Abstract
Background:
To assess and compare the effectiveness of two surgical procedures (Beagle's technique and modified Beagle's technique) for the reconstruction of the lost interproximal dental papilla.
Materials and Methods:
Twenty sites were selected based on the selection criteria which included patients within the age group of 20–50 years and the presence of Class I and Class II recession of the papilla in the maxillary anterior region. They were divided randomly into Group A and Group B. Group A sites were treated with modified Beagle's technique, whereas Group B sites were treated by the Beagle's technique. The patients were recalled at 1 week, 1 month, 3 months, and 6 months postsurgery. Parameters including classification of loss of papilla height (Nordland and Tarnow), change in vertical dimension, mesiodistal dimension and area of the papillary defect, and radiographic parameters (papilla height and bone crest-root apex distance) were recorded preoperatively and postoperatively.
Results:
At 6-month postsurgery, there was a statistically significant reduction in vertical dimension, mesiodistal dimension, and area of the papilla defect in Group A compared to Group B. At 6-month postsurgery, there was an increase in the height of the papilla in Group A, whereas there was a decrease in the height of the papilla in Group B. At 6-month postsurgery too, there was a reduction in the mean bone crest-root apex distance in both groups.
Conclusion:
Thus, the modified Beagle's technique is an easy and effective technique when compared to the Beagle's surgical technique for papilla reconstruction.
Keywords: Beagle's technique, modified Beagle's technique, papilla height
INTRODUCTION
Dental esthetics has become a great concern, for both dental practitioners and patients, in addition to maintaining dental and periodontal health. The contour of the interdental tissues and the color and texture of keratinized tissues play a role in esthetics with the presence of interproximal papilla between the maxillary anterior teeth being the key esthetic component.[1]
Hence, one of the major esthetic challenges in periodontal plastic surgery is the ability to regenerate the lost papilla in the maxillary anterior segment.[1]
Black triangle or an open gingival embrasure occurs as a result of a deficiency or loss of papilla beneath the contact point. Numerous risk factors (mainly periodontal disease or as a consequence of periodontal surgery) lead to the development of open gingival embrasures or black triangles.[2]
Several surgical and nonsurgical techniques have been used to treat and restore the missing interdental papilla. If the loss of papilla is related to soft-tissue damage only, reconstructive techniques are able to restore it completely. If the loss of the interdental papilla is due to severe periodontal disease, with interproximal bone resorption, complete reconstruction is generally not achieved. The surgical techniques used for papilla reconstruction include several approaches.[3] However, the reconstruction of the lost interdental papilla has been elusive. The previous attempts were made to augment the interdental papilla using displaced flaps, connective tissue grafts, and repeated inflammatory stimulation, with diverse results.[4] This could be due to a number of factors which affect the presence or absence of the papilla. These factors are the availability of underlying osseous support, periodontal biotype, tooth morphology, and contact point between adjacent teeth.[5] The iconic study by Tarnow et al. determined that the distance from the base of the contact area to the crest of bone could be correlated with the presence or absence of the interproximal papilla.[6] The 5-mm rule given by Tarnow et al. states that when the distance from the contact point to the interproximal osseous crest is 5 mm or less, there is complete fill of the gingival embrasures with an interdental papilla. For every 1 mm above 5 mm, the chance of complete fill is progressively reduced by 50%.[6]
Hence, the present study was undertaken to assess and compare the effectiveness of two surgical procedures (Beagle's technique and modified Beagle's technique) for the reconstruction of the lost interproximal dental papilla to solve the patient's problem of an unesthetic black triangle between the maxillary anterior teeth.
MATERIALS AND METHODS
This study was approved by the Ethical Committee of Bharati Vidyapeeth Deemed University Dental College and Hospital, Pune. Patients presenting with black triangle in the anterior region were selected from the Outpatient Department of Periodontology, fulfilling the inclusion and exclusion criteria. The analysis of the radiographic parameters pertinent to this study was carried out in the Department of Oral Radiology. Twenty sites were selected (the sample size was determined in consultation with the statistician) from these patients based on the selection criteria which included; patients within age group of 20–50 years, presence of Class I and Class II recession of the papilla in the maxillary anterior region,[7] patients having adequate zone of attached gingiva at the selected region, and no evidence of periodontal pockets at the selected site and patients with acceptable oral hygiene (i.e., evidence of minimal or no plaque and the absence of inflammation at the gingival margin).
Patients with any kind of systemic diseases, drug usage, allergy, etc., which can alter the healing process, patients with harmful oral habits, patients with high frenum attachment, patients with interdental diastema, patients with excessive gingival pigmentation (obtaining a pedicle graft from hyperpigmented area of attached gingiva would lead to a hyperpigmented interdental papilla; which would lead to an unesthetic appearance), and smokers were excluded from this study.
A detailed case history was recorded. Intraoral examination was carried out under standard conditions of light using a mouth mirror and a UNC 15 periodontal probe. Phase I therapy was carried out for all the patients, to eliminate the etiological factors. The patients were recalled for the revaluation, 4 weeks after the Phase I therapy. The following parameters were recorded at the selected sites as per the proforma, as baseline measurements:
Classification for the loss of papilla height (Nordland and Tarnow)
Photographic evaluation
Radiographic Evaluation.
Photographic evaluation
Clinical photographs of the selected site (black triangle) were taken. These photographs were standardized, by setting a grid over the camera screen, while clicking them. The photographs are taken such that the black triangle, adjacent teeth, and the papilla between them is clearly visible. The zoom of the photographs was standardized to 25%. These photographs were then analyzed using software, “meazure.” Using this software, the following measurements were calculated:
Vertical papillary defect height
Mesiodistal papillary defect width
Total papillary defect area.
At the end of 6-month postsurgery, the changes in the abovementioned dimensions were then calculated.
Radiographic evaluation
For measurement of the length of the interdental papilla, a radiopaque material consisting of calcium hydroxide and iodoform (Metapex) was placed at the tip of the papilla with a probe. The length of the papilla was calculated by measuring the distance from the alveolar bone crest to the radiopaque mark at the tip of the papilla (BC-PT) [Figure 1].[8] The distance from the alveolar bone crest to the root apex (BC-RA) was measured and used as a reference to evaluate the change, if any, in the level of alveolar bone crest, postsurgery. The measurements were repeated at 3 months and 6 months postsurgery, (with the preoperative bite record used as a guide for the postoperative placement of the XCP device), to determine the changes in the height of the papilla (BC-PT) and the level of the alveolar crest (BC-RA) [Figure 2].
Figure 1.

Radiopaque material placed at the papilla tip
Figure 2.
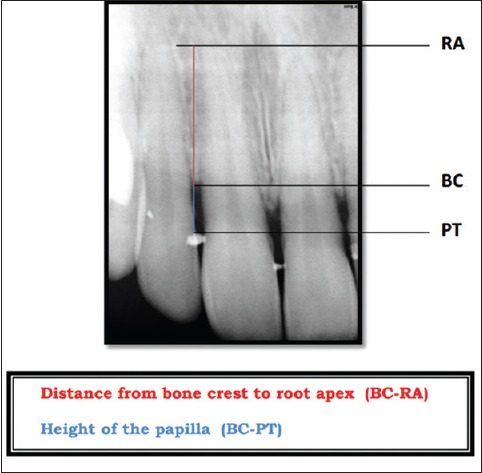
Digital radiograph showing radiopaque material at the papilla tip
The sites were then divided randomly into two groups (Group A and Group B). Group A sites were treated with modified Beagle's technique, whereas Group B sites were treated by the Beagle's technique. Either of the surgical technique was randomly assigned to each site by computer generation.
Surgical procedure
The surgical procedure was performed using routine local anesthetic (2% xylocaine with epinephrine 1: 200,000). In the modified Beagle's technique,[9] incisions were given with an ophthalmic crescent knife, at the adjacent line angles of the interdental papilla, such that the length is more than the length of the black triangle space to be reconstructed [Figures 3 and 4]. These vertical incisions were connected by a horizontal incision at the apical end. A partial thickness pedicle flap was elevated. The papillary unit was carefully dissected from the teeth and the interdental area so that the papillary unit can be mobilized freely. The pedicle graft is then advanced coronally to completely obliterate the black triangle space [Figure 5]. The flap is then sutured coronally to the adjacent tissues, with a 6-0 silk suture. The patients were recalled at 1 week, 1 month, 3 months, and 6 months postsurgery [Figure 6].
Figure 3.

Modified Beagle's technique (Site at baseline)
Figure 4.

Modified Beagle's Technique – Incision on labial aspect
Figure 5.

Modified Beagle's technique – Suturing
Figure 6.

Modified Beagle's technique – 6-month follow-up
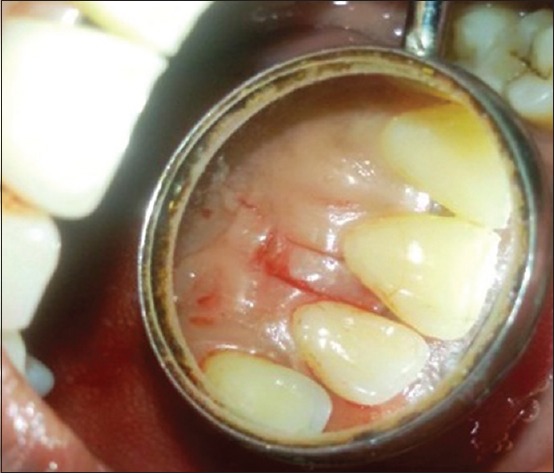
In the Beagle's technique,[10] a partial thickness incision was made along the line angles of adjacent teeth on the palatal aspect with an ophthalmic crescent knife [Figures 7 and 8]. The sulcular incisions were given in the interdental region to separate the papillary unit. The partial thickness flap was elevated to the labial aspect. The elongated papilla was folded on itself, to approximate the connective tissue sides [Figure 9]. A 6-0 silk suture was used to bind the laminated papilla together and suspend it between the adjacent teeth [Figure 10]. All patients were prescribed a course of antibiotics (Capsule Amoxicillin 500 mg, thrice a day for 5 days) and analgesic (Tablet Diclofenac sodium 50 mg + Paracetamol 500 mg, twice a day for 3 days). Posttreatment instructions were given. All the surgeries were performed by the same individual.
Figure 7.

Beagle's technique (Site at baseline)
Figure 8.
Beagle's technique – Incision on palatal aspect
Figure 9.

Beagle's technique – Reflection of partial thickness pedicle graft from palatal to the labial aspect
Figure 10.

Beagle's technique – Suturing
The patients were recalled on the next day of surgery and for suture removal after 1 week. Oral hygiene was reinstituted, and oral hygiene instructions were repeated. The patients were recalled at 1 week, 1 month, 3 months, and 6 months postsurgery [Figure 11].
Figure 11.

Beagle's technique – 6-month follow-up
The data thus collected were subjected to statistical analysis. Paired t-test was used for intragroup comparison, whereas independent sample t-test was used for intergroup comparison.
RESULTS
It was observed from the results that there was statistically significant improvement in the height of the interdental papilla (according to the Nordland and Tarnow classification, 1988), in Group A than in Group B [Graph 1].
Graph 1.
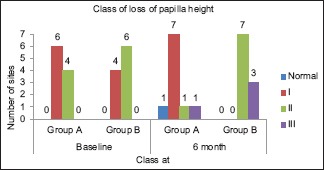
Graph showing comparison of change in papilla height according to the Nordland and Tarnow classification
At 6-month postsurgery, there was a reduction in the mean vertical dimension of the papillary defect in Group A, whereas there was a slight increase in the mean vertical dimension of the papillary defect in Group B and the results were statistically significant (P < 0.001) [Table 1].
Table 1.
Comparison of the vertical and mesiodistal dimension of the papillary defect
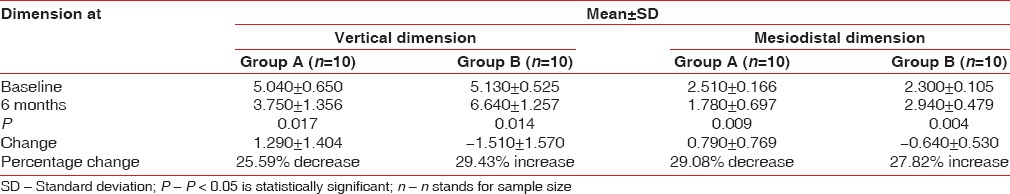
At 6-month postsurgery, there was a reduction in the mean mesiodistal dimension of the papillary defect in Group A, whereas there was a slight increase in the mean mesiodistal dimension of the papillary defect in Group B, and the results were statistically significant (P < 0.001) [Table 1].
At 6-month postsurgery, there was a reduction in the mean area of the papillary defect in Group A (i.e., an increase in the bulk of the papilla), whereas there was a slight increase in the mean area of the papillary defect in Group B (i.e., shrinkage of papilla). Observations revealed that the mean value of total area of the papillary defect in Group B at 6-month postsurgery was greater than that at baseline indicating that there is more shrinkage in the interdental tissues at 6-month postsurgery in Group B than in Group A [Table 2 and Graph 2].
Table 2.
Comparison of the total area of the papillary defect
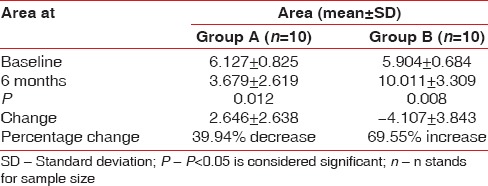
Graph 2.
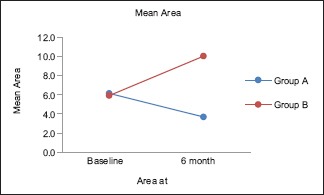
Graph showing the comparison of the total area of the papillary defect in Group A and Group B at baseline and 6 months postsurgery
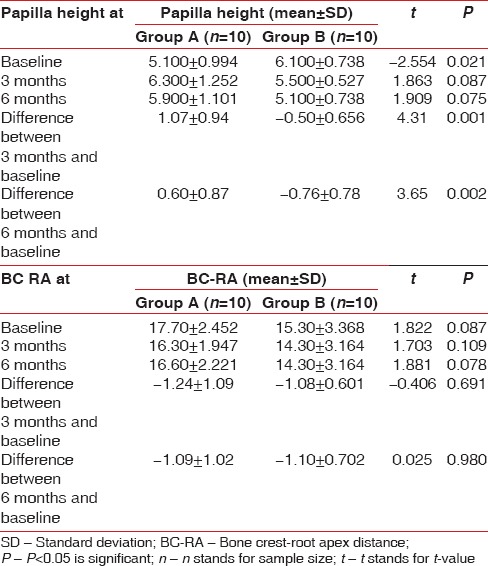
Observations showed that there was an increase in the mean height of the papilla in Group A at 3 months and 6 months postsurgery when compared with baseline. It is observed that there is a reduction in the height of the papilla in Group B at 3 months and further reduction at 6-month postsurgery in Group B at 3 months and further reduction at 6 month postsurgery. When the change in the mean papilla height was compared between Group A and Group B, the difference was statistically significant at both 3 and 6 months post-surgery, as P-value <0.05 (increase in papilla height in Group A, while reduction in Group B) [Table 3 and Graph 3].
Table 3.
Intergroup comparison of papilla height and bone crest-root apex distance
Graph 3.
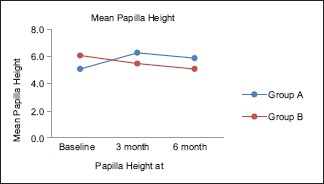
Graph showing the comparison of the papilla height in Group A and Group B at baseline, 3 months and 6 months postsurgery
It is observed that the BC-RA distance reduced at 3 and 6 months postsurgery indicating that there was slight crestal bone loss postsurgery [Table 3].
DISCUSSION
The observations made from photographic evaluation revealed that there was a statistically significant improvement (reduction) in the mean vertical dimension and mesiodistal dimension of the papillary defect in Group A as compared to Group B (where there was an increase). There was a statistically significant improvement (reduction) in the total area of the papillary defect in Group A as compared to Group B (where there was an increase), indicating that there is more shrinkage in the interdental tissues with Group B. Thus, there was an increase in height, width, and area of the papilla with Group A at 6 months. Similar results were observed by Beagle in 1992.[10] He had reported that his procedure (Beagle's technique) produced a much improved cosmetic situation, which remained stable over the observed 18-month period, with slight shrinkage.
Similar study was conducted by Nayak, wherein increase in the contour of interdental tissues in 22.73% cases was observed at 3-month postsurgery.[11]
The results obtained in our study are similar to the observations by Sawai and Kohad,[9] who used a modification of the original Beagle's technique to cover the open gingival embrasures. A similar technique was utilized in this study. They had observed that when compared with the preoperative contour of the interdental papilla there was statistically significant increase in contour at 24 weeks postoperatively. The contour of the interdental papilla increased 1 week postoperatively in 66.6% cases but then showed slight gingival shrinkage. The slight shrinkage of the interdental papilla at 6-month postsurgery, maybe because of the following reasons:
Grupe and Warren documented that any form of pedicle grafting is much more predictable if a proper donor tissue is found adjacent to the recipient site, as abundant blood supply from the base of the pedicle can be obtained for the predictable “take” of the graft. As the interdental space is narrow, the movement of the gingival tissue in a pedicle-like manner provides a small surface area in terms of blood supply to the donor tissue. This increases the chances of sloughing of the flap due to inadequate blood supply to form the papilla.[12] Another reason for the shrinkage of the interdental papilla could be the presence of dead space between the coronally displaced flap and underlying tissues in the embrasure area.[13]
Radiographic evaluation revealed that, at 3-month postsurgery, there was an increase in the height of the papilla in Group A, whereas there was a slight decrease in the height of the papilla in Group B. At 6-month postsurgery, there was an increase in the height of the papilla in Group A, whereas there was a decrease in the height of the papilla in Group B.
At 3-month postsurgery, there was a reduction in the BC-RA distance in Group A as well as in Group B. At 6-month postsurgery too, there was a reduction in the mean BC-RA distance in both groups. When the mean BC-RA distance was compared at 6-month postsurgery in both the groups, the results were statistically insignificant (P > 0.05). However, the results cannot be compared directly with other studies, as the majority of them are case reports and similar parameters were not included in other studies.
Thus, the modified Beagle's technique is an easy and effective technique when compared to the Beagle's surgical technique for papilla reconstruction. However, if bone grafting techniques or connective tissue techniques are used in conjunction with this surgical technique, there may be increased chances of obtaining better results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shruthi S, Gujjari SK, Mallya KP. Comparison of two surgical techniques for the reconstruction of interdental papilla. J Interdiscip Dent. 2015;5:17–22. [Google Scholar]
- 2.Babu KB, Madhu Babu DS, Dodani K, Sekhar, Leela, Reddy NR. Reconstruction of the interdental papillae using an interdisciplinary approach following orthodontic treatment: A case report. Int J Contemp Dent. 2011;2:34–7. [Google Scholar]
- 3.Deepalakshmi D, Ahathya RS, Raja S, Kumar A. Surgical reconstruction of lost interdental papilla: A case report. Perio. 2007;4:229–34. [Google Scholar]
- 4.Carranza N, Zogbi C. Reconstruction of the interdental papilla with an underlying subepithelial connective tissue graft: Technical considerations and case reports. Int J Periodontics Restorative Dent. 2011;31:e45–50. [PubMed] [Google Scholar]
- 5.Singh VP, Uppoor AS, Nayak DG, Shah D. Black triangle dilemma and its management in esthetic dentistry. Dent Res J (Isfahan) 2013;10:296–301. [PMC free article] [PubMed] [Google Scholar]
- 6.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–6. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 7.Nordland WP, Tarnow DP. A classification system for loss of papillary height. J Periodontol. 1998;69:1124–6. doi: 10.1902/jop.1998.69.10.1124. [DOI] [PubMed] [Google Scholar]
- 8.Lee DW, Kim CK, Park KH, Cho KS, Moon IS. Non-invasive method to measure the length of soft tissue from the top of the papilla to the crestal bone. J Periodontol. 2005;76:1311–4. doi: 10.1902/jop.2005.76.8.1311. [DOI] [PubMed] [Google Scholar]
- 9.Sawai ML, Kohad RM. An evaluation of a periodontal plastic surgical procedure for the reconstruction of interdental papillae in maxillary anterior region: A clinical study. J Indian Soc Periodontol. 2012;16:533–8. doi: 10.4103/0972-124X.106897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beagle JR. Surgical reconstruction of the interdental papilla: Case report. Int J Periodontics Restorative Dent. 1992;12:145–51. [PubMed] [Google Scholar]
- 11.Nayak S. Clinical evaluation of a surgical procedure for the reconstruction of the interdental papillae, as a treatment modality for unesthetic open embrasure in the maxillary anterior region – A pilot study. Dissertation Submitted to University of Bombay [Google Scholar]
- 12.Grupe HE, Warren RF. Repair of gingival defects by a sliding flap operation. J Periodontol. 1957;27:92. [Google Scholar]
- 13.de Waal H, Kon S, Ruben MP. The laterally positioned flap. Dent Clin North Am. 1988;32:267–85. [PubMed] [Google Scholar]


