, more stress, poorer quality sleep, lower pro-drinking social influence, and less alcohol salience to predict greater drinking. It was also hypothesized that commitment and confidence would not impact drinking as strongly for older adults as for younger adults.
2. Method
Data was collected during a week of baseline assessment prior to the start of a randomized controlled trial with problem drinkers (Morgenstern et al., 2016). All procedures were approved by the Institutional Review Board.
2.1 Participants
Participants seeking treatment to reduce but not stop drinking were recruited using advertising online and in local media. Prospective participants were screened by phone and, if eligible, scheduled for an in-person screening assessment. Participants were eligible if they: (1) were age 18 to 75; (2) consumed an estimated weekly average > 15 or 24 standard drinks per week, for women and men respectively, and (3) had a current AUD. Participants were excluded if they had: (1) a substance use disorder or were regular (greater than weekly) drug users; (2) a serious psychiatric disorder or suicide or violence risk; (3) physical withdrawal symptoms or a history of serious withdrawal symptoms; (4) a legal mandate to substance abuse treatment; (5) social instability (e.g., homeless); (6) a desire to achieve abstinence at baseline; or (7) a desire or intent to pursue additional substance abuse treatment during the treatment period.
2.2 Procedures
For the in-person screening assessment, participants were asked to complete a series of standard, global self-report assessments. Afterwards, participants were asked to complete a daily online survey via a smartphone, once in the morning and once in the evening, for the next seven days prior to randomization. Participants were then assessed again at baseline, the point of randomization. No data from the treatment period was included in the present analysis.
2.2.1 Daily Assessment Procedures
Participants received text message prompts twice each day (morning, evening) asking that they complete an online survey using the web browser on their smartphone. Participants who did not have a smartphone of their own were given one to use for the duration of the study; all but three participants included in the current analysis already owned a smartphone when they entered the study. Participants chose the timing of the prompts to align with their schedules for optimal response rates. Each survey took about 2 to 6 minutes to complete. Compliance rates for the first 7 days were 87.7% and 77.7% for the morning and evening surveys, respectively.
2.3 Measures
2.3.1 Person-Level Assessments
All person level variables were collected at the baseline assessment.
2.3.1.1 Sociodemographics
A self-report, demographic questionnaire collected data on age, gender, educational and occupational information, race and ethnicity.
2.3.1.2 AUD Diagnosis
DSM-IV criteria for abuse and dependence were assessed using the Composite International Diagnostic Instrument, Substance Abuse Module (Cottler et al., 1989). A proxy for DSM-5 alcohol use disorder (American Psychiatric Association, 2013) was created by summing abuse and dependence criteria together, excluding the legal criterion from abuse. Number of possible criteria endorsed ranged from 0 to 10.
2.3.2 Daily Assessments
Focal predictors and drinking outcomes were assessed at the daily level via online surveys. All variables utilized in this study were from the morning survey with the exception of social factors and salience, which were only measured in the evening survey. We used morning data, where possible, given its higher level of completeness.
2.3.2.1 Drinking Outcomes
Drinking was assessed by asking, “Did you drink yesterday since your morning survey?” If participants responded “yes”, they were asked to report the number of standard drinks of beer, wine, and liquor respectively that they consumed in the last 24 hours. Standard drinks were defined for each category. Participants who responded “no” to the question of whether they drank yesterday were coded as drinking 0 drinks in the prior day. Totals were lagged to align with reports of the focal predictors so that drinking represented what occurred in the following 24 hours (subsequent drinks).
2.3.2.2 Mood
Participants were asked “Please click on the item below which comes closest to your mood over the last hour” and presented with responses ranging from 1 “extremely sad” to 8 “extremely happy.” Within this spectrum, 4 represented “slightly sad” and 5 represented “slightly happy.”
2.3.2.3 Loneliness
One item measured loneliness, “In the past hour, how lonely do you feel?” The response set on these items ranged from 0 “not at all” to 8 “extremely.”
2.3.2.4 Boredom
One item measured boredom, “In the past hour, how bored do you feel?” The response set on these items ranged from 0 “not at all” to 8 “extremely.”
2.3.2.5 Stress
One item measured stress, “In the past hour, how stressed out do you feel?” The response set on these items ranged from 0 “not at all” to 8 “extremely.”
2.3.2.6 Poor Sleep Quality
One item asked participants to “rate your sleep quality last night overall.” The response set for this item ranged from 1 “very good” to 4 “very bad.”
2.3.2.7 Social Influence
Participants were asked in the evening, “Are you with people who...” and then were provided a list of potential scenarios, such as “People who you typically drink around” or “You would rather not drink around (e.g., kid, boss)”. Participants could respond to more than one option. Each item was then given a point—positive for those scenarios encouraging drinking, negative for those scenarios discouraging drinking. The points were then summed to provide a score of social influence. Scores ranged from −3 to 4.
2.3.2.8 Commitment
One item asked participants “How committed are you not to drink heavily (> 5 standard drinks) over the next 24 hours?” The response set on these items ranged from 0 “not at all” to 8 “extremely.”
2.3.2.9 Confidence
One item asked participants “How confident are you not to drink heavily (> 5 standard drinks) over the next 24 hours?” The response set on these items ranged from 0 “not at all” to 8 “extremely.”
2.3.2.10 Alcohol Salience
An item asked: “Please check all that apply about your current location/situation.” The response set was included options related to the availability and visibility of alcohol, such as “alcohol is available, and I can see it”, “alcohol reminders are visible but alcohol is not available”, or “alcohol is NOT available, but it will be in the near future”. Participants could select more than one response, and each response was given a point—positive for alcohol being available and/or visible and negative for alcohol not visible or available. Points were then summed to provide a total score. Scores for this sample ranged from −1 to 5.
2.4 Analytic Plan
Multilevel models (MLMs) with daily ratings (level 1) nested within persons (level 2) were estimated in SAS 9.4 (SAS Institute Inc., 2002–2012). MLMs account for the non-independence of observations due to nesting, are robust to missing data, and can include random terms to model individual variability (Gibbons et al., 2010; Raudenbush and Bryk, 2002; Singer and Willett, 2003). These analyses were performed using the GLIMMIX procedure, with a Poisson distribution and log link specified to account for the non-normal distribution of drinking in this sample. For this study, we also tested models using a negative binomial distribution, with consistent results; however, we report results for the models using a Poisson distribution because they provided much better model fit. All models included random intercept terms to allow for individual variability in drinking levels. We also tested random slope terms, and due to poor model fit or lack of significance, they were excluded. An unstructured variance-covariance matrix was specified, and all analyses utilized residual pseudolikelihood estimation.
Daily ratings of each of the focal predictors were averaged to create estimates of person-level averages (i.e., person or grand mean) and daily-level averages within person for each construct. Person-level averages were used as covariates in their respective models to isolate the within-person (i.e., daily) changes in the focal predictors and their impact on subsequent drinking from the between-person changes (Bolger and Laurenceau, 2013). Subsequent drinking (number of drinks consumed in the immediate 24 hours after the report) was the primary outcome variable. As stated previously, the outcome variable was lagged to align with all the theorized drivers of drinking.
First, age, gender, education, employment, AUD diagnosis, and a variable indicating whether a day was a weekday or not were tested independently as covariates. All but the weekday variable were insignificant (p > .05) and were excluded. Weekday was significant and retained as a covariate for all the models. Next, MLMs tested whether drinking impacted by daily mood, loneliness, boredom, stress, poor sleep, social influence, commitment, confidence, or alcohol salience were moderated by age (entered as a continuous variable), with separate models for each predictor. Where appropriate, significant interactive effects were graphed based on their respective models. All models were re-run with yesterday’s drinking as a covariate, and results were equivalent. Models reported here are those without yesterday’s drinking as a covariate. All figures were derived from the statistical models.
3. Results
3.1 Sample Description
Tables 1 and 2 present baseline demographics and variables of interest by age. Age ranged from 20 to 73, with a mean of just over 43 years. Problem drinkers over 50 were significantly more likely to be White than younger problem drinkers. Overall, participants were a majority female, well educated, and employed at least part-time. A majority of participants met criteria for current DSM-5 severe AUD. Participants drank heavily in the week prior to treatment, consuming an average of just over three standard drinks per day, with no significant differences between groups. On average, older participants significantly differed from younger adults in that they reported being slightly happier, less lonely, less bored, slightly better quality of sleep, and lower stress than their younger counterparts on a daily basis. They also reported higher amounts of commitment, confidence, and alcohol salience than their younger counterparts.
Table 1.
Ch racteristics of Study Sample by Age
| Adults < 49 | Adults > 50 | Total | t or x2statistic | p-value | |
|---|---|---|---|---|---|
| (N=91) | (N=48) | (N=139) | |||
| M (SD) or % | M (SD) or % | M (SD) or % | |||
| Demographics | |||||
| Age | 35.8 (7.9) | 57.5 (5.4) | 43.2 (12.5) | −19.0 | <.001 |
| Female | 59.3 | 52.1 | 56.8 | .55 | .47 |
| Race/Ethnicity | 10.4 | <.01 | |||
| Hispanic/Latino, any race | 21.7 | 10.6 | 18.0 | ||
| White, Non-Hispanic | 58.7 | 85.1 | 67.6 | ||
| Other | 19.6 | 4.3 | 14.4 | ||
| Education | 4.68 | .70 | |||
| High School or Equivalent | 5.5 | 10.4 | 7.2 | ||
| Some College | 23.1 | 22.9 | 23.0 | ||
| Bachelor’s Degree | 37.4 | 35.4 | 36.7 | ||
| Some Graduate Education/Higher | 34.1 | 31.2 | 33.1 | ||
| Employment | 18.0 | <.01 | |||
| Full Time | 67.0 | 52.1 | 61.9 | ||
| Part Time | 13.2 | 20.8 | 15.8 | ||
| Unemployed, Looking for Work | 11.0 | 6.3 | 9.3 | ||
| Disabled | 1.1 | 6.3 | 2.9 | ||
| Retired | 0.0 | 10.4 | 3.6 | ||
| Not in Labor Force | 7.7 | 4.1 | 6.5 | ||
| Baseline Drinking Severity | |||||
| DSM-5 alcohol use disorder criteria meta | 6.8 (2.2) | 6.1 (2.3) | 6.5 (2.3) | 1.7 | .09 |
| Mild (2–3 criteria) | 13.2 | 17.4 | 14.6 | 1.11 | .58 |
| Moderate (4–5 criteria) | 11.0 | 15.2 | 12.2 | ||
| Severe (6+ criteria) | 75.8 | 67.4 | 73.0 | ||
| Age of Onset of Problems with Alcohol | 25.4 (9.0) | 41.0 (12.1) | 30.9 (12.7) | −7.65 | <.001 |
| < 30 | 72.5 | 25.5 | 56.5 | 35.2 | <.001 |
| 31–49 | 27.5 | 38.3 | 28.3 | ||
| > 50 | 0.0 | 36.2 | 15.2 | ||
| EMA Compliance | |||||
| Morning | 86.3 | 89.6 | 87.5 | 1.44 | .23 |
| Evening | 72.4 | 86.3 | 77.2 | 50.1 | <.001 |
Proxy based on DSM-IV dependence and abuse criteria combined. The former abuse criterion regarding legal problems was removed. There was no item for craving.
Table 2.
Descriptives of Focal Predictors and Drinking over Seven Days by Age
| Adults < 49 | Adults > 50 | Total | t-statistic | p-value | |
|---|---|---|---|---|---|
| (N=91) | (N=48) | (N=139) | |||
| M (SD) | M (SD) | M (SD) | |||
| Age Related Focal Predictors | |||||
| Mood | 5.1 (1.4) | 5.4 (1.4) | 5.1 (1.4) | −2.80 | <.01 |
| Loneliness | 1.4 (1.9) | .81 (1.4) | 1.2 (1.7) | 4.70 | <.001 |
| Boredom | 1.2 (1.8) | .66 (1.1) | 1.0 (1.6) | 5.34 | <.001 |
| Stress | 1.9 (2.0) | 1.2 (1.4) | 1.6 (1.8) | 6.07 | <.001 |
| Poor Quality Sleepa | 2.2 (.8) | 2.0 (.7) | 2.2 (.77) | 5.33 | <.001 |
| Social Factors | .62 (1.7) | .46 (1.3) | .49 (1.5) | 1.14 | .25 |
| Common Focal Predictors | |||||
| Commitment | 5.2 (2.7) | 5.9 (2.3) | 5.6 (2.6) | −3.73 | <.001 |
| Confidence | 5.0 (2.5) | 5.4 (2.2) | 5.3 (2.5) | −2.68 | <.01 |
| Alcohol Salience | 1.7 (1.5) | 2.1 (1.1) | 1.8 (1.4) | −4.00 | <.001 |
| Subsequent Drinksb | 3.4 (3.9) | 3.6 (3.3) | 3.5 (3.7) | −.333 | .74 |
Poor quality sleep was indicated by a higher value.
Total drinks reported in morning survey, lagged to align with prior day’s ratings.
3.2 Focal Predictors of Drinking Moderated by Age
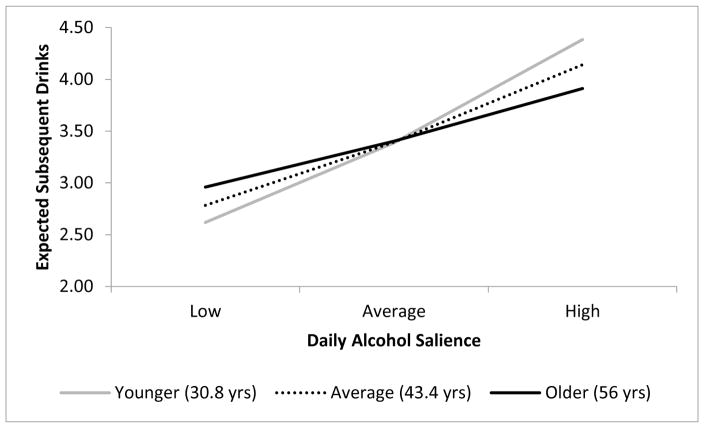
Table 3 shows the results for five models for which there were significant interactions. Age moderated the effects of boredom, poor quality sleep, commitment, confidence, and alcohol salience on subsequent drinks. Consistent with hypotheses, older age and greater boredom yielded greater drinks per day (Figure 1). Contrary to hypotheses, Figure 2 demonstrates that older age and poorer quality sleep yield fewer drinks per day compared to younger counterparts who drank more in the context of poorer quality sleep. While drinking was impacted by high person-level commitment equivalently across age, older adults drank more at low commitment compared to younger adults (Figure 3). Additionally, high daily commitment was not as protective for older adults as it was for younger adults (Figure 3). Greater daily confidence and younger age predicted a low level of drinking; whereas consistent with hypotheses, older adults with greater confidence did not reduce drinking as much as younger adults (Figure 4). Finally, consistent with hypotheses, drinking for older adults was not as influenced by daily alcohol salience as it was for younger adults (Figure 5).
Table 3.
Parameter Estimates of Significant Independent Multilevel Models of Age Moderating Focal Predictors on Subsequent Drinks
| Models | B | SE | t | p |
|---|---|---|---|---|
| Mood | ||||
| Age × Daily | .00 | .00 | −.65 | .51 |
| Age × Person-average | .00 | .00 | 1.44 | .15 |
| Loneliness | ||||
| Age × Daily | .003 | .002 | 1.52 | .13 |
| Age × Person-average | −.004 | .003 | −1.20 | .23 |
| Boredom | ||||
| Age | .002 | .00 | .40 | .69 |
| Person-average | .04 | .04 | .94 | .35 |
| Daily | .04 | .02 | 1.83 | .07 |
| Age × Daily | .004 | .002 | 2.05 | .04 |
| Poor Quality Sleep | ||||
| Age | .00 | .00 | .01 | .99 |
| Person-average | .03 | .11 | .28 | .78 |
| Daily | −.04 | .03 | −1.14 | .26 |
| Age × Person-average | −.02 | .01 | −2.14 | .03 |
| Commitment | ||||
| Age | .005 | .004 | 1.18 | .24 |
| Person-average | −.10 | .03 | −3.72 | < .001 |
| Daily | −.13 | .01 | −11.5 | < .0001 |
| Age × Person-average | −.005 | .002 | −2.06 | .04 |
| Age × Daily | .002 | .001 | 2.93 | < .01 |
| Confidence | ||||
| Age | .004 | .004 | 1.2 | .24 |
| Person-average | −.20 | .03 | −7.39 | < .0001 |
| Daily | −.15 | .01 | −13.2 | < .0001 |
| Age × Daily | .003 | .001 | 3.6 | < .001 |
| Alcohol salience | ||||
| Age | 0.0 | .005 | .04 | .97 |
| Person-average | .26 | .06 | 4.28 | < .0001 |
| Daily | .19 | .20 | 8.26 | < .0001 |
| Age × Daily | −.005 | .002 | −2.41 | .02 |
Note: B = parameter estimate; SE = standard error. Daily variables were centered at the individual person-mean. All others were centered at the grand mean. Covariates time and weekday were entered into all models. Models for mood and loneliness show only the insignificant interaction terms. All other variables show the reduced model.
Figure 1.
Model based expected drinks for daily boredom by age interaction.
Figure 2.
Model based expected drinks for poor quality sleep by age interaction. Higher values of poor quality sleep indicate poorer quality sleep.
Figure 3.
Model based expected subsequent drinks for person-level and daily commitment by age interactions.
Figure 4.
Model based expected drinks for the daily confidence by age interaction.
Figure 5.
Model based expected subsequent drinks for daily alcohol salience by age interaction. Figure 1
4. Discussion
Potentially hazardous drinking (greater than recommended guidelines) among Baby Boomers is high relative to previous birth cohorts and is expected to increase as the population ages. Extant epidemiological and treatment studies suggest problem drinking in middle to late life is associated with depressed mood, loneliness, boredom, stress, sleep problems, and other social factors. This study examined how age impacts these factors' influences on daily drinking habits using EMA via a smartphone among problem drinkers. Findings reveal that prior to treatment, daily fluctuations in mood, loneliness, stress, and social influences were not moderated by age. In other words, these factors effected daily drinking across age equivalently. Both boredom and poor quality sleep were moderated by age, suggesting that greater daily boredom and better overall quality of sleep may be important factors associated with heavier daily drinking among older individuals.
While alcohol salience, commitment and confidence were all moderated by age in generally expected directions, they yielded new information. Older age muted the impact of alcohol salience, commitment and confidence to reduce drinking, suggesting these constructs may operate differently for adults over 50—a group with presumably more long term drinking habits. Older participants may be particularly entrenched in their habits or automatic processes, which remain powerful even in the face of high self-efficacy to change, high motivation, or low alcohol salience. Regardless, findings still suggest that high commitment and confidence are important for reduced drinking, even if their impact are less potent among older adults than for younger adults.
Important findings can be gleaned from this study. This is the first study known to these authors to utilize EMA via smartphones in a sample that included a sizeable proportion of middle-aged and older adult problem drinkers. Compliance rates for daily EMA completion were high for both younger and older drinkers, yet significantly higher for older drinkers on the evening survey than the younger drinkers. Rates indicate that using EMA with this age group is feasible and well received, at least among a group who owned a smartphone. This is counter to existing stereotypes that older adults are not capable or willing to engage with technology but consistent with existing literature on older adult engagement with mobile technology (Kuerbis et al., 2017).
Results also paint a picture of a group of older problem drinkers who report little distress compared to their younger counterparts on a daily basis. While a majority endorsed AUD criteria such that they qualified for severe AUD, it would appear that, overall, older participants were happy, feeling little stress, and had average quality sleep while drinking heavily. This is interesting given that two-thirds of older adults in this sample reported experiencing alcohol problems prior to age 50, suggesting that problems have been present in their lives for at least some time. Participants in this study may not rate the alcohol problems they experience as important or as severe as other problem drinkers do. Alternative explanations may be that older adults are not aware of negative affect or stress, such as would be reflected in the EMA, or it may be that participants responded in a socially biased manner.
4.1 Implications for Clinical Treatment
These findings have important implications for clinical treatment. Other than boredom, there were no age differences on factors previously identified and targeted as fundamental points for intervention among older adult drinkers (e.g., Center for Substance Abuse Treatment, 2005; Schonfeld and Dupree, 1995). While factors such as loneliness, mood, and social influence may indeed be important, findings suggest these are not unique to older adults. Instead, findings point to alternative, important differences across age. Many treatments, including motivational interviewing and cognitive behavioral therapy, specifically focus on increasing motivation and self-efficacy. Given that high confidence, high commitment and low alcohol salience among older adults did not reduce drinking at the same rate as for younger adults, treatments may need to be adapted for optimal effect. Without further understanding of the overt (client reported) and covert (automatic processes that occur outside the awareness of the client) factors that drive substance use, treatment efforts will continue to underperform.
4.2 Limitations
This study has a number of limitations, and findings should be interpreted accordingly. First, this is a secondary data analysis. Assessments, including the EMA, were not specifically tailored to test for drivers of daily drinking for older adults specifically. Psychometric properties of these single item questions, their performance and validity for this group of participants remains relatively unexplored. Second, generalizability is limited to primarily White problem drinkers who own smartphones. It is entirely possible that a more socioeconomically varied or racially diverse sample might yield distinct findings. Despite its lack of socioeconomic and racial diversity, this is one of the few studies to include this age group and to have a substantial representation of women. Third, pre-treatment data collection was limited to only a seven day period. It is possible that, given more days and thus more data points, distinct patterns might emerge. Fourth, responses from participants may be biased in a positive light; however, given the level at which participants were reporting drinking, this seems unlikely.
4.3 Future Research
Future research on older adults and AUD must include varied data collection methods and sampling with greater numbers of participants. Mobile technology should continue to be used to assess drinkers across a spectrum of age, as it demonstrates utility in expanding understanding of how drivers of daily drinking can vary across age group and potentially life stage. In conjunction with greater use of mobile technology, greater understanding of the psychometric properties of EMA is crucial to future research using this methodology, particularly across distinct groups of users. Future analyses should explore how responses to these questions change for this sample over time. For example, loneliness scores may increase as participants go through treatment and raise self-awareness of their emotions. Clearly, research must also expand to include a socioeconomically and racially diverse group, as well as a more heterogeneous group of older adults with a wider age range. Finally, specific efforts should focus on expanding the understanding of how self-efficacy, one of the few mechanisms of behavior change to have consistent support, may operate differently among older adults.
5.0 Conclusion
This study underscores the importance of exploring these factors methodically, scientifically, and from a multipronged approach. Unique daily drivers of drinking among middle-aged and older adults remain relatively unidentified, yet findings have important implications for understanding middle-aged and older problem drinkers.
Highlights.
Using smartphones to collect daily data with people 50 and older is feasible.
Boredom seems to be a particular risk factor for daily drinking among older adults.
Daily confidence does not reduce drinking among older adults like younger adults.
Daily commitment does not reduce drinking among older adults like younger adults.
Older adults do not appear as reactive to alcohol salience as younger adults.
Acknowledgments
Role of Funding Source
This study was supported with funding from the National Institute on Alcohol Abuse and Alcoholism (Grant R01 AA020077; PI: Morgenstern) and the Professional Staff Congress of the City University of New York (PI: Kuerbis).
Footnotes
Contributors
Kuerbis and Treloar were primary for the write up and implementation of the current analysis. Shao was responsible for cleaning and managing data and running models in this paper. Houser, Muench, and Morgenstern were involved in parent study design and implementation and write up of the manuscript. All authors approved of the final manuscript before submission.
Conflict of Interest
No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adlaf EM, Smart RG. Alcohol use, drug use, and well-being in older adults in Toronto. Int J Addict. 1995;30:1985–2016. doi: 10.3109/10826089509071063. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- Arndt S, Clayton R, Schultz S. Trends in substance abuse treatment 1998–2008: Increasing older adult first time admissions for illicit drugs. Am J Geriatr Psychiatry. 2011;19:704–711. doi: 10.1097/JGP.0b013e31820d942b. [DOI] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Barry KL. The relationship between alcohol problems and health functioning of older adults in primary care settings. J Am Geriatr Soc. 2000a;48:769–774. doi: 10.1111/j.1532-5415.2000.tb04751.x. [DOI] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Chermack ST, Mudd SA, Brower KJ. Older adult treatment outcome following elder-specific inpatient alcoholism treatment. J Subst Abuse Treat. 2000b;19:67–75. doi: 10.1016/s0740-5472(99)00101-4. [DOI] [PubMed] [Google Scholar]
- Bolger N, Laurenceau JP. Intensive longitudinal methods: An introduction to diary and experience sampling research. The Guilford Press; New York: 2013. [Google Scholar]
- Borok J, Galier P, Dinolfo M, Welgreen S, Hoffing M, Davis MD, Ramirez KD, Liao DH, Tang L, Karno MP, Sacco P, Lin CF, Moore AA. Why do older unhealthy drinkers decide to make changes or not in their alcohol consumption? Data from the Health Living as You Age Study. J Am Geriatr Soc. 2013;61:1296–1302. doi: 10.1111/jgs.12394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan PL, Schutte KK, Moos RH. Reciprocal relations between stressors and drinking behavior: A three-wave panel study of late middle-aged and older women and men. Addiction. 1999;94:737–749. doi: 10.1046/j.1360-0443.1999.94573712.x. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Rychtarik RG, Prue DM. Behavioral treatment of the geriatric alcohol abuser: A long-term follow up study. Addict Behav. 1985;10:307–311. doi: 10.1016/0306-4603(85)90012-7. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Substance abuse among older adults: Treatment Improvement Protocol (TIP) Series 26. Substance Abuse and Mental Health Services Administration; Rockville, MD: 1998. [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Substance abuse relapse prevention for older adults: A group treatment approach. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2005. [Google Scholar]
- Christopherson VA, Escher MC, Bainton BR. Reasons for drinking among the elderly in rural Arizona. J Stud Alcohol. 1984;45:417–423. doi: 10.15288/jsa.1984.45.417. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Robins LN, Helzer JE. The reliability of the Composite International Diagnostic Interview Substance Abuse Module-(CIDI-SAM): A comprehensive substance abuse interview. Br J Addict. 1989;84:801–814. doi: 10.1111/j.1360-0443.1989.tb03060.x. [DOI] [PubMed] [Google Scholar]
- Dupree LW, Broskowski H, Schonfeld L. The Gerontology Alcohol Project: A behavioral treatment program for elderly alcohol abusers. Gerontologist. 1984;24:510–516. doi: 10.1093/geront/24.5.510. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker D, DuToit S. Advances in analysis of longitudinal data. Annu Rev Clin Psychol. 2010;6:79–107. doi: 10.1146/annurev.clinpsy.032408.153550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Gfroerer JC, Colliver JD, Penne MA. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104:88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- Han BH, Moore AA, Sherman S, Keyes KM, Palamar JJ. Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005–2014. Drug Alcohol Depend. 2017;170:198–207. doi: 10.1016/j.drugalcdep.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson VL. Technology skill and age: What will be the same 20 years from now? Universal Access Inf. 2011;10:443–452. [Google Scholar]
- Institute of Medicine. Retooling for an aging America: Building the health care workforce. The National Academies Press; Washington, DC: 2008. [PubMed] [Google Scholar]
- Institute of Medicine. The mental health and substance use workforce for older adults: In whose hands? The National Academies Press; Washington, DC: 2012. [PubMed] [Google Scholar]
- Kuerbis A, Armeli S, Muench F, Morgenstern J. Motivation and self-efficacy in the context of moderated drinking: Global self-report and ecological momentary assessment. Psychol Addict Behav. 2013;27:934–943. doi: 10.1037/a0031194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Mulliken A, Muench F, Moore AA, Gardner D. Older adults and mobile technology: Toward a better understanding of utilization and applications to behavioral health. Ment Health Addict Res. 2017;2:1–11. [Google Scholar]
- Kuerbis A, Sacco P. The impact of retirement on the drinking patterns of older adults: A review. Addict Behav. 2012;37:587–595. doi: 10.1016/j.addbeh.2012.01.022. [DOI] [PubMed] [Google Scholar]
- Moore AA, Karno MP, Grella CE, Lin JC, Warda U, Liao DH, Hu P. Alcohol, tobacco, and nonmedical drug use in older U.S. adults: Data from the 2001/02 National Epidemiologic Survey of Alcohol and Related Conditions. J Am Geriatr Soc. 2009;57:2275–2281. doi: 10.1111/j.1532-5415.2009.02554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Kuerbis A, Sacco P, Chen G, Garcia MB. Screening and assessment of unhealthy alcohol use in older adults. In: Kuerbis A, Moore AA, Sacco P, Zanjani F, editors. Alcohol and aging: Clinical and public health perspectives. Springer; New York: 2017. pp. 169–180. [Google Scholar]
- Moore AA, Whiteman EJ, Ward KT. Risks of combined alcohol/medication use in older adults. Am J Geriatr Pharmacother. 2007;5:64–74. doi: 10.1016/j.amjopharm.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Brennan P, Fondacaro M, Moos B. Approach and avoidance coping responses among older problem and nonproblem drinkers. Psychol Aging. 1990;5:31–40. doi: 10.1037//0882-7974.5.1.31. [DOI] [PubMed] [Google Scholar]
- Moos RH, Brennan PL, Schutte KK, Moos BS. Older adults' health and late-life drinking patterns: A 20-year perspective. Aging Ment Health. 2010a;14:33–43. doi: 10.1080/13607860902918264. [DOI] [PubMed] [Google Scholar]
- Moos RH, Brennan PL, Schutte KK, Moos BS. Social and financial resources and high-risk alcohol consumption among older adults. Alcohol Clin Exp Res. 2010b;34:646–654. doi: 10.1111/j.1530-0277.2009.01133.x. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Kuerbis A, Houser J, Muench FJ, Shao S, Treloar H. Within-person associations between daily motivation and self-efficacy and drinking among problem drinkers in treatment. Psychol Addict Behav. 2016;30:630–638. doi: 10.1037/adb0000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers JE, Harper MC. Evidence-based effective practices with older adults. J Couns Dev. 2004;82:207–218. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Rethinking drinking. Bethesda, MD: 2013. [Google Scholar]
- Oslin DW, Mavandadi S. Alcohol and drug problems. In: Blazer DG, Steffens DC, editors. Textbook of Geriatric Psychiatry. American Psychiatric Publishing; Arlington, VA: 2009. pp. 1–17. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- Sacco P, Burruss K, Smith CA, Kuerbis A, Harrington D, Moore AA, Resnick B. Drinking behavior among older adults at a continuing care retirement community: Affective and motivational influences. Aging Ment Health. 2015a;19:279–289. doi: 10.1080/13607863.2014.933307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco P, Unick GJ, Kuerbis A, Koru AG, Moore AA. Alcohol-related diagnoses in hospital admissions for all causes among middle-aged and older adults: Trends and cohort differences from 1993 to 2010. J Aging Health. 2015b;27:1358–1374. doi: 10.1177/0898264315583052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS software, Version 13.1 for Windows. Author; Cary, NC: 2002–2012. [Google Scholar]
- Schonfeld L, Dupree LW. Treatment approaches for older problem drinkers. Int J Addict. 1995;30:1819–1842. doi: 10.3109/10826089509071057. [DOI] [PubMed] [Google Scholar]
- Schonfeld L, Dupree LW, Dickson-Fuhrman E, Royer CM, McDermott CH, Rosansky JS, Taylor S, Jarvik LF. Cognitive-behavioral treatment of older veterans with substance abuse problems. J Geriatr Psychiat Neur. 2000;13:124–128. doi: 10.1177/089198870001300305. [DOI] [PubMed] [Google Scholar]
- Schonfeld L, King-Kallimanis BL, Duchene DM, Etheridge RL, Herrera JR, Barry KL, Lynn N. Screening and brief intervention for substance misuse among older adults: The Florida BRITE project. Am J Public Health. 2010;100:108–114. doi: 10.2105/AJPH.2008.149534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press; New York: 2003. [Google Scholar]
- Sjoerds Z, van den Brink W, Beekman ATF, Penninx BWJH, Veltman DJ. Cue reactivity is associated with duration and severity of alcohol dependence: An fMRI study. PLoS One. 2014;9:e84560. doi: 10.1371/journal.pone.0084560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Wardle J. Positive affect measured using ecological momentary assessment and survival in older men and women. Proc Natl Acad Sci USA. 2011;108:18244–18248. doi: 10.1073/pnas.1110892108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of national findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013. NSDUH Series H-46, HHS Publication No. (SMA) 13–4795. [Google Scholar]
- Witteman J, Post H, Tarvainen M, de Bruijn A, Perna Ede S, Ramaekers JG, Wiers RW. Cue reactivity and its relation to craving and relapse in alcohol dependence: a combined laboratory and field study. Psychopharmacology (Berl) 2015;232:3685–3696. doi: 10.1007/s00213-015-4027-6. [DOI] [PMC free article] [PubMed] [Google Scholar]