Abstract
Background: In 2002 the American Thoracic Society/European Respiratory Society (ATS/ERS) classification of idiopathic interstitial pneumonias (IIPs) defined seven specific entities, and provided standardized terminology and diagnostic criteria. In addition, the historical “gold standard” of histologic diagnosis was replaced by a multidisciplinary approach. Since 2002 many publications have provided new information about IIPs.
Purpose: The objective of this statement is to update the 2002 ATS/ERS classification of IIPs.
Methods: An international multidisciplinary panel was formed and developed key questions that were addressed through a review of the literature published between 2000 and 2011.
Results: Substantial progress has been made in IIPs since the previous classification. Nonspecific interstitial pneumonia is now better defined. Respiratory bronchiolitis–interstitial lung disease is now commonly diagnosed without surgical biopsy. The clinical course of idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia is recognized to be heterogeneous. Acute exacerbation of IIPs is now well defined. A substantial percentage of patients with IIP are difficult to classify, often due to mixed patterns of lung injury. A classification based on observed disease behavior is proposed for patients who are difficult to classify or for entities with heterogeneity in clinical course. A group of rare entities, including pleuroparenchymal fibroelastosis and rare histologic patterns, is introduced. The rapidly evolving field of molecular markers is reviewed with the intent of promoting additional investigations that may help in determining diagnosis, and potentially prognosis and treatment.
Conclusions: This update is a supplement to the previous 2002 IIP classification document. It outlines advances in the past decade and potential areas for future investigation.
Keywords: idiopathic interstitial pneumonia, usual interstitial pneumonia, nonspecific interstitial pneumonia, respiratory bronchiolitis, desquamative interstitial pneumonia, cryptogenic organizing pneumonia, acute interstitial pneumonia, lymphoid interstitial pneumonia, pleuroparenchymal fibroelastosis, acute fibrinous and organizing pneumonia
Contents
Executive Summary
Introduction
Methods
Summary of Major Revisions of the IIP Classification
General Progress in IIPs since 2002
Multidisciplinary Approach
Observer Agreement in Diagnosis of IIP
Important Differential Diagnostic Considerations
Hypersensitivity Pneumonitis
Collagen Vascular Disease
Familial Interstitial Pneumonia
Coexisting Patterns
Progress in Specific IIPs since 2002
Chronic Fibrosing IIPs
Smoking-related IIPs
Acute or Subacute IIPs
Rare IIPs
Idiopathic Lymphocytic Interstitial Pneumonia
Idiopathic Pleuroparenchymal Fibroelastosis
Rare Histologic Patterns
Acute Fibrinous and Organizing Pneumonia
Bronchiolocentric patterns of interstitial pneumonia
Unclassifiable IIP
Clinical Classification of Disease Behavior
Biomarkers
Executive Summary
There are several specific areas that are given special attention in this revision of the 2002 American Thoracic Society/European Respiratory Society idiopathic interstitial pneumonia (IIP) statement.
-
1.
Idiopathic nonspecific interstitial pneumonia (NSIP) is now accepted as a specific clinicopathologic entity. It has become evident that clinical progression is highly heterogeneous, with several studies suggesting that a subset of patients demonstrate progression to end-stage fibrosis; criteria to define this group at the time of diagnosis would be helpful.
-
2.
New information has accumulated on smoking-related interstitial lung disease, including patients with combined emphysema and interstitial fibrosis. In clinical practice, respiratory bronchiolitis–interstitial lung disease is increasingly diagnosed without surgical lung biopsy in smokers on the basis of clinical and imaging features (ground-glass opacities and centrilobular nodules) and bronchoalveolar lavage (smoker’s macrophages and absence of lymphocytosis).
-
3.
The natural progression of idiopathic pulmonary fibrosis (IPF) is acknowledged to be heterogeneous with some patients remaining stable for prolonged periods, others showing more rapid steady progression, and still others succumbing to acute exacerbation.
-
4.
Acute exacerbation is better defined and recognized to occur in chronic fibrosing IIPs (IPF and NSIP).
-
5.
Some patients with IIP are difficult to classify, often because of mixed patterns of lung injury.
-
6.
It is recognized that there is a need to provide a clinical algorithm for classifying and managing IIP cases. This is particularly applicable when no biopsy is available and high-resolution computed tomography is not diagnostic.
-
7.
Pleuroparenchymal fibroelastosis is recognized as a specific rare entity, usually idiopathic. Other less well-defined histologic patterns, such as bronchiolocentric inflammation and fibrosis, are also included.
-
8.
A rapidly emerging field of molecular markers holds promise for improving diagnostic approaches. These markers may also be useful in predicting prognosis and response to different therapies. Incorporation of genetic and molecular studies may revolutionize the approach to diagnosis and classification of the IIPs.
Introduction
The objective of this statement is to update the 2002 American Thoracic Society/European Respiratory Society (ATS/ERS) classification of idiopathic interstitial pneumonias (IIPs) (1). Focus is placed on describing changes to previously described clinical entities, describing new clinical entities, and describing new histologic patterns. This update is not intended as a stand-alone document and should be used as a supplement to the original 2002 IIP classification. In 2002, the ATS/ERS IIP classification (1) defined seven disease categories, and proposed standardized terminology and diagnostic criteria. In addition, the historical “gold standard” of histologic diagnosis was replaced by a “dynamic integrated approach” using multidisciplinary discussion (MDD). The 2002 IIP classification was used in 75% (157 of 208) of all clinical publications on the topic of IIPs between 2004 and 2011. The new information from these publications is incorporated in this update.
Methods
This project was performed under supervision by the ATS Documents Development and Implementation Committee in collaboration with the ERS (Table E1 in the online supplement). An international multidisciplinary panel was assembled. The panel consisted of 34 experts in interstitial lung diseases (19 pulmonologists, 4 radiologists, 5 pathologists, 2 experts in evidence-based medicine, and 4 molecular biologists). Several meetings were held by members of the international multidisciplinary panel (Table E2), who disclosed conflicts of interest, which were vetted according to ATS and ERS policies.
Key questions were developed that the committee believed important for the classification of IIPs (see Appendix 1 in the online supplement). A literature search was performed to identify new publications that pertained to these key questions, assisted by two librarians experienced in literature searches for pulmonary diseases. Literature retrieved from Medline searches between 2000 and 2011 was used to produce this statement.
The committee was divided into subgroups assigned to specific sections of the document. These subgroups reviewed the relevant literature and produced the first draft of their respective sections. These sections were compiled by the committee chair and a complete first draft was edited by the writing subcommittee. This document was reviewed and edited by all committee members before final review by the writing subcommittee. The revised document was approved by all authors.
Summary of Major Revisions of the IIP Classification
In the revision of the IIP classification, the main entities are preserved (Table 1). However, there are several important changes. First, cryptogenic fibrosing alveolitis is removed, leaving idiopathic pulmonary fibrosis (IPF) as the sole clinical term for this diagnosis. Second, idiopathic nonspecific interstitial pneumonia (NSIP) is now accepted as a distinct clinical entity with removal of the term “provisional” (2). Third, major IIPs are distinguished from rare IIPs and unclassifiable cases. Fourth, rare histologic patterns of acute fibrinous and organizing pneumonia (AFOP) and interstitial pneumonias with a bronchiolocentric distribution are recognized. Fifth, the major IIPs are grouped into chronic fibrosing (IPF and NSIP; Figures 1 and 2), smoking-related (respiratory bronchiolitis–interstitial lung disease [RB-ILD] and desquamative interstitial pneumonia [DIP]; Figure 3), and acute/subacute IIPs (cryptogenic organizing pneumonia [COP] and acute interstitial pneumonia [AIP]; Figure 4 and Table 2). Sixth, a clinical disease behavior classification is proposed. Last, molecular and genetic features are reviewed.
TABLE 1.
REVISED AMERICAN THORACIC SOCIETY/EUROPEAN RESPIRATORY SOCIETY CLASSIFICATION OF IDIOPATHIC INTERSTITIAL PNEUMONIAS: MULTIDISCIPLINARY DIAGNOSES
| Major idiopathic interstitial pneumonias |
| Idiopathic pulmonary fibrosis |
| Idiopathic nonspecific interstitial pneumonia |
| Respiratory bronchiolitis–interstitial lung disease |
| Desquamative interstitial pneumonia |
| Cryptogenic organizing pneumonia |
| Acute interstitial pneumonia |
| Rare idiopathic interstitial pneumonias |
| Idiopathic lymphoid interstitial pneumonia |
| Idiopathic pleuroparenchymal fibroelastosis |
| Unclassifiable idiopathic interstitial pneumonias* |
Causes of unclassifiable idiopathic interstitial pneumonia include (1) inadequate clinical, radiologic, or pathologic data and (2) major discordance between clinical, radiologic, and pathologic findings that may occur in the following situations: (a) previous therapy resulting in substantial alteration of radiologic or histologic findings (e.g., biopsy of desquamative interstitial pneumonia after steroid therapy, which shows only residual nonspecific interstitial pneumonia [153]); (b) new entity, or unusual variant of recognized entity, not adequately characterized by the current American Thoracic Society/European Respiratory Society classification (e.g., variant of organizing pneumonia with supervening fibrosis) (79); and (c) multiple high-resolution computed tomography and/or pathologic patterns that may be encountered in patients with idiopathic interstitial pneumonia.
Figure 1.
Atypical usual interstitial pneumonia/idiopathic pulmonary fibrosis. Computed tomography (CT) features: (A) CT image of atypical usual interstitial pneumonia (UIP). Prone axial CT through the lung bases in a patient with histologically proven UIP shows predominantly peribronchovascular ground-glass/reticular opacities with traction bronchiectasis. Under the ATS/ERS/JRS/ALAT Statement (8), this would be classified as inconsistent with UIP. Histologic features: (B) The biopsy shows patchy subpleural dense fibrosis with honeycomb change adjacent to preserved lung. (C) Dense scarring fibrosis is present with a small nodular fibroblastic focus.
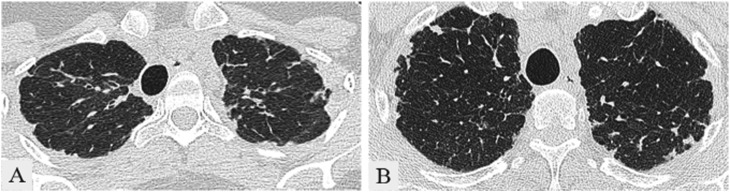
Figure 2.
Nonspecific interstitial pneumonia. Computed tomography (CT) features: (A) Axial and (B) coronal CT reconstructions show confluent bilateral lower lobe ground-glass opacities with marked traction bronchiectasis and lower lobe volume loss. The peribronchovascular predominance with subpleural sparing is well shown on the axial image. (C and D) Histologic features: Lung biopsy shows diffuse alveolar wall thickening by uniform fibrosis. The alveolar architecture is preserved and no honeycombing or fibroblastic foci are seen. Interstitial inflammation is mild.
Figure 3.
Respiratory bronchiolitis–interstitial lung disease. (A) Axial and (B) coronal computed tomography (CT) reconstructions in a 47-year-old heavy cigarette smoker show moderately extensive ground-glass opacities and centrilobular nodules (circles). The bronchi are markedly thick-walled and there is minimal emphysema. Bronchoalveolar lavage yielded 91% macrophages. (C) Histologic features: lung biopsy shows peribronchiolar pigmented macrophage accumulation and emphysema. (D) There is mild bronchiolar fibrosis and pigmented macrophages within airspaces.
Figure 4.
Cryptogenic organizing pneumonia. Computed tomography (CT) features with (A) peripheral consolidation and air bronchograms, (B) bronchocentric distribution, (C) perilobular pattern showing focal right lower lobe consolidation, with more central ground-glass opacity, corresponding to the reversed halo sign, and (D) bandlike consolidation.
TABLE 2.
CATEGORIZATION OF MAJOR IDIOPATHIC INTERSTITIAL PNEUMONIAS
| Category | Clinical–Radiologic–Pathologic Diagnoses | Associated Radiologic and/or Pathologic–Morphologic Patterns |
|---|---|---|
| Chronic fibrosing IP | Idiopathic pulmonary fibrosis | Usual interstitial pneumonia |
| Idiopathic nonspecific interstitial pneumonia | Nonspecific interstitial pneumonia | |
| Smoking-related IP* | Respiratory bronchiolitis-interstitial lung disease | Respiratory bronchiolitis |
| Desquamative interstitial pneumonia | Desquamative interstitial pneumonia | |
| Acute/subacute IP | Cryptogenic organizing pneumonia | Organizing pneumonia |
| Acute interstitial pneumonia | Diffuse alveolar damage |
Definition of abbreviation: IP = interstitial pneumonia.
Desquamative interstitial pneumonia can occasionally occur in nonsmokers.
General Progress in IIPs since 2002
Multidisciplinary Approach
The process of achieving a multidisciplinary diagnosis in a patient with IIP is dynamic, requiring close communication between clinician, radiologist, and when appropriate, pathologist (1). Clinical data (presentation, exposures, smoking status, associated diseases, lung function, laboratory findings) and radiologic findings are essential for multidisciplinary diagnosis.
The multidisciplinary approach does not lessen the importance of lung biopsy in the diagnosis of IIPs; rather, it defines the settings where biopsy is more informative than high-resolution computed tomography (HRCT) and those where biopsy is not needed. Also, once a pathologist has recognized a histologic pattern (e.g., NSIP or organizing pneumonia [OP]), the clinician should reconsider potential causes (e.g., hypersensitivity pneumonitis [HP], collagen vascular disease [CVD], and drug exposure).
The diagnosis of IIPs requires exclusion of known causes of interstitial lung disease such as drug or inhalational exposure and CVD. Despite the known association of smoking with RB-ILD and DIP, these disorders were included in the classification in 2002 and they are maintained in this revision.
Observer Agreement in Diagnosis of IIP
Observer agreement is dependent on observer experience and the integration of data from all modalities. In early series, observer agreement was marginal among clinicians, radiologists, and pathologists (3–5). However, agreement between radiologists and pathologists has improved substantially with accumulated experience (6) and, especially, with integration of clinical data in a multidisciplinary conference (4, 7). Academic physicians in a multidisciplinary setting have better diagnostic agreement than community physicians, who are more likely to assign the diagnosis of IPF (7). These data underline the need for patient evaluation in regional centers using multidisciplinary evaluation (7, 8).
Important Differential Diagnostic Considerations
Hypersensitivity Pneumonitis
IIPs are frequently confused with HP, and vice versa, except when the exposure is readily apparent. The ATS workshop on NSIP showed that MDD is particularly important in distinguishing HP from NSIP (2). In the past 10 years, the clinical (9), HRCT (10–12), and pathologic (13–15) features of chronic HP have been more sharply defined, helping to separate these cases from the IIPs, particularly IPF and NSIP (9, 11–16). HRCT findings suggesting HP include centrilobular nodules, mosaic air-trapping, and upper lobe distribution (Figures 5A and 5B) (11, 12). Biopsy findings suggesting HP include bronchiolocentric distribution and poorly formed granulomas (Figures 5C and 5D) (13–15). A detailed search for potential exposure in patients with these findings is essential, including consideration of specific circulating IgG antibodies, but up to 30% of subjects with histologic HP have no identifiable exposure (17, 18).
Figure 5.
Fibrotic hypersensitivity pneumonitis. (A) Axial and (B) coronal computed tomography (CT) reconstructions in a 76-year-old bird-keeper with progressive shortness of breath over 6 years show upper lung–predominant subpleural reticulation with some confluent areas of dense opacification, traction bronchiectasis, and patchy ground-glass opacities. Honeycombing is not identified. (C) Histology shows a bronchiolocentric cellular and fibrosing interstitial pneumonia. (D) There is a patchy cellular interstitial infiltrate and poorly formed granulomas.
Collagen Vascular Disease
CVD is a frequent cause of interstitial pneumonia patterns, especially NSIP. Clinical, serologic, HRCT, and histologic findings may be helpful in distinguishing IIPs from ILD associated with CVD (19–22). The extent of serologic evaluation to be performed in the evaluation of suspected IPF has been suggested previously (8). A substantial percentage of patients with NSIP have findings suggesting, but not meeting, criteria for a defined CVD (23–25). However, these cases are still accepted as IIPs.
Familial Interstitial Pneumonia
IIPs have been reported in closely related family members in 2–20% of cases (26–29). These cases remain classified as IIPs despite the genetic predisposition. Heterozygous mutations in SFTPC (∼1%), SFTPA2 (∼1%), TERT (∼15%), and TERC (∼1%) are responsible for about 20% of all familial interstitial pneumonias (FIPs) (29–32). Sporadic IPF, in the absence of telomerase mutations, is often associated with telomere shortening, suggesting that pathways involved in familial disease may contribute to sporadic disease (33–35). Most FIP families (80%) have evidence of vertical transmission suggesting single autosomal dominant mechanisms, but most responsible genes have not yet been identified. A recent genome-wide linkage scan showed that a common variant in the promoter of the MUCB gene is associated with the development of both familial and sporadic IPF. This result was confirmed in an independent cohort (36, 37).
Familial IIPs can be indistinguishable from nonfamilial cases on HRCT and lung biopsy. All patients with suspected IIP should therefore be questioned about relevant family history as this may guide gene mutation search, and management or evaluation of other family members (38).
Coexisting Patterns
Most patients with a chronic IIP can be given a single clinical–radiologic–pathologic diagnosis. However, multiple pathologic and/or HRCT patterns may be found in the same patient. Different patterns may be seen in a single biopsy or in biopsies from multiple sites (e.g., usual interstitial pneumonia [UIP] in one lobe and NSIP in another) (39), or when pathologic and HRCT patterns differ. In smokers, multiple HRCT and histologic features may coexist including Langerhans’ cell histiocytosis, respiratory bronchiolitis (RB), desquamative interstitial pneumonia (DIP), pulmonary fibrosis (UIP or NSIP), and emphysema (40–42). Combined pulmonary fibrosis and emphysema (CPFE) is an example of coexisting patterns. CPFE comprises a heterogeneous population of patients, not believed to represent a distinctive IIP. Patients with CPFE have increased risk of developing pulmonary hypertension, which portends poor prognosis (43–46). When coexisting patterns occur, MDD may determine the clinical significance of individual patterns (4, 47, 48).
Progress in Specific IIPs since 2002
Chronic Fibrosing IIPs
Idiopathic pulmonary fibrosis.
An updated evidence-based guideline for the diagnosis and management of IPF was recently published (8). A new diagnostic algorithm and schema for correlating histologic and radiologic findings in patients with suspected IPF was provided in this guideline (8). New aspects of this algorithm included criteria for three levels of certainty for patterns of UIP based on HRCT findings (UIP, possible UIP, and inconsistent with UIP) and four levels of certainty for pathologic diagnosis (UIP, probable, possible, and not UIP) (8). The diagnosis of IPF requires (1) exclusion of other known causes of ILD, (2) the presence of a UIP pattern on HRCT in patients not subjected to surgical lung biopsy (SLB), and (3) specific combinations of HRCT and SLB patterns in patients subjected to SLB (Figures 1A–1C).
Histologic UIP may be associated with atypical HRCT patterns (Figures 1A–1C) (8), including extensive ground-glass opacity, nodules, or mosaic attenuation, and after MDD some of these patients will be diagnosed with IPF (49–52). Typical UIP HRCT pattern is illustrated elsewhere (1, 8). Patients with IPF and definite UIP by HRCT have shorter survival than those with indeterminate HRCT findings (49, 51, 53).
Idiopathic nonspecific interstitial pneumonia.
The diagnostic criteria for NSIP were summarized in a recent ATS workshop (2). On the basis of the analysis of cases and the available literature, this workshop recommended that NSIP be accepted as a distinct entity among the IIPs, with removal of the term “provisional.” Importantly, the NSIP pattern occurs not only as an idiopathic condition, but also in a variety of settings including CVD, HP, and drug toxicity, and in some patients with familial pulmonary fibrosis. MDD is especially important to establish the diagnosis of idiopathic NSIP (2).
The most common HRCT abnormality in NSIP is bilateral ground-glass opacity (Figures 2A and 2B) (26, 54–62). Irregular reticular opacities with traction bronchiectasis and bronchiolectasis occur in approximately 75% of cases (2, 54–62). Subpleural sparing may be helpful in distinguishing NSIP from UIP (2, 12, 52). Consolidation, if present, reflects an OP component and may suggest CVD. Honeycombing is sparse or absent at presentation but may increase in prevalence and extent during follow-up (63).
The histologic features include varying amounts of interstitial inflammation and fibrosis with a uniform appearance (Figures 2C and 2D) (2, 64, 65). Most cases of NSIP have a predominantly fibrotic pattern of injury with rare cases of isolated cellular NSIP (59, 62, 66). OP and honeycomb fibrosis should be inconspicuous or absent.
The prognosis is variable. Some patients improve, others remain stable or improve on treatment, but some evolve to end-stage fibrosis and eventually die of the disease (2, 63, 67).
Smoking-related IIPs
RB-ILD and desquamative interstitial pneumonia (DIP) represent a histologic spectrum of macrophage accumulation, with the distinction dependent on the extent and distribution of this process (and also reflected by the pattern of disease on HRCT). However, clinical presentation, imaging findings, and response to therapy differ and they remain classified separately. In the last decade, the term “smoking-related interstitial lung disease” has increasingly been used, encompassing most cases of DIP, and nearly all cases of RB-ILD and Langerhans’ cell histiocytosis (68, 69).
Respiratory bronchiolitis–interstitial lung disease.
Histologic RB is always present in current smokers (70) and can be viewed as a physiological response to smoking, which in a few individuals becomes extensive enough to result in an interstitial lung disease (RB-ILD). Characteristic HRCT features are ground-glass opacity and centrilobular nodules (Figures 3A and 3B). In clinical practice, RB-ILD is increasingly diagnosed without surgical lung biopsy in smokers with these HRCT findings and where bronchoalveolar lavage demonstrates smokers’ macrophages and the absence of lymphocytosis (potentially suggestive of HP in this setting, although HP is uncommon in smokers) (68, 71). The disease course is heterogeneous, with a significant minority having progression despite smoking cessation (72).
Desquamative interstitial pneumonia.
DIP has been recognized in nonsmokers (69), perhaps reflecting extension of childhood DIP into adult life (with the latter often due to surfactant protein [SP] gene mutations) (73, 74). Ten-year survival remains approximately 70%, with resistance to treatment in a significant minority.
Airspace enlargement with fibrosis.
DIP and RB-ILD need to be distinguished from the smoking-related changes including respiratory bronchiolitis and airspace enlargement with fibrosis (AEF) that have been described in the nonneoplastic lung parenchyma in lung cancer resection specimens (75, 76). These incidental HRCT and histologic findings in smokers are not regarded as a distinct form of IIP, but AEF shows more interstitial fibrosis than described in the classic definition of emphysema (77). AEF is an incidental histologic or HRCT finding, whereas patients with CPFE have clinically manifestations reflecting coexisting patterns of interstitial fibrosing and emphysema.
Acute or Subacute IIPs
IIPs may have an acute or subacute presentation, or an acute exacerbation may occur in a previously subclinical or unrecognized chronic IIP.
Cryptogenic organizing pneumonia.
COP continues to be included in the classification of IIP because of its idiopathic nature and the tendency on occasions to be confused with other forms of IIP, especially when there is progression to fibrosis. Because many cases are secondary, use of the generic term “OP” for this reaction pattern is suggested with modifiers as appropriate, for example, OP associated with rheumatoid arthritis.
Patients with COP typically present with a subacute illness of relatively short duration (median, less than 3 mo) with variable degrees of cough and dyspnea (78–81). HRCT characteristically demonstrates patchy and often migratory consolidation in a subpleural, peribronchial, or bandlike pattern (Figures 4A–4D) (82–84), commonly associated with ground-glass opacity (79, 83). Perilobular opacities and reversed halo (or atoll) sign (Figure 4C) may be helpful in suggesting the diagnosis (85, 86). Small unilateral or bilateral pleural effusion may occur in 10–30% of patients (83, 84, 86). The OP pattern is a patchy process characterized primarily by organizing pneumonia involving alveolar ducts and alveoli with or without bronchiolar intraluminal polyps. Some cases show more marked interstitial inflammation such that there is overlap with cellular NSIP.
The majority of patients recover completely with oral corticosteroids, but relapse is common (2, 78, 87). Sporadic reports have identified a subgroup of patients with OP that does not completely resolve despite prolonged treatment. Some of these cases are characterized by residual or progressive interstitial fibrosis, with or without recurrent episodes of OP (79, 88, 89). It is likely that some patients reported with fibrotic NSIP fall into this subgroup of patients with a fibrosing variant of OP. In such patients consolidation is prominent on HRCT, variably associated with reticular abnormalities. Some patients with this pattern of mixed fibrosis and organizing pneumonia are found to have underlying polymyositis or antisynthetase syndrome (90).
Acute interstitial pneumonia.
AIP is a distinct IIP characterized by rapidly progressive hypoxemia, mortality of 50% or more, and no proven treatment. Survivors usually have a good long-term prognosis (similar to adult respiratory distress syndrome [ARDS] survivors) but some experience recurrences or chronic, progressive interstitial lung disease (91–93). AIP is idiopathic and should be distinguished from ARDS with known cause.
In the early, exudative phase of AIP, HRCT shows bilateral patchy ground-glass opacities, often with consolidation of the dependent lung (94–96). The later, organizing stage of AIP is associated with distortion of bronchovascular bundles and traction bronchiectasis. HRCT scoring of extent of abnormality is independently associated with mortality (93, 97). Biopsy shows an acute and/or organizing form of diffuse alveolar damage (DAD) that is indistinguishable from the histologic pattern found in ARDS (1). In the organizing phase, when most patients undergo biopsy, hyaline membranes may be inconspicuous or absent and the key findings include diffuse distribution, loose organizing connective tissue causing alveolar wall thickening and prominent pneumocyte hyperplasia. Occult background fibrosis may be present and if this shows features of UIP, acute exacerbation of underlying IPF should be considered (98). AIP can progress to a pattern similar to fibrotic NSIP (64) or to severe fibrosis resembling honeycombing (99).
Acute exacerbation of IIP.
Acute exacerbation occurs mostly in IPF, but is also found in other fibrosing interstitial pneumonias (100–106). Diagnostic criteria have been published for acute exacerbation of IPF (107). In acute exacerbations of IPF, HRCT shows new bilateral ground-glass opacities and/or consolidation superimposed on a reticular pattern or honeycombing (Figures 6A and 6B) (108–110). The pathology most often shows a mixed pattern of UIP and DAD (Figures 6C and 6D), but OP and prominent fibroblastic foci are also described as the acute component (103). It is important to exclude infection, left heart failure, and other identifiable causes of acute lung injury before diagnosing an acute exacerbation of an underlying IIP (107).
Figure 6.
Acute exacerbation of idiopathic pulmonary fibrosis (IPF). Computed tomography (CT) features: (A) Axial image through the upper lungs at baseline shows mild peripheral, basal predominant reticular abnormality without honeycombing and mild emphysema. (B) Axial image during an acute exacerbation 4 months later shows extensive new bilateral ground-glass opacities, with some superimposed reticular abnormality. (C and D) Histologic features: (C) Usual interstitial pneumonia pattern with honeycomb fibrosis and fibroblastic foci. (D) Focally, features of diffuse alveolar damage are present with uniform thickening of alveolar walls and hyaline membranes.
Rare IIPs
The category of rare IIPs has been created to include idiopathic lymphoid interstitial pneumonia (LIP) and idiopathic pleuroparenchymal fibroelastosis (PPFE). In addition, several rare histologic patterns of ILD have been described including AFOP and a group of bronchiolocentric patterns, although current data do not support these as distinct IIPs.
Idiopathic Lymphoid Interstitial Pneumonia
Most cases of LIP are associated with other conditions, although idiopathic cases still rarely occur (111). Idiopathic LIP has therefore been moved to the category of rare IIPs. The clinical, imaging, and histopathologic criteria for LIP proposed in 2002 remain unchanged, apart from recognition that some cases show striking cyst formation on HRCT (111, 112). Both the 2002 IIP classification and the ATS NSIP project demonstrated that many of the cases previously diagnosed as LIP are now considered cellular NSIP (1, 2). Consequently, few cases of idiopathic LIP have been published since 2002 (111).
Idiopathic Pleuroparenchymal Fibroelastosis
PPFE is a rare condition that consists of fibrosis involving the pleura and subpleural lung parenchyma, predominantly in the upper lobes. HRCT shows dense subpleural consolidation with traction bronchiectasis, architectural distortion, and upper lobe volume loss (Figures 7A and 7B) (113). The fibrosis is elastotic, and intraalveolar fibrosis is present (Figures 8A and 8B) (113–117). It presents in adults with a median age of 57 years and has no sex predilection (113). Approximately half of patients have experienced recurrent infections. Pneumothorax is common. A minority has familial interstitial lung disease and nonspecific autoantibodies. Histologically, biopsies may show mild changes of PPFE or other patterns such as UIP. Disease progression occurs in 60% of patients with death from disease in 40% (113, 118).
Figure 7.
Pleuroparenchymal fibroelastosis. Computed tomography (CT) features: (A) High-resolution computed tomography (HRCT) through the upper lobes shows irregular pleural-based opacities and a reticular pattern associated with parenchymal distortion. The pleura and lungs in the lower lobes appeared normal. (B) Section through the upper lobes shows scattered pleuroparenchymal opacities and some distortion of the underlying lung parenchyma. In the lower lobes there was no pleural irregularity, but there was a subtle subpleural reticular pattern.
Figure 8.
Pleuroparenchymal fibroelastosis. (A) Low power shows pleural thickening and subpleural fibrosis. (B) Dense masses of elastic fibers are highlighted beneath the fibrotically thickened pleura (elastic stain).
Rare Histologic Patterns
Rare histologic interstitial pneumonia patterns have been described and these were not included as new IIP entities because of questions concerning whether they are variants of existing IIPs or exist only in association with other conditions such as HP or CVD. When encountered histologically, these terms may be of value in provisionally classifying biopsy features before MDD.
Acute Fibrinous and Organizing Pneumonia
AFOP was first reported in 17 patients with acute respiratory failure and initially regarded to represent a possible new IIP (119). The principal HRCT findings are bilateral basal opacities and areas of consolidation (Figure 9A). The dominant histologic pattern is intraalveolar fibrin deposition and associated organizing pneumonia (Figures 9C and 9D). Classical hyaline membranes of DAD are absent. AFOP may represent a histologic pattern that can occur in the clinical spectrum of DAD and OP or it may reflect a tissue sampling issue. AFOP may be idiopathic or associated with CVD (120), hypersensitivity pneumonitis (121), or drug reaction (122). As this pattern can be seen in eosinophilic pneumonia, this diagnosis should be excluded by absence of tissue and peripheral eosinophilia.
Figure 9.
Acute fibrinous and organizing pneumonia. Computed tomography (CT) features. (A) Axial CT through the lung bases shows multiple poorly defined nodules and areas of consolidation, with peribronchovascular and basal predominance. Pleural and pericardial effusions are present. Histologic features: (B) Biopsy shows nodules of alveolar fibrin and organizing pneumonia. (C) The histology is dominated by intraalveolar plugs of alveolar fibrin.
Bronchiolocentric Patterns of Interstitial Pneumonia
Several small retrospective series have recently described bronchiolocentric fibroinflammatory changes (123–126). Of these, two studies in particular suggest these cases may be an IIP centered on airways (123, 125), although imaging findings were not well characterized and in one series there were environmental or occupational exposures in most cases (123). One study described cases of peribronchiolar metaplasia-ILD, which probably represent a form of small airway disease. The HRCTs in these cases were either normal or showed air trapping (124).
Unclassifiable IIP
The 2002 ATS/ERS classification proposed an “unclassifiable” category of IIP, acknowledging that a final diagnosis may not be achieved, even after lengthy MDD (1). Examples of circumstances in which a case cannot be satisfactorily classified are summarized in Table 1 (127). Cases that are “unclassifiable” in terms of overlap of histologic patterns often prove to be related to CVD (e.g., interstitial pneumonia and follicular bronchiolitis in a patient with rheumatoid arthritis) or drug induced, rather than being idiopathic on MDD. If ILD is difficult, or impossible, to classify, management should be based on the most probable diagnosis after MDD and consideration of the expected disease behavior (as described below).
Clinical Classification of Disease Behavior
Patterns of disease behavior in diffuse lung disorders and related treatment approaches can be broadly subdivided as shown in Table 3. This approach is most useful in unclassifiable cases and for some IIPs, such as NSIP, that can be associated with all five patterns of disease behavior. This disease behavior classification is complementary to the IIP classification and should not be used as a justification for delaying SLB. Such delays increase the risk of surgical complications and may result in inappropriate management. This classification system needs to be validated for practicality and clinical relevance (127).
TABLE 3.
IDIOPATHIC INTERSTITIAL PNEUMONIAS: CLASSIFICATION ACCORDING TO DISEASE BEHAVIOR*
| Clinical Behavior | Treatment Goal | Monitoring Strategy |
|---|---|---|
| Reversible and self-limited (e.g., many cases of RB-ILD) | Remove possible cause | Short-term (3- to 6-mo) observation to confirm disease regression |
| Reversible disease with risk of progression (e.g., cellular NSIP and some fibrotic NSIP, DIP, COP) | Initially achieve response and then rationalize longer term therapy | Short-term observation to confirm treatment response. Long-term observation to ensure that gains are preserved |
| Stable with residual disease (e.g., some fibrotic NSIP) | Maintain status | Long-term observation to assess disease course |
| Progressive, irreversible disease with potential for stabilization (e.g., some fibrotic NSIP) | Stabilize | Long-term observation to assess disease course |
| Progressive, irreversible disease despite therapy (e.g., IPF, some fibrotic NSIP) | Slow progression | Long-term observation to assess disease course and need for transplant or effective palliation |
Definition of abbreviations: COP = cryptogenic organizing pneumonia; DIP = desquamative interstitial pneumonia; HRCT = high-resolution computed tomography; IPF = idiopathic pulmonary fibrosis; NSIP = nonspecific interstitial pneumonia; RB-ILD = respiratory bronchiolitis–interstitial pneumonia.
The distinctions in Table 3 are made by assimilating several factors: (1) A confident multidisciplinary diagnosis that often identifies the expected pattern of disease behavior (e.g., IPF). However, in other idiopathic interstitial pneumonias (e.g., NSIP) more than one pattern of behavior is possible; (2) disease severity, based on lung function and/or HRCT. In severe NSIP (154) a progressive irreversible course is frequent; (3) evaluation of potentially reversible and irreversible features based on review of the HRCT and biopsy if available; and (4) short-term disease behavior. Disease behavior classification must be refined over time in individual patients considering longitudinal changes in disease severity.
Biomarkers
Identification of biomarkers has been focused on IPF and usually in small cohorts and without independent validation. However, some interesting findings have emerged that may have implications for diagnosis, management, or prognostication of other IIPs (Table 4). For example, rapidly declining lung function and/or reduced survival have been associated with high serum levels of some epithelial or macrophage-related proteins such as SP-A, SP-D, KL-6 (Krebs von den Lungen-6), CCL18 (chemokine ligand-18), and MMP-7 (matrix metalloproteinase-7) (29, 128–131). These associations require validation, but suggest that biomarkers may be clinically useful to identify patients at high risk of progression.
TABLE 4.
BIOMARKERS FOR OUTCOME IN BLOOD AND BRONCHOALVEOLAR LAVAGE (HIGHER LEVELS PREDICTING POOR SURVIVAL)
| Biomarker | Patients | HR (95% CI) | P Value | Reference |
|---|---|---|---|---|
| SP-A | 52 IPF (survivors vs. nonsurvivors) | 0.0125 | Takahashi et al. (155) | |
| SP-D | 0.0032 | |||
| SP-A | 142 IPF | 1.73 | 0.031 | Greene et al. (156) |
| SP-D | 2.04 | 0.003 | ||
| KL-6 (>1,000 U/ml) | 27 IPF | 12.56 (1.195–131.90) | 0.035 | Yokoyama et al. (157) |
| KL-6 (≥1,000 U/ml) | 152 IIP and 67 CVD | 2.95 (1.71–5.08) | 0.0001 | Satoh et al. (129) |
| SP-D (≥253) | 82 IPF | 0.0013 | Takahashi et al. (158) | |
| SP-A | NS | |||
| KL-6 (>1.014) | 0.0087 | |||
| Oxidative stress levels | 21 IPF | FVC r = –0.79 | <0.01 | Daniil et al. (159) |
| DlCOr = –0.75 | <0.01 | |||
| MMP-7 | 74 IPF | Higher decline of DlCO (r = –0.53) and FVC (r = –0.51) | 0.002 | Rosas et al. (160) |
| MMP-1 | 0.002 | |||
| SP-A | 82 IPF | 3.27 (1.49–7.17) | 0.003 | Kinder et al. (128) |
| SP-D (>460 ng/ml) | 72 IPF | 3.22 (1.33– 7.81) | 0.01 | Barlo et al. (29) |
| CCL18 above 150 ng/ml | 72 IPF | 7.98 (2.49–25.51) | 0.0005 | Prasse et al. (131) |
| CD4+CD28null > 18% of total CD4 | 89 IPF | 13.0 (1.6–111.1) | 0.0004 | Gilani et al. (161) |
| MMP-7, ICAM-1, IL-8, VCAM-1, S100-A12 | 241 IPF (140, derivation; 101, validation) | In the derivation cohort, high concentration predicted poor survival, poor transplant-free survival and poor progression-free survival. In the validation cohort high concentrations of all five were predictive of poor transplant-free survival; MMP-7, ICAM-1, and IL-8 of overall survival; and ICAM-1 of poor progression-free survival | Overall survival derivation cohort | Richards et al. (162) |
| MMP-7: 0.0021 | ||||
| ICAM-1: 0.0015 | ||||
| IL-8: 0.029 | ||||
| VCAM-1: 0.00030 | ||||
| S100-A12: 0.0013 | ||||
| BAL | 20 IPF | Higher in rapid progressors | 0.028 | McKeown et al.* (163) |
| MMP-8, MMP-9 | 0.015 | |||
| BAL | 39 IPF | Higher in nonsurvivors | <0.02 | Shinoda et al.* (164) |
| CCL2 | ||||
| BAL | 20 IPF | Negative correlation with PFT | Richter et al.* (165) | |
| Endostatin | FVC (r = –0.604) | 0.006 | ||
| TlCO (r = –0.612) | 0.005 |
Definition of abbreviations: BAL = bronchoalveolar lavage; CI = confidence interval; CCL = chemokine ligand; CVD = collagen vascular disease; DlCO = diffusing capacity or transfer factor of the lung for carbon monoxide; HR = hazard ratio; ICAM = intercellular adhesion molecule; IPF = idiopathic pulmonary fibrosis; KL-6 = Krebs von den Lungen-6; MMP = matrix metalloproteinase; NS = not significant; PFT = pulmonary function test; S100-A12 = protein encoded by S100-A12 gene; SP = surfactant protein; TlCO = carbon monoxide diffusion factor; VCAM = vascular cell adhesion protein.
Regarding biomarkers for differential diagnosis, serum SP-A and SP-D were found significantly higher in IPF compared with NSIP/COP or CVD-IP, respectively (132, 133). Likewise, higher levels of serum DNA seem to distinguish patients with IPF from non-IPF patients (134). Studies in lungs and bronchoalveolar lavage fluid indicate that NSIP is characterized by a helper T-cell type 1–like pattern whereas a helper T-cell type 2–like response with increased expression of chemokine receptor-7 (CCR7) and CCL7 is observed in IPF (135–138). Last, gene expression profiling has given contradictory results. Whereas one study found that most NSIP lungs did not resemble IPF, another identified only minor gene expression differences between UIP and NSIP (139).
Many association studies have failed to identify genetic polymorphisms that may confer increased risk of developing IPF (140, 141), whereas those showing association have not been validated in independent cohorts (140–152).
Acknowledgments
This official statement was prepared by an ad hoc subcommittee of the Assembly on Clinical Problems.
Members of the ATS/ERS Committee on Idiopathic Interstitial Pneumonias:
William D. Travis, M.D. (Chair)
Talmadge E. King, Jr., M.D. (Co-Chair)
Ulrich Costabel, M.D. (Co-Chair)
Athol U. Wells, M.D. (Co-Chair)
Writing Committee
William D. Travis, M.D.
Ulrich Costabel, M.D.
David M. Hansell, M.D., M.P.H.
Talmadge E. King, Jr., M.D.
David A. Lynch, M.B.B.Ch.
Andrew G. Nicholson, D.M.
Christopher J. Ryerson, M.D.
Jay H. Ryu, M.D.
Moisés Selman, M.D.
Athol U. Wells, M.D.
Pulmonary
Jay H. Ryu, M.D. (Subcommittee Chair)
Jurgen Behr, M.D.
Demosthenes Bouros, M.D., Ph.D.
Kevin K. Brown, M.D.
Harold R. Collard, M.D.
Carlos Robalo Cordeiro, M.D., Ph.D.
Vincent Cottin, M.D., Ph.D.
Marjolein Drent, M.D., Ph.D.
Jim Egan, M.D., M.B.B.Ch.B.A.O.
Kevin Flaherty, M.D., M.S.
Yoshikazu Inoue, M.D., Ph.D.
Dong Soon Kim, M.D.
Fernando J. Martinez, M.D., M.S.
Ganesh Raghu, M.D.
Luca Richeldi, M.D., Ph.D.
Dominique Valeyre, M.D.
Radiology
David M. Hansell, M.D. (Subcommittee Co-Chair)
David A. Lynch, M.B.B.Ch. (Subcommittee Co-Chair)
Takeshi Johkoh, M.D., Ph.D.
Nicola Sverzellati, M.D.
Pathology
Andrew G. Nicholson, D.M. (Subcommittee Chair)
Thomas V. Colby, M.D.
Masanori Kitaichi, M.D.
Jeffrey Myers, M.D.
Molecular Biology
Moisés Selman, M.D. (Subcommittee Chair)
Bruno Crestani, M.D., Ph.D.
Cory Hogaboam, Ph.D.
James Loyd, M.D.
Evidence-based Analysis
Christopher J. Ryerson, M.D. (Subcommittee Chair)
Jeffrey Swigris, D.O., M.S.
Reference Librarians
Rosalind F. Dudden, M.L.S.
Shandra Protzko, M.S.
Acknowledgment
The committee acknowledges the American Thoracic Society and European Respiratory Society for supporting this project; the staff of the University of Modena and Reggio Emilia, Italy; Shandra Protzko and Rosalin Dudden of the Library and Knowledge Services, National Jewish Health, Denver, Colorado; the Department of Pathology, VU University Medical Center Amsterdam, Amsterdam, The Netherlands, and the Department of Pathology, Memorial Sloan-Kettering Cancer Center, New York, New York for assistance with face-to-face meetings; the ATS staff for administrative assistance; and members of the ATS Documentation and Implementation Committee. The committee also acknowledges the following individuals who helped review the document: Arata Azuma (Japan), Mary Beth Beasley (United States), Alain Borczuk (United States), Marco Chilosi (Italy), Teri Franks (United States), Jeffrey Galvin (United States), Katrien Grunberg (The Netherlands), Richard Helmers (United States), Kevin Leslie (United States), Robert Kaner (United States), Heber MacMahon (United States), Nestor Muller (Brazil), David Naidich (United States), Marieke Overbeek (The Netherlands), Lynette Sholl (United States), Zarir F. Udwadia (India), and Dean W. Wallace (United States).
Footnotes
This Official statement of the American Thoracic Society (ATS) and the European Respiratory Society (ERS) was approved by the ATS Board of Directors, June 2013, and by the ERS Steering Committee, March 2013
This document has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author Disclosures: D.M.H. reported consulting for Astra Zeneca ($1,000–$4,999). T.E.K. reported serving on advisory committees of Immune Works ($1–4,999) and Intermune ($50,000–99,999). D.A.L. reported consulting for Gilead (no payments), Intermune (no payments), and Perceptive Imaging ($25,000–49,999); he received research support from Centocor ($25,000–49,999) and Siemens ($250,000+). A.G.N. reported consulting for Actelion ($50,000–99,999) and Boehringer Ingelheim ($10,000–49,999). C.J.R. reported serving as a speaker and on advisory committees of Intermune ($5,000–24,999), and received research support from Intermune ($50,000–99,999). J.B. reported serving as a consultant, speaker, and on advisory committees of Actelion ($25,000–49,999), and received research support from Actelion ($25,000–49,999); he served as a consultant, speaker, and on advisory committees of Boehringer Ingelheim ($5,000–24,999) and Intermune ($50,000–99,999); he received research support from Intermune ($25,000–49,999). K.K.B. served as a consultant for Almirall ($1–4,999), Amgen ($1–4,999), Array BioPharma ($1–4,999), Genzyme (no payments), GlaxoSmithKline (no payments), Ikaria ($1–4,999), Ironwood ($1–4,999), and Pfizer (no payments); he served on advisory committees of Actelion ($5,000–24,999), Array BioPharma ($1–4,999), Boehringer Ingelheim ($5,000–24,999), Centocor ($1–4,999), Fibrogen ($1–4,999), Genentech ($1–4,999), GeNo (no payments), Gilead ($5,000–24,999), Medimmune ($1–4,999), Mesoblast ($1–4,999), Promedior ($1–4,999), and Stromedix/Biogen ($1–4,999); he received research support from Actelion ($100,000–249,999), Amgen ($25,000–49,999), Genentech ($25,000–49,999), and Gilead ($5,000–24,999). H.R.C. reported consulting for Boehringer Ingelheim ($5,000–24,999), BMS ($1–4,999), Gilead ($5,000–24,999), and Promedior ($1–4,999); he served on advisory committees of Fibrogen ($5,000–24,999), Five Prime ($1–4,999), Genoa ($1–4,999), Medimmune ($1–4,999), and Mesoblast ($1–4,999), and received research support from Genentech ($5,000–24,999) and Intermune (no payments). V.C. reported serving as a speaker and on advisory committees of Intermune ($5,000–24,999); he served on advisory committees of Boehringer Ingelheim ($5,000–24,999) and received research support from Boehringer Ingelheim ($5,000–24,999). B.C. reported consulting for Sanofi ($1–4,999) and serving on advisory committees of Astra Zeneca ($1,000–4,999) and Intermune ($1–4,999); he was a speaker for Intermune ($1–4,999) and Stallergenes ($1–4,999), and received research support from Intermune ($100,000+). J.E. served on advisory committees of Pfizer (Wyeth) ($1–4,999). K.F. served as a speaker for GlaxoSmithKline ($10,000–49,999) and on advisory committees of Boehringer Ingelheim ($1–9,999), Fibrogen ($1–9,999), and GlaxoSmithKline ($1–9,999); he received research support from Centocor ($50,000–99,999), Immune Works ($50,000–99,999), and Intermune ($100,000+). D.S.K. served on advisory committees of Boehringer Ingelheim ($5,000–24,999). M.K. was patent holder with Daikin Industries of a process for preparing a fluorine-containing polymer and a cross-linked fluororubber diaphragm. F.J.M. reported consulting for Almirall ($1–4,999), American Institute for Research ($1–4,999), Astra Zeneca ($1–4,999), Bayer ($1–4,999), Boehringer Ingelheim ($5,000–24,999), Caden Jennings ($1–4,999), Cardiomema (no payments), Forest ($25,000–49,999), GlaxoSmithKline ($25,000–49,999), HCRC-TC ($1–4,999), Ikarta ($5,000–24,999), Medimmune ($1–4,999), Merck ($5,000–24,999), Merion-TC ($1–4,999), Novartis ($5,000–24,999), Pearl ($5,000–24,999), Pfizer ($1–4,999), Sudler-Hennessey-TC ($1–4,999), and Vertex ($1–4,999); he served as a speaker for Astra Zeneca ($1–4,999), Bayer ($5,000–24,999), Forest ($5,000–24,999), GlaxoSmithKline ($50,000–49,999), and Nycomed/Takeda ($50,000–49,999), and on advisory committees of Actelion ($5,000–24,999), Bayer ($1–4,999), Biogen/Stromedix ($1–4,999), Janssen ($1–4,999), Mpex (no payments), Nycomed/Takeda ($50,000–99,999), Pfizer ($1–4,999), and Vertex ($1–4,999); he received research support from Actelion ($5,000–24,999) and royalties from Informa ($1–4,999). G.R. reported consulting for Actelion ($5,000–24,999), Bayer ($1,000–4,999), Boehringer Ingelheim ($1–4,999), Centocor ($1–4,999), Celgene ($1–4,999), Fibrogen ($1–4,999), GlaxoSmithKline ($1–4,999), GeNo ($1–4,999), Gilead ($1–4,999), Intermune ($1–4,999), Promedior ($1–4,999), Sanofi-Aventis ($1–4,999), Stromedix ($1–4,999), and Takeda ($1–4,999). L.R. reported consulting for Fibrogen ($1–4,999) and Genentech ($1–4,999), and was a speaker for Boehringer Ingelheim ($1–4,999) and Intermune ($5,000–24,999); he served on advisory committees of Boehringer Ingelheim ($1–4,999), Intermune ($1–4,999), GlaxoSmithKline ($1–4,999), Medimmune ($1–4,999), and Sanofi-Aventis ($1–4,999); he received research support from Intermune ($50,000–99,999). J.S. consulted for Genentech ($1–4,999) and received research support from Intermune ($50,000–99,999). D.V. served on advisory committees of Actelion ($1–4,999) and as an expert witness for Sanofi-Aventis (<$1,000). W.D.T., U.C., J.H.R., M.S., A.U.W., D.B., T.V.C., C.R.C., M.D., R.F.D., C.H., Y.I., T.J., J.L., J.M., S.P., and N.S. reported they had no relevant commercial interests.
References
- 1.American Thoracic Society, European Respiratory Society. American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2002;165:277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 2.Travis WD, Hunninghake G, King TE, Jr, Lynch DA, Colby TV, Galvin JR, Brown KK, Chung MP, Cordier J-F, du Bois RM, et al. Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project. Am J Respir Crit Care Med. 2008;177:1338–1347. doi: 10.1164/rccm.200611-1685OC. [DOI] [PubMed] [Google Scholar]
- 3.Aziz ZA, Wells AU, Hansell DM, Bain GA, Copley SJ, Desai SR, Ellis SM, Gleeson FV, Grubnic S, Nicholson AG, et al. HRCT diagnosis of diffuse parenchymal lung disease: inter-observer variation. Thorax. 2004;59:506–511. doi: 10.1136/thx.2003.020396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flaherty KR, King TE, Jr, Raghu G, Lynch JP, III, Colby TV, Travis WD, Gross BH, Kazerooni EA, Toews GB, Long Q, et al. Idiopathic interstitial pneumonia: what is the effect of a multidisciplinary approach to diagnosis? Am J Respir Crit Care Med. 2004;170:904–910. doi: 10.1164/rccm.200402-147OC. [DOI] [PubMed] [Google Scholar]
- 5.Nicholson AG, Addis BJ, Bharucha H, Clelland CA, Corrin B, Gibbs AR, Hasleton PS, Kerr KM, Ibrahim NBN, Stewart S, et al. Inter-observer variation between pathologists in diffuse parenchymal lung disease. Thorax. 2004;59:500–505. doi: 10.1136/thx.2003.011734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomeer M, Demedts M, Behr J, Buhl R, Costabel U, Flower CDR, Verschakelen J, Laurent F, Nicholson AG, Verbeken EK, et al. Idiopathic Pulmonary Fibrosis International Group Exploring N-Acetylcysteine I Annual (IFIGENIA) Study Group. Multidisciplinary interobserver agreement in the diagnosis of idiopathic pulmonary fibrosis. Eur Respir J. 2008;31:585–591. doi: 10.1183/09031936.00063706. [DOI] [PubMed] [Google Scholar]
- 7.Flaherty KR, Andrei A-C, King TE, Jr, Raghu G, Colby TV, Wells A, Bassily N, Brown K, du Bois R, Flint A, et al. Idiopathic interstitial pneumonia: do community and academic physicians agree on diagnosis? Am J Respir Crit Care Med. 2007;175:1054–1060. doi: 10.1164/rccm.200606-833OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, et al. ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selman M.Hypersensitivity pneumonitis: a multifaceted deceiving disorder Clin Chest Med 200425531–547.vi [DOI] [PubMed] [Google Scholar]
- 10.Lynch DA, Newell JD, Logan PM, King TE, Jr, Müller NL. Can CT distinguish hypersensitivity pneumonitis from idiopathic pulmonary fibrosis? AJR Am J Roentgenol. 1995;165:807–811. doi: 10.2214/ajr.165.4.7676971. [DOI] [PubMed] [Google Scholar]
- 11.Silva CI, Churg A, Müller NL. Hypersensitivity pneumonitis: spectrum of high-resolution CT and pathologic findings. AJR Am J Roentgenol. 2007;188:334–344. doi: 10.2214/AJR.05.1826. [DOI] [PubMed] [Google Scholar]
- 12.Silva CIS, Müller NL, Lynch DA, Curran-Everett D, Brown KK, Lee KS, Chung MP, Churg A. Chronic hypersensitivity pneumonitis: differentiation from idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia by using thin-section CT. Radiology. 2008;246:288–297. doi: 10.1148/radiol.2453061881. [DOI] [PubMed] [Google Scholar]
- 13.Akashi T, Takemura T, Ando N, Eishi Y, Kitagawa M, Takizawa T, Koike M, Ohtani Y, Miyazaki Y, Inase N, et al. Histopathologic analysis of sixteen autopsy cases of chronic hypersensitivity pneumonitis and comparison with idiopathic pulmonary fibrosis/usual interstitial pneumonia. Am J Clin Pathol. 2009;131:405–415. doi: 10.1309/AJCPNWX4SLZRP9SW. [DOI] [PubMed] [Google Scholar]
- 14.Churg A, Muller NL, Flint J, Wright JL. Chronic hypersensitivity pneumonitis. Am J Surg Pathol. 2006;30:201–208. doi: 10.1097/01.pas.0000184806.38037.3c. [DOI] [PubMed] [Google Scholar]
- 15.Churg A, Sin DD, Everett D, Brown K, Cool C. Pathologic patterns and survival in chronic hypersensitivity pneumonitis. Am J Surg Pathol. 2009;33:1765–1770. doi: 10.1097/PAS.0b013e3181bb2538. [DOI] [PubMed] [Google Scholar]
- 16.Fenton ME, Cockcroft DW, Wright JL, Churg A. Hypersensitivity pneumonitis as a cause of airway-centered interstitial fibrosis. Ann Allergy Asthma Immunol. 2007;99:465–466. doi: 10.1016/S1081-1206(10)60573-X. [DOI] [PubMed] [Google Scholar]
- 17.Sahin H, Brown KK, Curran-Everett D, Hale V, Cool CD, Vourlekis JS, Lynch DA. Chronic hypersensitivity pneumonitis: CT features comparison with pathologic evidence of fibrosis and survival. Radiology. 2007;244:591–598. doi: 10.1148/radiol.2442060640. [DOI] [PubMed] [Google Scholar]
- 18.Hanak V, Golbin JM, Ryu JH. Causes and presenting features in 85 consecutive patients with hypersensitivity pneumonitis. Mayo Clin Proc. 2007;82:812–816. doi: 10.4065/82.7.812. [DOI] [PubMed] [Google Scholar]
- 19.Felício CH, Parra ER, Capelozzi VL. Idiopathic and collagen vascular disease nonspecific interstitial pneumonia: clinical significance of remodeling process. Lung. 2007;185:39–46. doi: 10.1007/s00408-006-0104-2. [DOI] [PubMed] [Google Scholar]
- 20.Park JH, Kim DS, Park IN, Jang SJ, Kitaichi M, Nicholson AG, Colby TV. Prognosis of fibrotic interstitial pneumonia: idiopathic versus collagen vascular disease-related subtypes. Am J Respir Crit Care Med. 2007;175:705–711. doi: 10.1164/rccm.200607-912OC. [DOI] [PubMed] [Google Scholar]
- 21.Hwang J-H, Misumi S, Sahin H, Brown KK, Newell JD, Lynch DA. Computed tomographic features of idiopathic fibrosing interstitial pneumonia: comparison with pulmonary fibrosis related to collagen vascular disease. J Comput Assist Tomogr. 2009;33:410–415. doi: 10.1097/RCT.0b013e318181d551. [DOI] [PubMed] [Google Scholar]
- 22.Song JW, Do K-H, Kim M-Y, Jang SJ, Colby TV, Kim DS. Pathologic and radiologic differences between idiopathic and collagen vascular disease–related usual interstitial pneumonia. Chest. 2009;136:23–30. doi: 10.1378/chest.08-2572. [DOI] [PubMed] [Google Scholar]
- 23.Corte TJ, Copley SJ, Desai SR, Zappala CJ, Hansell DM, Nicholson AG, Colby TV, Renzoni E, Maher TM, Wells AU. Significance of connective tissue disease features in idiopathic interstitial pneumonia. Eur Respir J. 2012;39:661–668. doi: 10.1183/09031936.00174910. [DOI] [PubMed] [Google Scholar]
- 24.Suda T, Kono M, Nakamura Y, Enomoto N, Kaida Y, Fujisawa T, Imokawa S, Yasuda K, Hashizume H, Yokomura K, et al. Distinct prognosis of idiopathic nonspecific interstitial pneumonia (NSIP) fulfilling criteria for undifferentiated connective tissue disease (UCTD) Respir Med. 2010;104:1527–1534. doi: 10.1016/j.rmed.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 25.Kinder BW, Collard HR, Koth L, Daikh DI, Wolters PJ, Elicker B, Jones KD, King TE., Jr Idiopathic nonspecific interstitial pneumonia: lung manifestation of undifferentiated connective tissue disease? Am J Respir Crit Care Med. 2007;176:691–697. doi: 10.1164/rccm.200702-220OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.García-Sancho C, Buendía-Roldán I, Fernández-Plata MR, Navarro C, Pérez-Padilla R, Vargas MH, Loyd JE, Selman M. Familial pulmonary fibrosis is the strongest risk factor for idiopathic pulmonary fibrosis. Respir Med. 2011;105:1902–1907. doi: 10.1016/j.rmed.2011.08.022. [DOI] [PubMed] [Google Scholar]
- 27.Hodgson U, Laitinen T, Tukiainen P. Nationwide prevalence of sporadic and familial idiopathic pulmonary fibrosis: evidence of founder effect among multiplex families in Finland. Thorax. 2002;57:338–342. doi: 10.1136/thorax.57.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marshall RP, Puddicombe A, Cookson WO, Laurent GJ. Adult familial cryptogenic fibrosing alveolitis in the United Kingdom. Thorax. 2000;55:143–146. doi: 10.1136/thorax.55.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barlo NP, van Moorsel CHM, Ruven HJT, Zanen P, van den Bosch JMM, Grutters JC. Surfactant protein-D predicts survival in patients with idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis. 2009;26:155–161. [PubMed] [Google Scholar]
- 30.Nogee LM, Dunbar AE, III, Wert SE, Askin F, Hamvas A, Whitsett JA. A mutation in the surfactant protein C gene associated with familial interstitial lung disease. N Engl J Med. 2001;344:573–579. doi: 10.1056/NEJM200102223440805. [DOI] [PubMed] [Google Scholar]
- 31.Kirwan M, Dokal I. Dyskeratosis congenita, stem cells and telomeres. Biochim Biophys Acta. 2009;1792:371–379. doi: 10.1016/j.bbadis.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Moorsel CH, van Oosterhout MF, Barlo NP, de Jong PA, van der Vis JJ, Ruven HJ, van Es HW, van den Bosch JM, Grutters JC. Surfactant protein C mutations are the basis of a significant portion of adult familial pulmonary fibrosis in a Dutch cohort. Am J Respir Crit Care Med. 2010;182:1419–1425. doi: 10.1164/rccm.200906-0953OC. [DOI] [PubMed] [Google Scholar]
- 33.Alder JK, Chen JJL, Lancaster L, Danoff S, Su SC, Cogan JD, Vulto I, Xie M, Qi X, Tuder RM, et al. Short telomeres are a risk factor for idiopathic pulmonary fibrosis. Proc Natl Acad Sci USA. 2008;105:13051–13056. doi: 10.1073/pnas.0804280105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cronkhite JT, Xing C, Raghu G, Chin KM, Torres F, Rosenblatt RL, Garcia CK. Telomere shortening in familial and sporadic pulmonary fibrosis. Am J Respir Crit Care Med. 2008;178:729–737. doi: 10.1164/rccm.200804-550OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lawson WE, Crossno PF, Polosukhin VV, Roldan J, Cheng D-S, Lane KB, Blackwell TR, Xu C, Markin C, Ware LB, et al. Endoplasmic reticulum stress in alveolar epithelial cells is prominent in IPF: association with altered surfactant protein processing and herpesvirus infection. Am J Physiol Lung Cell Mol Physiol. 2008;294:L1119–L1126. doi: 10.1152/ajplung.00382.2007. [DOI] [PubMed] [Google Scholar]
- 36.Seibold MA, Wise AL, Speer MC, Steele MP, Brown KK, Loyd JE, Fingerlin TE, Zhang W, Gudmundsson G, Groshong SD, et al. A common MUC5B promoter polymorphism and pulmonary fibrosis. N Engl J Med. 2011;364:1503–1512. doi: 10.1056/NEJMoa1013660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang Y, Noth I, Garcia JG, Kaminski N. A variant in the promoter of MUC5B and idiopathic pulmonary fibrosis. N Engl J Med. 2011;364:1576–1577. doi: 10.1056/NEJMc1013504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lawson WE, Loyd JE, Degryse AL. Genetics in pulmonary fibrosis—familial cases provide clues to the pathogenesis of idiopathic pulmonary fibrosis. Am J Med Sci. 2011;341:439–443. doi: 10.1097/MAJ.0b013e31821a9d7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Monaghan H, Wells AU, Colby TV, du Bois RM, Hansell DM, Nicholson AG. Prognostic implications of histologic patterns in multiple surgical lung biopsies from patients with idiopathic interstitial pneumonias. Chest. 2004;125:522–526. doi: 10.1378/chest.125.2.522. [DOI] [PubMed] [Google Scholar]
- 40.Ryu JH, Colby TV, Hartman TE, Vassallo R. Smoking-related interstitial lung diseases: a concise review. Eur Respir J. 2001;17:122–132. doi: 10.1183/09031936.01.17101220. [DOI] [PubMed] [Google Scholar]
- 41.Aubry MC, Wright JL, Myers JL.The pathology of smoking-related lung diseases Clin Chest Med 20002111–35.vii [DOI] [PubMed] [Google Scholar]
- 42.Vassallo R, Jensen EA, Colby TV, Ryu JH, Douglas WW, Hartman TE, Limper AH. The overlap between respiratory bronchiolitis and desquamative interstitial pneumonia in pulmonary Langerhans cell histiocytosis: high-resolution CT, histologic, and functional correlations. Chest. 2003;124:1199–1205. doi: 10.1378/chest.124.4.1199. [DOI] [PubMed] [Google Scholar]
- 43.Cottin V, Le Pavec J, Prévot G, Mal H, Humbert M, Simonneau G, Cordier JF GERM“O”P. Pulmonary hypertension in patients with combined pulmonary fibrosis and emphysema syndrome. Eur Respir J. 2010;35:105–111. doi: 10.1183/09031936.00038709. [DOI] [PubMed] [Google Scholar]
- 44.Cottin V, Cordier JF. The syndrome of combined pulmonary fibrosis and emphysema. Chest. 2009;136:1–2. doi: 10.1378/chest.09-0538. [DOI] [PubMed] [Google Scholar]
- 45.Cottin V, Nunes H, Brillet PY, Delaval P, Devouassoux G, Tillie-Leblond I, Israel-Biet D, Court-Fortune I, Valeyre D, Cordier JF Groupe d’Etude et de Recherche sur les Maladies Orphelines Pulmonaires (GERM“O”P) Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur Respir J. 2005;26:586–593. doi: 10.1183/09031936.05.00021005. [DOI] [PubMed] [Google Scholar]
- 46.Mejía M, Carrillo G, Rojas-Serrano J, Estrada A, Suárez T, Alonso D, Barrientos E, Gaxiola M, Navarro C, Selman M. Idiopathic pulmonary fibrosis and emphysema: decreased survival associated with severe pulmonary arterial hypertension. Chest. 2009;136:10–15. doi: 10.1378/chest.08-2306. [DOI] [PubMed] [Google Scholar]
- 47.Akira M, Inoue Y, Kitaichi M, Yamamoto S, Arai T, Toyokawa K. Usual interstitial pneumonia and nonspecific interstitial pneumonia with and without concurrent emphysema: thin-section CT findings. Radiology. 2009;251:271–279. doi: 10.1148/radiol.2511080917. [DOI] [PubMed] [Google Scholar]
- 48.Flaherty KR, Travis WD, Colby TV, Toews GB, Kazerooni EA, Gross BH, Jain A, Strawderman RL, Flint A, Lynch JP, et al. Histopathologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med. 2001;164:1722–1727. doi: 10.1164/ajrccm.164.9.2103074. [DOI] [PubMed] [Google Scholar]
- 49.Flaherty KR, Thwaite EL, Kazerooni EA, Gross BH, Toews GB, Colby TV, Travis WD, Mumford JA, Murray S, Flint A, et al. Radiological versus histological diagnosis in UIP and NSIP: survival implications. Thorax. 2003;58:143–148. doi: 10.1136/thorax.58.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sverzellati N, Wells AU, Tomassetti S, Desai SR, Copley SJ, Aziz ZA, Zompatori M, Chilosi M, Nicholson AG, Poletti V, et al. Biopsy-proved idiopathic pulmonary fibrosis: spectrum of nondiagnostic thin-section CT diagnoses. Radiology. 2010;254:957–964. doi: 10.1148/radiol.0990898. [DOI] [PubMed] [Google Scholar]
- 51.Sumikawa H, Johkoh T, Colby TV, Ichikado K, Suga M, Taniguchi H, Kondoh Y, Ogura T, Arakawa H, Fujimoto K, et al. Computed tomography findings in pathological usual interstitial pneumonia: relationship to survival. Am J Respir Crit Care Med. 2008;177:433–439. doi: 10.1164/rccm.200611-1696OC. [DOI] [PubMed] [Google Scholar]
- 52.Silva CI, Müller NL, Hansell DM, Lee KS, Nicholson AG, Wells AU. Nonspecific interstitial pneumonia and idiopathic pulmonary fibrosis: changes in pattern and distribution of disease over time. Radiology. 2008;247:251–259. doi: 10.1148/radiol.2471070369. [DOI] [PubMed] [Google Scholar]
- 53.Lynch DA, Godwin JD, Safrin S, Starko KM, Hormel P, Brown KK, Raghu G, King TE, Jr, Bradford WZ, Schwartz DA, et al. Idiopathic Pulmonary Fibrosis Study Group. High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med. 2005;172:488–493. doi: 10.1164/rccm.200412-1756OC. [DOI] [PubMed] [Google Scholar]
- 54.Kim EY, Lee KS, Chung MP, Kwon OJ, Kim TS, Hwang JH. Nonspecific interstitial pneumonia with fibrosis: serial high-resolution CT findings with functional correlation. AJR Am J Roentgenol. 1999;173:949–953. doi: 10.2214/ajr.173.4.10511155. [DOI] [PubMed] [Google Scholar]
- 55.Hartman TE, Swensen SJ, Hansell DM, Colby TV, Myers JL, Tazelaar HD, Nicholson AG, Wells AU, Ryu JH, Midthun DE, et al. Nonspecific interstitial pneumonia: variable appearance at high-resolution chest CT Radiology 2000217701–705.Published erratum appears in Radiology 218:606 [DOI] [PubMed] [Google Scholar]
- 56.Park JS, Lee KS, Kim JS, Park CS, Suh YL, Choi DL, Kim KJ. Nonspecific interstitial pneumonia with fibrosis: radiographic and CT findings in seven patients. Radiology. 1995;195:645–648. doi: 10.1148/radiology.195.3.7753988. [DOI] [PubMed] [Google Scholar]
- 57.Cottin V, Donsbeck AV, Revel D, Loire R, Cordier JF. Nonspecific interstitial pneumonia: individualization of a clinicopathologic entity in a series of 12 patients. Am J Respir Crit Care Med. 1998;158:1286–1293. doi: 10.1164/ajrccm.158.4.9802119. [DOI] [PubMed] [Google Scholar]
- 58.Nagai S, Kitaichi M, Itoh H, Nishimura K, Izumi T, Colby TV. Idiopathic nonspecific interstitial pneumonia/fibrosis: comparison with idiopathic pulmonary fibrosis and BOOP. Eur Respir J. 1998;12:1010–1019. doi: 10.1183/09031936.98.12051010. [DOI] [PubMed] [Google Scholar]
- 59.Johkoh T, Müller NL, Colby TV, Ichikado K, Taniguchi H, Kondoh Y, Fujimoto K, Kinoshita M, Arakawa H, Yamada H, et al. Nonspecific interstitial pneumonia: correlation between thin-section CT findings and pathologic subgroups in 55 patients. Radiology. 2002;225:199–204. doi: 10.1148/radiol.2251011555. [DOI] [PubMed] [Google Scholar]
- 60.Johkoh T, Müller NL, Cartier Y, Kavanagh PV, Hartman TE, Akira M, Ichikado K, Ando M, Nakamura H. Idiopathic interstitial pneumonias: diagnostic accuracy of thin-section CT in 129 patients. Radiology. 1999;211:555–560. doi: 10.1148/radiology.211.2.r99ma01555. [DOI] [PubMed] [Google Scholar]
- 61.Nishiyama O, Kondoh Y, Taniguchi H, Yamaki K, Suzuki R, Yokoi T, Takagi K. Serial high resolution CT findings in nonspecific interstitial pneumonia/fibrosis. J Comput Assist Tomogr. 2000;24:41–46. doi: 10.1097/00004728-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 62.MacDonald SL, Rubens MB, Hansell DM, Copley SJ, Desai SR, du Bois RM, Nicholson AG, Colby TV, Wells AU. Nonspecific interstitial pneumonia and usual interstitial pneumonia: comparative appearances at and diagnostic accuracy of thin-section CT. Radiology. 2001;221:600–605. doi: 10.1148/radiol.2213010158. [DOI] [PubMed] [Google Scholar]
- 63.Akira M, Inoue Y, Arai T, Okuma T, Kawata Y. Long-term follow-up high-resolution CT findings in non-specific interstitial pneumonia. Thorax. 2011;66:61–65. doi: 10.1136/thx.2010.140574. [DOI] [PubMed] [Google Scholar]
- 64.Katzenstein AL, Fiorelli RF. Nonspecific interstitial pneumonia/fibrosis: histologic features and clinical significance. Am J Surg Pathol. 1994;18:136–147. [PubMed] [Google Scholar]
- 65.Travis WD, Matsui K, Moss J, Ferrans VJ. Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns: survival comparison with usual interstitial pneumonia and desquamative interstitial pneumonia. Am J Surg Pathol. 2000;24:19–33. doi: 10.1097/00000478-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 66.Tsubamoto M, Müller NL, Johkoh T, Ichikado K, Taniguchi H, Kondoh Y, Fujimoto K, Arakawa H, Koyama M, Kozuka T, et al. Pathologic subgroups of nonspecific interstitial pneumonia: differential diagnosis from other idiopathic interstitial pneumonias on high-resolution computed tomography. J Comput Assist Tomogr. 2005;29:793–800. doi: 10.1097/01.rct.0000182853.90520.84. [DOI] [PubMed] [Google Scholar]
- 67.Park IN, Jegal Y, Kim DS, Do KH, Yoo B, Shim TS, Lim CM, Lee SD, Koh Y, Kim WS, et al. Clinical course and lung function change of idiopathic nonspecific interstitial pneumonia. Eur Respir J. 2009;33:68–76. doi: 10.1183/09031936.00158507. [DOI] [PubMed] [Google Scholar]
- 68.Hidalgo A, Franquet T, Giménez A, Bordes R, Pineda R, Madrid M. Smoking-related interstitial lung diseases: radiologic–pathologic correlation. Eur Radiol. 2006;16:2463–2470. doi: 10.1007/s00330-006-0340-0. [DOI] [PubMed] [Google Scholar]
- 69.Craig PJ, Wells AU, Doffman S, Rassl D, Colby TV, Hansell DM, Du Bois RM, Nicholson AG. Desquamative interstitial pneumonia, respiratory bronchiolitis and their relationship to smoking. Histopathology. 2004;45:275–282. doi: 10.1111/j.1365-2559.2004.01921.x. [DOI] [PubMed] [Google Scholar]
- 70.Fraig M, Shreesha U, Savici D, Katzenstein AL. Respiratory bronchiolitis: a clinicopathologic study in current smokers, ex-smokers, and never-smokers. Am J Surg Pathol. 2002;26:647–653. doi: 10.1097/00000478-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 71.Vassallo R, Ryu JH. Tobacco smoke–related diffuse lung diseases. Semin Respir Crit Care Med. 2008;29:643–650. doi: 10.1055/s-0028-1101274. [DOI] [PubMed] [Google Scholar]
- 72.Portnoy J, Veraldi KL, Schwarz MI, Cool CD, Curran-Everett D, Cherniack RM, King TE, Jr, Brown KK. Respiratory bronchiolitis-interstitial lung disease: long-term outcome. Chest. 2007;131:664–671. doi: 10.1378/chest.06-1885. [DOI] [PubMed] [Google Scholar]
- 73.Doan ML, Guillerman RP, Dishop MK, Nogee LM, Langston C, Mallory GB, Sockrider MM, Fan LL. Clinical, radiological and pathological features of ABCA3 mutations in children. Thorax. 2008;63:366–373. doi: 10.1136/thx.2007.083766. [DOI] [PubMed] [Google Scholar]
- 74.Bullard JE, Wert SE, Whitsett JA, Dean M, Nogee LM. ABCA3 mutations associated with pediatric interstitial lung disease. Am J Respir Crit Care Med. 2005;172:1026–1031. doi: 10.1164/rccm.200503-504OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kawabata Y, Hoshi E, Murai K, Ikeya T, Takahashi N, Saitou Y, Kurashima K, Ubukata M, Takayanagi N, Sugita H, et al. Smoking-related changes in the background lung of specimens resected for lung cancer: a semiquantitative study with correlation to postoperative course. Histopathology. 2008;53:707–714. doi: 10.1111/j.1365-2559.2008.03183.x. [DOI] [PubMed] [Google Scholar]
- 76.Katzenstein AL, Mukhopadhyay S, Zanardi C, Dexter E. Clinically occult interstitial fibrosis in smokers: classification and significance of a surprisingly common finding in lobectomy specimens. Hum Pathol. 2010;41:316–325. doi: 10.1016/j.humpath.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 77.Snider GL, Kleinerman J, Thurlbeck WM, Bengali ZH. The definition of emphysema: report of a National Heart, Lung, and Blood Institute, Division of Lung Diseases workshop. Am Rev Respir Dis. 1985;132:182–185. doi: 10.1164/arrd.1985.132.1.182. [DOI] [PubMed] [Google Scholar]
- 78.King TE, Jr, Mortenson RL. Cryptogenic organizing pneumonitis: the North American experience. Chest. 1992;102(1, Suppl):8S–13S. [PubMed] [Google Scholar]
- 79.Lee JW, Lee KS, Lee HY, Chung MP, Yi CA, Kim TS, Chung MJ. Cryptogenic organizing pneumonia: serial high-resolution CT findings in 22 patients. AJR Am J Roentgenol. 2010;195:916–922. doi: 10.2214/AJR.09.3940. [DOI] [PubMed] [Google Scholar]
- 80.Sen T, Udwadia ZF. Cryptogenic organizing pneumonia: clinical profile in a series of 34 admitted patients in a hospital in India. J Assoc Physicians India. 2008;56:229–232. [PubMed] [Google Scholar]
- 81.Oymak FS, Demirbaş HM, Mavili E, Akgun H, Gulmez I, Demir R, Ozesmi M. Bronchiolitis obliterans organizing pneumonia: clinical and roentgenological features in 26 cases. Respiration. 2005;72:254–262. doi: 10.1159/000085366. [DOI] [PubMed] [Google Scholar]
- 82.Lee JS, Lynch DA, Sharma S, Brown KK, Müller NL. Organizing pneumonia: prognostic implication of high-resolution computed tomography features. J Comput Assist Tomogr. 2003;27:260–265. doi: 10.1097/00004728-200303000-00027. [DOI] [PubMed] [Google Scholar]
- 83.Lee KS, Kullnig P, Hartman TE, Müller NL. Cryptogenic organizing pneumonia: CT findings in 43 patients. AJR Am J Roentgenol. 1994;162:543–546. doi: 10.2214/ajr.162.3.8109493. [DOI] [PubMed] [Google Scholar]
- 84.Müller NL, Staples CA, Miller RR. Bronchiolitis obliterans organizing pneumonia: CT features in 14 patients. AJR Am J Roentgenol. 1990;154:983–987. doi: 10.2214/ajr.154.5.2108572. [DOI] [PubMed] [Google Scholar]
- 85.Ujita M, Renzoni EA, Veeraraghavan S, Wells AU, Hansell DM. Organizing pneumonia: perilobular pattern at thin-section CT. Radiology. 2004;232:757–761. doi: 10.1148/radiol.2323031059. [DOI] [PubMed] [Google Scholar]
- 86.Kim SJ, Lee KS, Ryu YH, Yoon YC, Choe KO, Kim TS, Sung KJ. Reversed halo sign on high-resolution CT of cryptogenic organizing pneumonia: diagnostic implications. AJR Am J Roentgenol. 2003;180:1251–1254. doi: 10.2214/ajr.180.5.1801251. [DOI] [PubMed] [Google Scholar]
- 87.Epler GR, Colby TV, McLoud TC, Carrington CB, Gaensler EA. Bronchiolitis obliterans organizing pneumonia. N Engl J Med. 1985;312:152–158. doi: 10.1056/NEJM198501173120304. [DOI] [PubMed] [Google Scholar]
- 88.Lohr RH, Boland BJ, Douglas WW, Dockrell DH, Colby TV, Swensen SJ, Wollan PC, Silverstein MD. Organizing pneumonia: features and prognosis of cryptogenic, secondary, and focal variants. Arch Intern Med. 1997;157:1323–1329. doi: 10.1001/archinte.157.12.1323. [DOI] [PubMed] [Google Scholar]
- 89.Lazor R, Vandevenne A, Pelletier A, Leclerc P, Court-Fortune I, Cordier JF Groupe d’Etudes et de Recherche sur les Maladies “Orphelines” Pulmonaires (GERM“O”P) Cryptogenic organizing pneumonia: characteristics of relapses in a series of 48 patients. Am J Respir Crit Care Med. 2000;162:571–577. doi: 10.1164/ajrccm.162.2.9909015. [DOI] [PubMed] [Google Scholar]
- 90.Fischer A, Swigris JJ, du Bois RM, Lynch DA, Downey GP, Cosgrove GP, Frankel SK, Fernandez-Perez ER, Gillis JZ, Brown KK. Anti-synthetase syndrome in ANA and anti–Jo-1 negative patients presenting with idiopathic interstitial pneumonia. Respir Med. 2009;103:1719–1724. doi: 10.1016/j.rmed.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bouros D, Nicholson AC, Polychronopoulos V, du Bois RM. Acute interstitial pneumonia. Eur Respir J. 2000;15:412–418. doi: 10.1034/j.1399-3003.2000.15b31.x. [DOI] [PubMed] [Google Scholar]
- 92.Vourlekis JS, Brown KK, Cool CD, Young DA, Cherniack RM, King TE, Schwarz MI. Acute interstitial pneumonitis: case series and review of the literature. Medicine (Baltimore) 2000;79:369–378. doi: 10.1097/00005792-200011000-00003. [DOI] [PubMed] [Google Scholar]
- 93.Ichikado K, Suga M, Müller NL, Taniguchi H, Kondoh Y, Akira M, Johkoh T, Mihara N, Nakamura H, Takahashi M, et al. Acute interstitial pneumonia: comparison of high-resolution computed tomography findings between survivors and nonsurvivors. Am J Respir Crit Care Med. 2002;165:1551–1556. doi: 10.1164/rccm.2106157. [DOI] [PubMed] [Google Scholar]
- 94.Primack SL, Hartman TE, Ikezoe J, Akira M, Sakatani M, Müller NL. Acute interstitial pneumonia: radiographic and CT findings in nine patients. Radiology. 1993;188:817–820. doi: 10.1148/radiology.188.3.8351354. [DOI] [PubMed] [Google Scholar]
- 95.Johkoh T, Müller NL, Taniguchi H, Kondoh Y, Akira M, Ichikado K, Ando M, Honda O, Tomiyama N, Nakamura H. Acute interstitial pneumonia: thin-section CT findings in 36 patients. Radiology. 1999;211:859–863. doi: 10.1148/radiology.211.3.r99jn04859. [DOI] [PubMed] [Google Scholar]
- 96.Desai SR, Wells AU, Rubens MB, Evans TW, Hansell DM. Acute respiratory distress syndrome: CT abnormalities at long-term follow-up. Radiology. 1999;210:29–35. doi: 10.1148/radiology.210.1.r99ja2629. [DOI] [PubMed] [Google Scholar]
- 97.Ichikado K, Suga M, Muranaka H, Gushima Y, Miyakawa H, Tsubamoto M, Johkoh T, Hirata N, Yoshinaga T, Kinoshita Y, et al. Prediction of prognosis for acute respiratory distress syndrome with thin-section CT: validation in 44 cases. Radiology. 2006;238:321–329. doi: 10.1148/radiol.2373041515. [DOI] [PubMed] [Google Scholar]
- 98.Araya J, Kawabata Y, Jinho P, Uchiyama T, Ogata H, Sugita Y. Clinically occult subpleural fibrosis and acute interstitial pneumonia a precursor to idiopathic pulmonary fibrosis? Respirology. 2008;13:408–412. doi: 10.1111/j.1440-1843.2008.01277.x. [DOI] [PubMed] [Google Scholar]
- 99.Rice AJ, Wells AU, Bouros D, du Bois RM, Hansell DM, Polychronopoulos V, Vassilakis D, Kerr JR, Evans TW, Nicholson AG. Terminal diffuse alveolar damage in relation to interstitial pneumonias: an autopsy study. Am J Clin Pathol. 2003;119:709–714. doi: 10.1309/UVAR-MDY8-FE9F-JDKU. [DOI] [PubMed] [Google Scholar]
- 100.Song JW, Hong SB, Lim CM, Koh Y, Kim DS. Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur Respir J. 2011;37:356–363. doi: 10.1183/09031936.00159709. [DOI] [PubMed] [Google Scholar]
- 101.Agarwal R, Jindal SK. Acute exacerbation of idiopathic pulmonary fibrosis: a systematic review. Eur J Intern Med. 2008;19:227–235. doi: 10.1016/j.ejim.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 102.Silva CIS, Müller NL, Fujimoto K, Kato S, Ichikado K, Taniguchi H, Kondoh Y, Johkoh T, Churg A. Acute exacerbation of chronic interstitial pneumonia: high-resolution computed tomography and pathologic findings. J Thorac Imaging. 2007;22:221–229. doi: 10.1097/01.rti.0000213588.52343.13. [DOI] [PubMed] [Google Scholar]
- 103.Churg A, Müller NL, Silva CIS, Wright JL. Acute exacerbation (acute lung injury of unknown cause) in UIP and other forms of fibrotic interstitial pneumonias. Am J Surg Pathol. 2007;31:277–284. doi: 10.1097/01.pas.0000213341.70852.9d. [DOI] [PubMed] [Google Scholar]
- 104.Suda T, Kaida Y, Nakamura Y, Enomoto N, Fujisawa T, Imokawa S, Hashizume H, Naito T, Hashimoto D, Takehara Y, et al. Acute exacerbation of interstitial pneumonia associated with collagen vascular diseases. Respir Med. 2009;103:846–853. doi: 10.1016/j.rmed.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Park IN, Kim DS, Shim TS, Lim C-M, Lee SD, Koh Y, Kim WS, Kim WD, Jang SJ, Colby TV. Acute exacerbation of interstitial pneumonia other than idiopathic pulmonary fibrosis. Chest. 2007;132:214–220. doi: 10.1378/chest.07-0323. [DOI] [PubMed] [Google Scholar]
- 106.Miyazaki Y, Tateishi T, Akashi T, Ohtani Y, Inase N, Yoshizawa Y. Clinical predictors and histologic appearance of acute exacerbations in chronic hypersensitivity pneumonitis. Chest. 2008;134:1265–1270. doi: 10.1378/chest.08-0866. [DOI] [PubMed] [Google Scholar]
- 107.Collard HR, Moore BB, Flaherty KR, Brown KK, Kaner RJ, King TE, Jr, Lasky JA, Loyd JE, Noth I, Olman MA, et al. Idiopathic Pulmonary Fibrosis Clinical Research Network Investigators. Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007;176:636–643. doi: 10.1164/rccm.200703-463PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Akira M, Kozuka T, Yamamoto S, Sakatani M. Computed tomography findings in acute exacerbation of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2008;178:372–378. doi: 10.1164/rccm.200709-1365OC. [DOI] [PubMed] [Google Scholar]
- 109.Akira M, Hamada H, Sakatani M, Kobayashi C, Nishioka M, Yamamoto S. CT findings during phase of accelerated deterioration in patients with idiopathic pulmonary fibrosis. AJR Am J Roentgenol. 1997;168:79–83. doi: 10.2214/ajr.168.1.8976924. [DOI] [PubMed] [Google Scholar]
- 110.Fujimoto K, Taniguchi H, Johkoh T, Kondoh Y, Ichikado K, Sumikawa H, Ogura T, Kataoka K, Endo T, Kawaguchi A, et al. Acute exacerbation of idiopathic pulmonary fibrosis: high-resolution CT scores predict mortality. Eur Radiol. 2012;22:83–92. doi: 10.1007/s00330-011-2211-6. [DOI] [PubMed] [Google Scholar]
- 111.Cha SI, Fessler MB, Cool CD, Schwarz MI, Brown KK. Lymphoid interstitial pneumonia: clinical features, associations and prognosis. Eur Respir J. 2006;28:364–369. doi: 10.1183/09031936.06.00076705. [DOI] [PubMed] [Google Scholar]
- 112.Johkoh T, Müller NL, Pickford HA, Hartman TE, Ichikado K, Akira M, Honda O, Nakamura H. Lymphocytic interstitial pneumonia: thin-section CT findings in 22 patients. Radiology. 1999;212:567–572. doi: 10.1148/radiology.212.2.r99au05567. [DOI] [PubMed] [Google Scholar]
- 113.Reddy TL, Tominaga M, Hansell DM, von der Thusen J, Jr, Rassl D, Parfrey H, Guy S, Twentyman O, Rice A, Maher TM, et al. Pleuroparenchymal fibroelastosis: a spectrum of histopathological and imaging phenotypes. Eur Respir J. 2012;40:377–385. doi: 10.1183/09031936.00165111. [DOI] [PubMed] [Google Scholar]
- 114.Becker CD, Gil J, Padilla ML. Idiopathic pleuroparenchymal fibroelastosis: an unrecognized or misdiagnosed entity? Mod Pathol. 2008;21:784–787. doi: 10.1038/modpathol.2008.56. [DOI] [PubMed] [Google Scholar]
- 115.Frankel SK, Cool CD, Lynch DA, Brown KK. Idiopathic pleuroparenchymal fibroelastosis: description of a novel clinicopathologic entity. Chest. 2004;126:2007–2013. doi: 10.1378/chest.126.6.2007. [DOI] [PubMed] [Google Scholar]
- 116.von der Thüsen JH, Hansell DM, Tominaga M, Veys PA, Ashworth MT, Owens CM, Nicholson AG. Pleuroparenchymal fibroelastosis in patients with pulmonary disease secondary to bone marrow transplantation. Mod Pathol. 2011;24:1633–1639. doi: 10.1038/modpathol.2011.114. [DOI] [PubMed] [Google Scholar]
- 117.Amitani R, Niimi A, Kuze F. Idiopathic pulmonary upper lobe fibrosis (IPUF) [in Japanese] Kokyu. 1992;11:693–699. [Google Scholar]
- 118.Watanabe K, Nagata N, Kitasato Y, Wakamatsu K, Nabeshima K, Harada T, Hirota T, Shiraishi M, Fujita M. Rapid decrease in forced vital capacity in patients with idiopathic pulmonary upper lobe fibrosis. Respir Investig. 2012;50:88–97. doi: 10.1016/j.resinv.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 119.Beasley MB, Franks TJ, Galvin JR, Gochuico B, Travis WD. Acute fibrinous and organizing pneumonia: a histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med. 2002;126:1064–1070. doi: 10.5858/2002-126-1064-AFAOP. [DOI] [PubMed] [Google Scholar]
- 120.Balduin R, Giacometti C, Saccarola L, Marulli G, Rea F, Bartoli M, Agostini C, Calabrese F. Acute fibrinous and organizing pneumonia in a patient with collagen vascular disease “stigma.”. Sarcoidosis Vasc Diffuse Lung Dis. 2007;24:78–80. [PubMed] [Google Scholar]
- 121.Hariri LP, Mino-Kenudson M, Shea B, Digumarthy S, Onozato M, Yagi Y, Fraire AE, Matsubara O, Mark EJ. Distinct histopathology of acute onset or abrupt exacerbation of hypersensitivity pneumonitis. Hum Pathol. 2012;43:660–668. doi: 10.1016/j.humpath.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 122.Yokogawa N, Alcid DV. Acute fibrinous and organizing pneumonia as a rare presentation of abacavir hypersensitivity reaction. AIDS. 2007;21:2116–2117. doi: 10.1097/QAD.0b013e3282f08c5a. [DOI] [PubMed] [Google Scholar]
- 123.Churg A, Myers J, Suarez T, Gaxiola M, Estrada A, Mejia M, Selman M. Airway-centered interstitial fibrosis: a distinct form of aggressive diffuse lung disease. Am J Surg Pathol. 2004;28:62–68. doi: 10.1097/00000478-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 124.Fukuoka J, Franks TJ, Colby TV, Flaherty KR, Galvin JR, Hayden D, Gochuico BR, Kazerooni EA, Martinez F, Travis WD. Peribronchiolar metaplasia: a common histologic lesion in diffuse lung disease and a rare cause of interstitial lung disease: clinicopathologic features of 15 cases. Am J Surg Pathol. 2005;29:948–954. doi: 10.1097/01.pas.0000168177.71405.ac. [DOI] [PubMed] [Google Scholar]
- 125.Yousem SA, Dacic S. Idiopathic bronchiolocentric interstitial pneumonia. Mod Pathol. 2002;15:1148–1153. doi: 10.1097/01.MP.0000037309.04985.B4. [DOI] [PubMed] [Google Scholar]
- 126.Mark EJ, Ruangchira Urai R. Bronchiolitis interstitial pneumonitis: a pathologic study of 31 lung biopsies with features intermediate between bronchiolitis obliterans organizing pneumonia and usual interstitial pneumonitis, with clinical correlation. Ann Diagn Pathol. 2008;12:171–180. doi: 10.1016/j.anndiagpath.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 127.Ryerson CJ, Urbania TH, Richeldi L, Mooney JJ, Lee JS, Jones KD, Elicker BM, Koth LL, King TE, Jr, Wolters PJ, et al. Prevalence and prognosis of unclassifiable interstitial lung disease. Eur Respir J. 2013;42:750–757. doi: 10.1183/09031936.00131912. [DOI] [PubMed] [Google Scholar]
- 128.Kinder BW, Brown KK, McCormack FX, Ix JH, Kervitsky A, Schwarz MI, King TE., Jr Serum surfactant protein-A is a strong predictor of early mortality in idiopathic pulmonary fibrosis. Chest. 2009;135:1557–1563. doi: 10.1378/chest.08-2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Satoh H, Kurishima K, Ishikawa H, Ohtsuka M. Increased levels of KL-6 and subsequent mortality in patients with interstitial lung diseases. J Intern Med. 2006;260:429–434. doi: 10.1111/j.1365-2796.2006.01704.x. [DOI] [PubMed] [Google Scholar]
- 130.Prasse A, Probst C, Bargagli E, Zissel G, Toews GB, Flaherty KR, Olschewski M, Rottoli P, Müller-Quernheim J. Serum CC-chemokine ligand 18 concentration predicts outcome in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2009;179:717–723. doi: 10.1164/rccm.200808-1201OC. [DOI] [PubMed] [Google Scholar]
- 131.Prasse A, Pechkovsky DV, Toews GB, Schäfer M, Eggeling S, Ludwig C, Germann M, Kollert F, Zissel G, Müller-Quernheim J. CCL18 as an indicator of pulmonary fibrotic activity in idiopathic interstitial pneumonias and systemic sclerosis. Arthritis Rheum. 2007;56:1685–1693. doi: 10.1002/art.22559. [DOI] [PubMed] [Google Scholar]
- 132.Ishii H, Mukae H, Kadota J, Kaida H, Nagata T, Abe K, Matsukura S, Kohno S. High serum concentrations of surfactant protein A in usual interstitial pneumonia compared with non-specific interstitial pneumonia. Thorax. 2003;58:52–57. doi: 10.1136/thorax.58.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Ohnishi H, Yokoyama A, Kondo K, Hamada H, Abe M, Nishimura K, Hiwada K, Kohno N. Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. Am J Respir Crit Care Med. 2002;165:378–381. doi: 10.1164/ajrccm.165.3.2107134. [DOI] [PubMed] [Google Scholar]
- 134.Casoni GL, Ulivi P, Mercatali L, Chilosi M, Tomassetti S, Romagnoli M, Ravaglia C, Gurioli C, Gurioli C, Zoli W, et al. Increased levels of free circulating DNA in patients with idiopathic pulmonary fibrosis. Int J Biol Markers. 2010;25:229–235. [PubMed] [Google Scholar]
- 135.Pignatti P, Brunetti G, Moretto D, Yacoub M-R, Fiori M, Balbi B, Balestrino A, Cervio G, Nava S, Moscato G. Role of the chemokine receptors CXCR3 and CCR4 in human pulmonary fibrosis. Am J Respir Crit Care Med. 2006;173:310–317. doi: 10.1164/rccm.200502-244OC. [DOI] [PubMed] [Google Scholar]
- 136.Ishii H, Mukae H, Kadota J, Fujii T, Abe K, Ashitani J, Kohno S. Increased levels of interleukin-18 in bronchoalveolar lavage fluid of patients with idiopathic nonspecific interstitial pneumonia. Respiration. 2005;72:39–45. doi: 10.1159/000083399. [DOI] [PubMed] [Google Scholar]
- 137.Choi ES, Pierce EM, Jakubzick C, Carpenter KJ, Kunkel SL, Evanoff H, Martinez FJ, Flaherty KR, Moore BB, Toews GB, et al. Focal interstitial CC chemokine receptor 7 (CCR7) expression in idiopathic interstitial pneumonia. J Clin Pathol. 2006;59:28–39. doi: 10.1136/jcp.2005.026872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Choi ES, Jakubzick C, Carpenter KJ, Kunkel SL, Evanoff H, Martinez FJ, Flaherty KR, Toews GB, Colby TV, Kazerooni EA, et al. Enhanced monocyte chemoattractant protein-3/CC chemokine ligand-7 in usual interstitial pneumonia. Am J Respir Crit Care Med. 2004;170:508–515. doi: 10.1164/rccm.200401-002OC. [DOI] [PubMed] [Google Scholar]
- 139.Yang IV, Burch LH, Steele MP, Savov JD, Hollingsworth JW, McElvania-Tekippe E, Berman KG, Speer MC, Sporn TA, Brown KK, et al. Gene expression profiling of familial and sporadic interstitial pneumonia. Am J Respir Crit Care Med. 2007;175:45–54. doi: 10.1164/rccm.200601-062OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lawson WE, Grant SW, Ambrosini V, Womble KE, Dawson EP, Lane KB, Markin C, Renzoni E, Lympany P, Thomas AQ, et al. Genetic mutations in surfactant protein C are a rare cause of sporadic cases of IPF. Thorax. 2004;59:977–980. doi: 10.1136/thx.2004.026336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kim KK, Flaherty KR, Long Q, Hattori N, Sisson TH, Colby TV, Travis WD, Martinez FJ, Murray S, Simon RH. A plasminogen activator inhibitor-1 promoter polymorphism and idiopathic interstitial pneumonia. Mol Med. 2003;9:52–56. [PMC free article] [PubMed] [Google Scholar]
- 142.Markart P, Ruppert C, Wygrecka M, Schmidt R, Korfei M, Harbach H, Theruvath I, Pison U, Seeger W, Guenther A, et al. Surfactant protein C mutations in sporadic forms of idiopathic interstitial pneumonias. Eur Respir J. 2007;29:134–137. doi: 10.1183/09031936.00034406. [DOI] [PubMed] [Google Scholar]
- 143.Zorzetto M, Ferrarotti I, Campo I, Trisolini R, Poletti V, Scabini R, Ceruti M, Mazzola P, Crippa E, Ottaviani S, et al. NOD2/CARD15 gene polymorphisms in idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis. 2005;22:180–185. [PubMed] [Google Scholar]
- 144.Hutyrová B, Pantelidis P, Drábek J, Zůrková M, Kolek V, Lenhart K, Welsh KI, Du Bois RM, Petrek M. Interleukin-1 gene cluster polymorphisms in sarcoidosis and idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2002;165:148–151. doi: 10.1164/ajrccm.165.2.2106004. [DOI] [PubMed] [Google Scholar]
- 145.Renzoni E, Lympany P, Sestini P, Pantelidis P, Wells A, Black C, Welsh K, Bunn C, Knight C, Foley P, et al. Distribution of novel polymorphisms of the interleukin-8 and CXC receptor 1 and 2 genes in systemic sclerosis and cryptogenic fibrosing alveolitis. Arthritis Rheum. 2000;43:1633–1640. doi: 10.1002/1529-0131(200007)43:7<1633::AID-ANR29>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 146.Zorzetto M, Ferrarotti I, Trisolini R, Lazzari Agli L, Scabini R, Novo M, De Silvestri A, Patelli M, Martinetti M, Cuccia M, et al. Complement receptor 1 gene polymorphisms are associated with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2003;168:330–334. doi: 10.1164/rccm.200302-221OC. [DOI] [PubMed] [Google Scholar]
- 147.Hodgson U, Tukiainen P, Laitinen T. The polymorphism C5507G of complement receptor 1 does not explain idiopathic pulmonary fibrosis among the Finns. Respir Med. 2005;99:265–267. doi: 10.1016/j.rmed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 148.Kubistova Z, Mrazek F, Lympany PA, Lagan AL, Arakelyan A, Kriegova E, Welsh KI, Kolek V, Zatloukal J, Hutyrova B, et al. The CR1 C5507G polymorphism is not involved in susceptibility to idiopathic pulmonary fibrosis in two European populations. Tissue Antigens. 2008;72:483–486. doi: 10.1111/j.1399-0039.2008.01133.x. [DOI] [PubMed] [Google Scholar]
- 149.Mushiroda T, Wattanapokayakit S, Takahashi A, Nukiwa T, Kudoh S, Ogura T, Taniguchi H, Kubo M, Kamatani N, Nakamura Y Pirfenidone Clinical Study Group. A genome-wide association study identifies an association of a common variant in TERT with susceptibility to idiopathic pulmonary fibrosis. J Med Genet. 2008;45:654–656. doi: 10.1136/jmg.2008.057356. [DOI] [PubMed] [Google Scholar]
- 150.Selman M, Lin H-M, Montaño M, Jenkins AL, Estrada A, Lin Z, Wang G, DiAngelo SL, Guo X, Umstead TM, et al. Surfactant protein A and B genetic variants predispose to idiopathic pulmonary fibrosis. Hum Genet. 2003;113:542–550. doi: 10.1007/s00439-003-1015-4. [DOI] [PubMed] [Google Scholar]
- 151.Falfán-Valencia R, Camarena A, Juárez A, Becerril C, Montaño M, Cisneros J, Mendoza F, Granados J, Pardo A, Selman M. Major histocompatibility complex and alveolar epithelial apoptosis in idiopathic pulmonary fibrosis. Hum Genet. 2005;118:235–244. doi: 10.1007/s00439-005-0035-7. [DOI] [PubMed] [Google Scholar]
- 152.Checa M, Ruiz V, Montaño M, Velázquez-Cruz R, Selman M, Pardo A. MMP-1 polymorphisms and the risk of idiopathic pulmonary fibrosis. Hum Genet. 2008;124:465–472. doi: 10.1007/s00439-008-0571-z. [DOI] [PubMed] [Google Scholar]
- 153.Matsushima H, Takayanagi N, Sakamoto T, Kawata I, Motegi M, Ubukata M, Yanagisawa T, Sugita Y, Kanazawa M, Kawabata Y. Pathologic findings both before and after steroid therapy in a case of desquamative interstitial pneumonia [article in Japanese] Nihon Kokyuki Gakkai Zasshi. 2001;39:609–614. [PubMed] [Google Scholar]
- 154.Latsi PI, du Bois RM, Nicholson AG, Colby TV, Bisirtzoglou D, Nikolakopoulou A, Veeraraghavan S, Hansell DM, Wells AU. Fibrotic idiopathic interstitial pneumonia: the prognostic value of longitudinal functional trends. Am J Respir Crit Care Med. 2003;168:531–537. doi: 10.1164/rccm.200210-1245OC. [DOI] [PubMed] [Google Scholar]
- 155.Takahashi H, Fujishima T, Koba H, Murakami S, Kurokawa K, Shibuya Y, Shiratori M, Kuroki Y, Abe S. Serum surfactant proteins A and D as prognostic factors in idiopathic pulmonary fibrosis and their relationship to disease extent. Am J Respir Crit Care Med. 2000;162:1109–1114. doi: 10.1164/ajrccm.162.3.9910080. [DOI] [PubMed] [Google Scholar]
- 156.Greene KE, King TE, Jr, Kuroki Y, Bucher-Bartelson B, Hunninghake GW, Newman LS, Nagae H, Mason RJ. Serum surfactant proteins-A and -D as biomarkers in idiopathic pulmonary fibrosis. Eur Respir J. 2002;19:439–446. doi: 10.1183/09031936.02.00081102. [DOI] [PubMed] [Google Scholar]
- 157.Yokoyama A, Kondo K, Nakajima M, Matsushima T, Takahashi T, Nishimura M, Bando M, Sugiyama Y, Totani Y, Ishizaki T, et al. Prognostic value of circulating KL-6 in idiopathic pulmonary fibrosis. Respirology. 2006;11:164–168. doi: 10.1111/j.1440-1843.2006.00834.x. [DOI] [PubMed] [Google Scholar]
- 158.Takahashi H, Shiratori M, Kanai A, Chiba H, Kuroki Y, Abe S. Monitoring markers of disease activity for interstitial lung diseases with serum surfactant proteins A and D. Respirology. 2006;11:S51–S54. doi: 10.1111/j.1440-1843.2006.00809.x. [DOI] [PubMed] [Google Scholar]
- 159.Daniil ZD, Papageorgiou E, Koutsokera A, Kostikas K, Kiropoulos T, Papaioannou AI, Gourgoulianis KI. Serum levels of oxidative stress as a marker of disease severity in idiopathic pulmonary fibrosis. Pulm Pharmacol Ther. 2008;21:26–31. doi: 10.1016/j.pupt.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 160.Rosas IO, Richards TJ, Konishi K, Zhang Y, Gibson K, Lokshin AE, Lindell KO, Cisneros J, Macdonald SD, Pardo A, Sciurba F, Dauber J, Selman M, Gochuico BR, Kaminski N. MMP1 and MMP7 as potential peripheral blood biomarkers in idiopathic pulmonary fibrosis. PLoS Med. 2008;5:e93. doi: 10.1371/journal.pmed.0050093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Gilani SR, Vuga LJ, Lindell KO, Gibson KF, Xue J, Kaminski N, Valentine VG, Lindsay EK, George MP, Steele C, et al. CD28 down-regulation on circulating CD4 T-cells is associated with poor prognoses of patients with idiopathic pulmonary fibrosis. PLoS One. 2010;5:e8959. doi: 10.1371/journal.pone.0008959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Richards TJ, Kaminski N, Baribaud F, Flavin S, Brodmerkel C, Horowitz D, Li K, Choi J, Vuga LJ, Lindell KO, Klesen M, Zhang Y, Gibson KF. Peripheral blood proteins predict mortality in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2012;185:67–76. doi: 10.1164/rccm.201101-0058OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.McKeown S, Richter AG, O’Kane C, McAuley DF, Thickett DR. MMP expression and abnormal lung permeability are important determinants of outcome in IPF. Eur Respir J. 2009;33:77–84. doi: 10.1183/09031936.00060708. [DOI] [PubMed] [Google Scholar]
- 164.Shinoda H, Tasaka S, Fujishima S, Yamasawa W, Miyamoto K, Nakano Y, Kamata H, Hasegawa N, Ishizaka A. Elevated CC chemokine level in bronchoalveolar lavage fluid is predictive of a poor outcome of idiopathic pulmonary fibrosis. Respiration. 2009;78:285–292. doi: 10.1159/000207617. [DOI] [PubMed] [Google Scholar]
- 165.Richter AG, McKeown S, Rathinam S, Harper L, Rajesh P, McAuley DF, Heljasvaara R, Thickett DR. Soluble endostatin is a novel inhibitor of epithelial repair in idiopathic pulmonary fibrosis. Thorax. 2009;64:156–161. doi: 10.1136/thx.2008.102814. [DOI] [PubMed] [Google Scholar]