Abstract
This systematic review evaluates efforts to date to involve community health workers (CHWs) in delivering evidence-based mental health interventions to under-served communities in the United States and in low- and middle-income countries. Forty-three articles (39 trials) were reviewed to characterize the background characteristics of CHW, their role in intervention delivery, the types of interventions they delivered, and the implementation supports they received. The majority of trials found that CHW-delivered interventions led to symptom reduction. Training CHWs to support the delivery of evidence-based practices may help to address mental health disparities. Areas for future research as well as clinical and policy implications are discussed.
Keywords: Community health workers, Mental health disparities
Introduction
Globally and domestically, the gap between individuals who need mental health care and those who receive it is sizeable (Roll et al. 2013). In low- and middle-income countries (LMICs), over 75% of individuals who would benefit from care do not receive it (World Health Organization 2008, 2010). In the United States (US), ethnic and racial minorities are less likely to receive mental health treatment than non-Hispanic white individuals (Alegría et al. 2008; Coker et al. 2009; Wells et al. 2001). In both contexts, when treatment is available for underserved communities, it is rarely evidence-based or high quality (Alegría et al. 2008; Dua et al. 2011). Making evidence-based treatments (EBTs) or evidence-informed practices accessible for underserved communities has been a major focus of international and domestic policies as a strategy to reduce the global burden of mental disorders (Barry and Huskamp 2011; Becker and Kleinman 2013; World Health Organization 2010). The World Health Organization (WHO) launched the Mental Health Gap Action Programme to scale-up EBTs for individuals with mental health, neurological, and substance use disorders in LMICs (Dua et al. 2011; World Health Organization 2010). Domestically, the Patient Protection and Affordable Care Act emphasizes the provision of evidence-based care (Barry and Huskamp 2011). However, even with these policies in place, innovative solutions and a public health model of workforce development are needed to address existing mental health disparities. This systematic review consolidates literature for one recommended solution to address mental health disparities in the US and LMICs—the incorporation of community health workers (CHWs) into mental health service delivery (Acevedo-Polakovich et al. 2013; Chavira et al. 2015; Kazdin and Rabbitt 2013; van Ginneken et al. 2012).
CHWs have been referred to by a variety of terms, including but not limited to, promotores, lay health workers, lay providers, indigenous paraprofessionals, peer support specialists, and natural helpers. In this review, we use the term CHW for interventionists without formal mental health training and who are members of the community they serve (Ayala et al. 2010; Viswanatha et al. 2010). CHW-delivered mental health interventions can increase the availability of care, given substantial workforce challenges to meet service needs. In the US, the number of interventionists that can provide linguistically and culturally appropriate care is insuffcient to address the needs of vulnerable populations (Kakuma et al. 2011; McGuire and Miranda 2008). In LMICs, there is a substantial shortage of mental health professionals, with one study estimating that 239,000 additional providers are needed to address the needs of 58 countries (Bruckner et al. 2011). CHWs can provide cost-effective care in low-resourced communities and agencies (Buttorff et al. 2012, Kazdin and Rabbit 2013).
Even when services are available, a wide range of factors impact whether individuals access or seek care, including, structural barriers (e.g., lack of transportation), low mental health literacy, mental health stigma, and negative perceptions of mental health care providers (Alegría et al. 2010; Chow et al. 2003; Kilbourne et al. 2006; Nadeem et al. 2007). Furthermore, individuals from non-Western cultures may conceptualize their mental health symptomatology as being related to spiritual or metaphysical factors, and prefer to seek care from traditional healers or religious centers as opposed to mental health providers (Raguram et al. 2002; Saravanan et al. 2007). As members of the communities they serve, CHWs may be uniquely positioned to build trust and address barriers to seeking care among traditionally underserved communities (Katigbak et al. 2015). Relatedly, CHWs can reduce the stigma associated with receiving mental health care, which in turn has been shown to increase service engagement even for highly stigmatized conditions such as HIV and schizophrenia (Balaji et al. 2012; Morris et al. 2009).
Current Models of CHW-Involved Care
CHW models of care delivery have been used most frequently to address physical health disparities. For example, CHWs have been found to be effective for promoting the rates of childhood immunizations and improving outcomes for individuals with chronic health conditions such as diabetes, obesity, and asthma (Ayala et al. 2010; Lewin et al. 2010; Perry et al. 2014; Rhodes et al. 2007; Viswanathan et al. 2010). Given the growing evidence that CHWs are effective in improving physical health outcomes, increased attention has been focused on incorporating CHWs into mental health services (e.g., Stacciarini et al. 2012). Existing models for incorporating CHWs in mental health interventions can be classified into four categories: (1) CHWs can conduct outreach to facilitate entry into provider settings, a role that has been described as a “bridge” between the community and care providers (e.g., Ayala et al. 2010); (2) CHWs can provide auxiliary support of mental health treatment delivery through case management and promotion of patient adherence to treatment (e.g., Barnett et al. 2016); (3) within a stepped-care model, CHWs can provide lower levels of care to patients with less intensive needs while mental health professionals provide a higher level of care to patients with more severe symptomatology (e.g., Araya 2006; Patel et al. 2010); (4) finally, CHWs can be responsible for the delivery of mental health services as the sole treatment provider (e.g., Bolton et al. 2014a; Murray et al. 2015).
Although there have been successful examples employing CHWs in each of these functions, there remain multiple practical, implementation, and policy questions about the most appropriate roles for CHWs both domestically and globally. These questions are especially relevant to the provision of EBTs or evidence-informed practices, as individuals with advanced training in mental health (e.g., Master's or Doctorate degrees in Psychology or Social Work) typically deliver these interventions. In order to establish the extent to which CHWs can reduce population mental health burden, it will be useful to review the types of interventions they have delivered successfully. Beyond identifying the most appropriate interventions to deliver, it remains to be seen which CHWs functions may be most effective in increasing access to care and the effectiveness of services provided (van Ginneken et al. 2012). Given differences in the availability of mental health providers in the US and LMICs and local regulations in who can provide care, it is likely that the roles that CHWs can occupy will vary based on location. Regarding implementation, the level of training and support that CHW must receive to effectively carry out these various roles has not been established, though limited data suggests that ongoing supervision is needed (Rhodes et al. 2007).
Recently, a Cochrane review was conducted to investigate the effectiveness of mental health service delivery by “non-specialist health workers” in LMICs (van Ginneken et al. 2012). Non-specialist health workers included CHWs, along with other professional health workers (e.g., nurses, doctors), and teachers without formal mental health training. The objective of the Cochrane review was to identify whether non-specialized health workers were effective in reducing the global health burden of mental, neurological, and substance abuse disorders in developing countries. The review concluded that non-specialized health workers were effective in improving outcomes for depression, post-traumatic stress disorder, and alcohol use disorder. The authors recommended that future systematic reviews focus on identifying strategies to integrate CHW programs in to mental health systems of care and identify if these programs impact disparities in care. Furthermore, the Cochrane review did not include efforts outside of LMICs; additional attention is needed on how CHWs may address mental health disparities in the US and other developed nations.
Purpose and Research Questions
Given the growing mobilization of CHWs in mental health care, and the vast variability of their roles in mental health care delivery, this systematic review sought to consolidate supporting literature for CHW mobilization in evidence-based mental health intervention delivery globally and domestically. The primary purpose of the review was to evaluate efforts to date to involve CHWs in the delivery of evidence-based mental health interventions and to identify areas for future research as well as clinical and policy implications. We described the backgrounds of the CHWs, the types of interventions they were involved in delivering, the roles occupied by CHWs, and the implementation supports they received in the delivery of these interventions. Based on recent efforts to increase access to EBTs for underserved communities (Barry and Huskamp 2011; Dua et al. 2011), we also characterized the level of evidence supporting the interventions delivered by CHWs. For the purposes of this review, we contrasted EBTs, evidence-informed practices, and novel, community developed interventions. EBTs were defined as specific protocols that have been previously tested in randomized-control trials (RCTs), such as Trauma Focused Cognitive Behavioral Therapy (Cohen et al. 2006), Interpersonal Therapy (Klerman et al. 1984), or Behavioral Activation (Dimidjian et al. 2008). Evidence-informed practices, included interventions that were described as being based on evidence-based practices (e.g., used components of cognitive behavioral therapy), but had not been previously evaluated in a controlled trial. Novel, community-informed interventions were those interventions that were developed through a community-participatory process or by community providers. In the second objective, we contrasted the nature of CHW involvement in the delivery of mental health interventions in LMICs and the US. No trials of CHW-involved care in other developed nations met the inclusion criteria, so this review only incudes trials conducted in the US. Based on the differences in resources available for mental health care, we expected there to be differences in the rigor of the research design, the roles of the CHWs, and the evidence-base of the interventions used in the US versus LMIC settings. Third, the review sought to describe the clinical outcomes of the subset of studies that were RCTs of CHW-involved mental health interventions, in order to provide a more comprehensive understanding of whether CHWs are effective in reducing mental health disparities. In this review, CHW-involved mental health interventions were considered effective if they performed significantly better than a comparison condition on the primary mental health outcome measured.
Method
Inclusion and Exclusion Criteria
This systematic review identified empirical research from 1990 to 2015 involving CHWs providing or supporting the delivery of a psychosocial intervention targeting a mental health outcome. To be included, studies had to meet criteria related to the study design, providers, participants, interventions, and outcome measures. (1) Study designs included in this review were: randomized control trials, quasi-experimental trials, and pre-post non-experimental trials. Single subject design studies were excluded from the review. (2) Providers needed to include CHWs, defined as community members without formalized mental health training. Studies that focused on task-shifting mental health care to other health professionals (e.g., medical professionals) were not included in this review, though this topic has been reviewed elsewhere (van Ginneken et al. 2012). (3) Participants either needed to reside in an LMIC or if the study was conducted in the US, the majority of the treated sample needed to be composed of racial/ethnic minorities. This inclusion criterion was set to maintain the focus on the potential of CHW mobilization to reduce disparities in mental health service delivery. (4) Interventions needed to have a primary focus on treating or preventing a mental health disorder or symptoms in children, adolescents, or adults. Studies of interventions that primarily focused on a physical health target (e.g., obesity prevention, infant health and development) that included measurement of mental health outcomes were excluded from this review. (5) Outcome measures needed to include patient-level mental health outcomes as a primary outcome. Secondary implementation outcomes (e.g., cost, fidelity) could be included, but studies with a focus on implementation outcomes as opposed to clinical effectiveness were excluded from the review.
Search Strategy
In order to target the literature on mental health services, we searched PsycINFO and PubMed using the EBSCO database host. The search strategy included a joint function of two concepts: (1) terms for CHW and (2) mental health target areas (see Table 1 for specific search terms used). We reviewed all titles and abstracts to identify relevant articles. The full-text of remaining articles were reviewed, with specific attention to the methods section, to guarantee that articles met all inclusion criteria. Furthermore, we reviewed the articles that were included in the Cochrane review and included those that specifically involved CHWs in mental health care. We also completed searches of the reference lists of all articles identified in the search above that met inclusion criteria, along with searches for articles that cited theses articles, to guarantee comprehensiveness of the review.
Table 1. Search strategy.
| Search string |
|---|
| 1. (“Community Health Worker” OR CHW OR “Lay Counselor” OR “Lay Health Worker” OR LHW OR Paraprofessional OR Task Shifting OR Promotor* OR “Natural Helper” or “Lay Health Advisor” OR “Family Support Specialist” OR “Peer Support Specialist”) AND |
| 2. (“Mental health” OR Depression OR Anxiety OR Trauma OR Disruptive behavior OR conduct OR Parent* OR Autism OR Psychosis “Substance Use” OR “Alcohol Use”) |
Data Extraction and Coding Procedures
A codebook with definitions of each construct included in the review was created and used to train a team of four research assistants to code each article. At least two coders independently reviewed and extracted data from each article. Consensus meetings were held between the two coders for each article to determine final codes. Remaining questions concerning coding were discussed in biweekly meetings led by the first author, which led to code refinement and consensus.
Methods of Synthesis
Based on recommendations for narrative synthesis for systematic reviews, we primarily used tabulation, textual descriptions, and vote counting to summarize the included studies and answer the primary research questions (Popay et al. 2006). We used tabulation and textual descriptions to better understand the backgrounds of CHW, the roles CHW had in interventions, the interventions they delivered, and the implementation supports (e.g., supervision, fidelity monitoring) they received (see Table 2). Textual descriptions included writing brief descriptions of selection criteria for CHWs and implementation supports to begin to synthesize data on these topics. In order to evaluate differences between studies conducted in LMICs and the US, we used tabulation, in which characteristics of studies in both settings were compiled and compared (see Table 3). Finally, we used vote counting, in which we calculated the number of studies that achieved statistically significant results on mental health outcomes in comparisons to those that did not, to begin to identify patterns in studies that had positive outcomes (see Table 4).
Table 2. Characteristics of studies.
| Trial | Study design | Location | Client demographics | CHW demographics | Intervention | Implemention supports described | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||||
| N (interention) | Age group | Race/ethnicity | N | Race/ethnicity | Minimum education level | Setting | CHW primary role | Target problem | Practice Type | Training | Supervision | Fidelity monitoring | |||
| 1. Ali et al. (2003)* Gul and Ali (2004)* |
RCT | LMIC | 366 (216) | Adult | Asian | 21 | Asian | N/R | Home | Sole provider | Depression anxiety | Evidence-informed | Yes | N/R | N/R |
| 2. Ayon et al. (2014)* | Pre/post | US | 71 | Child/family | Latino | 36 | Latino | BA | Schools, community | Sole provider | Substance Use | Novel | Yes | N/R | N/R |
| 3. Barlow et al. (2013)* Barlow et al. (2015)* |
RCT | US | 322 (159) | Child/family | Native American | N/R | Native American | N/R | Home | Sole provider | Parenting | Novel | Yes | N/R | Yes |
| 4. Bolton et al. (2003)* Bass (2006)* |
RCT | LMIC | 284 (139) | Adult | African | N/R | African | High school | N/R | Sole provider | Depression | EBT | Yes | N/R | N/R |
| 5. Bolton et al. (2014a)* | RCT | LMIC | 281 (215) | Adult | Middle Eastern | 20 | Middle Eastern | High school | Medical | Sole provider | Depression | EBT | Yes | Yes | N/R |
| 6. Bolton et al. (2014b)* | RCT | LMIC | 347 (182) | Adult | Asian | 20 | Asian | High school | Home, community | Sole provider | Anxiety depression trauma | Evidence-informed | Yes | Yes | Yes |
| 7. Edelblute et al. (2014) | Pre/post | LMIC | 60 | Adult | Latino | 7 | Latino | N/R | Community | Stepped care | Anxiety depression | Evidence-informed | N/R | Yes | N/R |
| 8. Ernst et al. (1999)* | RCT | US | 96 (65) | Child/family | African American, Native American, Asian, Latino | N/R | N/R | N/R | Home | Case management | Substance use | Novel | N/R | N/R | N/R |
| 9. Ertl (2011) | RCT | LMIC | 85 (29) | Child/family | African | 14 | African | N/R | Community | Sole provider | Depression | EBT | Yes | Yes | Yes |
| 10. Fayyaad et al. (2010)* | Pre/post | LMIC | 87 | Child/family | Middle Eastern | 20 | Middle Eastern | BA | Community | Sole provider | Trauma | Evidence-informed | Yes | Yes | N/R |
| 11. Ginsburg et al. (2012)* | RCT | US | 47 (22) | Child/family | Native American | 47 | Native American | AA | Home, mental health clinic | Sole provider | Parenting | Evidence-informed | Yes | Yes | Yes |
| 12. Han et al. (2012)* | Pre/post | US | 9 | Adult | Asian | 1 | Asian | N/R | Mental health clinic | Co-Therapy | Prenatal depression | Novel | Yes | N/R | N/R |
| 13. Hirani et al. (2010) | RCT | LMIC | 24 (7) | Adult | Asian | N/R | Asian | N/R | Community | Sole provider | Depression | Evidence-informed | Yes | N/R | N/R |
| 14. Hovey et al. (2014)* | Pre/post | US | 6 | Adult | Latino | 1 | Latino | N/R | Community | Co-Therapy | Anxiety depression | Evidence-informed | N/R | Yes | N/R |
| 15. Jordans et al. (2010)* | RCT | LMIC | 324 (164) | Child/family | Asian | N/R | Asian | N/R | Schools | Sole provider | Trauma | Evidence-informed | Yes | Yes | N/R |
| 16. Kaufman et al. (2013)* | Pre/post | LMIC | 36 | Child/family | Asian | 8 | Asian | Some college | Community | Sole provider | Anxiety depression | Evidence-informed | Yes | Yes | Yes |
| 17. Magaña et al. (2015) | Pre/post | US | 19 | Child/family | Latino | 3 | Latino | N/R | Home | Sole provider | Autism | Novel | Yes | N/R | N/R |
| 18. Moore et al. (2016)* | RCT | US | 29 (14) | Adult | Latino | 4 | Latino | N/R | Community | Sole provider | Substance use | Evidence-informed | Yes | Yes | Yes |
| 19. Murray et al. (2015)* | RCT | LMIC | 157 (131) | Child/family | African | 20 | African | High school | Home, medical, schools, community | Sole provider | Trauma | EBT | Yes | Yes | Yes |
| 20. Murray et al. (2013)* | Pre/post | LMIC | 94 | Child/family | African | 18 | African | N/R | Community | Sole provider | Trauma | EBT | Yes | Yes | Yes |
| 21. Nadkarni et al. (2015)* | RCT | LMIC | 53 (27) | Adult | Asian | 12 | Asian | 10th grade | Medical | Sole provider | Substance use | Evidence-informed | N/R | Yes | N/R |
| 22. Neuner et al. (2008)* | RCT | LMIC | 277 (111) | Adult | African | 9 | African | Primary school | Community | Sole provider | Trauma | EBT | Yes | Yes | Yes |
| 23. Nimgaonkar and Menon (2015)* | Pre/post | LMIC | 268 | Adult | Asian | 114 | Asian | N/R | Medical | Stepped care | Psychiatric illnesses | Novel | Yes | Yes | N/R |
| 24. O'Donnell et al. (2014)* | Pre/post | LMIC | 64 | Child/family | African | 4 | African | Some college | Community | Sole provider | Trauma | EBT | Yes | Yes | Yes |
| 25. Papas et al. (2011)* | RCT | LMIC | 75 (42) | Adult | African | 2 | African | High school | Medical | Sole provider | Substance use | Evidence-informed | N/R | Yes | Yes |
| 26. Papas et al. (2010)* | Pre/Post | LMIC | 27 | Adult | African | 2 | African | High school | Medical | Sole provider | Substance Use | Evidence-informed | Yes | Yes | Yes |
| 27. Patel et al. (2010)* | RCT | LMIC | 2796 (1,360) | Adult | Asian | N/R | Asian | N/R | Medical | Stepped care | Anxiety/depression | Evidence-informed | Yes | N/R | N/R |
| 28. Peterson et al. (2012)* | Quasi-experimental | LMIC | 60 (30) | Adult | African | 30 | African | N/R | Mental health clinic | Sole provider | Depression | EBT | Yes | N/R | N/R |
| 29. Puffer et al. (2015)* | RCT | LMIC | 270 (135) | Child/family | African | 2 | African | N/R | Community | Sole provider | Parenting | Evidence-informed | N/R | N/R | N/R |
| 30. Rahman (2008)* | RCT | LMIC | 903 (463) | Child/family | Asian | 40 | Asian | High school | Home | Sole provider | Depression | Evidence-informed | N/R | Yes | N/R |
| 31. Roman et al. (2007)*, (2009)* | RCT | US | 613 (266) | Child/family | Latino, African American, Caucasian | N/R | N/A | High school or GED | Home | Co-therapy | Depression | Novel | Yes | Yes | N/R |
| 32. Rosenburg et al. (2002)* | RCT | US | 159 (88) | Child/family | Hispanic, African American | 3 | N/A | N/R | Home | Sole provider | Parenting | Novel | Yes | N/R | N/R |
| 33. Sorsdahl (2015)* | RCT | LMIC | 335 (225) | Adult | African | 5 | African | BA | Medical | Sole provider | Substance use | EBT & evidence-informed | Yes | Yes | Yes |
| 34. Tol et al. (2008)* | RCT | LMIC | 403 (182) | Child/family | Asian | N/R | Asian | High school | Schools | Sole provider | Trauma | Evidence-informed | Yes | N/R | N/R |
| 35. Tol et al. (2014)* | RCT | LMIC | 329 (153) | Child/Family | African | N/R | African | High school | Schools | Sole provider | Trauma | Evidence-informed | Yes | Yes | N/R |
| 36. Waitzikin (2011)* | RCT | US | 120 (N/R) | Adult | Latino | 2 | Latino | High school | Medical | Case management | Depression | Novel | Yes | N/R | N/R |
| 37. Walkup et al. (2009)* | RCT | US | 167 (81) | Child/family | Native American | N/R | Native American | High school | Home | Sole provider | Parenting | Novel | Yes | Yes | Yes |
| 38. Weiss et al. (2015)* | RCT | LMIC | 342 (228) | Adult | Middle Eastern | 29 | Middle Eastern | N/R | Home, medical | Sole provider | Trauma, anxiety, depression | EBT & Evidence-informed | Yes | Yes | Yes |
| 39. Williamson et al. (2014)* | RCT | US | 194 (113) | Child/family | Latino | N/R | Latino | N/R | Home | Sole provider | Parenting | Evidence-informed | Yes | Yes | N/R |
N/R not reported
Original study in a trail
Table 3. Differences between trials in LMICs and US settings.
| LMICS n (%) | US n (%) | χ2 | p | |
|---|---|---|---|---|
| Trial design | 0.00 | 1.00 | ||
| RCT | 18 (73.1%) | 9 (69.2%) | – | – |
| Quasi-experiment or pre/post | 7 (26.9%) | 4 (30.8%) | – | – |
| Age served | 2.51 | 0.113 | ||
| Child/Family | 11 (42.3%) | 9 (69.2%) | – | – |
| Adult | 15 (57.7%) | 4 (30.8%) | – | – |
| Intervention | 14.09 | 0.001 | ||
| EBT | 10 (38.5%) | 0 (0%) | 6.76 | 0.009 |
| Evidence-informed | 15 (57.7%) | 4 (30.8%) | 1.10 | 0.271 |
| Novel, community-driven | 1 (3.9%) | 9 (69.2%) | 16.00 | >0.001 |
| CHW primary role | 12.29 | 0.002 | ||
| Sole provider | 23 (88.5%) | 8 (61.5%) | 4.00 | 0.194 |
| Stepped care | 3 (11.5%) | 0 (0%) | 1.69 | 0.230 |
| Auxiliary | 0 (0%) | 5 (38.5%) | 11.56 | >0.001 |
| Implementation support described | ||||
| Training | 21 (80.8%) | 10 (76.9%) | 0.09 | 0.768 |
| Ongoing supervision | 19 (73.1%) | 6 (46.2%) | 2.73 | 0.098 |
| Fidelity monitoring | 11 (42.3%) | 4 (30.8%) | 0.48 | 0.485 |
LMICs = 26 trials, US = 13 trials
Table 4. Effectiveness of CHW-involved interventions in RCTs.
| Trial | Intervention type | Comparison group | N (intervention) | Sig. group differences |
|---|---|---|---|---|
| 1. Ali et al. (2003)* Gul and Ali (2004)* |
Evidence-informed | WLC | 366 (216) | Yes Yes |
| 2. Barlow et al. (2013)* Barlow et al. (2015)* |
Novel | Enhanced UC | 322 (159) | Yes |
| 3. Bolton et al. (2003)* Bass (2006)* |
EBT | UC | 284 (139) | Yes Yes |
| 4. Bolton et al. (2014a)* | EBT | WLC | 281 (215) | Yes |
| 5. Bolton et al. (2014b)* | Evidence-informed | WLC | 347 (182) | Yes |
| 6. Ernst et al. (1999)* | Novel | No treatment | 96 (65) | No |
| 7. Ertl (2011) | EBT | WLC, active control | 85 (29) | Yes |
| 8. Ginsburg et al. (2012)* | Evidence-informed | Active control | 47 (22) | No |
| 9. Hirani et al. (2010) | Evidence-informed | No treatment, active Control | 24 (7) | No |
| 10. Jordans et al. (2010)* | Evidence-informed | WLC | 325 (164) | No |
| 11. Moore et al. (2016)* | Evidence-informed | Active control | 29 (14) | No |
| 12. Murray et al. (2015)* | EBT | UC | 257 (131) | Yes |
| 13. Nadkarni et al. (2015)* | Evidence-informed | Enhanced UC | 53 (27) | No |
| 14. Neuner et al. (2008)* | EBT | UC, no treatment | 277 (11) | No |
| 15. Papas et al. (2011)* | Evidence-informed | UC | 75 (42) | Yes |
| 17. Patel et al. (2010)* | Evidence-informed | Enhanced UC | 2796 (1360) | Yes |
| 18. Pufer et al. (2015)* | Evidence-informed | WLC | 270 (135) | Yes |
| 19. Rahman (2008)* | Evidence-informed | UC | 903 (463) | Yes |
| 20. Roman et al. (2007)*, (2009)* | Novel | UC | 613 (307) | Yes |
| 21. Rosenburg et al. (2002)* | Novel | UC | 159 (88) | Yes |
| 22. Sorsdahl (2015)* | EBT & evidence-informed | Bibliotherapy | 335 (225) | Yes |
| 23. Tol et al. (2008)* | Evidence-informed | WLC | 403 (182) | Yes |
| 24. Tol et al. (2014)* | Evidence-informed | WLC | 329 (153) | No |
| 25. Waitzikin (2011)* | Novel | Enhanced UC | 120 (N/R) | No |
| 26. Walkup et al. (2009)* | Novel | Active control | 167 (81) | Yes |
| 27. Weiss et al. (2015)* | EBT & evidence-informed | dWLC | 342 (228) | Yes |
| 28. Williamson et al. (2014)* | Evidence-informed | WLC | 194 (113) | Yes |
N/R not reported
Original study in a trial
Results
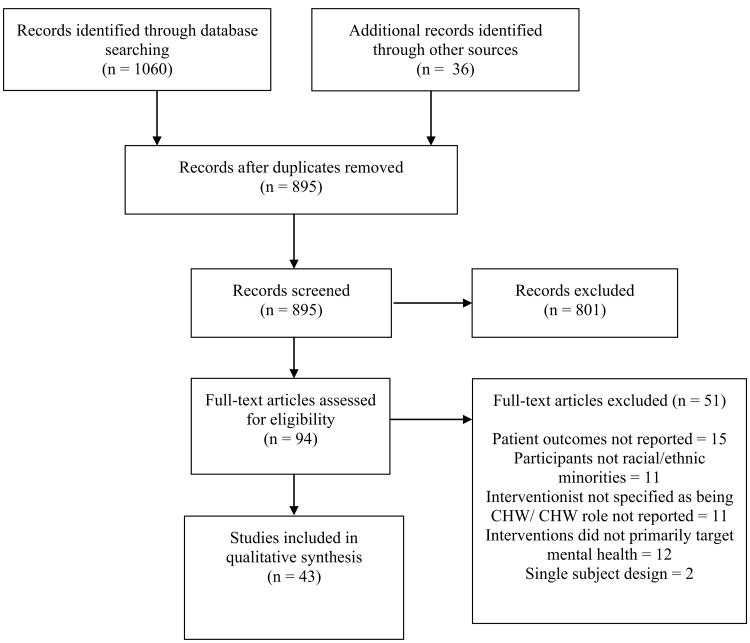
Of the 95 articles assessed for eligibility, 43 articles (39 trials) met inclusion criteria for this review (Table 2). Figure 1 shows the flow of studies from identification using the search strategy to ultimate inclusion in the final sample for analysis. The majority of the studies were RCTs (n = 27; 62.8%) and were conducted in LMICs (n = 26; 66.7%). Even though the literature search extended from 1990 to May 2016, the majority of articles (n = 31; 72.1%) that met inclusion criteria were published after 2010, indicating a rapid and recent increase in research on involving CHWs in the delivery of psychosocial interventions for mental health conditions. Studies varied dramatically in terms of their scope and sample size. For example, Patel et al. (2011) and Rahman et al. (2008) conducted large-scale cluster randomized trials; whereas Han et al. (2012) and Hovey et al. (2014) had fewer than 10 participants in their studies.
Fig. 1. Prisma flow diagram.
Objective 1: Characterize CHWs and Their Involvement in the Delivery of Mental Health Interventions Within the Treatment Outcome Literature
Background Characteristics of CHWs
Twenty-eight trials reported the number of CHWs involved in interventions. In these 28 trials, 477 individual CHWs provided services. A variety of terms were used for CHW providers, with the most frequent terms being promotora/es, paraprofessionals, and lay counselors. Of the 38 trials that reported the race/ethnicity of the CHWs, 31.6% included CHWs of African descent (i.e., African, African-American, Afro-Caribbean), 28.9% of Asian/Pacific Islander descent, 18.4% of Latino descent, 7.9% of Middle Eastern descent, and 7.9% were Native American.
Regarding the preparation and education backgrounds of CHWs in these studies, 51.3% of trials (n = 20) reported the CHWs' educational level. Of the 20 studies that described education levels of the CHWs, the majority (n = 12; 60.0%) reported that CHWs had a minimum of a high school degree or equivalent. In two studies, CHWs had less than a high school degree, and in six studies CHWs had either an Associate's or Bachelor's degrees or some college. Though it was not consistently described in the studies, CHWs often were selected because they had similar backgrounds and life experiences as the populations they were recruited to serve. For example, CHWs included Latina mothers of children with an Autism Spectrum Disorder diagnosis (Magaña et al. 2015), Burmese refugees (Bolton et al. 2014b), or past or present migrant farm workers (Hoveyet al. 2014). Other studies selected CHWs who were already employed in this role and had previously provided other health promotion services (e.g., Peterson et al. 2012; Williamson et al. 2014).
Interventions
The interventions targeted a range of clinical problems, including depression (n = 16), psychological trauma (n = 10), anxiety (n = 7), substance use (n = 7), and childhood disruptive behavior disorders (n = 6), and autism spectrum disorders (n = 1). Multiple studies targeted more than one problem area. Interventions were delivered in community (e.g., churches, refugee settlements, literacy centers), medical, mental health, school, and home settings. Nineteen of the trials included interventions that targeted adults (48.7%) and 20 trials (51.3%) targeted children or families. Interventions were classified as being for children/families if the study included measurement of child mental health outcomes, a focus on parenting, or targeted maternal mental health with the purpose of ultimately improving child or family outcomes.
Regarding the delivered interventions, ten trials tested EBT protocols (e.g., Trauma-Focused Cognitive Behavioral Therapy, Cohen et al. 2006), 22 trials tested interventions that were informed by evidence-based practices (e.g., cognitive-behavioral principles), and ten trials tested novel, community-informed interventions. The total number of interventions tested is greater than the number of trials because two of the trials that tested an EBT also included an intervention arm that included an evidence-informed practice (Sorsdahl et al. 2015; Weiss et al. 2015) and another trial included two arms with two different EBT (Bolton et al. 2014a).
CHW Roles
In the majority of trials (n = 31; 79.5%), the CHWs served as the sole provider of the intervention. CHWs also were involved in stepped-care interventions (n = 3; 7.7%), where they provided a lower level of care for clients with low-severity mental health concerns (e.g., psychoeducation about depression) and professionals provided higher intensity services for individuals with more severe symptomatology (e.g., medication management; Patel et al. 2010). Apart from sole provider and stepped care models, CHWs provided other auxiliary roles, including co-therapy alongside a professional mental health provider or nurse practitioner (n = 3; Han et al. 2012; Hovey et al. 2014; Roman et al. 2007; Roman et al. 2009), and providing case management as their primary roles (n = 2; Ernst et al. 1999; Waitzikin et al. 2011). CHWs were described as conducting outreach in multiple studies, but this was never described as their primary role.
Implementation Supports
Thirty-two of the trials (82.1%) included descriptions of the CHW training protocol, with varying level of detail. Trainings ranged from 2 days to 3 months of training. Reported training activities included didactic, role-playing, and proficiency testing. Twenty-five of the articles (64.1%) described ongoing supervision for the CHWs during the course of the intervention. Group and individual supervision models were used, with supervision provided locally (e.g. Murray et al. 2015; Williamson et al. 2014) or through conference calls or Skype sessions (e.g. Papas et al. 2011; Walkup et al. 2009). Supervision activities included case discussions, role-plays, adherence ratings, and live or video observation. Fifteen articles (38.46%) described procedures for fidelity monitoring of CHW-delivered interventions. Fidelity monitoring included review of case notes, CHWs completing fidelity checklists, behavior observations of sessions, and review of session materials (e.g., review of trauma narratives; Neuner et al. 2008).
Objective 2: Contrast Characteristics of LMIC and US Studies of CHW-Involved Mental Health Interventions
Chi square analyses were conducted to examine potential differences between trials conducted in LMICs and the US for the following characteristics (1) evidence-base for the intervention used, (2) the primary role of the CHWs, (3) the study design, (4) clients served and (5) descriptions provided for implementation support. For the evidence-base and primary role analyses, which had more than two categories, post-hoc analyses were conducted to determine which categories were significantly different across settings. Based on recommendation for protecting against Type 1 error, a cell-wise adjusted residual method was used, with the Bonferroni correction made (MacDonald and Gardner 2000). Based on this correction, alpha levels were set at 0.017 to determine if there were significant differences in the categories between trials in LMICs and the US.
Omnibus tests revealed significant differences between settings for the evidence-base for the interventions delivered, χ2 (2) = 18.13, p < .001. Post-hoc analyses indicated trials in LMICs were significantly more likely to test an EBT (n = 10; 38.46%) than US trials (n = 0, 0%), χ2 (1) = 6.76, p = .009; though there were no differences between settings in evidence-informed interventions (e.g., treatments based on cognitive-behavioral therapy without a previously tested protocol), χ2 (1) = 1.10, p = .271. Trials in the US were significantly more likely to test novel interventions (n = 9; 69.2%) than LMICS (n = 1, 3.9%), χ2 (1) = 19.43, p > .001. Overall, the role of the CHW also significantly differed between studies carried out in LMICs and the US, χ2 (2) = 12.29, p = .002, with significant differences in the use of auxiliary roles between the US and LMICs, χ2 (1) = 11.56, p > .001. CHW in trials in the US performed auxiliary roles, such as co-therapy or case management (n = 5; 38.5%), but these roles were never described in trials in LMICs. CHWs in LMICs were involved in stepped-care (n = 3; 11.5%), whereas this role was never reported in trials in the US, but differences were not significant, χ2 (1) = 1.69, p = .230. In both LMICs and the US, CHWs were most frequently the sole providers of interventions (LMICs: n = 23; 88.5%; US: n = 23; 61.5%), with no significant differences between groups, χ2 (1) = 4.00, p = .194. There were no significant differences between settings in the use of RCT as the study design, χ2 (1) = 0.00, p = 1.00. Similarly, the age group served (child/family or adult) did not differ between settings, χ2 (1) = 2.51, p = .113. Regarding implementation supports, there were no significant differences between the studies that provided descriptions of training, χ2 (1) = 0.09, p = .768, supervision, χ2 (1) = 2.73, p = .098, or fidelity monitoring, χ2 (1) = 0.48, p = .485.
Objective 3: Outcomes from RCTs of CHW-Involved Mental Health Interventions
Among the 27 RCTs of CHW-involved mental health interventions, the majority (n = 18; 69.2%) found that the CHW-involved interventions performed significantly better than a comparison condition on the primary mental health outcome measured. Comparing studies conducted in different settings, 72.2% of trials in LMICs (n = 13) found that the intervention groups outperformed the comparison group, whereas 55.6% (n = 5) of trials in the US demonstrated these positive, significant findings. However, these differences in positive outcomes between settings were not significant, χ2 (1) = 0.75, p = .386. Of the four trials reporting on the sustainment of effects at a follow-up assessment, the intervention groups continued to outperform the comparison groups. Regarding the nine trials without significant findings, three were underpowered with fewer than 30 participants in the intervention conditions. Three trials showed significant improvement from baseline to post-intervention clinical scores for the target intervention and active comparison condition (Ginsburg et al. 2012; Moore et al. 2016; Neuner et al. 2008). One of these trials included a no treatment control arm, which did not show similar improvement. The two trials in which CHW primary role was case management did not demonstrate significant findings (Ernst et al. 1999; Waitzkin et al. 2011). Finally, two trials tested the same school-based intervention and found that it did not lead to significant differences from the waitlist control condition in either trial (Jordans et al. 2010; Tol et al. 2014), even though a previous trial of this intervention showed significant improvements in symptomatology (Tol et al. 2008). Control conditions ranged from a waitlist control or no treatment comparison arm (n = 10; 37.0%), to inclusion of a usual care or enhanced usual care services arm (n = 10; 37.0%), to some other active or attention control condition (e.g., educational support; n = 4; 14.8%), to bibliotherapy (n = 1; 3.7%). Bibliotherapy includes the use of written-materials (e.g., books or brochures) as a mode of psychoeducation or treatment.
Discussion
This systematic review revealed a rapid and recent increase in research being conducted on CHW-involved mental health care. In line with the first objective of this review, we identified that CHWs have been involved in delivering mental health interventions to address a range of clinical disorders, including depression, anxiety, psychological trauma, and disruptive behavior disorders. In the majority of trials, CHWs were the sole treatment providers, and delivered or supported EBTs or interventions informed by evidence-based practices. Significant differences existed between settings, with trials in LMICs testing EBTs more frequently than the in US, whereas the studies in the US were more likely to test novel, community developed interventions. Based on this review, evidence suggests that CHW models of mental health service delivery can be effective in addressing global and domestic disparities in care for underserved populations, as two-thirds of the randomized controlled trials demonstrated positive mental health outcomes for traditionally underserved communities over a comparison condition. However, this review also revealed inconsistencies in reporting methods among published studies involving CHWs, which need to be addressed to further our knowledge about how to best replicate efforts to leverage CHWs to address disparities.
More research with CHW-delivered mental health interventions has been conducted in LMICs than in the US, which is likely related to differences in workforce and resources in these two settings (Bruckner et al. 2011; Saraceno et al. 2007; van Ginneken et al. 2012). Not only were more CHW-involved mental health interventions studied in LMICs, the interventions were more likely to be EBTs than the interventions provided in the US. This finding is likely related to a number of factors. In 2008, the WHO launched two initiatives that were dedicated scaling up of EBTs for mental health, neurological, and substance use disorders, especially in LMICs (Barbui et al. 2010; Dua et al. 2011; World Health Organization 2008). These initiatives explicitly recommended using EBTs such as cognitive-behavioral or interpersonal therapy for depression, and parent management training for childhood behavior disorders. Furthermore, a number of domestic regulations regarding who can provide mental health services likely impact the roles that CHWs may occupy in evidence-based intervention delivery. These regulations include insurance requirements about who is allowed to bill for services, along with requirements from the organizations that oversee the implementation of different EBT protocols. For example, Trauma Focused-Cognitive Behavioral Therapy has been tested with CHW as the sole treatment provider in LMICs (Murray et al. 2013, 2015), but in the US providers are required to have a Master's degree in a mental health discipline and professional licensure (https://tfcbt.org/tf-cbt-certification-criteria/).
Given the differences between the US and LMICs in available workforce and regulations governing mental health care delivery, CHWs may fulfill different roles in the delivery of evidence-based mental health interventions in these different settings. Interestingly, studies in LMICs and the US have predominately investigated CHW models where they were the sole providers of the intervention. Differences did exist between settings, with CHW providing auxiliary support more frequently in the US. However, there are very few trials investigated auxiliary or stepped-care models, making it challenging to determine the most effective roles for CHWs, especially in the US where there are barriers to them being the primary providers of evidence-based interventions. Given the disparities that exist in the quality of mental health care for ethnic and racial minorities in the US, findings from LMICs could have important implications for efforts in the US to address mental health disparities. For example, given evidence that CHWs can effectively deliver EBTs, it is possible that their roles and responsibilities domestically could be expanded to meet the needs of communities with access and utilization disparities. Potentially, CHWs may be mobilized to step into the role of primary providers of EBTs in settings with severe workforce shortages, but even in higher resourced settings they may be involved in EBT delivery for individuals with lower levels of need, such as those who would benefit from prevention services. CHW-delivered prevention and early intervention services would allow trained mental health professionals to focus their expertise on individuals who require more intensive services (Acevedo-Polakovich et al. 2013; Patel et al. 2010). However, based on this review, this stepped-care model of mental health care delivery with CHWs has yet to be evaluated in the US. Similarly, CHWs could be incorporated within evidence-based interventions that are delivered by mental health professional, with roles focused on promoting access and engagement (Barnett et al. 2016). Further investigation of CHW-supported delivery of evidence-based interventions is warranted in the US and other developed nations with mental health service disparities.
In order for CHW-delivered evidence-based interventions to be scaled up effectively, it is critical to understand the implementation strategies that are needed to train and support them. Lessons can be drawn from the field of implementation science, which has predominately focused on training Master's-level clinicians to deliver mental health EBTs in community settings. CHWs are likely to require a high level of support through ongoing supervision and consultation, as this is also required for mental health professionals to deliver EBTs with competence (Beidas and Kendall 2010; Herschell et al. 2010). Future research should evaluate the costs of training and supporting CHWs in comparison to mental health professionals. If CHWs require substantially more time and resources than Master's-level clinicians, the benefits of training them to deliver or support EBTs may not be necessary in locations with an adequate professional mental health workforce to meet the needs of local communities. However, in settings with limited professional workforce, it is critical to identify what the minimal versus optimal level of implementation supports are needed to mobilize CHWs to provide evidence-based care. Though high intensity implementation support (e.g., frequent consultation with treatment developers) may aid the effectiveness of services, this is unlikely to lead to long-term sustainability of CHW-delivered interventions (Murray and Jordans 2016).
Several limitations of this review need to be considered. First, the diverse range of clinical interventions, settings, CHW roles, and outcomes evaluated makes it challenging to establish the effectiveness of CHW-involved mental health interventions. The “vote counting” method of synthesis limits the conclusions that can be drawn, in that it gives equal weight to studies regardless of their sample size and effect sizes, but it provides a useful overview of patterns in the literature, which can inform future research (Popay et al. 2006). Though the focus of this review was on outcome studies that included measures of effectiveness for patient-level outcomes, questions related to implementation outcomes also need to be addressed. This review provided a summary of how implementation supports (i.e., training, supervision, and fidelity monitoring) were described in trials, but no conclusions can be drawn from about the amount of training or support the CHW need to deliver or support delivery of mental health care because these descriptions often provided limited details. Finally, as no trials in this review compared CHW to professional mental health interventionists, it cannot be stated whether CHW are as effective as specialized providers.
Importantly, the present review identified several methodological limitations and inconsistencies in reporting of methods in published studies involving CHWs in mental health care delivery, and future research on CHW-involved mental health interventions must continue to address gaps in the current literature. Based on results of this review, we offer several recommendations to improve reporting of methods and CHW characteristics in future publications. First, important characteristics of CHW were not specified in many of the published trials, which may limit the ability of other researchers and systems to replicate and scale-up these efforts. We recommend that trials explicitly describe the educational background, detailed training and supervision procedures of CHW providers for the roles they occupy in mental health intervention delivery, and the criteria used to select them for these roles. Regarding implementation, it is important not only to better specify the training and support that CHW receive, additional research should examine the implementation strategies, such as supervision procedures, that are most effective for CHW delivery of care. In addition, we recommend that future studies report information regarding intervention adherence and fidelity to evaluate the internal validity of the study. With improved reporting on CHW and implementation characteristics, a meta-analysis could help illuminate factors that lead to effective CHW-delivered interventions. Finally, though increasing evidence suggests that CHW-delivered evidence-based interventions can be effective and feasible, the ability to scale-up and sustain these efforts has yet to be established (Murray and Jordans 2016).
As the first systematic review to consolidate literature on CHW-involved mental health care in LMICs and the US, this review provides important insights into how CHW can address global and domestic mental health disparities. Given accumulating evidence that CHW can effectively deliver evidence-based and informed practices, training and supporting CHW to address mental health disparities seems like a promising approach to improve care for under-served communities. As this review also included studies that investigated novel, community informed interventions, it would also be valuable to how these interventions compare in effectiveness to EBTs, which is an important area for future research. However, it is worth noting that studies that tested EBTs or evidence-informed interventions frequently would use community-partnered approaches, such as community-based participatory research, to adapt the treatments to fit with the local cultures and contexts (e.g., Ginsburg et al. 2012; Murray et al. 2013; Papas et al. 2010), and therefore community involvement was present across different types of interventions. Finally, this review also indicates that additional research is needed to understand how to sustain efforts to incorporate CHW into evidence-based interventions both domestically and globally, in order to maximize an enduring impact on mental health disparities.
Acknowledgments
Funding for this project was supported by NIMH K01MH110608 (Barnett).
Footnotes
Conflict of interest: All authors declare that they have no confict of interest.
Compliance with Ethical Standards: Ethical Approval: This article does not contain any studies with human participants or animals performed by any of the authors.
References marked with an asterisk indicate studies included in the systematic review
- Acevedo-Polakovich ID, Niec LN, Barnett ML, Bell KM. Incorporating natural helpers to address service disparities for young children with conduct problems. Children and Youth Services Review. 2013;35:1463–1467. doi: 10.1016/j.childyouth.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Chatterji P, Wells K, Cao Z, Chen CN, Takeuchi D, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services. 2008;59:1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child and Adolescent Psychiatric Clinics of North America. 2010;19:759–774. doi: 10.1016/j.chc.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ali BS, Rahbar MH, Naeem S, Gul A. The effectiveness of counseling on anxiety and depression by minimally trained counselors: A randomized controlled trial. American Journal of Psychotherapy. 2003;57:324–336. doi: 10.1176/appi.psychotherapy.2003.57.3.324. [DOI] [PubMed] [Google Scholar]
- Araya R, Flynn T, Rojas G, Fritsch R, Simon G. Cost-effectiveness of a primary care treatment program for depression in low-income women in Santiago, Chile. American Journal of Psychiatry. 2006;163:1379–1387. doi: 10.1176/ajp.2006.163.8.1379. [DOI] [PubMed] [Google Scholar]
- Ayala GX, Vaz L, Earp JA, Elder JP, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: An examination by role. Health Education Research. 2010;25:815–840. doi: 10.1093/her/cyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ayón C, Peña V, Naddy MBG. Promotoras' efforts to reduce alcohol use among Latino youths: Engaging Latino parents in prevention efforts. Journal of Ethnic & Cultural Diversity in Social Work: Innovation in Theory, Research & Practice. 2014;23:129–147. [Google Scholar]
- Balaji M, Chatterjee S, Koschorke M, Rangaswamy T, Chavan A, Dabholkar H, et al. The development of a lay health worker delivered collaborative community based intervention for people with schizophrenia in India. BMC Health Services Research. 2012;12:1. doi: 10.1186/1472-6963-12-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbui C, Dua T, van Ommeren M, Yasamy MT, Fleischmann A, Clark N, et al. Challenges in developing evidence-based recommendations using the GRADE approach: The case of mental, neurological, and substance use disorders. PLoS Medicine. 2010;7:e1000322. doi: 10.1371/journal.pmed.1000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Barlow A, Mullany B, Neault N, Compton S, Carter A, Hastings R, et al. Walkup JT. Effect of a paraprofessional home-visiting intervention on American Indian teen mothers' and infants' behavioral risks: A randomized controlled trial. The American Journal of Psychiatry. 2013;170:83–93. doi: 10.1176/appi.ajp.2012.12010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Barlow A, Mullany B, Neault N, Goklish N, Billy T, Hastings R, et al. Paraprofessional-delivered home-visiting intervention for American Indian teen mothers and children: 3-year outcomes from a randomized controlled trial. The American Journal of Psychiatry. 2015;172:154–162. doi: 10.1176/appi.ajp.2014.14030332. [DOI] [PubMed] [Google Scholar]
- Barnett ML, Jent JF, Davis EM, White J, Callejas LM, Acevedo-Polakovich ID, Niec LN. The development and evaluation of a natural helper training program to increase the engagement of urban, Hispanic families in parent-child interaction therapy. Children and Youth Services Review. 2016;65:17–25. doi: 10.1016/j.childyouth.2016.03.016. [DOI] [Google Scholar]
- Barry CL, Huskamp HA. Moving beyond parity—mental health and addiction care under the ACA. New England Journal of Medicine. 2011;365:973–975. doi: 10.1056/NEJMp1108649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bass J, Neugebauer R, Clougherty KF, Verdeli H, Wickramaratne P, Ndogoni L, et al. Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes. The British Journal of Psychiatry. 2006;188:567–573. doi: 10.1192/bjp.188.6.567. [DOI] [PubMed] [Google Scholar]
- Becker AE, Kleinman A. Mental health and the global agenda. New England Journal of Medicine. 2013;369:66–73. doi: 10.1056/NEJMra1110827. [DOI] [PubMed] [Google Scholar]
- Beidas RS, Kendall PC. Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective. Clinical Psychology: A Publication of the Division of Clinical Psychology of the American Psychological Association. 2010;17:1–30. doi: 10.1111/j.1468-2850.2009.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, et al. Group interpersonal psychotherapy for depression in rural Uganda: A randomized controlled trial. JAMA: The Journal of the American Medical Association. 2003;289:3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- *.Bolton P, Bass JK, Zangana GAS, Kamal T, Murray SM, Kaysen D, et al. A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry. 2014a;14:1–15. doi: 10.1186/s12888-014-0360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, Robinson C, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PloS Med. 2014b doi: 10.1371/journal.pmed.1001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruckner TA, Scheffler RM, Shen G, Yoon J, Chisholm D, Morris J, et al. The mental health workforce gap in low-and middle-income countries: a needs-based approach. Bulletin of the World Health Organization. 2011;89:184–194. doi: 10.2471/BLT.10.082784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttorff C, Hock RS, Weiss HA, Naik S, Araya R, Kirk-wood BR, et al. Economic evaluation of a task-shifting intervention for common mental disorders in India. Bulletin of the World Health Organization. 2012;90:813–821. doi: 10.2471/BLT.12.104133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira DA, Bustos CE, Garcia MS, Ng B, Camacho A. Delivering CBT to rural Latino children with anxiety disorders: A qualitative study. Community Mental Health Journal. 2015 doi: 10.1007/s10597-015-9903-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow JCC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. American Journal of Public Health. 2003;93:792–797. doi: 10.2105/AJPH.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. New York: Guilford Press; 2006. [Google Scholar]
- Coker TR, Elliott MN, Kataoka S, Schwebel DC, Mrug S, Grunbaum JA, et al. Racial/ethnic disparities in the mental health care utilization of fifth grade children. Academic Pediatrics. 2009;9:89–96. doi: 10.1016/j.acap.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Martell CR, Addis ME, Herman-Dunn R, Barlow DH. Behavioral activation for depression. Clinical Handbook of Psychological Disorders: A Step-by-Step Treatment Manual. 2008;4:328–364. [Google Scholar]
- Dua T, Barbui C, Clark N, Fleischmann A, Poznyak V, van Ommeren M, et al. Evidence-based guidelines for mental, neurological, and substance use disorders in low- and middle-income countries: Summary of WHO recommendations. PloS Med. 2011 doi: 10.1371/journal.pmed.1001122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Edelblute HB, Clark S, Mann L, McKenney KM, Bischof JJ, Kistler C. Promotoras across the border: A pilot study addressing depression in Mexican women impacted by migration. Journal of Immigrant and Minority Health. 2014;16:492–500. doi: 10.1007/s10903-012-9765-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ernst CC, Grant TM, Streissguth AP, Sampson PD. Intervention with high-risk alcohol and drug-abusing mothers: II. Three-year findings from the Seattle model of para-professional advocacy. Journal of Community Psychology. 1999;27:19–38. [Google Scholar]
- *.Ertl V, Pfeiffer A, Schauer E, Elbert T, Neuner F. Community-implemented trauma therapy for former child soldiers in Northern Uganda: a randomized controlled trial. JAMA: The Journal of the American Medical Association. 2011;306:503–512. doi: 10.1001/jama.2011.1060. [DOI] [PubMed] [Google Scholar]
- *.Fayyad JA, Farah L, Cassir Y, Salamoun MM, Karam EG. Dissemination of an evidence-based intervention to parents of children with behavioral problems in a developing country. European Child & Adolescent Psychiatry. 2010;19:629–636. doi: 10.1007/s00787-010-0099-3. [DOI] [PubMed] [Google Scholar]
- *.Ginsburg GS, Barlow A, Goklish N, Hastings R, Baker EV, Mullany B, et al. Postpartum depression prevention for reservation-based American Indians: Results from a pilot randomized controlled trial. Child & Youth Care Forum. 2012;41:229–245. doi: 10.1007/s10566-011-9161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gul A, Ali BS. The onset and duration of benefit from counselling by minimally trained counsellors on anxiety and depression in women. The Journal of the Pakistan Medical Association. 2004;54:549–552. [PubMed] [Google Scholar]
- *.Han M, Valencia M, Lee Y, De Leon J. Development and implementation of the culturally competent program with Cambodians: The pilot psycho-social-cultural treatment group program. Journal of Ethnic & Cultural Diversity in Social Work: Innovation in Theory, Research & Practice. 2012;21:212–230. doi: 10.1080/15313204.2012.700494. [DOI] [Google Scholar]
- Herschell AD, Kolko DJ, Baumann BL, Davis AC. The role of therapist training in the implementation of psychosocial treatments: A review and critique with recommendations. Clinical Psychology Review. 2010;30:448–466. doi: 10.1016/j.cpr.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hirani SS, Karmaliani R, McFarlane J, Asad N, Madhani F, Shehzad S. Testing a community derived intervention to promote women's health: Preliminary results of a 3-arm randomized controlled trial in Karachi. Southern Online Journal of Nursing Research. 2010;10:1–10. [Google Scholar]
- *.Hovey JD, Hurtado G, Seligman LD. Findings for a CBT support group for Latina migrant farmworkers in western Colorado. Current Psychology: A Journal for Diverse Perspectives on Diverse Psychological Issues. 2014;33:271–281. doi: 10.1007/s12144-014-9212-y. [DOI] [Google Scholar]
- *.Jordans MJ, Komproe IH, Tol WA, Kohrt BA, Luitel NP, Macy RD, De Jong JT. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: A cluster randomized controlled trial. Journal of Child Psychology and Psychiatry. 2010;51:818–826. doi: 10.1111/j.1469-7610.2010.02209.x. [DOI] [PubMed] [Google Scholar]
- Kakuma R, Minas H, van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, et al. Human resources for mental health care: Current situation and strategies for action. Lancet. 2011;378:1654–1663. doi: 10.1016/S0140-6736(11)61093-3. [DOI] [PubMed] [Google Scholar]
- Katigbak C, Van Devanter N, Islam N, Trinh-Shevrin C. Partners in health: A conceptual framework for the role of community health workers in facilitating patients' adoption of healthy behaviors. American Journal of Public Health. 2015;105:872–880. doi: 10.2105/AJPH.2014.302411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kaufman JA, Zeng W, Wang L, Zhang Y. Community-based mental health counseling for children orphaned by AIDS in China. AIDS Care. 2013;25:430–437. doi: 10.1080/09540121.2012.712661. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clinical Psychological Science. 2013;1(2):170–191. doi: 10.1177/2167702612463566. [DOI] [Google Scholar]
- Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: A conceptual framework. American Journal of Public Health. 2006;96:2113–2121. doi: 10.2105/AJPH.2005.07762821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville BJ. Interpersonal psychotherapy of depression. New York: Basic Books; 1984. [Google Scholar]
- Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, van Wyk BE, et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. The Cochrane Library. 2010 doi: 10.1002/14651858.CD004015.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald PL, Gardner RC. Type I error rate comparisons of post hoc procedures for Chi-Square tables. Educational and Psychological Measurement. 2000;60:735–754. doi: 10.1177/00131640021970871. [DOI] [Google Scholar]
- *.Magaña S, Li H, Miranda E, de Sayu RP. Improving health behaviours of Latina mothers of youths and adults with intellectual and developmental disabilities. Journal of Intellectual Disability Research. 2015;59:397–410. doi: 10.1111/jir.12139. [DOI] [PubMed] [Google Scholar]
- McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs. 2008;27:393–403. doi: 10.1377/hlthaf.27.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Moore AA, Karno MP, Ray L, Ramirez K, Barenstein V, Portillo MJ, et al. Development and preliminary testing of a promotora-delivered, Spanish language, counseling intervention for heavy drinking among male, Latino day laborers. Journal of Substance Abuse Treatment. 2016;62:96–101. doi: 10.1016/j.jsat.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris MB, Chapula BT, Chi BH, Mwango A, Chi HF, Mwanza J, et al. Use of task-shifting to rapidly scale-up HIV treatment services: Experiences from Luska, Zambia. BMC Health Services Research. 2009;9:5–14. doi: 10.1186/1472-6963-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Murray LK, Familiar I, Skavenski S, Jere E, Cohen J, Imasiku M, et al. An evaluation of trauma-focused cognitive behavioral therapy for children in Zambia. Child Abuse & Neglect. 2013;37:1175–1185. doi: 10.1016/j.chiabu.2013.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Jordans MJD. Rethinking the service delivery system of psychological interventions in low and middle income countries. BMC Psychiatry. 2016;16:234–240. doi: 10.1186/s12888-016-0938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Murray LK, Skavenski S, Kane JC, Mayeya J, Dorsey S, Cohen JA, et al. Effectiveness of trauma-focused cognitive behavioral therapy among trauma-affected children in LUSka, Zambia: A randomized clinical trial. JAMA Pediatrics. 2015;169:761–769. doi: 10.1001/jamapediatrics.2015.0580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and US-born black and Latina women from seeking mental health care? Psychiatric Services. 2007;58:1547–1554. doi: 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
- *.Nadkarni A, Velleman R, Dabholkar H, Shinde S, Bhat B, McCambridge J, et al. The systematic development and pilot randomized evaluation of mperezed for alcohol problems, a lay counselor-delivered psychological treatment for harmful drinking in primary care in India: The Premium study. Alcoholism: Clinical and Experimental Research. 2015;39:522–531. doi: 10.1111/acer.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2008;76:686–694. doi: 10.1037/0022-06X.76.4.686. [DOI] [PubMed] [Google Scholar]
- *.Nimgaonkar AU, Menon SD. A task shifting mental health program for an impoverished rural Indian community. Asian Journal of Psychiatry. 2015;16:41–47. doi: 10.1016/j.ajp.2015.05.044. [DOI] [PubMed] [Google Scholar]
- *.O'Donnell K, Dorsey S, Gong W, Ostermann J, Whetten R, Cohen JA, et al. Treating maladaptive grief and post-traumatic stress symptoms in orphaned children in Tanzania: group-based trauma-focused cognitive–behavioral therapy. Journal of Traumatic Stress. 2014;27:664–671. doi: 10.1002/jts.21970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Papas RK, Sidle JE, Gakinya BN, Baliddawa JB, Martino S, Mwaniki MM, et al. Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction (Abingdon, England) 2011;106:2156–2166. doi: 10.1111/j.1360-0443.2011.03518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Papas RK, Sidle JE, Martino S, Baliddawa JB, Songole R, Omolo OE, et al. Systematic cultural adaptation of cognitive-behavioral therapy to reduce alcohol use among HIV-infected outpatients in western Kenya. AIDS and Behavior. 2010;14:669–678. doi: 10.1007/s10461-009-9647-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): A cluster randomized controlled trial. Lancet. 2010;376:2086–2095. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annual Review of Public Health. 2014;35:399–421. doi: 10.1146/annurev-publhealth-032013-182354. [DOI] [PubMed] [Google Scholar]
- *.Petersen I, Bhana A, Baillie K MhaPP Research Programme Consortium. The feasibility of adapted group-based interpersonal therapy (IPT) for the treatment of depression by community health workers within the context of task shifting in South Africa. Community Mental Health Journal. 2012;48:336–341. doi: 10.1007/a10597-011-9429-2. [DOI] [PubMed] [Google Scholar]
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: A Product from the ESRC Methods Programme Version 1 2006 [Google Scholar]
- *.Puffer ES, Green EP, Chase RM, Sim AL, Zayzay J, Friis E, et al. Parents make the difference: A randomized-controlled trial of a parenting intervention in Liberia. Global Mental Health. 2015;2:e15. doi: 10.1017/gmh.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raguram R, Venkateswaran A, Ramakrishna J, Weiss MG. Traditional community resources for mental health: a report of temple healing from India. BMJ: British Medical Journal. 2002;325:38–40. doi: 10.1136/bmj.325.7354.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: A cluster-randomised controlled trial. Lancet. 2008;372:902–909. doi: 10.1016/S0140-6736(08)61400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. American Journal of Preventive Medicine. 2007;33:418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Roll JM, Kennedy J, Tran M, Howell D. Disparities in unmet need for mental health services in the United States, 1997–2010. Psychiatric Services. 2013;64:80–82. doi: 10.1176/appi.ps.201200071. [DOI] [PubMed] [Google Scholar]
- *.Roman LA, Gardiner JC, Lindsay JK, Moore JS, Luo Z, Baer LJ, et al. Alleviating perinatal depressive symptoms and stress: A nurse-community health worker randomized trial. Archives of Women's Mental Health. 2009;12:379–391. doi: 10.1007/s00737-009-0083-4. [DOI] [PubMed] [Google Scholar]
- *.Roman LA, Lindsay JK, Moore JS, Duthie PA, Peck C, Barton LR, et al. Addressing mental health and stress in Medicaid-insured pregnant women using a nurse-community health worker home visiting team. Public Health Nursing. 2007;24:239–248. doi: 10.1111/j.1525-1446.2007.00630.x. [DOI] [PubMed] [Google Scholar]
- *.Rosenberg SA, Robinson C, Fryer GE. Evaluation of paraprofessional home visiting services for children with special needs and their families. Topics in Early Childhood Special Education. 2002;22:158–168. [Google Scholar]
- Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370:1164–1174. doi: 10.1016/S0140-6736(07)61263-X. [DOI] [PubMed] [Google Scholar]
- Saravanan B, Jacob KS, Johnson S, Prince M, Bhugra D, David AS. Belief models in first episode schizophrenia in South India. Social Psychiatry and Psychiatric Epidemiology. 2007;42:446–451. doi: 10.1007/s00127-007-0186-z. [DOI] [PubMed] [Google Scholar]
- *.Sorsdahl K, Myers B, Ward CL, Matzopoulos R, Mtukushe B, Nicol A, et al. Adapting a blended motivational interviewing and problem-solving intervention to address risky substance use amongst South Africans. Psychotherapy Research. 2015;25:435–444. doi: 10.1080/10503307.2014.897770. [DOI] [PubMed] [Google Scholar]
- Stacciarini JMR, Rosa A, Ortiz M, Munari DB, Uicab G, Balam M. Promotoras in mental health: A review of English, Spanish, and Portuguese literature. Family & Community Health. 2012;35:92–102. doi: 10.1097/FCH.0b013e3182464f65. [DOI] [PubMed] [Google Scholar]
- TF-CBT Certification Criteria. Retrieved October 11 2016 from https://tfcbt.org/tf-cbt-certification-criteria/
- *.Tol WA, Komproe IH, Jordans MJ, Ndayisaba A, Ntamutumba P, Sipsma H, et al. School-based mental health intervention for children in war-affected Burundi: A cluster randomized trial. BMC Medicine. 2014;12:1–12. doi: 10.1186/1741-7015-12-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Tol WA, Komproe IH, Susnty D, Jordans MJ, Macy RD, De Jong JT. School-based mental health intervention for children affected by political violence in Indonesia: a cluster randomized trial. JAMA: The Journal of the American Medical Association. 2008;300:655–662. doi: 10.1001/jama.300.6.655. [DOI] [PubMed] [Google Scholar]
- van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera S, Pian J, et al. The effect of non-specialist health workers on people with mental, neurological and substance-abuse disorders in developing countries. The Cochrane Library. 2012 doi: 10.1002/14651858.CD009149.pub2. [DOI] [PubMed] [Google Scholar]
- Viswanathan M, Kraschnewski JL, Nishikawa B, Morgan LC, Honeycutt AA, Thieda P, et al. Outcomes and costs of community health worker interventions: A systematic review. Medical Care. 2010;48:792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]
- *.Waitzkin H, Getrich C, Heying S, Rodríguez L, Parmar A, Willging C, et al. Promotoras as mental health practitioners in primary care: A multi-method study of an intervention to address contextual sources of depression. Journal of Community Health: The Publication for Health Promotion and Disease Prevention. 2011;36:316–331. doi: 10.1007/s10900-010-9313-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Walkup JT, Barlow A, Mullany BC, Pan W, Goklish N, Hasting R, et al. Randomized controlled trial of a paraprofessional-delivered in-home intervention for young reservation-based American Indian mothers. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:591–601. doi: 10.1097/CHI.0b013e3181a0ab86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Weiss WM, Murray LK, Zangana GAS, Mahmooth Z, Kaysen D, Dorsey S, et al. Community-based mental health treatments for survivors of torture and militant attacks in southern Iraq: A randomized control trial. BMC Psychiatry. 2015;15:1–16. doi: 10.1186/s12888-015-0622-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry. 2001;158:2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- *.Williamson AA, Knox L, Guerra NG, Williams KR. A pilot randomized trial of community-based parent training for immigrant Latina mothers. American Journal of Community Psychology. 2014;53:47–59. doi: 10.1007/s10464-013-9612-4. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Mental Health Gap Action Programme: Scaling up care for mental, neurological, and substance use disorders. Geneva: WHO Press; 2008. [PubMed] [Google Scholar]
- Packages of interventions for family planning, safe abortion care, maternal, newborn and child health. Geneva: WHO Press; 2010. World Health Organization. [Google Scholar]