Abstract
Purpose
Breast cancer patients commonly experience sexual concerns, yet rarely discuss them with clinicians. The study examined patient and provider experiences and preferences related to communication about breast cancer-related sexual concerns with the goal of informing intervention development.
Methods
Patient data (n=28) were derived from focus groups and interviews with partnered and unpartnered women treated for breast cancer reporting sexual concerns. Provider data (n=11) came from interviews with breast cancer oncologists and nurse practitioners. Patient and provider data were analyzed separately using the framework method of qualitative analysis.
Results
Findings revealed individual and institutional barriers to effective communication about sexual concerns and highlighted key communication facilitators (e.g., a positive patient-provider relationship, patient communication as a driver of provider communication and vice versa). Patients expressed preferences for open, collaborative communication; providers expressed preferences for focused intervention targets (identifying concerns, offering resources/referrals) and convenient format. A model of effective communication of sexual concerns was developed to inform communication interventions.
Conclusions
Findings suggest that to improve patient-provider communication about sexual concerns, knowledge and skills-based interventions that activate patients and that equip providers for effective discussions about sexual concerns are needed, as are institutional changes that could incentivize such discussions.
Keywords: Breast Cancer, Communication, Patient-Provider Communication, Qualitative Research, Sexuality
Background
Over 90% of women diagnosed with breast cancer will survive 5 years beyond their diagnosis [1], making quality of life concerns such as sexuality highly significant. Up to 70% of breast cancer survivors report sexual function disturbances [2], compared to 43% of women ages 18–59 in a national U.S. probability sample [3]. Commonly reported distressing sexual sequelae of breast cancer treatment include vaginal dryness [4–6], loss of libido [6], and decreased sexual activity [7]. Concerns with body image is also common and associated with worse sexual functioning [4, 8, 9] and disruption in survivors’ intimate relationships [10].
Effective treatments are available to help women cope with post-treatment sexual concerns [11–13], but many women do not learn of these options because these concerns are not typically raised during the course of their clinic visits [14]. As a point of comparison, although rates of sexual concerns are comparable across survivors of breast and prostate cancer [15], in one large study of cancer survivors, most (80%) men diagnosed with prostate cancer reported discussing sexual concerns with their cancer providers, whereas only one third of women with breast cancer reported such discussions [16]. Many breast cancer survivors would like information about sexual health [17, 18]. Research both in both cancer and non-cancer populations has demonstrated that the absence of clinical discussion about sexual function and activity is associated with negative effects for patients’ sex lives, such as decreased sexual activity or worse sexual morbidity [19, 20]. Thus, improving communication about sexual concerns in this population should be a high priority in clinical care.
Communicating effectively about sexual concerns in the context of cancer is challenging [21–25], and in breast cancer barriers such as emotional discomfort and lack of knowledge can impede communication [17, 26]. Yet little information is available to guide the development of interventions that could enhance patient-provider communication about sexual concerns in this population. For instance, understanding patients’ and providers’ needs and preferences for communication about sexual concerns and for related interventions could help to identify critical content areas for an intervention as well as guide the selection of an appropriate intervention format. In this study, we characterize the experiences, needs, and intervention preferences of breast cancer survivors and healthcare providers with respect to patient-provider communication about sexual concerns in an effort to inform intervention development. The qualitative investigation was guided by two major influences: 1) social cognitive theory [27], particularly the role of beliefs as potential factors influencing patient-provider communication about sexual concerns in cancer; and 2) prior work on barriers and facilitators of such communication [23, 28–30].
Methods
Setting and Recruitment
Participants
The patient sample was recruited from a comprehensive cancer center, whose patients would be served by interventions being designed, and the sample reflects the breast cancer population treated in this center. Adult women with a breast cancer diagnosis were eligible if they had received any treatment for breast cancer and scored ≥ 3 on a sexual concerns screening item [31–33]. Medical oncology providers treating breast cancer patients (physicians, advanced practice nurses) were eligible. Provider participants were recruited from four cancer centers or community hospitals in or near Philadelphia offering cancer care (two urban, two suburban).
Procedures
The study protocol and procedures were approved by the Fox Chase Institutional Review Board. Medical data for patient participants were obtained through chart review. A convenience sampling approach was used to recruit (i.e., mailings to patients identified using the institutional tumor registry, flyers, and in-clinic recruitment). Providers were recruited through contact with the PI after identification through oncology colleagues or by Fox Chase staff who coordinate affiliate sites. Participants were reimbursed $75 for their time.
Qualitative Data Collection
Interviews and focus groups followed a semi-structured format that focused on areas of sexual concern, experiences of patient-provider communication, barriers to and beliefs about such communication, and desired aspects of communication and/or interventions (See Supplemental Table for sample questions). Overall, 20 transcripts from 11 provider interviews, five focus groups with partnered breast cancer survivors, and 4 interviews with unpartnered breast cancer survivors were coded. Data collection ceased when investigators determined that the focus groups and interviews were not generating new themes, suggesting that sufficient data had been collected to inform intervention development. Interviews were conducted with the unpartnered participants (rather than focus groups) because of difficulties in scheduling focus groups in this patient subgroup. Field notes were taken during all focus groups and interviews to aid analysis but were coded only for one interview in which there were audio recording difficulties. Separate focus groups and interviews were conducted with younger women (age ≤45 at diagnosis) and unpartnered women, respectively, because these groups may have unique concerns [8, 34]. The PI (JBR) led all groups and conducted provider interviews; a breast cancer survivor and survivorship expert (EB) co-led three focus groups.
Qualitative Data Analysis
Transcripts were content analyzed using the framework method, a systematic qualitative analytic approach that culminates in the development of a matrix output, a summary of the data by case and code that allows for analysis across and within cases [35, 36]. As recommended in the framework approach to qualitative analysis, the provider and patient data were analyzed separately, with the aim of developing unique codes and separate framework matrices. Across both data sets, the following analytic process was implemented: (1) independent coders conducted open coding of written transcripts (not using software) to generate a preliminary list of codes; (2) coders then had in-depth discussions to review codes and concepts and classify them into distinct and theoretically meaningful codes and then reclassify them into higher level themes; (3) N Vivo 10 software (QSR International) was then used to apply the coding scheme to all of the interview data; and (4) framework matrices were created to facilitate the contrast of codes both within and across cases (transcripts) and to determine thematic coverage. At the third stage, two trained coders independently applied codes to 60% of the data. In this stage of analysis, discrepancies between coders were identified and discussed until consensus was reached [37]. These discussions also promoted consistency in the application of codes. In the few instances of difficulties in reaching consensus, a third member of the team was consulted to make a final determination. For the remainder of the transcripts, one coder applied the codes to the transcripts after detailed discussion of themes. Within the patient data, 2 theme occurrences were missing (of 72 possible instances), indicating 97% thematic coverage; in the provider data, none of a possible 88 theme occurrences were missing, suggesting that thematic saturation was obtained [38].
Results
Sample Characteristics
The patient sample (n=28) was predominantly white (71%) or African American (21%), married (82%), college-educated (68% completed college or graduate degree), and employed full or part-time (68%). Ninety-three percent were diagnosed with early stage disease and most had received chemotherapy (89%) and/or radiation (75%). Eighteen percent of patients had completed chemotherapy in the previous 6 months, whereas the remainder of the women who had received chemotherapy completed this treatment at least 6 months prior. About one third of the sample were on tamoxifen (36%) or an aromatase inhibitor (36%); most had either mastectomy with reconstruction (50%) or lumpectomy (46%); 4% had mastectomy without reconstruction. Providers consisted of seven medical oncologists and four advanced practice nurses. Six of the providers were female, eight were white, and only one had < 5 years in practice.
Qualitative Themes Identified in Patient or Provider Data
Patient Communication Behaviors
Although some patients did not raise sexual concerns with providers, potentially because they were unprepared for what or how to do so (Table 1, Quote 1), others reported a wide range of communications with their provider related to sexual concerns. Generally, the women who raised sexual concerns tended to be those suffering from pronounced sexual distress, with some raising concerns they felt should have been addressed by a provider. For instance, one woman reported that “I think I actually had to say to the surgeon, ‘so will I be able to feel my breasts?’” Unpartnered women reported themselves to be sexually inactive. We surmised that perhaps for this reason, they seemed relatively more likely to speak about concerns about body image rather than sexual function concerns compared to the partnered women. For instance, one unpartnered patient commented that “Nobody brought it [sex] up and I didn’t bring it up because it wasn’t an issue with me. If it was an issue, I would have asked somebody.” Some providers also reported that women often did not raise sexual concerns, particularly concerns regarding libido or dyspareunia (Table 1, Quote 2).
Table 1.
Qualitative themes with illustrative quotes
| Theme | Illustrative Patient Quotes | Illustrative Provider Quotes |
|---|---|---|
| Patient Communication Behaviors | (1) “I think I should have asked as well. I just…thought it would eventually get better and be all right. I didn’t know to say.” | (2) “I have been a nurse practitioner doing breast cancer for 13 years…it is clearly the minority that will bring up libido issues or dyspareunia issues…” |
| Provider Communication Behaviors | (3) “I was asked about pain, physical pain in general, but…none of my doctors here have ever mentioned anything about sex.” | (4) “I generally don’t bring it up until they are done with chemo or if they are already on their hormonal therapy, and just ask as part of the routine follow-up questions.” |
| Patient Communication Barriers | (5) “[It’s] difficult to bring [sexual issues] up, or to talk about it with someone until you feel…really comfortable with them.” | (6) “…you don’t want to place a barrier between the patient-physician relationship so I think if there is a perception on my part that the patient is not going to welcome this conversation, I might not delve deeply into… something like that.” |
| Provider Communication Barriers | (7) “…for me it wasn’t so much time, but the barrier was when you first bring it up…the reaction that you get from your provider. It’s like ok, let me look at this file, let me look at this computer.” | (8) “…from the very beginning in medical school we are not really taught well how to communicate about these issues…Ob/Gyn…and urology, they are dealing specifically with the organ systems…” |
| Communication Facilitators | (9) “[I remember] her just saying, like, ‘this is what I am here for. This is my job…And if you are having an issue that was caused by something…like chemo, I want to be a part of helping you resolve that issue.’ | (10) “I think a good example…was a young patient who is currently sexually active and she was very forward…and we were able to have a very open discussion...” |
| Contextual Factors | (11) “I think when you come here for the very first time, I don’t think that is the time…when I was first diagnosed I certainly was not thinking about the next time I am having sex.” | (12) “[The specialist] actually came out and did a big discussion in terms of what to look for, what she can do in terms of interventions and therapeutic options, and so I have referred patients to her as well as my other associates.” |
| Communication/Intervention Preferences | (13) “I would have liked to hear something to the effect that, ‘…your sexual desire is going to diminish and that is normal…But if in three months from now you don’t feel better about your sexual desire…let’s talk about it...’” | (14) “I think it would be great for you to give a 10 minute overview in terms of what is known about the subject, because I came into this cold… I don’t know the background research.” |
Provider Communication Behaviors
Providers’ communication with respect to sexual concerns reflected a range of practice patterns, from avoiding such discussions (Table 1, Quote 3), to routinely asking about sexual concerns during clinical assessments (Table 1, Quote 4), to asking about some concerns (e.g., vaginal dryness) but not others (e.g., loss of libido), as with one provider who commented that “…I think that is probably an error in our screening…that [libido] is not routinely asked.” However, the vast majority of providers mentioned not discussing sexual concerns at least once in their interview. Further, although one nurse practitioner who focused on survivorship felt that she had the ability and time to delve into sexual concerns clinically, only a few other providers offered patients suggestions for dealing with motivational or emotional types of sexual problems and they tended to use referral sources in such cases. As one provider commented, “…in terms of decreased libido, decreased intimacy, I don’t feel as comfortable with that. That is where Dr. [referral source] comes in.” Indeed, some patients remarked of a tendency of providers to refer them elsewhere if sexual concerns were mentioned rather than to discuss them, leading to the potential to feel somewhat cast aside. As one patient remarked, “If it [the concern] had to do with sexual function you were referred to a support group. It takes me an hour to get here and so that wasn’t feasible for me...”
Patient Communication Barriers
Though a range of patient communication barriers were identified, the strongest barriers tended to be negative beliefs about discussing sexual concerns or feelings of emotional discomfort, which a number of patients pointed out made them less likely to raise sexual concerns (Table 1, Quote 5). One woman hinted that her own behavior seemed to reinforce the belief – held by her and potentially the provider as well – that discussions of sexual concerns are of low priority, noting that “it [sex] always gets tagged on, and I guess it is my fault too but it is always the last thing we discuss so therefore it is always the most rushed and I feel like they have one leg out the door.” However, other women lacked an awareness of potential sexual concerns and this lack of awareness served as a barrier to their raising sexual concerns (Table 1, Quote 1). Providers also perceived patient barriers to their discussion of sexual concerns. For instance, some providers worried that raising sexual concerns with patients who were uncomfortable could have detrimental effects on the patient-provider relationship (Table 1, Quote 6). As another example, when asked what should be addressed in an intervention for providers on how to discuss sexual concerns clinically, one provider commented: “I think it would help to know who wants [this information because] you can’t force this information on someone if they really don’t want to hear it.”
Provider Communication Barriers
Like patient barriers, provider barriers to communication also often consisted of negative beliefs about discussing sexual issues clinically, such as the belief that sexual concerns are of low priority. However, almost all providers also commented on knowledge or skills gaps that served as barriers (Table 1, Quote 8). For instance, one provider noted, “I think it is a major issue that they are dealing with and I am the first to say that I don’t necessarily have the skills to deal with it [sex].” Several providers mentioned being reluctant to raise sexual concerns without knowledge of available treatments, as one provider commented, “…I think part of it is [that] I don’t want to ask a question that I don’t have a solution for it.” Yet, even for providers who felt skilled at counseling patients on sexual concerns, the belief that there was inadequate time to discuss sexual concerns during clinic visits impeded communication. For instance, one of the nurse practitioners commented, “I feel very comfortable talking about sexual issues…I talk to them about the fact that…you don’t have interest in sex anymore, you have to try to think about what brought your interest in the past…I really do think that the biggest barrier is…oh my God, I need to get to my next patient.” Another provider commented, “I don’t talk in too much detail with them because of the time constraints and there are other things that I am trying to cover with them.” Time constraints could also be considered a potential contextual factor, discussed below, in that providers described experiencing realistic constraints on the time allowed for their clinic visits. Several patients cited the expectation of a dismissive reaction from the provider as a barrier (Table 1, Quote 7). Similarly, another patient acknowledged that feeling rushed makes her less likely to raise any concerns, stating, “I think that [question] would be one…that I wouldn’t ask because I feel like I would get a quick half-assed answer because she has to get out and get to her next patient.” Finally, one patient commented on the importance of providers’ confidence by commenting that “if they [the providers] come across [as] nervous you are not going to open up to them.”
Communication Facilitators
Both patients and providers described trust as a key characteristic of a positive patient-provider relationship that could facilitate effective communication about sexual concerns. As one patient noted, “I feel like I am comfortable enough with my oncologist…to be personal like that. I feel that when I tell her my comment about what I would sexually be doing with my husband it would be confidential.” The patients who discussed experiences of effective communication believed that their expressions of sexual concerns would be well-received by their providers. This is evident in the quote from one patient who reported receiving reassurance from her provider that any treatment-related sexual concerns she experienced could be dealt with appropriately (Table 1, Quote 9). For providers, some commented that positive prior experiences in discussing sexual concerns with patients had led them to feel more comfortable discussing sexual concerns, and hence, more likely to discuss such concerns with their patients. For example, when asked about his/her level of confidence about discussing sexual concerns, one provider noted, “I think I have become much more comfortable discussing it and really it has been the patients that have volunteered the information that made me feel more comfortable to be able to ask other patients about it.” Several providers also commented on the importance of patient communication as a driver, or facilitator, of their communication (Table 1, Quote 10). Moreover, one provider commented that “time is a barrier and may not let you explore things as much as you think they need to unless the patient is giving you signals that they need something,” suggesting that patients’ communication could drive discussions about sexual concerns even in the context of time constraints. Although few providers reported having received any specialized training or education about discussing sexual concerns with their patients, the few who had described this experience as being helpful in giving them awareness of referral options and confidence to discuss sexual concerns clinically with their patients.
Contextual Factors
Contextual factors included patient factors (e.g., age, cultural background), provider factors (e.g., provider role, gender), and institutional or organizational factors (e.g., clinic practice, availability of referral sources) that patients and providers believed could influence communication about sexual concerns. As an example, whereas some patients felt that the consultation appointment would have been a poor time to discuss sexual concerns (Table 1, Quote 11), others noted that discussing sexual concerns early on could start a “continuous conversation” beginning with information about potential treatment effects on sexual health. With regard to patient age, although discussions with providers about sexual concerns appeared to be more common for the younger women, this need not be static, as one provider noted, “I also have a number of open patients…in their 50’s and 60’s who are open and wanted to ask sexual discussions… I learned through this process that I really do need to focus on older patients as well.” Another important contextual factor was the availability of a competent referral source for a provider which – if present – could facilitate clinical discussions (Table 1, Quote 12). Finally, relative to the physicians, the nurse practitioners tended to report deeper clinical discussions about sexual concerns, and some patients also noticed this. For example, one patient commented that “none of my doctors here have ever mentioned anything about sex…it is the nurses who tell you things.”
Communication or Intervention Preferences
A common thread within patients’ communication preferences was the notion of collaboration between patients and providers. For example, one unpartnered woman suggested that a provider might say to her, “‘I know you are…not married, but here is some information that I know you can use…’ so it is up to me whether or not I want to [use it].” Some patients hoped their providers would specifically ask about sexual concerns and normalize their concerns (Table 1, Quote 13); others cited a preference for information to be delivered with a balance of empathy and directness. Providers highlighted several key content areas they wanted to see in a provider-focused communication intervention, including the etiology of breast cancer-related sexual function disturbances (Table 1, Quote 14), current research on treatments, and skills training. Providers generally agreed that at minimum the breast cancer care provider could “identify whether or not this is an issue…then adequately refer for those with more detailed issues that we can’t handle…” Although providers reported a range of individual preferences for intervention formats, including a web-based approach, an in-service type of format, or even a podcast, they tended to agree that convenience and brevity were critical. Providers also acknowledged the important role of patient education, shown in the comment of one provider who noted that “I also think patients can drive this agenda…if patients ask, you are not going to say no…So if you educate patients that this is important, that they have a right to have this issue addressed, I think it will move the field.”
Additional Themes from Patient Data
Three themes emerged uniquely from the patient data: experiences of sexual and general health concerns following treatment; information and support needs with respect to sexuality; and past positive or negative communication experiences. Vaginal dryness, described by one woman as “sand paper” that “has not gotten any better two to three years later,” was the most commonly discussed type of sexual concern, whereas libido, breast changes, body image, dating concerns (for unpartnered women), and orgasmic difficulties were commonly experienced but hardly ever mentioned with providers. Yet despite this wide range in experiences of sexual concerns, women’s reported information needs fell into just a few key areas, including whether sex was safe (e.g., during chemotherapy, after surgery), preparation for treatment-related sexual difficulties, e.g., a leaflet “that gives you all of the information how your body is going to change from the chemo,” and methods to cope with sexual concerns. Finally, women who described either negative or positive prior communication experiences commonly cited resulting negative or positive emotions and a corresponding decrease or increase in the likelihood of raising the issue again. For instance, whereas one woman reported that “I always had to bring it up…it was so uncomfortable and embarrassing that I never brought it up with her again,” another woman reported that “I have a really good relationship with [my oncologist] where I am comfortable bringing it [sexual issues] up and…now every time I come she says, ‘How is it going?’ She makes me feel comfortable enough to continue to bring it up.”
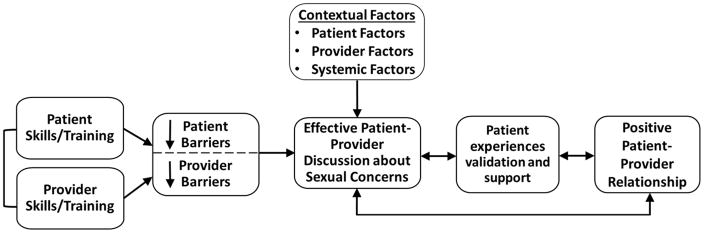
Model of Effective Patient-Provider Communication about Sexual Concerns
A conceptual model was developed to guide efforts at promoting effective patient-provider communication about sexual concerns. An effective discussion about sexual concerns is defined as one that meets patients’ information needs and fosters a positive patient-provider relationship (i.e., one that is characterized by mutual trust and respect). As shown in Figure 1, key implications of this model are that (a) effective communication can be self-sustaining, (b) knowledge and skills-based interventions for patients and providers could each result in effective discussions about sexual concerns, (c) a mechanism through which patient and provider interventions could lead to effective discussions is through increasing positive beliefs about such communication, such as that discussions of sexual concerns are important, need not take very long to accomplish, and will be well-received, and (d) contextual factors consisting of patient, provider, and systemic factors can influence whether discussions are effective and should be addressed in interventions.
Figure 1.
Model of Effective Patient-Provider Communication about Sexual Concerns in Cancer
Discussion
Although prior research has highlighted differences in cancer providers’ and patients’ perspectives on communication about sexual concerns [23], findings from the current study suggested intriguing areas of overlap in these perspectives. First, both patients and providers recognized that there were multiple and multi-level (e.g., individual, institution-wide) challenges to effective patient-provider communication about sexual concerns. Second, patients and providers acknowledged the mutual influence of communication by the other group as driving their own. Third, in recalling effective discussions of sexual concerns, some patients and providers offered notable positive examples of discussions which they described as occurring against a backdrop of a trusting patient-provider relationship. Finally, although both patients and providers expressed individual communication or intervention preferences, patients generally sought open and collaborative communication characterized by the provider raising the discussion and the patient deciding on the path of action. Providers cited individual preferences for intervention format but agreed that a feasible intervention aimed at improving their communication with breast cancer patients about sexual concerns should be convenient, brief, and primarily target identifying patients with concerns and offering referrals/resources. Provided patients are given first-line written information to prepare them for sexual changes, the safety of sexual activity, and sexual rehabilitation, such a focused provider approach to interventions may be appropriate.
Clinical Implications
A key implication of the proposed model of effective patient-provider communication about sexual concerns is that a multi-pronged approach utilizing both patient-focused and provider-focused interventions is necessary to improve clinical discussions about sexual concerns. Although this model was derived from breast cancer patient and provider data, the emergent themes echo those found using other cancer samples [28, 39, 40], suggesting the model may have applicability beyond breast cancer. Within this approach, a skills-based patient-focused intervention could help patients identify and prioritize their concerns, normalize the concerns and the expression of such concerns, and offer basic communication skills practice. By offering education and training in key communication skills (e.g., asking questions, normalizing patients’ concerns), a provider-focused intervention could foster the development of positive provider beliefs (i.e., that sexual concerns are important to discuss clinically, that discussions of sexual concerns need not take long clinically), and decrease providers’ emotional discomfort in having discussions about sexual concerns. Although few prior studies have evaluated patient-provider communication interventions about cancer-related sexual concerns [41, 42], findings from this study suggest that activating patients (i.e., increasing awareness, self-advocacy, and communication skills) to discuss sexual concerns may ultimately be one of the most critical strategies for driving increased provider communication. Interestingly, some women in this study reported feeling cast aside when given referrals that did not meet their needs. This suggests the importance of openly discussing the rationale for making a referral as well as offering clear expectations for a specialist visit. Additionally, the incorporation of electronic health records prompts and symptom summaries could help identify patients in need of clinical discussion [43, 44] while institutional policies that promote delivery of clinical practice guidelines around sexual function (e.g., NCCN Clinical Practice Guidelines for Sexual Function) [45, 46] might increase such discussions, though this has not yet been tested. Moreover, because contextual factors (e.g., patient age, partner in the room) may influence communication, such factors should be addressed in interventions even if they cannot be directly modified. Overall, findings from this qualitative study support the notion that effective communication about sexual concerns can validate patients’ concerns, cement a positive patient-provider relationship, and lead to support and solutions.
Limitations
Several limitations of this study warrant consideration. First, given the scope and goal of this study, the sample was recruited from a clinic population, and included everyone who expressed willingness to participate. The sample is unintentionally skewed towards more highly educated women, and those with early stage disease, which may create concerns regarding generalizability. There is a need to ensure accessibility of communication interventions to women with more limited education and for additional research as to the needs of women with advanced disease. Second, the study sample was heterosexual and mostly made up of white women; future studies should examine the communication needs and preferences of women across other sexual orientations and racial groups with large enough samples to do so. Third, relatively few unpartnered women enrolled in the study and those who did reported relatively few sexual concerns. Yet clinical experience suggests that unpartnered women may experience issues with vaginal dryness and other sexual concerns; these issues could go unaddressed if providers assume that sexual concerns need not be discussed with unpartnered women because of their lack of an intimate partner. Additional research should focus on the needs of this understudied group. However, the study has several strengths, including rigorous qualitative methods conducted separately with patients and providers and findings that may help inform interventions addressing the undertreated issue of sexual concerns in cancer.
Supplementary Material
Relevance to inform research, policies, and/or programs.
Sexual concerns are among the most common, distressing, and persistent supportive care concerns experienced by breast cancer survivors. Improving communication about sexual concerns should therefore be a high priority in clinical care. Key implications of the model developed to explain effective patient-provider communication about sexual concerns in the context of breast cancer are that effective communication can be self-sustaining, that skills-based interventions for patients and providers could each enhance communication potentially through increasing positive beliefs about such communication and contextual factors consisting of patient, provider, and systemic factors can influence whether discussions are effective. Effective communication about sexual concerns is important because it can validate patients’ concerns, underscore a positive patient-provider relationship, and lead to the adoption of strategies supporting patients’ health and relationship outcomes.
Acknowledgments
This study was supported by a Mentored Research Scholar Grant (MRSG-14-031-CPPB) from the American Cancer Society and R21CA191354 from the National Cancer Institute. Dr. Reese is also supported by P30CA006927 from the National Cancer Institute.
Footnotes
Compliance with Ethical Standards
The funding agencies had no role in the conduct of this study and the authors declare they have no conflicts of interest to report. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. This article does not contain any studies with animals performed by any of the authors.
References
- 1.Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, et al. SEER Cancer Statistics Review, 1975–2013. National Cancer Institute; Bethesda, MD: Apr, 2016. http://seer.cancer.gov/csr/1975_2013/, based on November 2015 SEER data submission, posted to the SEER web site. [Google Scholar]
- 2.Panjari M, Bell RJ, Davis SR. Sexual Function after Breast Cancer. J Sex Med. 2011;8:294–302. doi: 10.1111/j.1743-6109.2010.02034.x. [DOI] [PubMed] [Google Scholar]
- 3.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 4.Boquiren VM, Esplen MJ, Wong J, Toner B, Warner E, Malik N. Sexual functioning in breast cancer survivors experiencing body image disturbance. Psychooncology. 2016;25:66–76. doi: 10.1002/pon.3819. [DOI] [PubMed] [Google Scholar]
- 5.Ussher JM, Perz J, Gilbert E. Perceived causes and consequences of sexual changes after cancer for women and men: a mixed method study. BMC Cancer. 2015;15:268. doi: 10.1186/s12885-015-1243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Safarinejad MR, Shafiei N, Safarinejad S. Quality of life and sexual functioning in young women with early-stage breast cancer 1 year after lumpectomy. Psychooncology. 2013;22:1242–1248. doi: 10.1002/pon.3130. [DOI] [PubMed] [Google Scholar]
- 7.Lee M, Kim YH, Jeon MJ. Risk factors for negative impacts on sexual activity and function in younger breast cancer survivors. Psychooncology. 2015;24:1097–1103. doi: 10.1002/pon.3772. [DOI] [PubMed] [Google Scholar]
- 8.Fobair P, Stewart SL, Chang SB, D’Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psychooncology. 2006;15:579–594. doi: 10.1002/Pon.991. [DOI] [PubMed] [Google Scholar]
- 9.Pesek S, Onstad M, Fogarty S, Stuckey A, Raker C, Clark M, Kunkel E, Gass J. Sexual Function After Breast Cancer Surgery. Gynecol Oncol. 2015;139:588. doi: 10.1016/j.ygyno.2015.09.033. [DOI] [Google Scholar]
- 10.Reese JB, Porter LS, Casale KE, Bantug ET, Bober SL, Schwartz SC, Smith KC. Adapting a couple-based intimacy enhancement intervention to breast cancer: A developmental study. Health Psychol. 2016;35:1085–1096. doi: 10.1037/hea0000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seav SM, Dominick SA, Stepanyuk B, Gorman JR, Chingos DT, Ehren JL, Krychman ML, Su HI. Management of sexual dysfunction in breast cancer survivors: a systematic review. Women’s Midlife Health. 2015;1:1–27. doi: 10.1186/s40695-015-0009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carter J, Goldfrank D, Schover LR. Simple Strategies for Vaginal Health Promotion in Cancer Survivors. The Journal of Sexual Medicine. 2011;8:549–559. doi: 10.1111/j.1743-6109.2010.01988.x. [DOI] [PubMed] [Google Scholar]
- 13.Melisko ME, Goldman M, Rugo HS. Amelioration of sexual adverse effects in the early breast cancer patient. J Cancer Surviv. 2010;4:247–255. doi: 10.1007/s11764-010-0130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reese JB, Sorice K, Beach MC, Porter LS, Tulsky JA, Daly MB, Lepore SJ. Patient-Provider Communication about Sexual Concerns in Cancer: A Systematic Review. J Cancer Surviv. 2016 doi: 10.1007/s11764-016-0577-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crowley SA, Foley SM, Wittmann D, Jagielski CH, Dunn RL, Clark PM, Griggs JJ, Peterson C, Leonard M, An LC, Wei JT, Montie JE, Janz NK. Sexual Health Concerns Among Cancer Survivors: Testing a Novel Information-Need Measure Among Breast and Prostate Cancer Patients. J Cancer Educ. 2015:1–7. doi: 10.1007/s13187-015-0865-5. [DOI] [PubMed] [Google Scholar]
- 16.Flynn KE, Reese JB, Jeffery DD, Abernethy AP, Lin L, Shelby RA, Porter LS, Dombeck CB, Weinfurt KP. Patient experiences with communication about sex during and after treatment for cancer. Psychooncology. 2012;21:594–601. doi: 10.1002/pon.1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ussher JM, Perz J, Gilbert E. Information needs associated with changes to sexual well-being after breast cancer. J Adv Nurs. 2012;69:327–337. doi: 10.1111/j.1365-2648.2012.06010.x. [DOI] [PubMed] [Google Scholar]
- 18.Hill EK, Sandbo S, Abramsohn E, Makelarski J, Wroblewski K, Wenrich ER, McCoy S, Temkin SM, Yamada SD, Lindau ST. Assessing gynecologic and breast cancer survivors’ sexual health care needs. Cancer. 2011;117:2643–2651. doi: 10.1002/cncr.25832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindau ST, Gavrilova N, Anderson D. Sexual morbidity in very long term survivors of vaginal and cervical cancer: a comparison to national norms. Gynecol Oncol. 2007;106:413–418. doi: 10.1016/j.ygyno.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindau ST, Abramsohn E, Gosch K, Wroblewski K, Spatz ES, Chan PS, Spertus J, Krumholz HM. Patterns and loss of sexual activity in the year following hospitalization for acute myocardial infarction (a United States National Multisite Observational Study) Am J Cardiol. 2012;109:1439–1444. doi: 10.1016/j.amjcard.2012.01.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perz J, Ussher JM, Gilbert E. Constructions of sex and intimacy after cancer: Q methodology study of people with cancer, their partners, and health professionals. BMC Cancer. 2013;13:270. doi: 10.1186/1471-2407-13-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gilbert E, Perz J, Ussher JM. Talking about sex with health professionals: the experience of people with cancer and their partners. Eur J Cancer Care (Engl) 2016;25:280–293. doi: 10.1111/ecc.12216. [DOI] [PubMed] [Google Scholar]
- 23.Hordern AJ, Street AF. Communicating about patient sexuality and intimacy after cancer: mismatched expectations and unmet needs. Med J Aust. 2007;186:224–227. doi: 10.5694/j.1326-5377.2007.tb00877.x. hor10740_fm [pii] [DOI] [PubMed] [Google Scholar]
- 24.Hordern AJ, Street AF. Constructions of sexuality and intimacy after cancer: patient and health professional perspectives. Soc Sci Med. 2007;64:1704–1718. doi: 10.1016/j.socscimed.2006.12.012. S0277-9536(06)00618-6 [pii] [DOI] [PubMed] [Google Scholar]
- 25.Dyer K, das Nair R. Why Don’t Healthcare Professionals Talk About Sex? A Systematic Review of Recent Qualitative Studies Conducted in the United Kingdom. J Sex Med. 2013;10:2658–2670. doi: 10.1111/j.1743-6109.2012.02856.x. [DOI] [PubMed] [Google Scholar]
- 26.Taylor S, Harley C, Takeuchi E, Brown J, Velikova G. Detecting and Discussing Sexual Problems during Chemotherapy for Breast Cancer. Breast Journal. 2013;19:566–567. doi: 10.1111/tbj.12168. [DOI] [PubMed] [Google Scholar]
- 27.Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice Hall, Inc; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 28.Ussher JM, Perz J, Gilbert E, Wong WKT, Mason C, Hobbs K, Kirsten L. Talking about sex after cancer: A discourse analytic study of health care professional accounts of sexual communication with patients. Psychol Health. 2013;28:1370–1390. doi: 10.1080/08870446.2013.811242. [DOI] [PubMed] [Google Scholar]
- 29.Hordern AJ, Street AF. Let’s talk about sex: risky business for cancer and palliative care clinicians. Contemp Nurse. 2007;27:49–60. doi: 10.5555/conu.2007.27.1.49. [DOI] [PubMed] [Google Scholar]
- 30.Park ER, Norris RL, Bober SL. Sexual Health Communication During Cancer Care: Barriers and Recommendations. Cancer J. 2009;15:74–77. doi: 10.1097/PPO.0b013e31819587dc. [DOI] [PubMed] [Google Scholar]
- 31.Reese JB, Shelby RA, Keefe FJ, Porter LS, Abernethy AP. Sexual concerns in cancer patients: a comparison of GI and breast cancer patients. Support Care Cancer. 2010;18:1179–1189. doi: 10.1007/s00520-009-0738-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reese JB, Shelby RA, Abernethy AP. Sexual concerns in lung cancer patients: an examination of predictors and moderating effects of age and gender. Support Care Cancer. 2011;19:161–165. doi: 10.1007/s00520-010-1000-0. [DOI] [PubMed] [Google Scholar]
- 33.Fortner B, Okon T, Schwartzberg L, Tauer K, Houts AC. The Cancer Care Monitor: psychometric content evaluation and pilot testing of a computer administered system for symptom screening and quality of life in adult cancer patients. J Pain Symptom Manage. 2003;26:1077–1092. doi: 10.1016/j.jpainsymman.2003.04.003. S0885392403004342 [pii] [DOI] [PubMed] [Google Scholar]
- 34.Biglia N, Moggio G, Peano E, Sgandurra P, Ponzone R, Nappi RE, Sismondi P. Effects of Surgical and Adjuvant Therapies for Breast Cancer on Sexuality, Cognitive Functions, and Body Weight. J Sex Med. 2010;7:1891–1900. doi: 10.1111/j.1743-6109.2010.01725.x. [DOI] [PubMed] [Google Scholar]
- 35.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gale NK, Shapiro J, McLeod HS, Redwood S, Hewison A. Patients-people-place: developing a framework for researching organizational culture during health service redesign and change. Implement Sci. 2014;9:106. doi: 10.1186/s13012-014-0106-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42:1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corbin J, Strauss A. Grounded theory research: Procedures, canons, and evaluative criteria. Qual Sociol. 1990;13:3–21. doi: 10.1007/BF00988593. [DOI] [Google Scholar]
- 39.Arora NK, Jensen RE, Sulayman N, Hamilton AS, Potosky AL. Patient-physician communication about health-related quality-of-life problems: are non-Hodgkin lymphoma survivors willing to talk? J Clin Oncol. 2013;31:3964–3970. doi: 10.1200/jco.2012.47.6705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCallum M, Lefebvre M, Jolicoeur L, Maheu C, Lebel S. Sexual health and gynecological cancer: conceptualizing patient needs and overcoming barriers to seeking and accessing services. Journal of Psychosomatic Obstetrics and Gynecology. 2012;33:135–142. doi: 10.3109/0167482x.2012.709291. [DOI] [PubMed] [Google Scholar]
- 41.Hordern A, Grainger M, Hegarty S, Jefford M, White V, Sutherland G. Discussing sexuality in the clinical setting: The impact of a brief training program for oncology health professionals to enhance communication about sexuality. Asia-Pacific Journal of Clinical Oncology. 2009;5:270–277. doi: 10.1111/j.1743-7563.2009.01238.x. [DOI] [Google Scholar]
- 42.Vadaparampil ST, Gwede CK, Meade C, Kelvin J, Reich RR, Reinecke J, Bowman M, Sehovic I, Quinn GP, Quinn GP. ENRICH: A promising oncology nurse training program to implement ASCO clinical practice guidelines on fertility for AYA cancer patients. Patient Educ Couns. 2016 doi: 10.1016/j.pec.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berry DL, Blumenstein BA, Halpenny B, Wolpin S, Fann JR, Austin-Seymour M, Bush N, Karras BT, Lober WB, McCorkle R. Enhancing Patient-Provider Communication With the Electronic Self-Report Assessment for Cancer: A Randomized Trial. J Clin Oncol. 2011;29:1029–1035. doi: 10.1200/jco.2010.30.3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hilarius DL, Kloeg PH, Gundy CM, Aaronson NK. Use of health-related quality-of-life assessments in daily clinical oncology nursing practice: a community hospital-based intervention study. Cancer. 2008;113:628–637. doi: 10.1002/cncr.23623. [DOI] [PubMed] [Google Scholar]
- 45.Ligibel JA, Denlinger CS. New NCCN Guidelines® for Survivorship Care. J Natl Compr Canc Netw. 2013;11:640–644. doi: 10.6004/jnccn.2013.0191. [DOI] [PubMed] [Google Scholar]
- 46.Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, Cannady RS, Pratt-Chapman ML, Edge SB, Jacobs LA, Hurria A, Marks LB, LaMonte SJ, Warner E, Lyman GH, Ganz PA. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA Cancer J Clin. 2016;66:43–73. doi: 10.3322/caac.21319. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.