Abstract
Objectives. To compare the effectiveness of patient navigation–enhanced case management in supporting engagement in HIV care upon release from jail relative to existing services.
Methods. We randomized 270 HIV-infected individuals to receive navigation-enhanced case management for 12 months or standard case management for 90 days following release from jail between 2010 and 2013. Participants were interviewed at 2, 6, and 12 months after release. We abstracted medical data from jail and city health records.
Results. Patient navigation–enhanced case management resulted in greater linkage to care within 30 days of release (odds ratio [OR] = 2.15; 95% confidence interval [CI] = 1.23, 3.75) and consistent retention over 12 months (OR = 1.95; 95% CI = 1.11, 3.46). Receipt of treatment for substance use disorders in jail also resulted in early linkage (OR = 4.06; 95% CI = 1.93, 8.53) and retention (OR = 2.52; 95% CI = 1.21, 5.23). Latinos were less likely to be linked to (OR = 0.35; 95% CI = 0.14, 0.91) or retained in (OR = 0.28; 95% CI = 0.09, 0.82) HIV care.
Conclusions. Patient navigation supports maintaining engagement in care and can mitigate health disparities, and should become the standard of care for HIV-infected individuals leaving jail.
Of the more than 2 million people incarcerated in the United States,1,2 correctional facilities hold more than 20 000 people living with HIV.3 The rate of HIV among incarcerated individuals is 5 times that of the general population,3 largely because of increased incarceration for crimes related to drug use associated with HIV.4,5 In San Francisco, California, nearly all individuals with HIV detained in jail reported active drug use in the 30 days before entering jail.6
An estimated 1 in 7 people living with HIV leave prisons and jails each year in the United States,7 and many struggle to access care and treatment upon release, with as many as 95% experiencing a gap in HIV treatment.8–11 HIV care, including antiretroviral treatment, not only benefits the individuals who receive it but also prevents transmission of the infection.12 However, challenges facing individuals when they leave jail as basic as finding housing and food can prevent or delay reintegration into HIV care in the community.13,14
Reentry into the community can be a stressful and dangerous time for all individuals released from correctional settings and particularly hard for individuals with substance dependence. Enforced abstinence without drug treatment is the standard in most jails and prisons, and it does not adequately prepare an individual to cope when they are released. These individuals face higher risk of HIV transmission and death from overdose upon release compared with individuals without substance use disorders.11
Discharge planning and intensive case management programs can help ease the transition back to the community.15 Although strategies and practice vary from one setting to another, traditional case management coordinates social, mental health, medical, and other services for a client. Studies have shown variable success in HIV-related outcomes.15–18 Some studies have shown associations between case management and improved HIV clinical outcomes,19 and linkage to medical, social, and addiction services.20
As an enhancement to case management or as a stand-alone, the patient navigation model, initially developed for cancer care, has been increasingly used with vulnerable HIV-infected populations.21,22 The navigator, usually a nonclinical paraprofessional or peer, acts as a kind of a “coach” to the client. Navigators use a strengths-based philosophy to support clients in leveraging their own personal resources, talents, and strengths to best access available services.22 Navigators do not take the place of traditional case managers, but work as part of a care team to ensure continuity of care.21
To assess whether navigation could help HIV-infected individuals in jail successfully transition back into the community, we evaluated a navigation intervention delivered in San Francisco. This article describes the outcomes of the project in terms of linkage to and engagement in HIV care over the course of 1 year. We also examined intervention effects on substance use and risky sexual behavior.
METHODS
This study took place in the San Francisco County Jail from 2010 to 2013. At the time of the study, the jail housed approximately 1200 inmates distributed among 9 distinct facilities. More than 20 000 unique persons are booked into the jail and 50 000 total repeated bookings flow through 1 centralized entry facility in a given year. The jail population at the time of the study was 80% male and 20% female, 35% African American, 30% Latino, and 30% White. HIV care and treatment services are delivered by what was then called the Forensic AIDS Project (FAP), a division of the San Francisco Department of Public Health renowned for innovative programs and services.
Overall Study Design and Participants
The study design was a randomized controlled trial. We randomized with a computerized algorithm. Surveys were administered via audio computer-assisted self-interview (ACASI) inside the jail at baseline, and follow-up surveys were conducted by study staff at 2, 6, and 12 months following the index release. Medical data were abstracted from electronic records.
Participants were HIV-infected adults incarcerated in the San Francisco County Jail not held in a high level of security during the time of initial recruitment. All participants were arrested in San Francisco and admitted to the San Francisco County Jail (were not transfers), were English speaking, reported previous or current drug use, and were detained for at least 48 hours. We recruited participants likely to be released to the community during the recruitment phase of the study. Those enrolled were able to provide informed, written consent for participation.
Procedures
Baseline recruitment and randomization.
People living with HIV in the jail system were asked by medical providers if they would be willing to participate in the study. Interested individuals met with study staff and, if interested and eligible, gave informed consent. After completing the baseline ACASI in a private room inside the jail, participants were randomized to receive either treatment as usual (TAU) or navigation-enhanced case management (NAV).
Treatment as usual.
The TAU at the time of this study was discharge planning and up to 90 days of as-needed case management provided by FAP, based on standards developed and adopted in San Francisco.23 In the jail, HIV-infected individuals were stabilized with access to comprehensive medical services and psychiatric assessment and counseling. All HIV-infected clients received one-on-one counseling and regular visits from a registered nurse or a case manager. Individuals with substance dependence issues received ongoing psychiatric evaluations and therapeutic interventions to address them and also to prepare clients for coping with these issues upon release.
When a client was within 30 days of release, the FAP case manager prepared a discharge plan. On the basis of the assessment completed at the initial intake visit with the patient, plans included objectives in each of 5 domains: medical health, psychiatric health, criminal justice requirements (e.g., reporting to probation, work, or treatment programs), drug and alcohol addiction care, and life care (housing, benefits, job training, or employment). Referrals and appointments were set up in all domains necessary and available. AIDS Drug Assistance Program recertification or enrollment to cover costs of HIV-associated medications was also activated by FAP. Clients received a 7-day supply of HIV medications at the time of release and typically a prescription for a 1-month supply of medications, depending on the discharge plan and the client’s insurance. Upon release, case managers provided clients with some support for transportation, clothing, household goods, and food. The model was developed with the goal of transitioning clients into community-based HIV care within 30 days of release, although FAP case managers would work with a client for up to 90 days.
Intervention.
The NAV intervention was designed by experts at the San Francisco Pre-Trial Diversion Project, a community-based organization that has been working with individuals recently released from jail since 1976. Based on strengths-based social work and harm-reduction principles, the intervention involved specialized risk-reduction discharge planning along with navigation upon release to achieve HIV care and service outcomes. Project START, a proven-effective intervention recommended for replication by the Centers for Disease Control and Prevention, was used as the HIV risk-reduction framework. START is a client-centered HIV, sexually transmitted infection, and hepatitis risk-reduction and engagement-in-care intervention for persons being released from prison or jail.24 On the basis of harm reduction, the intervention uses prevention case management and motivational interviewing techniques to encourage sexual and drug risk reduction. The patient navigators used START’s principles to facilitate reentry into care in the community, referrals for housing, employment, substance dependence, mental health treatment, legal issues, referrals associated with obtaining social benefits such as general assistance, and social security insurance, and also counseled clients about how to avoid reincarceration. The intervention was manualized and is available from the authors upon request.
Patient navigators were selected and hired because they shared characteristics with the clients served; they were HIV-infected and shared similar backgrounds, including past histories of incarceration and substance use disorders. In addition, all demonstrated consistent engagement with social and medical services and possessed good organizational and communications skills. Navigators worked in tandem with a professional case manager to monitor adherence to care while also providing coaching and mentoring support across all aspects of the client’s life. Before release, the case manager (who had a security clearance) provided discharge planning and patient education and served as a liaison to the courts. After release, patient navigators enhanced case management services by, for example, securing transportation for clients to medical and social service appointments, accompanying clients to medical or social service appointments, providing coaching and social support, and helping clients secure food and housing services. Further detail on the intervention has been published elsewhere.25
Evaluation.
Study staff collected data on health status, drug use, and participant characteristics through the ACASI at baseline (in private rooms in the jail) and follow-up visits (in a private study office near the jail). For intervention participants, detailed records were kept on the amount and type of services provided by navigators. Study staff abstracted medical record and laboratory test information from 2 electronic medical record systems: the jail medical record and the city electronic medical record, which holds records of services provided in community public health settings. They abstracted data for all visit dates, HIV tests, and for all medications dispensed through the jail medical care system. Pharmacy records were not available for community care as these are not captured by the city electronic medical record systems.
Predictors.
The ACASI covered demographic characteristics, physical health, mental health, substance use and other risk behaviors, health-seeking behaviors, and medication use. Participants reported mental health and physical health scores with the 12-item Short-Form Survey (SF-12) scale.26 We calculated scores according to published guidelines.27 Participants completed the Brief Symptom Inventory to assess depression.28 Participants completed the Drug Abuse Screening Test-10 (DAST-10), and drug use was defined as any moderate, substantial, or severe drug use in the 12 months before baseline.29 We determined problematic alcohol use with the 3-item Modified Alcohol Use Disorders Identification Test (AUDIT-C), defined as having an “active alcohol use disorder.”30
Primary outcome measures.
We considered participants to be linked to care if they had at least 1 documented nonurgent visit to a community medical provider within 30 days of their release from jail (to coincide with the amount of antiretroviral treatment they were able to access upon release). We chose nonurgent visits as an outcome because they are indicative of participant engagement. We considered participants to be consistently engaged in care during the follow-up year if they had a nonurgent medical care visit between each of the follow-up visits (2, 6, and 12 months).
We abstracted viral load measures from both jail- and city-based laboratory databases. We evaluated viral suppression in 2 ways. One way was having a measured viral load below 50 copies per milliliter at the end of the follow-up year (between 9 and 18 months after release). If more than 1 measure was available during that window, we used the final measure. The other way was a measure of sustained suppression—defined here as having at least 2 viral load measures during the follow-up year, with all viral loads measuring less than 200 copies per milliliter.
We defined risky sex as participating in at least 1 condomless sexual act during the previous assessment period that could transmit HIV to an HIV-negative or unknown-status partner. We defined risky drug use as self-reported use of illicit substances on a weekly basis at any point during follow-up. In addition, drug use was measured with a urine test. For those who agreed to testing, we compared the proportion of participants who screened positive for methamphetamines, cocaine, THC (marijuana), or benzodiazepines during a follow-up visit. We did not include opioid medications because we were unable to determine a difference between medical and recreational use.
Analysis.
The primary aim of the analysis was to explore whether there were statistically significant differences after release among participants in the NAV and TAU groups on any of the primary outcome measures. To evaluate unadjusted comparisons, we used the χ2 test. For primary HIV care outcomes, we used an intention-to-treat–based logistic regression. We also constructed expanded multivariable logistic models including additional factors shown in the literature or suspected to influence linkage to and engagement in HIV care, including demographics (age, gender, race/ethnicity, education) and receipt of services for either substance dependence or mental health with control for intervention status. We conducted all analyses with SAS version 9.4 statistical software (SAS Institute, Cary, NC).
RESULTS
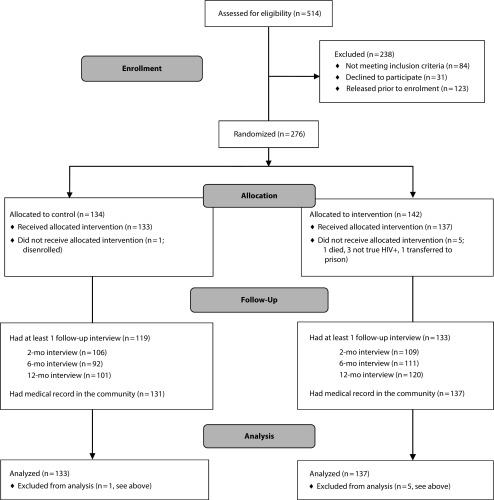
We assessed 514 individuals for eligibility, of whom we excluded 238 because they did not meet inclusion criteria, declined to participate, or were released before enrollment (Figure 1). We randomized 276 to either the TAU (n = 134) or NAV (n = 142) groups. Of participants randomized, we subsequently excluded 6 because they did not receive the intervention for a variety of reasons (Figure 1). Of 270 participants analyzed, 252 completed at least 1 follow-up ACASI interview. Although retention was high across the study, participants in the intervention arm were more likely to return for an interview visit during the follow-up period (97% vs 89%; P < .05). Medical records from the city systems, our main source of primary outcome data, were available for almost all participants (n = 268). Urine drug testing was available for a limited group of participants (201 participants were tested at least once). Individuals in the NAV arm utilized a mean of 48.6 hours of services, predominantly in the first 2 months following release (9 hours per month in months 1 and 2 vs 2.5 hours per month from months 6 through 12). The duration of services for the TAU clients was not available to the study.
FIGURE 1—
Study Enrollment and Participation: HIV-Infected Individuals Leaving Jail, San Francisco, CA, 2010–2013
Demographic Characteristics
Table 1 displays the baseline characteristics for participants overall and by study arm. Participants in the study were mostly male (81.5%) and primarily middle-aged (mean age = 43 years). The majority of participants had at least a high-school education (55.6%). Participants were mostly African American (43.7%), White (28.9%), and Latino (15.2%). Half of participants identified as heterosexual (49.3%). The overall average mental and physical health scores calculated with the SF-12 were 35.7 and 45, respectively, below the national averages of 50. There were no significant differences in demographic characteristics and mental and physical health status by study arm.
TABLE 1—
Characteristics of Participants Enrolled Stratified by Study Arm: HIV-Infected Individuals Leaving Jail, San Francisco, CA, 2010–2013
| Characteristics | All | TAU | NAV | P |
| Gender, no. (%) | .54 | |||
| Male | 220 (81.48) | 106 (79.7) | 114 (83.21) | |
| Female | 33 (12.22) | 18 (13.53) | 15 (10.95) | |
| Trans, male-to-female | 16 (5.93) | 9 (6.77) | 7 (5.11) | |
| Trans, female-to-male | 1 (0.37) | 0 (0) | 1 (0.73) | |
| Age, y, mean ±SD | 43.19 ±10.72 | 43.35 ±11.98 | 43.03 ±9.38 | .81 |
| Education, no. (%) | .19 | |||
| < high school | 83 (30.74) | 35 (26.32) | 48 (35.04) | |
| High-school diploma or GED | 150 (55.56) | 76 (57.14) | 74 (54.01) | |
| College or grad work | 37 (13.70) | 22 (16.54) | 15 (10.95) | |
| Race/ethnicity, no. (%) | .17 | |||
| Non-Hispanic Black | 118 (43.70) | 60 (45.11) | 58 (42.34) | |
| Non-Hispanic White | 78 (28.89) | 31 (23.31) | 47 (34.31) | |
| Hispanic or Latino | 41 (15.19) | 22 (16.54) | 19 (13.87) | |
| Other | 33 (12.22) | 20 (15.04) | 13 (9.49) | |
| Sexual orientation, no. (%) | .70 | |||
| Gay or lesbian | 67 (24.81) | 32 (24.06) | 35 (25.55) | |
| Bisexual | 67 (24.81) | 29 (21.8) | 38 (27.74) | |
| Straight or heterosexual | 133 (49.29) | 71 (53.38) | 62 (45.26) | |
| Other | 3 (1.11) | 1 (0.75) | 2 (1.46) | |
| Mental health score, SF-12,a mean ±SD | 34.58 ±11.62 | 33.42 ±12.75 | 35.70 ±10.35 | .15 |
| Physical health score, SF-12,a mean ±SD | 45.03 ±8.20 | 45.04 ±8.17 | 45.02 ±8.22 | .98 |
| Self-reported route of infection, no. (%) | .47 | |||
| Sex with an HIV-infected man | 111 (41.26) | 58 (43.61) | 53 (38.97) | |
| Sex with an HIV-infected woman | 57 (21.19) | 23 (17.29) | 34 (25.00) | |
| Needles or injection | 80 (29.74) | 39 (29.32) | 41 (30.15) | |
| Other | 21 (7.81) | 13 (9.77) | 8 (5.88) | |
| Risky sex in the 30 d prior to jail,a no. (%) | 59 (21.77) | 24 (18.05) | 35 (25.55) | .14 |
| Alcohol use in 30 d prior to jail, no. (%) | ||||
| Any alcohol | 178 (65.93) | 87 (65.41) | 91 (66.42) | .86 |
| Alcohol more than once per wk prior to jail | 134 (49.63) | 65 (47.44) | 69 (51.88) | .42 |
| Meet criteria for alcohol abuse on AUDIT screening, no. (%) | 90 (33.33) | 40 (29.19) | 50 (37.59) | .26 |
| Drug use in 30 d prior to jail, no. (%) | 255 (94.44) | 125 (91.24) | 130 (97.74) | .75 |
| Weekly drug usea | 204 (75.56) | 92 (69.17) | 112 (84.2) | .016 |
| Methamphetamine—any | 171 (63.33) | 83 (60.58) | 88 (66.16) | .76 |
| Methamphetamine > 1 per wka | 107 (39.63) | 44 (32.11) | 63 (47.37) | .012 |
| Crack—any | 153 (56.67) | 76 (55.47) | 77 (57.89) | .88 |
| Crack > 1 per wka | 99 (36.67) | 47 (34.3) | 52 (39.12) | .46 |
| Heroin—any | 80 (29.62) | 40 (29.2) | 39 (29.32) | .77 |
| Heroin > 1 per wka | 37 (13.72) | 21 (15.32) | 16 (12.03) | .31 |
| Meet criteria for substance abuse on the DAST, no. (%) | 229 (84.81) | 111 (83.46) | 118 (86.13) | .54 |
| Meet criteria for severe substance abuse on the DAST, no. (%) | 22 (8.15) | 10 (7.52) | 12 (8.76) | .71 |
| History of detentions | ||||
| Median age at first detention, y | 18 | 18 | 17 | |
| Median no. of detentions, ever | 15 | 15 | 15 | |
| Any detentions in y prior to index detention, no. (%) | 190 (70.9) | 92 (69.17) | 98 (72.59) | .54 |
| Mean no. of detentions in y prior to index detention, mean ±SD | 1.76 ±1.86 | 1.57 ±1.67 | 1.96 ±2.01 | |
| Mean length of index incarceration, d, mean ±SD | 98.30 ±129.02 | 97.90 ±106.50 | 98.79 ±148.30 | |
| Retained in care in y prior to index detention, no. (%) | 120 (44.44) | 61 (45.86) | 59 (43.07) | .70 |
Note. AUDIT = Alcohol Use Disorders Identification Test; DAST = Drug Abuse Screening Test; GED = general equivalency diploma; NAV = enhanced peer navigation group; SF-12 = 12-item Short Form Survey; TAU = treatment as usual.
The entire sample did not answer this question either because that indicator was not collected for all individuals or because it is restricted by a skip pattern.
Risk Behavior Before Incarceration
The most commonly reported “most likely route of HIV infection” was sex with an HIV-infected man (41.3%), followed by sharing needles with an HIV-infected person (29.7%) or sex with an HIV-infected woman (21.2%). About one fifth (21.8%) of all participants reported risky sex in the 30 days before entering jail.
Two thirds (65.7%) reported consuming alcohol in the 30 days before jail admission and, of these, most reported drinking more than once a week during that time (88.7%). One third met the case definition on AUDIT-C screening instruments for alcohol abuse. Drug use in the 30 days before jail was reported by 94.4% of participants with crystal methamphetamine being the primary drug used (63.1%). The majority of individuals (84.8%) screened positive for problematic drug use with the DAST-10. Individuals in the intervention group were more likely to report weekly drug use (84.2% compared with 69.2%; P < .05) and methamphetamine use more than once per week (47.4% compared with 32.1%, P < .05) in the 30 days before jail admission compared with those in the TAU group. There were no significant differences in risky sex or alcohol use by study arm.
Detention History
The majority of participants (n = 190; 71%) had been detained in the jail system at least once in the year before the index detention (Table 1). Mean number of detentions in the year before index detention was 1.76 and the mean length of the index incarceration was 98.3 days. The median age at first detention of individuals in the TAU group was 18 years and in the NAV group it was 17 years. Individuals in both groups reported a median 15 lifetime detentions.
Intervention Effects
Table 2 shows the measures of sexual and drug-related risk behaviors over the study follow-up period. There were no statistically significant differences in alcohol and drug use risk behavior between treatment groups at the 2-, 6-, or 12-month assessment points. Those randomized to the NAV condition reported less risky sex at the 12-month assessment (7.5% vs 17.8% among those in the TAU condition).
TABLE 2—
Substance and Sexual Risk Behavior During the Year Following Release from Jail by Study Arm: HIV-Infected Individuals, San Francisco, CA, 2010–2013
| 2 Mo |
6 Mo |
12 Mo |
|||||||
| Risk Behavior | NAV (n = 108), No. (%) | TAU (n = 106), No. (%) | P | NAV (n = 111), No. (%) | TAU (n = 92), No. (%) | P | NAV (n = 120), No. (%) | TAU (n = 101), No. (%) | P |
| Risky sex in last 30 da | 11 (10.2) | 9 (8.5) | .67 | 16 (14.4) | 9 (9.8) | .32 | 9 (7.5) | 18 (17.8) | .019 |
| Any alcohol use in last 30 d | 55 (50.9) | 54 (50.9) | > .99 | 65 (58.6) | 45 (48.9) | .17 | 66 (55.0) | 60 (59.4) | .51 |
| Any drug use in last 30 d | 96 (88.1) | 86 (81.1) | .16 | 85 (76.6) | 60 (65.2) | .07 | 87 (72.5) | 74 (73.3) | .90 |
| Weekly drug use in last 30 d | 73 (67.0) | 63 (59.4) | .25 | 65 (58.6) | 44 (47.8) | .13 | 72 (60.0) | 57 (56.4) | .59 |
| Urine drug results | |||||||||
| Total | 81 | 72 | 72 | 63 | 85 | 63 | |||
| Methamphetamine | 34 (42.0) | 22 (30.6) | .14 | 30 (41.7) | 27 (42.9) | .89 | 36 (42.4) | 23 (36.5) | .47 |
| Cocaine | 27 (33.3) | 34 (47.2) | .08 | 27 (37.5) | 28 (44.4) | .41 | 36 (42.4) | 29 (46.0) | .66 |
| Marijuana | 27 (33.3) | 31 (43.1) | .22 | 29 (40.3) | 32 (50.8) | .22 | 40 (47.1) | 35 (55.6) | .31 |
| Benzodiazepines | 6 (7.79) | 4 (5.8) | .75 | 5 (5.56) | 4 (6.67) | > .99 | 7 (8.33) | 3 (4.84) | .52 |
Note. NAV = enhanced peer navigation group; TAU = treatment as usual.
At least 1 unprotected sexual act that could transmit HIV to an HIV-uninfected or unknown-status partner.
Intervention participants were significantly more likely to have a nonurgent medical visit for HIV-related care within 30 days of release (44% vs 28% in the TAU group; P < .01). Intervention participants were also more likely to be consistently engaged in HIV care (attended medical visits in each of the 3 assessment periods throughout the follow-up year) relative to the TAU group (39% vs 28%; P < .05). There were no significant differences between groups in achieving undetectable viral load less than 50 copies per milliliter at study end, or sustained suppression of less than 200 copies per milliliter during the follow-up period.
Predictors of Health Services Utilization
In the intention-to-treat analysis (Table 3), those in the NAV arm were about twice as likely to be linked to care within 30 days of release compared with those in the TAU group (OR = 2.01; 95% CI = 1.21, 3.35). They were also almost twice as likely to be retained in care across the year of the project (OR = 1.71; 95% CI = 1.02, 2.87).
TABLE 3—
Predictors of Linkage and Retention in Care Among HIV-Infected Individuals Leaving Jail: San Francisco, California, 2010–2013
| Characteristic | Linked to Care, OR (95% CI) | Retained in Care, OR (95% CI) |
| Intention-to-treat (unadjusted) estimates | ||
| Study arm | ||
| TAU (Ref) | 1 | 1 |
| NAV | 2.01 (1.21, 3.35) | 1.71 (1.02, 2.87) |
| Adjusted estimates | ||
| Study arm | ||
| TAU (Ref) | 1 | 1 |
| NAV | 2.15 (1.24, 3.74) | 1.95 (1.11, 3.46) |
| Age at index incarceration | 1.01 (0.99, 1.04) | 1.03 (0.99, 1.06) |
| Gender | ||
| Male (Ref) | 1 | 1 |
| Female | 0.81 (0.33, 1.97) | 0.87 (0.36, 2.10) |
| Transgender: male-to-female | 1.32 (0.43, 4.08) | 0.44 (0.12, 2.65) |
| Race/ethnicity | ||
| Non-Hispanic White (Ref) | 1 | 1 |
| Non-Hispanic Black | 0.64 (0.33, 1.24) | 0.75 (0.39, 1.45) |
| Latino | 0.35 (0.14, 0.91) | 0.28 (0.09, 0.82) |
| Other | 0.74 (0.30, 1.84) | 1.20 (0.50, 2.90) |
| Highest level of education | ||
| < high school | 1.07 (0.59, 1.95) | 1.38 (0.75, 2.49) |
| ≥ high school (Ref) | 1 | 1 |
| Relationship status | ||
| Single | 1.62 (0.81, 3.23) | 1.89 (0.91, 3.91) |
| Married or in a committed relationship | 1.18 (0.52, 2.68) | 1.95 (0.84, 4.53) |
| Separated or divorced (Ref) | 1 | 1 |
| Treatment while incarcerated | ||
| Not in treatment (Ref) | 1 | 1 |
| In substance dependency treatment | 4.06 (1.93, 8.53) | 2.52 (1.21, 5.23) |
| In mental health treatment | 1.15 (0.54, 2.45) | 2.08 (0.99, 4.39) |
Notes. CI = confidence interval; NAV = enhanced peer navigation group; OR = odds ratio; TAU = treatment as usual. Confidence limits from Wald test.
In the expanded model predicting linkage, those in the NAV arm remained about twice as likely to be linked to care (OR = 2.15; 95% CI = 1.24, 3.74) after we controlled for demographics and treatment in jail. Individuals who received treatment of substance use disorders were 4 times as likely to be linked to care upon release (OR = 4.06; 95% CI = 1.93, 8.53). Latinos were less likely to be linked to care upon release (OR = 0.35; 95% CI = 0.14, 0.91).
Results were similar in expanded models predicting engagement in care. Individuals in the NAV arm were almost twice as likely to be retained in care across the year of the project (OR = 1.95; 95% CI = 1.11, 3.46). Receipt of treatment of substance dependency in jail was associated with an approximate 2.5-fold increase in the likelihood of engagement in care across the year (OR = 2.52; 95% CI = 1.21, 5.23). Latinos were less likely to be engaged across the year (OR = 0.28; 95% CI = 0.09, 0.82).
DISCUSSION
Patient navigation benefits individuals leaving jail by supporting their engagement in HIV care for up to a year after release. Also, in this study, receipt of treatment for substance use disorders inside jail led to better HIV care outcomes when people returned to care in the community. A variety of studies and initiatives have aimed to facilitate the transition to care in the community among people living with HIV leaving correctional settings.15–18 In our study, intervention participants were able to maintain levels of HIV care engagement similar to individuals who were not exposed to incarceration.31 Regardless of these findings, viral suppression was not different across study groups.
There was an important difference by race/ethnicity with Latinos being less likely to link or be retained in care. This finding has implications for adapting an intervention to a specific population; it was beyond the scope of this study to hire navigators who spoke Spanish, and this was a limitation that should be addressed in future studies. Furthermore, we did not collect information on the legal status of Latino participants, and that could have affected engagement in care over time.
This intervention was also successful in reducing sex that risks HIV transmission among participants by approximately 10% compared with the standard of care, which was likely attributable to the counseling that was part of the Project START–inspired component of the intervention. The TAU was active for a shorter time following release and did not specifically provide sexual risk reduction counseling. The effects of any counseling that may have occurred in the TAU arm also may have dissipated over time. These findings support the use of START-like counseling strategies in jail settings, particularly when they can be sustained over time.24,32
Limitations
The study limitations include the reliance on self-report for some of our data. There is evidence that self-report is reliable in similar populations, however.33 Study participants were not blinded to the intervention condition they had been assigned to, which may have biased survey question responses or affected their likelihood of returning for study visits. In addition, the outcomes for this study were collected passively through medical record abstraction; however, medical record data were available for almost all participants and would not be expected to have differed in quality by study arm. Results from this study reflect the additional benefit of patient navigation over an extended period compared with a standard of care in this setting, which is already higher than in many jail systems. In settings where services are less optimal, navigation may have an even greater benefit.
Public Health Implications
Our findings suggest that patient navigation can offer critical support for HIV-infected individuals leaving jail and also reinforce the evidence that addressing comorbid conditions is key to increasing engagement in HIV care. Patient navigation offers a practical, feasible way to improve HIV care outcomes. Our findings, in conjunction with other evidence in the literature, support navigation as the standard of care for individuals returning to the community from jail.
ACKNOWLEDGMENTS
This research was supported by the National Institute on Drug Abuse grant R01DA027209.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
HUMAN PARTICIPANT PROTECTION
The study was approved by the University of California, San Francisco, institutional review board, and a certificate of confidentiality was secured from the federal Office of Human Research Protections.
REFERENCES
- 1.Carson EA, Golinelli D. BJS Bulletin. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2013. Prisoners in 2012: trends in admissions and release, 1991–2012. [Google Scholar]
- 2.Minton TD, Golinelli D. BJS Bulletin. Washington, DC: US Bureau of Justice Statistics; 2014. Jail inmates at midyear 2013—statistical tables. [Google Scholar]
- 3.Maruschak LM. BJS Bulletin. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2012. HIV in prisons, 2001–2010. [Google Scholar]
- 4.Spaulding A, Stephenson B, Macalino et al. Human immunodeficiency virus in correctional facilities: a review. Clin Infect Dis. 2002;35(3):305–312. doi: 10.1086/341418. [DOI] [PubMed] [Google Scholar]
- 5.Blankenship KM, Smoyer AB, Bray SJ, Mattocks K. Black–White disparities in HIV/AIDS: the role of drug policy and the corrections system. J Health Care Poor Underserved. 2005;16(4 suppl B):140–156. doi: 10.1353/hpu.2005.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White MC, Tulsky JP, Estes M et al. Health and health behaviors in HIV-infected jail inmates, 1999 and 2005. AIDS Patient Care STDS. 2008;22(3):221–231. doi: 10.1089/apc.2007.0043. [DOI] [PubMed] [Google Scholar]
- 7.Spaulding AC, Seals RM, Page MJ et al. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iroh PA, Mayo H, Nijhawan AE et al. The HIV care cascade before, during and after incarceration: a systematic review. Am J Public Health. 2015;105(7):e5–e16. doi: 10.2105/AJPH.2015.302635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baillargeon J, Giordano TP, Rich JD et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–857. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leukefeld CG, Hiller ML, Webster JM et al. A prospective examination of high-cost health services utilization among drug using prisoners reentering the community. J Behav Health Serv Res. 2006;33(1):73–85. doi: 10.1007/s11414-005-9006-y. [DOI] [PubMed] [Google Scholar]
- 11.Binswanger IA, Stern MF, Deyo RA et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen MS, Chen YQ, McCauley M et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–839. doi: 10.1056/NEJMoa1600693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011;53(5):469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer JP, Chen NE, Springer SA. HIV treatment in the criminal justice system: Critical knowledge and intervention gaps. AIDS Res Treat. 2011;2011:680617. doi: 10.1155/2011/680617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spaulding AC, Messina LC, Kim BI et al. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS Behav. 2013;17(suppl 2):S203–S211. doi: 10.1007/s10461-012-0341-8. [DOI] [PubMed] [Google Scholar]
- 16.Myers JJ, Barker TA, Devore BS et al. CDC/HRSA HIV/AIDS intervention, prevention, and continuity of care demonstration project for incarcerated individuals within correctional settings and the community: part II, implementation issues during years one and two. J Correct Health Care. 2003;9(4):487–510. [Google Scholar]
- 17.Draine J, Ahuja D, Altice FL et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. AIDS Care. 2011;23(3):366–377. doi: 10.1080/09540121.2010.507738. [DOI] [PubMed] [Google Scholar]
- 18.Peterson J, Cota M, Gray H et al. Technology use in linking criminal justice reentrants to HIV care in the community: a qualitative formative research study. J Health Commun. 2015;20(3):245–251. doi: 10.1080/10810730.2014.927036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kushel MB, Golfax G, Ragland K et al. Case management is associated with improved antiretroviral adherence and CD4+ cell counts in homeless and marginally housed individuals with HIV infection. Clin Infect Dis. 2006;43(2):234–242. doi: 10.1086/505212. [DOI] [PubMed] [Google Scholar]
- 20.Zaller ND, Holmes L, Dyl AC et al. Linkage to treatment and supportive services among HIV-positive ex-offenders in Project Bridge. J Health Care Poor Underserved. 2008;19(2):522–531. doi: 10.1353/hpu.0.0030. [DOI] [PubMed] [Google Scholar]
- 21.Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer. 2005;104(4):848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 22.Bradford JB, Coleman S, Cunningham W. HIV system navigation: an emerging model to improve HIV care and access. AIDS Patient Care STDS. 2007;21(suppl 1):S49–S58. doi: 10.1089/apc.2007.9987. [DOI] [PubMed] [Google Scholar]
- 23.San Francisco HIV Health Services. The San Francisco standards of HIV care. 2000. Available at: http://sfhivcare.com/hhs-resources/standards-of-care. Accessed June 18, 2017.
- 24.Wolitski RJ. The Project START study group. Relative efficacy of a multi-session sexual risk-reduction intervention for young men released from prison in 4 states. Am J Public Health. 2006;96(10):1854–1861. doi: 10.2105/AJPH.2004.056044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koester KA, Morewitz M, Pearson C et al. Patient navigation facilitates medical and social services engagement among HIV-infected individuals leaving jail and returning to the community. AIDS Patient Care STDS. 2014;28(2):82–90. doi: 10.1089/apc.2013.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ware JE, Kosinski M, Keller SD. How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. Boston, MA: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 27.Ware J, Jr, Kosinski M, Keller SD. 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Galdón MJ, Durá E, Andreu Y et al. Psychometric properties of the brief symptom inventory-18 in a Spanish breast cancer sample. J Psychosom Res. 2008;65(6):533–539. doi: 10.1016/j.jpsychores.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 29.Skinner HA. The drug abuse screening test. Addict Behav. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 30.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 31.Bradley H, Hall HI, Wolitski RJ et al. Vital Signs: HIV diagnosis, care, and treatment among persons living with HIV—United States, 2011. MMWR Morb Mortal Wkly Rep. 2014;63(47):1113–1117. [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Compendium of Evidence-Based HIV Prevention Interventions. Atlanta, GA: Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 33.Schofield P, Butler T, Hollis S et al. Are prisoners reliable survey respondents? A validation of self-reported traumatic brain injury (TBI) against hospital medical records. Brain Inj. 2011;25(1):74–82. doi: 10.3109/02699052.2010.531690. [DOI] [PubMed] [Google Scholar]