Abstract
Background
We examined the relationship between two forms of ethnic discrimination – interpersonal and institutional – and smoking outcomes among Arab men in Israel, and whether social support buffered these associations.
Methods
We used cross-sectional data of adult Arab men, current or former smokers (n=954). Mixed-effects regression models estimated the association between discrimination and smoking status, and nicotine dependence among current smokers.
Results
Interpersonal discrimination was associated with higher likelihood of being a current smoker compared to a former smoker, whereas institutional group discrimination was not. Social support moderated the ethnic discrimination-nicotine dependence link. Among men with low social support, greater interpersonal discrimination was associated with greater nicotine dependence. Similarly, among smokers with high institutional group discrimination, those with high social support reported lower nicotine dependence compared to those with low social support.
Conclusion
Ethnic discrimination should be considered in efforts to improve smoking outcomes among Arab male smokers in Israel.
Keywords: Ethnic discrimination, interpersonal, institutional, smoking, Israel
Background
Social stratification, such as being a member of an ethnic minority, is central to stress processes that confer higher risk for negative health outcomes [1]. Among Arab Israeli citizens, who comprise 20.7% of the Israeli population, their status as an indigenous, non-Jewish ethnic minority plays a pivotal role in their exposure to social stressors. Despite improvements in their economic and health status since becoming Israeli citizens, Arabs in Israel remain significantly more economically disadvantaged [2] and exhibit poorer health than their Jewish counterparts [3].
Israeli Arab men are twice as likely to smoke as Jewish men (46.6% vs. 23.1%) [4], a disparity that has been increasing since the 1980s [5]. Arab men also smoke at higher intensity than Jewish men and exhibit higher morbidity and mortality rates from tobacco-related diseases [3, 6]. Though social stressors, such as ethnic discrimination, may contribute to the staggering high smoking rates among Arab men, no Israeli study has empirically examined the link between ethnic discrimination and smoking behavior in this population.
Israeli Arabs are exposed to both interpersonal and institutional forms of ethnic discrimination [7–10]. About 40% of Arabs report experiencing interpersonal ethnic discrimination [11] – prejudice and discriminatory actions perpetrated by individuals towards others [12] – especially in employment, education [13]. At the institutional level, discriminatory policies [12] restrict Arabs’ citizenship rights, employment opportunities, and political representation while simultaneously promoting the channeling of economic resources to Jewish citizens [7, 8, 10].
The association between discrimination and smoking behavior has long been established in studies conducted mostly in North America and the UK [14–17]. These studies generally focus on interpersonal discrimination and show that those who experience discrimination are more likely to smoke than those who do not. Two U.S studies also show everyday interpersonal discrimination is associated with lower likelihood of successful cessation and higher nicotine dependence among smokers [18, 19]. In comparison, institutional group discrimination has rarely been examined in relation to smoking. By limiting Arab’s opportunities for equal employment, education, and wealth acquisition [8–10, 20], institutional ethnic discrimination may lead to greater exposure to social stress with implications for smoking and addiction in this population.
As applied to discrimination studies [21, 22], the stress process model posits that personal and social resources, such as social support, can serve to safeguard against the damaging health effects of discrimination (i.e., a buffering effect). In that sense, social support provides individuals with a sense of security and belonging, which aids them in understanding that discrimination is a shared experience with other group members [23]. It can also guide individuals in using effective coping strategies to respond to discrimination [23]. Though the stress process model is widely used in health research, specific concepts, such as the buffering effects of social support, have received less empirical examination [21, 24–26]. In this study, we investigate the effect of two forms of ethnic discrimination against Arabs, interpersonal and perceived institutional group discrimination, on smoking outcomes and whether social support buffers those effects.
Methods
Participants and data collection
Data came from a cross-sectional study aimed at identifying the factors associated with smoking cessation among adult Arab male smokers and former smokers in Israel [27]. Eligible participants were (1) Arab male citizens of Israel, (2) aged 18–64 years, and (3) current or former cigarette smokers. The study utilized a stratified sampling design in which 20 towns were randomly selected from a list of 64 Arab towns in Israel. Sampling of Arab towns was proportionate to the distribution of Arab towns in each of three regions of Israel (south, center, north), their population size, and the socio-economic status of the locality. A list of men residing in these 20 towns was obtained from the Israeli population registry, and a simple random sample of men was drawn. Data were collected between September 2012 and September 2013. Participants (n=964) were interviewed face-to-face in their home (Participation rate=83%). The study was approved by the Ethics Review Board of the Academic institution in which the study was conducted [details omitted for blind review].
For the current analyses, we employed two analytic samples. The first sample included all participants (n=954; n=789 current smokers, n=165 former smokers) and was used to estimate the relationship between ethnic discrimination and smoking status. The second was a sub-sample of current smokers (n=721) and was used to estimate the relationship between ethnic discrimination and nicotine dependence. The discrepancy in the sample size of current smokers in the full sample and the subsample is due to item non-response on the outcome variable – nicotine dependence – used in the subsample analysis (n=68 with missing data).
Measures
Dependent variables
Smoking status
Men were asked whether they currently smoked and were classified as 1= current smokers or 0= former smokers if they reported quitting within the past six months or prior to that.
Nicotine dependence
The Fagerstrom Test for Nicotine Dependence (FTND) measure [28] was used to assess nicotine dependence among current smokers. Participants were asked: (1) how soon after you wake up do you smoke your first cigarette? (0=after 60 minutes, 1=31 to 60 minutes, 2=6 to 30 minutes and 3=within 5 minutes), (2) do you find it difficult to refrain from smoking in places where it is forbidden? (1=yes, 0=no), (3) which cigarette would you hate most to give up? (1=first one in the morning, 0=all others), (4) how many cigarettes per day do you smoke? (0=10 or less, 1=11 to 20, 2=21 to 30, and 3=31 cigarettes or more), (5) do you smoke more frequently during the first hours of waking than during the rest of the day? (1=yes, 0=no), and (6) do you smoke if you are ill that you are in bed most of the day? (1=yes, 0=no). Per convention, values were summed across items (minimum=0, maximum=10).
Independent variables
Interpersonal ethnic discrimination (EOD-A)
We assessed self-reported experiences of interpersonal discrimination using an adapted Arabic version of the “Experiences of Discrimination” (EOD-A) scale [29]. Original items were tailored to reflect settings outside of the segregated Arab towns where Arabs are likely to interact with the Jewish majority and hence where interpersonal ethnic discrimination may occur. Participants were asked to indicate how often, in their lifetime, they had been discriminated against or treated unfairly because they were Arab: “while getting health care services”, “in the street or in public places”, “while searching for a job”, “at their workplace”, “while getting services from public institutions”, “while interacting with the police”, “while searching for housing in mixed Arab-Jewish or Jewish cities”, “while applying for or studying in college or university”, and “while in the airport”. Response options were 0=never, 1=once, 2=2–3 times, and 3=4 times or more (Cronbach’s alpha .80). Scores were summed across all items with higher numbers indicating greater interpersonal ethnic discrimination (minimum=0, maximum=27). This measure exhibited good variability (Mean = 1.75, SD = 3.2, Coefficient of variation, calculated as the ratio of the standard deviation to the mean, > 1) and was modeled as a continuous variable. Results from psychometric examination supports the validity and reliability of this adapted measure [30].
Perceptions of Institutional Group Discrimination (IGD)
Perceptions of ethnic discrimination against Arabs as an ethnic group were assessed using the “Institutional Group Discrimination” (IGD) scale. The measure was developed specifically for this study and demonstrates good psychometric properties in this population [30]. The measure included 12 items that asked respondents for their level of agreement with statements that describe social inequalities between Arabs and Jews across various domains (e.g., education, employment, infrastructure, resource allocation, and others). For example, “Arabs are generally portrayed in a negative way in the Israeli media”, “Arabs in Israel have less employment opportunities compared to Jews”, and “Arab towns are underdeveloped compared to Jewish towns” (See full measure in Appendix A). Response options were measured on a 4-point likert scale, ranging from strongly disagree to strongly agree. Scores were summed across all items with higher numbers indicating greater perceived institutional group discrimination (Cronbach’s alpha .91). Because of low variability in participant responses and skewed distribution (Mean=27.5, SD=8.5, Coefficient of Variation <1), we dichotomized this variable into low vs. high IGD using the 50th percentile as the cutoff point.
Social support
Social support was measured using six items that asked how frequently participants received the following types of support: (1) someone gave them information, guidance, or advice during crisis, (2) someone gave them practical help when they needed it, (3) someone they could trust and talk to about themselves and their problems, (4) someone that shows affection and closeness toward them, (5) someone who supports them emotionally in times of crisis, and (6) someone who can provide them with material help. Response options ranged from 0=never to 4=all the time. Responses were summed across items (Minimum = 0, Maximum = 24). Because of low variability in participant responses and skewed distribution (Mean=16.0, SD=5.8, Coefficient of Variation <1), we categorized social support as low, moderate, and high using tertiles as the cutoff points.
Control variables
We included a set of variables that may be related to discrimination and smoking behavior: age, marital status, education, subjective economic position (assessed as the participant’s ranking of his family’s income relative to other families in Israeli society and categorized as worse or much worse, similar, and better or much better), employment status (unemployed vs. employed), and participant’s self-reported national identity (Palestinian/Arab vs. Israeli/Arab Israeli).
Statistical analysis
Mixed effect logistic (smoking status) and linear (nicotine dependence) regression models were used to account for clustering of observations at the town level. We first examined an unconditional model (i.e., a baseline model without any predictors) to calculate the interclass correlation coefficient (ICC). Then, we estimated the association between both forms of ethnic discrimination and smoking status or nicotine dependence, adjusting confounders (Model 1). Next, we included social support to estimate its main effect (Model 2). Lastly, we included an interaction term between interpersonal ethnic discrimination and social support (Model 3) and institutional group discrimination and social support (Model 4), respectively, to test the buffering effects of social support.
Approximately 37% of participants (n=357) were missing data on one or more study variable. Most item non-response occurred on the individual items comprising the institutional group discrimination measure (3%–17%). Assessment of item non-response patterns suggests data were missing at random (MAR). We imputed data on all covariates and all primary predictor variables at the item-level using the mi impute command with chained equations specification in Stata 13.0. This produced 50 data sets. Analyses were replicated across the 50 datasets and combined using mi estimate that uses Rubin’s combination rules to consolidate the obtained individual estimates into a single set of estimates. We use a one-tailed test to assess statistical significance at p<0.025. Lastly, to assess model fit we calculated the difference in the Bayesian Information Criterion (Δ BIC) [31] between each of the interaction models (Models 3–4) in relation to the main effect model (Model 2).
Results
Sample characteristics
The full sample (n=954) included both current (83%) and former (17%) smokers from 20 Arab towns (density = 8 to 164 men) (Table 1). Participants’ ages ranged from 18 to 64 (Mean = 37.3, SD = 13.1). Most men were married (66%) and employed (81%). Over 80% had a high school education or less. Forty-percent reported their income as worse or much worse relative to families in Israeli society. The subsample of current smokers (n=721) had a mean level of nicotine dependence (FTND) of 4.2 (minimum=0, maximum =10, SD=2.6).
Table 1.
Sample characteristics of Arab male current and former smokers, Israel
| Full sample (n=954) |
Subsample (n=721) |
|
|---|---|---|
|
| ||
| Variables | % or mean (SD) |
% or mean (SD) |
| Smoking status | ||
| Current smoker | 82.7 | 100.0 |
| Former smoker | 17.3 | |
| Fagerstrom Test for Nicotine Dependence (FTND) (range 0–10) | 4.2 (2.6) | |
| Interpersonal ethnic discrimination (EOD) (range 0–27) | 1.75 (3.2) | 1.97 (3.4) |
| Institutional group discrimination (IGD) | ||
| Low | 50.0 | 50.0 |
| High | 50.0 | 50.0 |
| Age (range 18–64) | 37.3 (13.1) | 36.8 (13.2) |
| Marital status | ||
| Unmarried | 33.9 | 36.3 |
| Married | 66.1 | 63.7 |
| Education | ||
| Primary-middle school | 21.6 | 23.3 |
| Vocational\regular high school | 61.0 | 60.7 |
| Above high school education | 17.4 | 16.0 |
| Subjective economic position (SEP) | ||
| Worse\much worse | 41.0 | 40.2 |
| Similar | 51.4 | 52.0 |
| Better\much better | 7.6 | 7.8 |
| Employment status | ||
| Unemployed | 19.3 | 18.9 |
| Employed | 80.7 | 81.1 |
| National identity | ||
| Arab\Palestinian | 40.1 | 40.0 |
| Israeli | 59.9 | 60.0 |
Smoking status
Adjusting for socio-demographics (Model 1, Table 2), greater interpersonal discrimination was associated with higher odds of being a current smoker compared to a former smoker [OR = 1.16, 95% CI 1.06, 1.27], whereas perceived institutional group discrimination was unrelated to smoking status [OR = 0.88, 95% CI 0.57, 1.36]. These associations remained the same after adjustment for social support (Model 2). We found no statistically significant interaction between either form of ethnic discrimination and social support (Models 3, 4) when predicting smoking status. As a result, the main effect model (Model 2) fit the data better than either interaction models (Δ BIC 13.3 and 9.6 for Model 3 and 4 respectively).
Table 2.
Mixed effects logistic regression models predicting current versus former smoking status among Arab male current and former smokers, Israel, n=954
| Variables | Model 1 OR [95% CI] |
Model 2 OR [95% CI] |
Model 3 OR [95% CI] |
Model 4 OR [95% CI] |
|---|---|---|---|---|
| Fixed Effects | ||||
| Interpersonal ethnic discrimination | 1.16* | 1.16* | 1.13 | 1.16* |
| [1.06, 1.27] | [1.06, 1.27] | [0.98, 1.30] | [1.06, 1.27] | |
| Institutional group discrimination (IGD) | ||||
| Low (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| High | 0.88 | 0.89 | 0.89 | 1.52 |
| [0.57, 1.36] | [0.57, 1.38] | [0.57, 1.38] | [0.71, 3.26] | |
| Social support | ||||
| Low (ref) | 1.00 | 1.00 | 1.00 | |
| Moderate | 0.81 | 0.75 | 1.27 | |
| [0.50, 1.30] | [0.44, 1.28] | [0.64, 2.53] | ||
| High | 0.75 | 0.73 | 1.00 | |
| [0.46, 1.22] | [0.43, 1.25] | [0.52, 1.92] | ||
| Interpersonal discrimination X moderate social support | 1.07 | |||
| [0.85, 1.35] | ||||
| Interpersonal discrimination X high social support | 1.02 | |||
| [0.83, 1.24] | ||||
| High institutional discrimination X moderate social support | 0.38 | |||
| [0.14, 1.05] | ||||
| High institutional discrimination X high social support | 0.52 | |||
| [0.20, 1.37] | ||||
|
| ||||
| Random Effects | ||||
| Intercept | 0.81 | 0.80 | 0.80 | 0.82 |
| 95% CI | [0.49, 1.34] | [0.48, 1.34] | [0.48, 1.32] | [0.50, 1.36] |
| Model fit | ||||
| BIC | 873.94 | 886.18 | 899.50 | 895.76 |
Notes. Outcome variable=smoking status (0=former smoker, 1= current smoker); Intraclass correlation from unconditional model = 0.180; Model 1 adjusts for age, marital status, education, subjective economic position, employment status and national identity; Model 2: main effect model with discrimination, and social support; Model 3: interaction model between interpersonal discrimination and social support; Model 4: interaction model between institutional discrimination and social support;
p<.025, one tailed test
Nicotine dependence
Neither form of ethnic discrimination was associated with nicotine dependence in Model 1 or Model 2 (Table 3). Social support, however, was a significant moderator of the discrimination-nicotine dependence relationship. Specifically, as interpersonal discrimination increased, men with low social support reported higher levels of nicotine dependence than men with high social support (Figure 1a). Indeed, the disparity in nicotine dependence when men reported no interpersonal discrimination was zero, but was almost 4 when interpersonal discrimination was greatest. Similarly, among men reporting high perceived institutional group discrimination, high social support was associated with lower nicotine dependence compared to men with low social support (Model 4) (Figure 1b). Model fit improved with the inclusion of the interactions (Model 3 (Δ BIC = −0.4) and Model 4 (Δ BIC = −2.3)).
Table 3.
Mixed effects linear regression models predicting nicotine dependence among Arab male current smokers, Israel, n=721
| Variables | Model 1 b [SE] |
Model 2 b [SE] |
Model 3 b [SE] |
Model 4 b [SE] |
|---|---|---|---|---|
| Intercept | 3.92 [0.52]* | 3.93 [0.53]* | 3.79 [0.53]* | 3.78 [0.53]* |
| Fixed Effects | ||||
| Interpersonal ethnic discrimination | 0.04 [0.03] | 0.04 [0.03] | 0.10 [0.04]* | 0.04 [0.03] |
| Institutional group discrimination (IGD) | ||||
| Low (ref) | ||||
| High | 0.07 [0.21] | 0.07 [0.21] | 0.10 [0.21] | 0.60 [0.34] |
| Social support | ||||
| Low (ref) | ||||
| Moderate | −0.03 [0.22] | 0.14 [0.26] | 0.12 [0.32] | |
| High | −0.04 [0.24] | 0.24 [0.27] | 0.57 [0.33] | |
| Interpersonal discrimination X moderate social support | −0.09 [0.06] | |||
| Interpersonal discrimination X high social support | −0.15 [0.06]* | |||
| High institutional discrimination X moderate social support | −0.40 [0.46] | |||
| High institutional discrimination X high social support | −1.23 [0.46]* | |||
|
| ||||
| Random Effects | ||||
| Intercept [SE] | 0.74 [0.16] | 0.74 [0.16] | 0.73 [0.16] | 0.72 [0.16] |
| Level 1 Error [SE] | 2.36 [0.06] | 2.36 [0.06] | 2.35 [0.06] | 2.35 [0.06] |
| Model fit | ||||
| BIC | 3372.71 | 3378.77 | 3378.37 | 3376.39 |
Notes. Intraclass correlation from Unconditional model =0.099; Model 1 adjusts for age, marital status, education, subjective economic position, employment status and national identity; Model 2: main effect model with discrimination and social support; Model 3: interaction model between interpersonal discrimination and social support; Model 4: interaction model between institutional discrimination and social support;
p<.025, one tailed test
Figure 1.
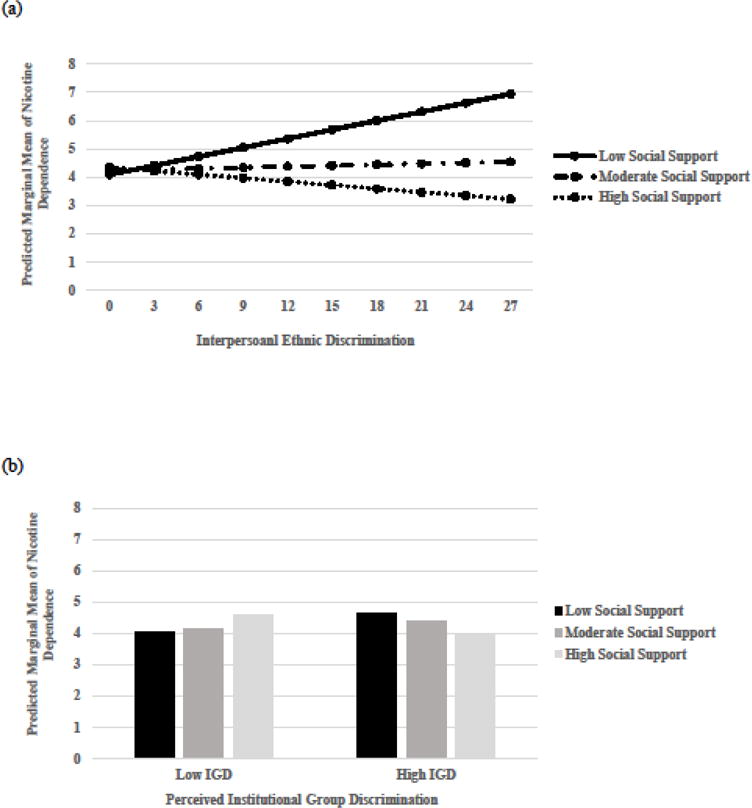
Predicted marginal means of nicotine dependence for low vs. high social support by a) interpersonal ethnic discrimination (Model 3, Table 3), and b) low vs. high perceived institutional group discrimination (Model 4, Table 3) among Arab male current smokers in Israel.
Discussion
We examined the link between ethnic discrimination and smoking-related outcomes among Israeli Arab men, a population that exhibits persistently high rates of tobacco use [4]. Greater interpersonal ethnic discrimination was associated with higher odds of being a current smoker compared to a former smoker. These results are consistent with U.S. research that finds interpersonal discrimination is associated with increased odds of smoking [32–35] and reduced odds of successful smoking cessation [18].
In main effect models, neither interpersonal discrimination nor perceived institutional discrimination was associated with nicotine dependence. Consistent with the stress process model, however, social support buffered the relationship between both forms of ethnic discrimination and nicotine dependence. Increasing interpersonal discrimination was associated with greater nicotine dependence among smokers with low social support but was unrelated to nicotine dependence among smokers with high social support. Similarly, among smokers who reported high levels of perceived institutional group discrimination, men with high social support reported lower nicotine dependence compared to men with low social support.
Findings from U.S. studies are inconsistent on whether social support buffers the effects of ethnic discrimination on health [21, 25, 36, 37]. Further, only one of these studies examined smoking-related outcomes and found that at low levels of social support, youth who experienced greater educational discrimination had higher levels of nicotine addiction severity than youth with high levels of social support [26]. Indeed, research on discrimination suggests that seeking social support is a commonly used coping strategy following interpersonal discriminatory events [38–40]. Social support may benefit Arab male smokers who face discrimination in many ways including providing a sense of security and connectedness, as well as access to information, advice, guidance and other social and economic resources, all of which may influence whether a smoker resorts to tobacco use or intensifies their tobacco consumption to mitigate discrimination stress.
About 40% of Arab men in our sample experienced interpersonal discrimination. This estimate is similar to those reported elsewhere [11, 13]. Over 80% of men, however, endorsed strong perceptions of institutional group discrimination against Arabs. These findings are in accord with the personal/group discrimination discrepancy (PGDD) phenomenon that has been discussed in studies outside of the health literature and which stipulates that people perceive higher levels of discrimination directed at their ethnic group than discrimination directed at themselves as individual members [41]. Explanations for this discrepancy include denial or minimization of personal discrimination, and cognitive and emotional biases related to information processing (e.g., recall biases and discomfort in confronting one’s own victimization) [42].
In Israel, extreme residential segregation between Arabs and Jews [2] may lead to personal/ group discrimination discrepancy. Residential segregation reduces opportunities for interethnic interactions, hence reduces the likelihood that interpersonal discrimination will occur. Residential segregation, however, can exacerbate Arabs’ sense of exclusion from Israeli society and their sense of economic deprivation compared to Jews. Nevertheless, discrimination at the interpersonal level as well as perceptions of group discrimination, both reflect the extent to which Arabs feel integrated into the fabric of Israeli society and may have unique influences on Arab men’s smoking behavior.
Limitations
Several limitations warrant consideration. According to the CDC (2009) [43], a current smoker is defined as someone who smoked at least 100 cigarettes in their lifetime and who smoked during the past 30 days. In this study, smoking status was established using one question about current smoking (i.e., do you smoke?) as more detailed questions about lifetime cigarette consumption and past 30-day behavior were unavailable. Other indicators of smoking behavior, however, (e.g., number of years smoking (Mean=16 years) and cigarettes smoked per day (80% smoked more than half a pack/day) show that most smokers in our sample were moderate to heavy smokers.
Perceptions and experiences of discrimination were self-reported, and may have been affected by recall bias and social desirability. The use of Arab interviewers likely minimized social desirability bias and reduced participants’ fear to report discriminatory experiences [44], but may not have eliminated those biases entirely. Social desirability in responses to the IGD measure may have resulted in participants strongly agreeing with most items, leading to low variation in this measure. Alternatively, the low variability in responses to the IGD items could be a function of who was included in the study (e.g., men, current and former smokers) or reflect the extent to which institutional ethnic discrimination against Israeli Arabs is systematic and pervasive. It is also possible that investigating perceptions of institutional group discrimination as it relates to health behavior is more informative when the sample includes multiple ethnic groups who are subjected to varying levels of institutional discrimination than only one ethnic group.
Finally, the exclusion of nonsmokers and women from our sample limits the generalizability of the findings to the larger Arab Israeli population. Whether Arabs exposed to discrimination are more likely to initiate smoking as compared to not smoking and whether the associations observed in this paper between discrimination, former smoking, and nicotine dependence hold among Arab female smokers remains unknown.
Conclusions
In light of the high rates of smoking among Arab men in Israel, it is important to understand the factors that promote smoking or intensify nicotine dependence in this population. This study’s results suggest that ethnic discrimination plays a role in shaping smoking outcomes among Arab men and that interpersonal ethnic discrimination appears to have a stronger association with smoking outcomes than perceptions of institutional group discrimination in this population. Consistent with the stress process model, social support buffers the effects of discrimination on nicotine dependence among Arab male smokers. Interventions to reduce smoking among Arab men should consider discrimination stress as a contributing factor to addiction in this population and accentuate seeking social support to help buffer the effects of discrimination stress on smoking outcomes.
Acknowledgments
Funding: Grant number P50 CA180907 from the National Cancer Institute and the FDA Center for Tobacco Products (CTP) supported the first author’s time spent writing the paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Appendix A – Ethnic Institutional Group Discrimination (IGD) Measure
Please indicate your level of agreement with the following statements:
Items
Arab towns and villages lack adequate health care services compared to Jewish towns
Arabs are generally portrayed in a negative way in the Israeli media
There are laws in Israel that discriminate against Arabs
Arabs in Israel have less employment opportunities compared to Jews
Arabs in Israel do not have enough influence in the political system
The use of military–service criterion as a condition for employment discriminates against Arabs
Arab towns are underdeveloped compared to Jewish towns
The Palestinian history is underrepresented in the educational curriculum taught in Arab schools
Arab schools enjoy less far funding and resources compared to Jewish schools
Arab students are greatly underrepresented colleges and universities in Israel compared to Jewish students
In Israel, the Arabic language is perceived as inferior to the Hebrew language
Arabs are treated in a discriminatory way by the security personnel in the airport
Note. Response options: 1. strongly disagree to 5. strongly agree
Footnotes
Data availability statement
The data analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Standard
The study was approved by the Ethics Review Board of the Academic institution in which the study was conducted [details omitted for blind review]. All participants gave written informed consent to participate in the study.
References
- 1.Pearlin LI. The sociological study of stress. Journal of Health and Social Behavior. 1989;30:241–56. [PubMed] [Google Scholar]
- 2.Lewin AC, Stier H, Caspi-Dror D. The place of opportunity: community and individual determinants of poverty among Jews and Arabs in Israel. Research in Social Stratification and Mobility. 2006;24:177–91. [Google Scholar]
- 3.Ministry of Health. Health status in Israel. Jerusalem, Israel: 2010. Retrieved from http://www.health.gov.il/PublicationsFiles/Health_Status_in_Israel2010.pdf. [Google Scholar]
- 4.Ministry of Health. The Minister’s Report on Smoking in Israel. Jerusalem, Israel: 2015. Retrieved from http://www.health.gov.il/PublicationsFiles/smoking_2015.pdf. [Google Scholar]
- 5.Baron-Epel O, Keinan-boker L, Weinstein R, Shohat T. Persistent High Rates of Smoking among Israeli Arab Males with Concomitant Decrease among Jews. Israel Medical Assocaition Journal. 2010;12:732–7. [PubMed] [Google Scholar]
- 6.Tarabeia J, Green MS, Barchana M, Baron-Epel O, Ifrah A, Fishler Y, Nitzan-kaluski D. Increasing lung cancer incidence among Israeli Arab men reflects a change in the earlier paradox of low incidence and high smoking prevalence. European Journal of Cancer Prevention. 2008;17(4):291–296. doi: 10.1097/CEJ.0b013e3282f0c0b7. [DOI] [PubMed] [Google Scholar]
- 7.Abu-saad I. Separate and unequal: the role of the state educational system in maintaining the subordination of Israel’s Palestinian arab citizens. Social Identities. 2004;10(1):101–127. [Google Scholar]
- 8.Adalah. Inequality Report: The Palestinian Arab Minority in Israel Israel. Haifa, Israel: 2011. Retrieved from http://adalah.org/upfiles/2011/Adalah_The_Inequality_Report_March_2011.pdf. [Google Scholar]
- 9.Adalah. New Discriminatory Laws and Bills in Israel. Haifa, Israel. Haifa, Israel: 2012. Retrieved from http://adalah.org/Public/files/English/Legal_Advocacy/Discriminatory_Laws/Discriminatory-Laws-in-Israel-October-2012-Update.pdf. [Google Scholar]
- 10.Golan-Agnon D. Separate but Not Equal: Discrimination Against Palestinian Arab Students in Israel. American Behavioral Scientist. 2006;49(8):1075–1084. [Google Scholar]
- 11.Daoud N, Shankardass K, O’Campo P, Anderson K, Agbaria AK. Internal displacement and health among the Palestinian minority in Israel. Social Science & Medicine. 2012;74(8):1163–71. doi: 10.1016/j.socscimed.2011.12.041. [DOI] [PubMed] [Google Scholar]
- 12.Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- 13.Baron-Epel O, Kaplan G, Moran M. Perceived discrimination and health-related quality of life among Arabs and Jews in Israel: A population-based survey. BMC Public Health. 2010;10:282. doi: 10.1186/1471-2458-10-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennett GG, Wolin KY, Robinson EL, Fowler S, Edwards CL. Perceived racial/ethnic harassment and tobacco use among African American young adults. American Journal of Public Health. 2005;95:238–40. doi: 10.2105/AJPH.2004.037812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey J, Krieger N. Unfair treatment, racial/ethnic discrimination, ethnic identification, and smoking among Asian Americans in the National Latino and Asian American Study. American Journal of Public Health. 2008;98(3):485–92. doi: 10.2105/AJPH.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graham H, Inskip HM, Francis B, Harman J. Pathways of disadvantage and smoking careers: evidence and policy implications. Journal of Epidemiology & Community Health. 2006;60(Supplement 2):ii7–ii12. doi: 10.1136/jech.2005.045583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 18.Kendzor DE, Businelle MS, Reitzel LR, Castro Y, Vidrine JI, Mazas CA, … Wetter DW. The influence of discrimination on smoking cessation among Latinos. Drug and Alcohol Dependence. 2014a;136:143–8. doi: 10.1016/j.drugalcdep.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kendzor DE, Businelle MS, Reitzel LR, Rios DM, Scheuermann TS, Pulvers K, Ahluwalia JS. Everyday discrimination is associated with nicotine dependence among African American, Latino, and White smokers. Nicotine & Tobacco Research. 2014b;16(6):633–40. doi: 10.1093/ntr/ntt198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okun BS, Friedlander D. Educational stratification among Arabs and Jews in Israel: historical disadvantage, discrimination, and opportunity. Population Studies. 2005;59(2):163–80. doi: 10.1080/00324720500099405. [DOI] [PubMed] [Google Scholar]
- 21.Mossakowski KN, Zhang W. Does Social Support Buffer the Stress of Discrimination and Reduce Psychological Distress Among Asian Americans? Social Psychology Quarterly. 2014;77(3):273–295. [Google Scholar]
- 22.Ong AD, Fuller-Rowell T, Burrow AL. Racial Discrimination and the Stress Process. Journal of Personality and Social Psychology. 2009;96(6):1259–1271. doi: 10.1037/a0015335. [DOI] [PubMed] [Google Scholar]
- 23.Brondolo E, ver Halen N, Pencille M. Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal of Behavioral Medicine. 2009;32(1):64–88. doi: 10.1007/s10865-008-9193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chao RCL. Managing Stress and Maintaining Well‐Being: Social Support, Problem‐Focused Coping, and Avoidant Coping. Journal of Counseling & Development. 2011;89(3):338–348. [Google Scholar]
- 25.Gee GC, Chen J, Spencer MS, See S, Kuester OA, Tran D, Takeuchi D. Social support as a buffer for perceived unfair treatment among Filipino Americans: Differences between San Francisco and Honolulu. American Journal of Public Health. 2006;96:677–684. doi: 10.2105/AJPH.2004.060442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hershberger A, Zapolski T, Aalsma MC. Social support as a buffer between discrimination and cigarette use in juvenile offenders. Addictive Behaviors. 2016;59:7–11. doi: 10.1016/j.addbeh.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anonymous et al. Details omitted for double-blind reviewing. 2015a [Google Scholar]
- 28.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerström test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 29.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Social Science & Medicine. 2005;61(7):1576–96. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 30.Anonymous et al. Details omitted for double-blind reviewing. 2015b [Google Scholar]
- 31.Kass RE, Raftery AE. Bayes factors. Journal of the American Statistical Association. 1995;90(430):773–795. [Google Scholar]
- 32.Borrell LN, Jacobs DR, Williams DR, Pletcher MJ, Houston TK, Kiefe CI. Self-reported racial discrimination and substance use in the Coronary Artery Risk Development in Adults Study. American Journal of Epidemiology. 2007;166(9):1068–79. doi: 10.1093/aje/kwm180. [DOI] [PubMed] [Google Scholar]
- 33.Corral I, Landrine H. Racial discrimination and health-promoting vs damaging behaviors among African-American adults. Journal of Health Psychology. 2012;17(8):1176–1182. doi: 10.1177/1359105311435429. [DOI] [PubMed] [Google Scholar]
- 34.Horton KD, Loukas A. Discrimination, religious coping, and tobacco use among White, African American, and Mexican American vocational school students. Journal of Religion and Health. 2013;52(1):169–183. doi: 10.1007/s10943-011-9462-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Purnell JQ, Peppone LJ, Alcaraz K, McQueen A, Guido JJ, Carroll JK, … Morrow GR. Perceived discrimination, psychological distress, and current smoking status: results from the Behavioral Risk Factor Surveillance System Reactions to Race module, 2004–2008. American Journal of Public Health. 2012;102(5):844–51. doi: 10.2105/AJPH.2012.300694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim I. The role of critical ethnic awareness and social support in the discrimination-depression relationship among Asian Americans: path analysis. Cultural Diversity & Ethnic Minority Psychology. 2014;20(1):52–60. doi: 10.1037/a0034529. [DOI] [PubMed] [Google Scholar]
- 37.Noh S, Kaspar V. Perceived discrimination and depression: Moderating effects of coping, acculturation, and ethnic support. American Journal of Public Health. 2003;93:232–238. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mellor D. Responses to racism: A taxonomy of coping styles used by aboriginal Australians. American Journal of Orthopsychiatry. 2004;74:56–71. doi: 10.1037/0002-9432.74.1.56. [DOI] [PubMed] [Google Scholar]
- 39.Shorter-Gooden K. Multiple resistance strategies: How African American women cope with racism and sexism. Journal of Black Psychology. 2004;30:406–425. [Google Scholar]
- 40.Thompson Sanders VL. Coping responses and the experience of discrimination. Journal of Applied Social Psychology. 2006;36:1198–1214. [Google Scholar]
- 41.Taylor DM, Wright SC, Moghaddam FM, Lalonde RN. The personal/group discrimination discrepancy perceiving my group, but not myself, to be a target for discrimination. Personality and Social Psychology Bulletin. 1990;16(2):254–262. [Google Scholar]
- 42.Crosby F. The denial of personal discrimination. American Behavioral Scientist. 1984;27(3):371–386. [Google Scholar]
- 43.Centers for Disease Control and Prevention (CDC) State-specific secondhand smoke exposure and current cigarette smoking among adults―United States, 2008. MMWR. 2009;58:1232–5. [PubMed] [Google Scholar]
- 44.Davis DW, Silver BD. Stereotype threat and race of interviewer effects in a survey on political knowledge. American Journal of Political Science. 2003;47(1):33–45. [Google Scholar]


