Abstract
Pyogenic granuloma (PG) is a nonneoplastic, tumor-like growth commonly seen in the oral mucosa or skin. Although nonpathological, its existence might lead to complications such as secondary infections or diastema formation. Hence, surgical removal of the growth seems mandatory. Histopathologic and radiographic evaluation is essential for accurate diagnosis and to rule out malignancy. A 28-year-old systemically healthy female patient reported with a swelling which involved the interdental space of maxillary left central and lateral incisors. The lesion initially developed as a “pimple-like” swelling and gradually increased in size over 2 years. It was managed in a novel method by reflecting a papilla preservation flap, excising the lesion from inside the flap till healthy tissue was visible, and then exposing to diode laser to prevent recurrence. Subsequent histopathologic examination confirmed the diagnosis of PG. This novel, less invasive esthetic procedure employed a papilla preservation flap and laser irradiation technique. This simple modification not only helped in healing by primary intention and producing a good esthetic outcome but also showed no recurrence till date.
Keywords: Diode laser, papilla preservation flap, pyogenic granuloma, recurrence
BACKGROUND
Pyogenic granuloma (PG) is nonneoplastic, tumor-like growth seen on oral mucosa or skin.[1] Gingiva is the most common site of occurrence (75%) compared to other oral locations.[2] Treatment usually involves its excision.
In this article, we report a case of PG of gingiva in the upper anterior region of the oral cavity in a female patient. Main focus of the article is the treatment aspect, which was carried out in a unique way to meet the esthetic demands and avoid complications.
CASE REPORT
A 28-year-old systemically healthy female patient reported to our department with a complaint of swelling in the upper front gum region for the past 2 years. She gave a history of similar growth in the same region that started during her third trimester of pregnancy, which was excised 6 months after delivery. Eight months later, she noticed a pimple-like swelling in the interdental area of the teeth #21and #22, which gradually increased to the present size. Although painless, the growth was associated with bleeding while brushing and chewing. On extraoral examination, the upper lip over the gingival swelling appeared swollen. Intraoral examination revealed a solitary, sessile, ovoid growth [Figure 1] measuring 1.5 cm × 2.0 cm in the interdental area of aforementioned teeth, extending mesiodistally from the midbuccal aspect of #21 to distobuccal aspect of #22 and apicocoronally from the mucogingival junction to the tip of the papilla. Its surface was smooth with well-defined extent. It was noncompressible, nonfluctuant, erythematous, and semifirm in consistency with sessile base. There was a diastema of about 4 mm between these teeth, which, according to the patient, had been present since their eruption. Subgingival calculus and plaque were present, and gingival margins were erythematous, which bled upon probing. There was neither a periodontal pocket nor mobility of the associated teeth. Periapical radiograph revealed no bone involvement. Based on the clinical and radiographic presentation, it was provisionally diagnosed as PG. After obtaining patient's consent, necessary blood investigations were performed and thorough scaling was done. This resulted in resolution of the inflammation, and the case was scheduled for the surgical treatment by a novel approach.
Figure 1.

Preoperative picture
Case management
A conventional excision technique would have exposed a wide area of bone leading to secondary, painful healing with increased soft tissue and bone loss. Hence, a papilla preservation flap was employed, where a full-thickness flap, including the growth, was reflected buccally till the mucogingival junction [Figure 2]. Granulation tissue was removed from the underside of the flap; fibrous and pathologic appearing tissue was excised and removed till the normal tissue became visible [Figure 3]. The adjacent bone appeared clinically normal and was not involved in the surgery. The excised tissue was preserved in 10% formalin, for histopathologic examination. Later, the underside of the flap, as well as the bone surface, was irradiated with diode laser (K-LASER®, wavelength: 970 nanometers, power output: 3.5 joules) in a focused, pulsed, contact mode for three cycles of 30 s each, to remove any possible remnants of PG and prevent its recurrence [Figure 4]. The site was irrigated with saline, and the charred tissue was removed using a curette. The flap was repositioned and secured with silk sutures [Figure 5]. The patient was instructed about postsurgical care and medication prescribed. Suture removal was scheduled on the seventh day.
Figure 2.
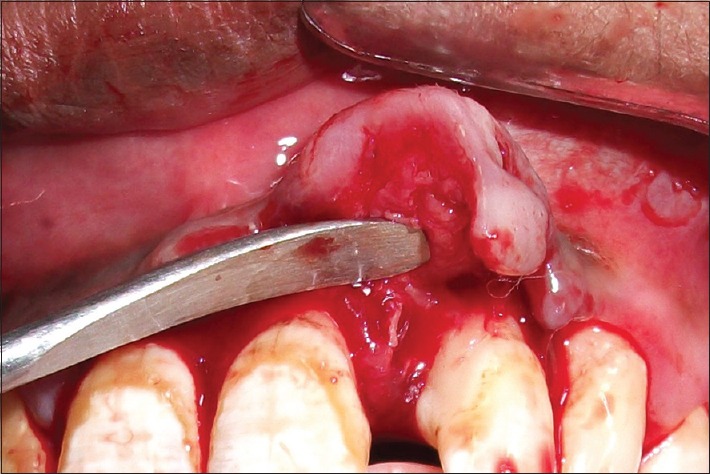
Reflection through papilla preservation approach
Figure 3.
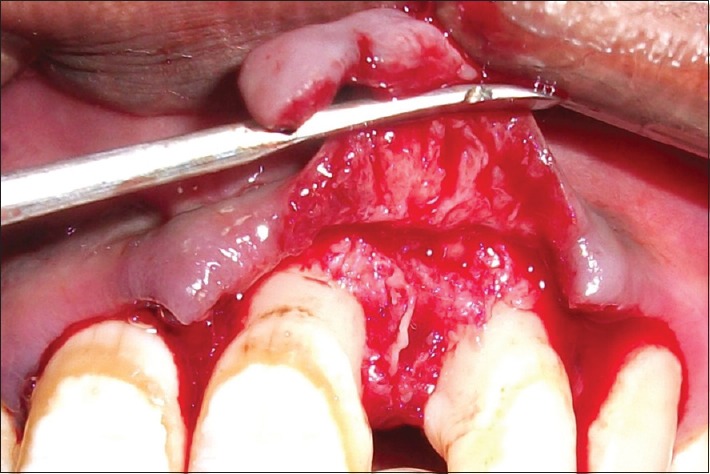
Tissue excised from undersurface of the flap
Figure 4.
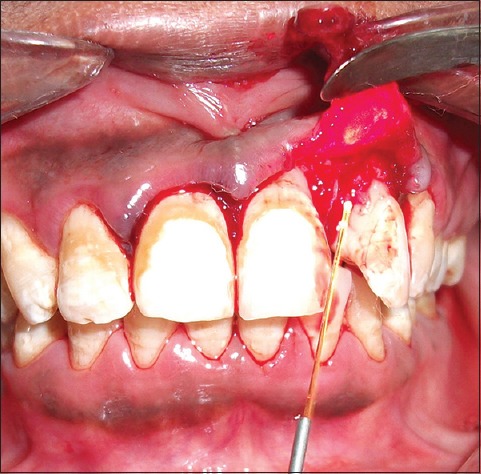
Soft tissue and bone irradiated with diode laser
Figure 5.

Postsuturing
Histopathology report confirmed the diagnosis of PG. It showed stratified squamous parakeratinized epithelium of varying thickness overlying a connective tissue stroma. The latter was mature, vascular, and fibrous. Numerous blood vessels of varying sizes were evident. Chronic inflammatory cells such as lymphocytes and plasma cells were also seen.
Clinical outcomes
On the day of suture removal, slight edema was noticed at the operated site [Figure 6]. At 3-month follow-up, soft tissue healing appeared complete, leaving no traces of the lesion [Figure 7]. The patient was followed up for 18 months, and no recurrence was reported [Figure 8].
Figure 6.

One-week postoperative picture
Figure 7.

Three-month postoperative picture
Figure 8.

Eighteen-month postoperative picture
DISCUSSION
In this case, PG presented itself in its most common location, i.e., maxillary anterior facial interdental, marginal and attached gingiva in a female patient in the third decade of her life. Various etiological factors have been described in literature by investigators. In the present case, hormonal factors could have played role in the development of PG during her third trimester of pregnancy, further exaggerated by chronic local irritation of calculus and plaque and constant irritation from the upper lip.
Many treatment procedures have been documented in literature with excision and removal of causative agents, being the mainstay. Excision up to periosteum[2] followed by scaling and root planing of the adjacent teeth is the usual treatment but involves risk of bone exposure of large area, bleeding, pain, bone loss and might result in unesthetic appearance in the anterior region. Other treatment options include excision using lasers,[3,4,5] cryosurgery,[6] or electrodesiccation.[7] These techniques would also result in large areas healing by secondary intention and limitations similar to excision. Injections of absolute alcohol,[8] sodium tetradecyl sulfate sclerotherapy,[8] and intralesional corticosteroid injections[9] could have been tried, which reduce the scar formation and other limitations but require multiple sittings and do not allow histopathologic examination. Recently, connective tissue grafting was tried after excision to prevent scar formation, albeit holds the disadvantage of second surgical site.[10]
Hence, a simple modification was tried by raising papilla preservation flap, including the growth in buccal flap and sectioning the pathologic tissue from underside of flap. This led to an esthetic, less invasive procedure with primary healing, reduced pain, and no bone exposure. Recurrence in PG cases is seen in up to 16%, attributable to incomplete elimination of etiologic factors, incomplete excision, or reinjury to the site.[11] To remove any possible remnants, thereby to prevent recurrence, a careful and thorough removal of the lesion till the extent of normal appearing tissue was done surgically, followed by laser irradiation. One and a half year follow-up showed no recurrence while producing an excellent result, both esthetically and functionally.
CONCLUSION
The use of a diode laser adjunctive to conventional surgical procedure to excise the lesion resulted in preservation of esthetics and lowered the chance of its recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initial will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hullihen SP. Case of aneurism by anastomosis of superior maxillae. Am J Dent Sci. 1844;4:160–2. [PMC free article] [PubMed] [Google Scholar]
- 2.Neville BW, Damm DD, Allen CM, Bouquot JE. Soft tissue tumors. In: Angela CC, Damm DD, Neville BW, Allen CM, Bouquot J, editors. Textbook of Oral and Maxillofacial Pathology. 3rd ed. Philadelphia: Saunders; 2009. pp. 451–2. [Google Scholar]
- 3.Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci. 2006;48:167–75. doi: 10.2334/josnusd.48.167. [DOI] [PubMed] [Google Scholar]
- 4.Hartwell MB. Granuloma pyogenicum. J Cutan Dis Syph. 1904;22:520–5. [Google Scholar]
- 5.Mussalli NG, Hopps RM, Johnson NW. Oral pyogenic granuloma as a complication of pregnancy and the use of hormonal contraceptives. Int J Gynaecol Obstet. 1976;14:187–91. doi: 10.1002/j.1879-3479.1976.tb00592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller RA, Ross JB, Martin J. Multiple granulation tissue lesions occurring in isotretinoin treatment of acne vulgaris – Successful response to topical corticosteroid therapy. J Am Acad Dermatol. 1985;12:888–9. doi: 10.1016/s0190-9622(85)80126-2. [DOI] [PubMed] [Google Scholar]
- 7.Fowler EB, Cuenin MF, Thompson SH, Kudryk VL, Billman MA. Pyogenic granuloma associated with guided tissue regeneration: A case report. J Periodontol. 1996;67:1011–5. doi: 10.1902/jop.1996.67.10.1011. [DOI] [PubMed] [Google Scholar]
- 8.Epivatianos A, Antoniades D, Zaraboukas T, Zairi E, Poulopoulos A, Kiziridou A, et al. Pyogenic granuloma of the oral cavity: Comparative study of its clinicopathological and immunohistochemical features. Pathol Int. 2005;55:391–7. doi: 10.1111/j.1440-1827.2005.01843.x. [DOI] [PubMed] [Google Scholar]
- 9.Sills ES, Zegarelli DJ, Hoschander MM, Strider WE. Clinical diagnosis and management of hormonally responsive oral pregnancy tumor (pyogenic granuloma) J Reprod Med. 1996;41:467–70. [PubMed] [Google Scholar]
- 10.Sternberg SS, Antonioli DA, Carter D, Mills SE, Oberman H. Diagnostic Surgical Pathology. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 1999. [Google Scholar]
- 11.Eversole LA. Clinical Outline of Oral Pathology: Diagnosis and Treatment. 3rd ed. Hamilton: BC Decker; 2002. [Google Scholar]


