Abstract
In global disease outbreaks, there are significant time delays between the source of an outbreak and collective action. Some delay is necessary, but recent delays have been extended by insufficient surveillance capacity and time-consuming efforts to mobilize action.
Three public health emergencies of international concern (PHEICs)—H1N1, Ebola, and Zika—allow us to identify and compare sources of delays and consider seven hypotheses about what influences the length of delays. These hypotheses can then motivate further research that empirically tests them. The three PHEICs suggest that deferred global mobilization is a greater source of delay than is poor surveillance capacity. These case study outbreaks support hypotheses that we see quicker responses for novel diseases when outbreaks do not coincide with holidays and when US citizens are infected. They do not support hypotheses that we see quicker responses for more severe outbreaks or those that threaten larger numbers of people.
Better understanding the reason for delays can help target policy interventions and identify the kind of global institutional changes needed to reduce the spread and severity of future PHEICs.
Increasing global trade, travel, and climate change have accelerated the spread of disease outbreaks beyond national borders to more quickly develop into international concerns. After the severe acute respiratory syndrome (SARS) epidemic, there were major efforts to build surveillance and response systems to identify outbreaks early, respond globally, and contain spread at the source.1
Yet despite these efforts, we still see prolonged time delays in severe outbreaks between their emergence and global collective action. To simplify, there are two main processes that can result in delays. First, there will be a delay between the emergence of an outbreak’s index case and the detection of the outbreak by health care providers, laboratories, and public health authorities. One goal of disease surveillance is to minimize this delay and maximize available information for guiding the public health response through ongoing data collection, analysis, and management. Second, there will be a delay between an outbreak’s detection and widespread recognition of the outbreak as an international concern. Should outbreaks involve international spread and require a coordinated international response, such recognition is best evidenced by a declaration from the World Health Organization (WHO) that it constitutes a public health emergency of international concern (PHEIC). In making this declaration, WHO’s director general considers the prevention, protection, and response needs of the situation and the advice of an emergency committee before potentially mobilizing efforts to address these needs.2
When the systems for recognizing and responding to disease outbreaks act too slowly, the result is unnecessary delay, greater disease spread, additional people affected, and more lives lost.3–6 We used the last three PHEICs—H1N1, Ebola, and Zika outbreaks—as case studies to compare sources of delays and to screen seven potential hypotheses of what influences the length of delays. Our goal was to identify and consider possible reasons for the delays to motivate future hypothesis-testing research that empirically assesses them and ultimately informs the design of evidence-based interventions that hasten future outbreak responses.
TECHNICAL VS POLITICAL DELAYS
If global surveillance was the main source of delay, there would be a significant lag between an outbreak’s index case and local health officials’ action that leads to laboratory diagnosis. In none of the three PHEICs can surveillance capacity challenges be blamed for the majority of delay.
Surveillance capacity caused no meaningful delay in the 2009 H1N1 influenza outbreak. Mexico identified the unusual respiratory illness within three days of its emergence.7,8 Mexico’s Ministry of Health swiftly notified the Pan-American Health Organization (PAHO) and implemented infection prevention and control measures throughout the country as it tracked the virus’s spread.8
Although such quick detection was not possible in Guinea and other West African countries when Ebola emerged on December 26, 2013, much of the delay derived from the incorrect thought that deaths were from cholera or Lassa fever.9 Diagnostic accuracy must be improved, as insufficient surveillance and laboratory capacity delayed the Ebola response by 2.5 months—the time from the outbreak’s detection to when French scientists at the Institut Pasteur de Lyon confirmed it was Ebola on March 22, 2014.9 Although this was a delay, it accounts for a small percentage of the total time to full mobilization.
Surveillance was not the main source of delay in the response to Zika in Latin America. Brazilian authorities swiftly noted the rise in microcephaly cases, even though the root cause of the microcephaly was not immediately identified.10 After initial data of a microcephaly cluster became available on October 17, 2015,11 local health officials immediately began investigating the cause, gathering further information in the face of uncertainty about the cluster, and Brazil’s Ministry of Health established emergency operations centers in affected areas only a month later.12
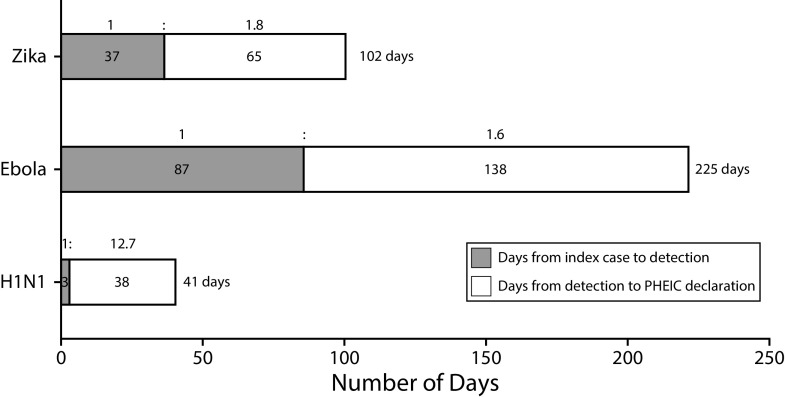
If surveillance is not a main source of delay, slow political mobilization following outbreak detection may be a culprit. In fact, overall, on the basis of these three PHEICs, poor mobilization is responsible for 1.9 times more delay than is insufficient surveillance capacity (i.e., 241 days vs 127 days cumulatively; Figure 1).
FIGURE 1—
Delays From Index Case to Outbreak Detection to PHEIC Declaration
Note. PHEIC = public health emergencies of international concern. The H1N1 outbreak began March 15, 2009, was detected March 18, 2009, and was declared a PHEIC April 25, 2009. The West African Ebola outbreak began December 26, 2013, was detected March 22, 2014, and was declared a PHEIC August 8, 2014. For the Zika outbreak, the main concern was microcephaly rather than Zika virus infections; thus we consider this outbreak to have begun October 22, 2015, when the rise in microcephaly cases was first identified, and we consider the outbreak detected November 28, 2015, once there was strong evidence of a link between the virus and the microcephaly cases. The Zika outbreak was declared a PHEIC February 1, 2016.
One cause of delayed mobilization is the contextual and scientific uncertainty in each case. As more data become available, interpretation of data, characterization of risk, and epidemiologic analysis become clearer and inform decisions to mobilize. Yet, there were delays after increased scientific certainty in the three PHEICs, indicating that there are additional causes of delayed political mobilization beyond surveillance and uncertain scientific evidence.
After laboratories isolated H1N1 on March 18, 2009, just three days after H1N1’s emergence, it took WHO one month to declare a PHEIC. The Mexican government started much of the effort needed to track and control the spread in the interim. By April 17, 2009, all hospitals were asked to report any case of severe respiratory illness and collect specimens, and by April 23, 2009, a case definition had been developed.8 In this case, there was relatively quick global mobilization once the nature of the pandemic was understood.
In stark contrast to the speed of global action in 2009 was the delay in responding to Ebola in 2014. After Ebola was confirmed on March 22, 2014,9 some action did happen: WHO mobilized its Global Outbreak Alert and Response Network, and Médecins Sans Frontières established a field presence.9,13 As the virus spread to Sierra Leone, WHO created an emergency response team.8 But despite growing evidence of the outbreak’s uncontrolled spread, a PHEIC was not declared until August 8, 2014—138 days after Ebola’s detection.14
Most recently, there was delayed global political mobilization for the Zika outbreak, despite Brazil’s declaration of a national emergency on November 11, 2015.12 Although PAHO formally warned of the link between Zika, neurologic syndromes, and microcephaly on December 1, 2015,15 it took another two months before WHO declared a PHEIC on February 1, 2016.16 There was little international news media coverage of Zika from early December 2015 to mid-January 2016 despite steadily increasing infection rates and an understanding of the link between the virus and neurologic abnormalities.
SCREENING HYPOTHESES ON FASTER RESPONSES
Why is global political mobilization much faster for some outbreaks than others? With so many unique factors playing a role in each outbreak, it is difficult to pinpoint exact determinants of delay. But these three PHEICs provide an opportunity to identify some likely hypotheses and consider whether they are consistent with what was actually seen during these outbreaks (seven hypotheses summarized in Table 1). Our exploratory analysis provides a basis for future empirical research to diagnose causes of delay and inform efforts to respond quickly to future outbreaks.
TABLE 1—
Hypotheses on What Elicits Faster Outbreak Responses and Evidence for Each Hypothesis From the H1N1, Ebola, and Zika Outbreaks
| Hypothesis | H1N1 (Fastest) | Zika (Intermediate) | Ebola (Slowest) | Supported by 3 Cases? | Explanation |
| More severe disease | Least severe | Intermediate severity | Most severe | Not supported | The more severe diseases did not elicit faster responses than did the less severe diseases |
| More countries affecteda | 3 countries | 21 countries | 5 countries | Not supported | H1N1 elicited fastest response after only 3 countries, whereas Zika’s slower response came after 21 countries were affected |
| More people at risk | Everyone at risk | Mostly future babies at risk | Close contacts and caregivers at highest risk | Not supported | Ebola, which risked an intermediate-sized population, had the slowest response |
| Disease novelty | No experience | Some experience | Considerable experience | Supported | Novel H1N1 virus elicited a fast response, whereas the known viruses elicited slower responses |
| Greater ease of transmission | Airborne | Vector, mosquito, sexual | Contact, sexual | Supported | H1N1, an airborne infection, led to fast response; Ebola, with more easily preventable transmission, had delayed response |
| Not spread during holiday seasons | No holiday | Christmas | Summer | Supported | Zika and Ebola, which worsened when many public health professionals took vacations, elicited slower responses |
| Impact on US citizens | First US citizen infected 10 d before PHEIC | First transmission in the US confirmed 7 d before PHEIC | First infected person in the US 6 d before PHEIC | Supported | PHEICs consistently declared within 10 d of having a direct impact on US citizens |
Note. PHEIC = public health emergencies of international concern. This table provides a summary of the evidence that either supports or does not support the 7 identified hypotheses. We considered hypotheses supported if their categorical ordering across the 3 PHEICs matches the order of how quickly the world responded to those PHEICs.
Number of countries with at least 1 infected person at the time of PHEIC declaration. For Zika, this is the number of countries with confirmed cases of Zika infection, not clusters of microcephaly.
First, one might expect the speed of political mobilization to increase with disease severity. Yet, the H1N1 outbreak caused the least severe disease of the three PHEICs and attracted the fastest global mobilization. It therefore seems unlikely that severity, especially as demonstrated by the early outbreak, dictates speed of mobilization.
A second hypothesis is that when more countries are affected, global response is faster. This makes sense because PHEICs, by definition, are invoked to mitigate diseases’ international spread; evidence of such spread should trigger discussion and even follow-up action. Yet the outbreak of microcephaly related to Zika virus contradicts this hypothesis, as the virus affected 21 countries before a PHEIC was finally declared. Only three countries had H1N1 infections when that outbreak was declared a PHEIC.
A third hypothesis is that the number of people at risk predicts mobilization, whereby diseases that easily spread to whole populations might be considered more concerning than those dangerous to smaller groups. H1N1, an airborne disease, could easily spread across whole populations. Although Zika infection is widespread, microcephaly is concentrated within a small subset of the population: fetuses within pregnant women. Ebola falls between the two; in West Africa, it primarily infected those caring for the sick and often spread to family and health care providers, including overseas volunteers. This hypothesis is therefore not supported by the three cases.
A fourth hypothesis is that disease novelty breeds fears of doomsday scenarios that motivate quicker precautionary action and that familiarity correspondingly causes global quiescence that lulls people into a false sense of security. This possibility cannot be ruled out on the basis of the last three PHEICs: H1N1 was a novel strain of influenza with quick mobilization, whereas the well-known Ebola virus elicited the slowest response. Although there was significant global experience with influenza outbreaks, Ebola had never affected large enough populations to cause an international emergency. The novelty of the West African setting and transmission within urban areas might even have precipitated delays in mobilization rather than action. Additionally, greater knowledge about familiar entities, such as influenza, might hasten mobilization attributable to a more complete understanding of the risk.
A fifth hypothesis is that the mode of transmission and its perception by the public affects mobilization. Airborne diseases, like H1N1, can spread more broadly, put more people at risk, be more difficult to contain, instill greater fear, and require more stringent precautions than do diseases like Ebola that spread only through contact and droplets. Vector-borne diseases like Zika are more predictable than are airborne diseases—probably eliciting less fear—but are harder for individuals to protect themselves against than are contact-borne infections. Vector-borne diseases require different infection prevention and control mechanisms, as quarantine and hygienic medical practice will not prevent their spread.
Furthermore, Zika was found to be sexually transmissible weeks before the PHEIC was declared; although the evidence was sparse, this could have contributed to mobilization because of additional public fear of a second mode of transmission that may be harder to detect and the virus’s ability to spread to areas without the main Aedes aegypti mosquito vector. If airborne diseases are most difficult to contain, they would more easily trigger an emergency. This is supported by the speed of PHEIC declaration during the H1N1 outbreak and delays for the other two. Airborne transmission may also more easily spread across international borders, which is the concern that would trigger a PHEIC. Although Ebola was found in 2015 to also be sexually transmitted, this was long after local and international communities had taken action.
A sixth hypothesis is that faster responses can be expected when diseases worsen outside holiday seasons, when public health authorities (e.g., WHO staff) are not on vacation. Perhaps it is just a wicked coincidence, but the disease with the slowest mobilization (Ebola) worsened over Geneva’s long summer holidays, and the disease with the second slowest mobilization (Zika) spread over the shorter Christmas holidays. The fastest mobilization (H1N1) was mounted when public health professionals, both locally and internationally, were at work—consistent with this hypothesis. Although data on staff vacation periods are not publicly available, this coincidence leads one to wonder whether staff availability played any role in delayed mobilization.
A final hypothesis is that outbreaks affecting US citizens, whose country is the world’s most powerful, are responded to most quickly; or, more concerning, that direct impact on the United States is a necessary condition for a PHEIC’s declaration. Evidence from all three case studies supports this hypothesis. For H1N1, a PHEIC was declared 10 days after the first US citizen had a documented infection, on April 15, 2009.17 Ebola was declared a PHEIC only six days after infected health care providers arrived for the first time in the United States on August 2, 2014, for treatment, although it coincided with the introduction of Ebola into Nigeria via a traveler from Liberia. Zika was declared a PHEIC two weeks after a Zika-positive microcephalic baby was born in Hawaii on January 15, 2016, and one week after the United States’ first laboratory-confirmed case of Zika on January 25, 2016, in the US Virgin Islands. Although this may simply reflect the nature of a PHEIC that there be demonstrable potential for international spread and the potential populations at risk, other examples of international spread in these outbreaks do not appear to be as closely tied to initiation of the global political response.
CONCLUSIONS
Understanding why collective action is delayed in global disease outbreaks provides guidance for hastening future responses. Using these three PHEICs as case studies, we have seen that greater delay seems to be attributable to poor political mobilization rather than technical surveillance capacity. This is in sharp contrast to the post-Ebola calls for increased surveillance as the key to appropriate outbreak response.18–20 More of the solution might actually reside in improving global institutional structures that currently slow political mobilization.
Some of these hypotheses, if true, could be seen as justifiable reasons for delayed political action. It would make sense that mobilization was slower for diseases that were less severe, affected fewer countries, or risked fewer people. Unfortunately, none of these hypotheses are consistent with the three recent PHEICs. Instead, half of the hypotheses that remain are actually extremely troubling, in that they point to the hazards of holidays and US exceptionalism.
Properly testing the four remaining hypotheses—that disease novelty, ease of transmission, transmission during nonholiday seasons, and outbreaks that affect US citizens hasten global mobilization—requires studying more cases. Process tracing from political science is one important tool for better understanding why different outbreaks receive different responses. Qualitative analysis of news media and political speeches can also be helpful.21 There are additional insights to be gained from probing why other recent outbreaks, such as the Middle East Respiratory Syndrome coronavirus, were not declared PHEICs. More research should also be conducted to better understand the role that scientific uncertainty may play in delaying political responses to outbreaks, as well as to better understand the additional factors beyond lagging political mobilization that contribute to delayed action.
Ultimately, we hope the causes of political delays are scientifically and ethically justifiable, even though we recognize that delays are probably multifactorial and include both enlightened and unsavory elements. Once the causes are known, global decision-makers should be able to better target policy interventions, open important conversations about how we prioritize disease control efforts, and identify the kinds of global institutional changes needed to reduce the spread and severity of pandemics.22–26 Further research may necessitate changes to the way we evaluate and declare outbreaks as PHEICs if the causes of political delays are confirmed to be scientifically or ethically suspect. In the meantime, we should plan additional hypothesis-testing research and experiment with mechanisms to reduce political delays so that global disease outbreaks are addressed as quickly as possible.
ACKNOWLEDGMENTS
This work was completed as part of the International Collaboration for Capitalizing on Cost-Effective and Life-Saving Commodities, which is funded by the Research Council of Norway’s Global Health & Vaccination Programme (GLOBVAC project 234608). S. J. H. is additionally funded by the Canadian Institutes of Health Research and the Ontario government’s Ministry of Research, Innovation and Science.
S. J. H. previously worked for the World Health Organization.
REFERENCES
- 1.Hoffman SJ. The evolution, etiology and eventualities of the global health security regime. Health Policy Plan. 2010;25(6):510–522. doi: 10.1093/heapol/czq037. [DOI] [PubMed] [Google Scholar]
- 2.Ottersen T, Hoffman SJ, Groux G. Ebola again shows the international health regulations are broken: what can be done differently to prepare for the next epidemic. Am J Law Med. 2016;42(2–3):356–392. doi: 10.1177/0098858816658273. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Report of the Ebola Interim Assessment Panel—July 2015. Geneva: 2015. [Google Scholar]
- 4.Moon S, Sridhar D, Pate MA et al. Will Ebola change the game? Ten essential reforms before the next pandemic. The report of the Harvard-LSHTM independent panel on the global response to Ebola. Lancet. 2015;386(10009):2204–2221. doi: 10.1016/S0140-6736(15)00946-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Commission on a Global Health Risk Framework for the Future. The Neglected Dimension of Global Security: A Framework to Counter Infectious Disease Crises. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 6.United Nations. Protecting Humanity From Future Health Crises: Report of the High-Level Panel on the Global Response to Health Crises. New York: 2016. [Google Scholar]
- 7.Hsieh YH, Ma S, Hernandez JX, Lee VJ, Lim WY. Early outbreak of 2009 influenza A (H1N1) in Mexico prior to identification of pH1N1 virus. PLoS One. 2011;6(8):e23853. doi: 10.1371/journal.pone.0023853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Outbreak of swine-origin influenza A (H1N1) virus infection—Mexico, March–April 2009. MMWR Morb Mortal Wkly Rep. 2009;58(17):467–470. [PubMed] [Google Scholar]
- 9.World Health Organization. Origins of the 2014 Ebola epidemic: one year into the Ebola epidemic. 2015. Available at: http://www.who.int/csr/disease/ebola/one-year-report/virus-origin/en. Accessed December 15, 2017.
- 10.Centers for Disease Control and Prevention. Increase in reported prevalence of microcephaly in infants born to women living in areas with confirmed Zika virus transmission during the first trimester of pregnancy—Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(9):242–247. doi: 10.15585/mmwr.mm6509e2. [DOI] [PubMed] [Google Scholar]
- 11.Ministério da Saúde. Ministério da Saúde divulga boletim epidemiológico. 2015. Available at: http://portalsaude.saude.gov.br/index.php/cidadao/principal/agencia-saude/20805-ministerio-da-saudedivulga-boletim-epidemiologico. Accessed December 12, 2017.
- 12.Ministério da Saúde. Portaria GM no 1.813, de 11 de Novembro de 2015. 2015. Available at: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2015/prt1813_11_11_2015.html. Accessed December 15, 2017.
- 13.Vetter P, Dayer JA, Schibler M et al. The 2014–2015 Ebola outbreak in West Africa: hands on. Antimicrob Resist Infect Control. 2016;5(1):17. [Google Scholar]
- 14.World Health Organization. Statement on the 1st meeting of the IHR Emergency Committee regarding the 2014 Ebola outbreak in West Africa. 2014. Available at: http://www.who.int/mediacentre/news/statements/2014/ebola-20140808/en. Accessed December 15, 2017.
- 15.Pan-American Health Organization. Neurological Syndrome, Congenital Malformations, and Zika Virus Infection. Implication for Public Health in the Americas. Washington, DC: 2015. [Google Scholar]
- 16.World Health Organization. WHO statement on the first meeting of the International Health Regulations (2005) Emergency Committee on Zika virus and observed increase in neurological disorders and neonatal malformations. 2016. Available at: http://www.who.int/mediacentre/news/statements/2016/1st-emergency-committee-zika/en. Accessed December 15, 2017.
- 17.Centers for Disease Control and Prevention. Swine influenza A (H1N1) infection in two children—Southern California, March–April 2009. MMWR Morb Mortal Wkly Rep. 2009;58(15):400–402. [PubMed] [Google Scholar]
- 18.Gates B. The next epidemic—lessons from Ebola. N Engl J Med. 2015;372(15):1381–1384. doi: 10.1056/NEJMp1502918. [DOI] [PubMed] [Google Scholar]
- 19.Tomori O. Will Africa’s future epidemic ride on forgotten lessons from the Ebola epidemic? BMC Med. 2015;13:116. doi: 10.1186/s12916-015-0359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalra S, Kelkar D, Galwankar SC et al. The emergence of Ebola as a global health security threat: from ‘lessons learned’ to coordinated multilateral containment efforts. J Glob Infect Dis. 2014;6(4):164–177. doi: 10.4103/0974-777X.145247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffman SJ, Justicz V. Automatically quantifying the scientific quality and sensationalism of news records mentioning pandemics: validating a maximum entropy machine-learning model. J Clin Epidemiol. 2016;75:47–55. doi: 10.1016/j.jclinepi.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoffman SJ, Caleo GM, Daulaire N et al. Strategies for achieving global collective action on antimicrobial resistance. Bull World Health Organ. 2015;93(12):867–876. doi: 10.2471/BLT.15.153171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffman SJ, Røttingen JA, Frenk J. Assessing proposals for new global health treaties: an analytic framework. Am J Public Health. 2015;105(8):1523–1530. doi: 10.2105/AJPH.2015.302726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gopinathan U, Watts N, Hougendobler D et al. Conceptual and institutional gaps: understanding how the WHO can become a more effective cross-sectoral collaborator. Global Health. 2015;11(46):1–13. doi: 10.1186/s12992-015-0128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoffman SJ. Mitigating inequalities of influence among states in global decision making. Global Policy. 2012;3(4):421–432. [Google Scholar]
- 26.Hoffman SJ, Røttingen JA. Assessing implementation mechanisms for an international agreement on research and development for health products. Bull World Health Organ. 2012;90(12):854–863. doi: 10.2471/BLT.12.109827. [DOI] [PMC free article] [PubMed] [Google Scholar]