Abstract
Eruptive vellus hair cyst (EVHC) is a rare follicular developmental abnormality of the vellus hair follicles. They are usually seen in children, adolescents, or young adults and manifest as reddish-brown smooth papules most commonly involving the chest, limbs, and abdomen. An 18-year-old male presented with asymptomatic papules on the trunk and flexor aspect of both forearms for the past 2 years. There was no family history of similar lesions. His medical history was also not contributory. A clinical diagnosis of steatocystoma multiplex and chronic folliculitis was given, and a punch biopsy from the papule was performed and sent for histopathological examination. On microscopic examination, a final diagnosis of EVHC was rendered. The patient was advised topical treatment of retinoic acid cream (0.05%) for 6 months, and he is currently under follow-up period. Due to its rarity and resemblance to many similar entities, histopathological examination plays a major role in establishing a definite diagnosis and further proper management of the patient. We report this unusual case to generate awareness about this rarely diagnosed condition.
Key words: Eruptive vellus hair cyst, reddish-brown papules, steatocystoma multiplex
INTRODUCTION
Eruptive vellus hair cyst (EVHC) is a rare follicular developmental abnormality of the vellus hair follicles.[1] The term EVHC was first proposed by Esterly and Cols in 1977,[2,3] and its etiology is still unknown. They are most commonly seen in children, adolescents, or young adults; they could be sporadic or autosomal dominant and manifest as reddish-brown smooth papules of 1–4 mm diameter usually involving the chest, limbs, and abdomen. They are uncommon benign tumors of pilosebaceous unit, and in about 25% of cases, spontaneous resolution occurs.[4,5] Histologically, it is characterized by cystic spaces lined by stratified squamous epithelium composed of variable amounts of laminated keratin and multiple transversely and obliquely cut vellus hair. They have a predilection for middle or upper dermis. Histopathological diagnosis can be a challenge due to their relative rarity and because they are often clinically misdiagnosed. We hereby report an unusual case of EVHC in a young male presenting as asymptomatic papules on the trunk and flexor aspect of both forearms.
CASE REPORT
An 18-year-old male presented with multiple asymptomatic skin-colored and black-colored elevated lesions on the flexor aspect of both forearms and trunk for the past 2 years. There was no family history of similar lesions. The patient denied use of any cosmetic product or excessive sun exposure or exposure to chemicals or mechanical trauma before the eruptions. Physical examination revealed multiple discrete, reddish-brown-colored, 2–3 mm sized dome-shaped hyperpigmented papules [Figure 1]. There was no central puncta or umbilications present. Mucosa, hair, and nail examination was normal. General examination and all other routine investigations were normal. A clinical diagnosis of steatocystoma multiplex (SCM) and chronic folliculitis was given, and a punch biopsy from the papule was performed and sent for histopathological examination. On microscopic examination, a cyst lined by two to three layers of squamous epithelium was noted in the lower dermis [Figure 2]. The cyst cavity contained abundant laminated keratinous debris, and numerous vellus hair shafts were identified [Figure 3a and b]. On serial sections, there were no sebaceous glands noted adjacent to or within the cyst wall. Therefore, based on the above findings, a final diagnosis of EVHC was rendered. The patient was advised topical treatment of retinoic acid cream (0.05%) to be applied daily at night for 6 months, and he is currently under follow-up period.
Figure 1.

Multiple, 1–2-mm, hyperpigmented papules on the flexor aspect of forearm
Figure 2.
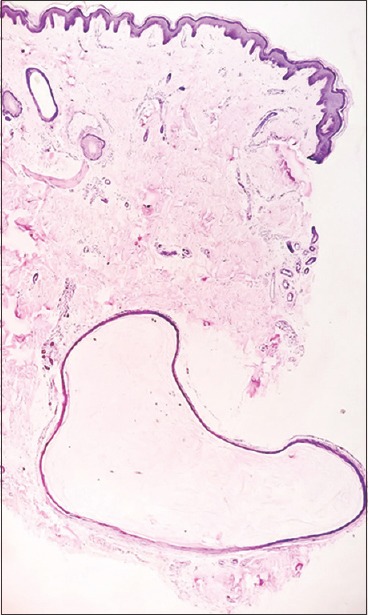
Acyst is seen in the lower dermis lined by flattened squamous epithelium(H and E, ×4)
Figure 3.
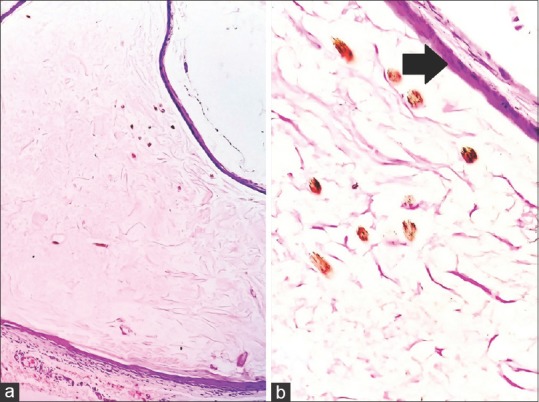
(a) Cyst cavity containing laminated keratinous material and multiple vellus hair shafts(H and E, ×10). (b) Cyst lining showing the presence of granular layer(arrow) and containing numerous vellus hairs and keratinous material(H and E, ×40)
DISCUSSION
EVHC may be inherited or acquired and may have an association with other genodermatoses, such as sebocystomatosis.[6] They may also represent hamartomatous follicular growth or probably due to occlusion of the infundibulum of vellus hair follicles with resultant cystic dilatation and retention of keratinous material and hairs, resulting in secondary atrophy of hair bulbs. The primary cause of obstruction is still unknown. They may also occur as an acquired hamartoma. Furthermore, mutations in the gene that encodes keratin 17 (K17) have been described.[7]
This condition is characterized by multiple, small normochromic or hyperpigmented, dome-shaped papules, soft to firm in consistency, ranging in size from 1 to 5 mm in diameter. They may be topped with central puncta, umbilicated or a hyperkeratotic crust. Common sites of involvement are chest and extremities, rarely abdomen, neck, axillae, face, and groin.[8,9] In our case, hyperpigmented papules were present on the flexor aspect of both forearms, and few of them were located on the chest and back. The usual age of onset is between 17 and 24 years, but they can occur at any age.
Histologically, EVHCs are characteristically located in the mid-dermis and/or upper-dermis as opposed to our case where the cyst was located in the lower dermis. The lining epithelium of the cyst wall resembles the infundibular or isthmic portion of the hair follicle and contains two to three layers of stratified squamous epithelium with focal areas of granular layer as was seen in our case. The cyst cavity contains variable amount of laminated keratin and numerous transversally and obliquely cut vellus hairs.[10] The cyst wall may be in continuity with an atrophied hair follicle or arrector pili muscle. Usually, no sebaceous glands are present within the cyst wall. The cyst may be surrounded by a granulomatous inflammation,[11] leading to partial destruction of the cyst wall.
The differential diagnosis of pilosebaceous cysts includes infundibular cysts, SCM, and EVHCs. All three occur as asymptomatic papules or nodules affecting the anterior chest wall most commonly. Infundibular cysts do not contain sebaceous glands or vellus hairs. The cyst of SCM arises in the sebaceous duct and has an eosinophilic hyaline lining to the cyst wall where there is an absence of granular layer. Steatocystoma also contains sebaceous glands or sebocytes arising within the cyst wall which was not present in this case.[12] Some authors have quoted that EVHC and SCM are variants of same disorders because both lesions have been reported in the same patient as “hybrid cysts”[13] while others believe that they are distinct entities based on different histologic patterns. Immunohistochemical staining with K10 and K17 revealed that EVHC and SCM were two distinct lesions.[7] SCM expresses both K10 and K17 while EVHC expresses only K17.
Another unique vellus hair dermatoses known as congenital vellus hamartoma first described by Headington in 1976[14] usually manifest as small papules and nodules on head and neck and are composed of abundant tightly packed well-formed vellus follicles. Clinically, it resembles vellus hair cyst; however, histopathologically, there is no cyst formation.[15]
Other clinical differentials include comedones, keratosis pilaris, syringoma, milium, and molluscum contagiosum.[16,17] EVHCs are often clinically misdiagnosed due to its resemblance to various mimicking lesions as it occurred in our case. Hence, histopathological examination is mandatory to differentiate these lesions from EVHC.
Spontaneous remission occurs in about 25% of the cases due to inflammatory destruction and transepidermal elimination. Although benign, this condition is difficult to treat with no response to oral isotretinoin.[12,16] Currently, there is no standard treatment for EVHC. Improvement with dermabrasion, erbium:YAG or carbon dioxide laser vaporization, and needle incision have been cited in the literature, but a large number hinders complete resolution.
It is believed that EVHC is more common than it actually appears due to its scarcity of literature[18] and paucity of reports from India indicating that it has been underdiagnosed and underreported. We could find only four reports until now from India.[10,19,20,21]
CONCLUSION
Due to its rarity and resemblance to many similar entities, histopathological examination plays a major role in establishing a definite diagnosis and further proper management of the patient. We report this case to generate awareness about this rarely diagnosed condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Reep MD, Robson KJ. Eruptive vellus hair cysts presenting as multiple periorbital papules in a 13-year-old boy. Pediatr Dermatol. 2002;19:26–7. doi: 10.1046/j.1525-1470.2002.00009.x. [DOI] [PubMed] [Google Scholar]
- 2.Esterly NB, Fretzin DF, Pinkus H. Eruptive vellus hair cysts. Arch Dermatol. 1977;113:500–3. [PubMed] [Google Scholar]
- 3.Baums K, Blume-Peytavi U, Dippel E, Goerdt S, Orfanos CE. Guess what! Eruptive vellus hair cysts. Eur J Dermatol. 2000;10:487–9. [PubMed] [Google Scholar]
- 4.Bovenmyer DA. Eruptive vellus hair cysts. Arch Dermatol. 1979;115:338–9. [PubMed] [Google Scholar]
- 5.Sina B, Burnett JW. Eruptive vellus hair cysts. Cutis. 1984;33:503–4. [PubMed] [Google Scholar]
- 6.Zaharia D, Kanitakis J. Eruptive vellus hair cysts: Report of a new case with immunohistochemical study and literature review. Dermatology. 2012;224:15–9. doi: 10.1159/000337209. [DOI] [PubMed] [Google Scholar]
- 7.Tomková H, Fujimoto W, Arata J. Expression of keratins (K10 and K17) in steatocystoma multiplex, eruptive vellus hair cysts, and epidermoid and trichilemmal cysts. Am J Dermatopathol. 1997;19:250–3. doi: 10.1097/00000372-199706000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Kwon KS, Lee HT, Jang HS, Chung TA, Oh CK. A case of generalized eruptive vellus hair cysts. J Dermatol. 1997;24:556–7. doi: 10.1111/j.1346-8138.1997.tb02842.x. [DOI] [PubMed] [Google Scholar]
- 9.Hong SD, Frieden IJ. Diagnosing eruptive vellus hair cysts. Pediatr Dermatol. 2001;18:258–9. doi: 10.1046/j.1525-1470.2001.018003258.x. [DOI] [PubMed] [Google Scholar]
- 10.Rao R, Balachandran C. Asymptomatic papular lesions on the trunk. Indian J Dermatol Venereol Leprol. 2009;75:217–9. doi: 10.4103/0378-6323.48687. [DOI] [PubMed] [Google Scholar]
- 11.Haritha K, Parthasaradhi A, Jalu J. Eruptive vellus hair cyst. Indian J Paediatr Dermatol. 2016;17:76–8. [Google Scholar]
- 12.Karen JK, Heller M, Wee SA, Mikkilineni R. Eruptive vellus hair cysts. Dermatol Online J. 2007;13:14. [PubMed] [Google Scholar]
- 13.Kiene P, Hauschild A, Christophers E. Eruptive vellus hair cysts and steatocystoma multiplex. Variants of one entity? Br J Dermatol. 1996;134:365–7. [PubMed] [Google Scholar]
- 14.Hendricks WM, Taub S, Hu CH. Congenital vellus hamartoma. Cutis. 1981;27:67–8. [PubMed] [Google Scholar]
- 15.Lai HH, Lee WR, Lai CC, Hu CH. Eruptive vellus hair cysts – Report of a facial Variant. Dermatol Sinca. 1998;16:191–5. [Google Scholar]
- 16.Karadag AS, Cakir E, Pelitli A. Eruptive vellus hair cysts: An alternative diagnosing method. Indian J Dermatol Venereol Leprol. 2009;75:537–8. doi: 10.4103/0378-6323.55421. [DOI] [PubMed] [Google Scholar]
- 17.Yamada A, Saga K, Jimbow K. Acquired multiple pilosebaceous cysts on the face having the histopathological features of steatocystoma multiplex and eruptive vellus hair cysts. Int J Dermatol. 2005;44:861–3. doi: 10.1111/j.1365-4632.2005.02227.x. [DOI] [PubMed] [Google Scholar]
- 18.Torchia D, Vega J, Schachner LA. Eruptive vellus hair cysts: A systematic review. Am J Clin Dermatol. 2012;13:19–28. doi: 10.2165/11589050-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Saha A, Das NK, Gharami RC, Chowdhury SN, Datta PK. A clinico-histopathological study of appendageal skin tumors, affecting head and neck region in patients attending the dermatology opd of a tertiary care centre in Eastern India. Indian J Dermatol. 2011;56:33–6. doi: 10.4103/0019-5154.77548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh A, Ponnaiya J. Eruptive vellus hair cysts: A case report. Indian J Pathol Microbiol. 1993;36:289–91. [PubMed] [Google Scholar]
- 21.Bhushan P, Singh A. Facial variant of eruptive vellus hair cyst. Indian J Dermatol Venereol Leprol. 2014;80:96. doi: 10.4103/0378-6323.125513. [DOI] [PubMed] [Google Scholar]


