Abstract
Background: Katz Index is a well-known index for assessing basic activities of daily living. The aim was to determine validity and reliability of the Katz Index in Iranian patients with acute stroke.
Methods: Eighty-seven patients (56 male, 31 female) with acute stroke (1-30 days post-stroke) participated in this psychometric properties study. Interval time for retest was 14 days. All participants were Iranian with Persian as native language, had no other major diseases (e.g. cancer, Alzheimer) and no psychiatric disorder. Cognitive mental score of all participants was above 18 (according to Mini-Mental State Examination). If they had another stroke during the following-up period, they were excluded from the study. Intraclass Correlation Coefficient (ICC), Standard Error of Measurement (SEM) and Minimum Detectable Change (MDC) were calculated to investigate the reliability of the KI. Criterion validity of the KI was assessed by Spearman’s Correlation Coefficient (ρ). Moreover, Confirmatory Factor Analysis (CFA) and Exploratory Factor Analysis (EFA) were performed to investigate the construct validity of the KI.
Results: Inter-rater and intra-rater reliability of Persian Katz Index were reasonable (ICC2,1=0.93, ICC2,1=0.83; respectively). Internal consistency of this index was high (cronbach’s alpha=0.79). The high to excellent correlation was found between Katz Index and the motion (ρ=0.88), self-care (ρ=0.98), and total scores (ρ=0.92) of Barthel Index. Factor analysis of the Persian Katz Index indicated two factors including motion (bathing, toileting, and transferring) and self-care (dressing, bowel & bladder control, and feeding).
Conclusion: The results of this study suggest that Persian version of Katz Index in patients with acute stroke can be considered as an acceptable clinical instrument in practice and research.
Keywords: Validation, Katz Index, Acute stroke
↑ What is “already known” in this topic:
Katz index (KI) is a valid and reliable measure for assessing basic activities of daily living in elderly and patients with cancer. Moreover, the predictive validity of KI regarding length of hospital stay, discharge to own home or death within one month after stroke has been investigated.
→ What this article adds:
This study, investigated the reliability and validity of KI in acute stroke patients and showed that Persian version of Katz Index in patients with acute stroke can be considered as an acceptable clinical instrument in practice and research.
Introduction
Stroke is the adults’ most common condition leading to sensory-motor defects and disability in activities of daily living (ADL) (1). The main focus of health measures is ADL (2) and it is related to subjective well-being feeling or quality of life in patients with stroke (1). Indeed, promotion of ADL independence during rehabilitation is valuable for a better quality of life in stroke patients (3).
Individuals’ activities aimed at protecting themselves and achieving independence in daily life are named as ADL (4). It describes the patient’s current status in self-care activities and also is a predictor of the treatment process and outcomes (5). In recent decades, various tools have been developed for functional ability assessment (4,6). The Katz Index (KI) and Barthel Index (BI) are two primary tests in the assessment of ADL performance. Katz et al. in 1959 developed KI based on theories of human development, activities, and anthropologic hierarchies. It is an important and useful tool in the prediction of fall incidences and complications, mortality/ morbidity, length of hospital stay and discharge, necessity of health services and institutionalization, and functional status of non-institutionalized community-dwelling in post-stroke patients (2,6,7). The reliability of KI has been well documented. Also, it has an adequate and acceptable validity in assessing basic ADL especially in patients hospitalized for the first time (2). In addition, it is adopted in clinical decision making and health status improvement (4). Although, BI is frequently used as a prognosis indicator in hospital and long-term care units, KI applications mostly include detecting subtle changes in health status and functional deterioration in severe diseases in long term as well as assessing the social adaptation of patients with different diseases (e.g. older adults, stroke, poliomyelitis, rheumatoid arthritis and hip fracture). In addition, it is adaptable to most clinical conditions especially chronic ones with high incidence such as cardiovascular diseases (2,4,6). KI is simple, inexpensive and reliable in practice and clinic (4,8). This Index creates a common language about changes of patients function between all therapist and clinicians involved in overall care and discharge planning (9,10). Validation of KI has been investigated in several studies (2,4,8). Eloah et al. (2015) surveyed the validation of KI in two groups including patients with and without cognitive impairment and reported the mean cronbach's alpha (α) of 0.96 for the first group and 0.97 for the second group (11). In 2013, investigation of KI in Greek individuals with cancer showed excellent reliability (cronbach's α was 0.88) and satisfactory validity (12). Nasser and Doumit (2009) studied the validity and reliability of Arabic version of KI in elderly older than 60 years and reported the cronbach's α of 0.9 for the first three subscales (i.e. bathing, dressing and going to the toilet) and 0.65 for second three subscales (i.e. mobility, continence and feeding) (13). Spanish version of KI in old people showed excellent reliability (2). Reijneveld et al. (2006) assessed the reliability and validity of Turkish KI in Turkey, Moroccan and Dutch elderly and showed good internal consistencies for each group (cronbach's α: 0.84-0.94) and reasonable criterion validity (14).
KI has been originally developed for evaluating the basic ADL in elderly (7). Alizadeh-Khoei et al. (2013) translated this index in Persian language and validated it in Iranian elderly population with cancer (8). This study has found that the KI is a reliable and valid instrument for evaluating basic ADL in patients with cancer. However, considering the different underlying pathologies in patients with stroke compared to those with cancer, the results of Alizadeh-Khoei et al. study cannot be directly applied to patients with stroke. Moreover, investigating the validity and reliability of this frequently used index in stroke patients allows comparison of the results with other pathologies and studies. Therefore, the purpose of the present study was to examine inter and intra-rater and internal consistency reliability, criteria and construct validity of the Persian version of KI in patients with acute stroke.
Methods
Participants
In this methodological research, eighty-seven patients (56 male, 31 female) by mean age of 61 yrs. (range: 40-80 yrs.) were recruited from neurological clinics and rehabilitation centers of Iran University of Medical Sciences by the simple non-probability method. Inclusion criteria were: passing maximum one month from the last stroke (based on physician's diagnosis) (15), being Iranian with Persian as native language, not having other major diseases (e.g. cancer, Alzheimer and dementia) or no known psychiatric disorder (based on physician's diagnosis), not having cognitive impairment (i.e. obtaining a score equal or higher than 18 on Mini-Mental State Examination) (16). Patients were excluded from the study if they had another stroke during the follow-up period or did not wish to continue participating in the study. All patients/ primary caregiver signed written informed consent to participate in this study. Two experienced occupational therapists performed the test through observation and face-to-face interviews with patients or primary caregivers. The time interval between test and retest was 14 days (1,8). The study protocol was approved by the Ethics Committee of Iranian University of Medical Sciences.
Translation of KI
The International Quality Of Life Assessment method (17) was used to translate and adapt this questionnaire from the original English version to Persian language version. First of all, permission license for KI translation was taken from “Oxford University Press” (License Number 2975190407921). Forward translation from the original English version to Persian was done by two native Persian speaker, independently. Then, the primary Persian form of KI was provided by translators and researchers. The backward translation from Persian to English was done by two native English language translators, separately. Finally, this questionnaire was checked by the expert committee including translators and authors, and the final version of this instrument was provided.
Measurements
Katz Index (KI): This Index has two versions: original version with seven items and modified new version with six items (18). The new version (used in this study) contains six basic functional tasks: bathing, dressing, toileting, transferring, bowel & bladder control, and feeding (7). KI as a Guttman-type scale presents items in a hierarchy of severity or difficulty of performing each task. Scoring of each item of this instrument includes independence [1] and dependence [0]. Independence is defined as performing these tasks without supervision, guidance or personal assistance while dependence is defined as doing the tasks with supervision, guidance or personal assistance. Total KI score is in the range of 0 to 6 which score of 6 represents an independent patient and 0 indicates a very dependent one (10,19). Completing this test lasts less than 5 minutes (2,14).
Barthel Index (BI): This Index has satisfactory psychometric properties in stroke patients (20). It evaluates dependence/ independence of functional ability 10 items including bowels, bladder, toilet use, bathing, dressing, grooming, feeding (as self-care items); and transfer (bed to chair and back), mobility, stair up and down (as motion items). Four point increments are used in scoring [0,5,10,15], with total score between 0 (dependent bed-ridden state), and 100 (fully independent in physical functioning). Scores of self-care items and motion items, as well as total sore of BI, were used in this survey. It takes approximately 5-10 minutes to be completed (2,8). Validation of this tool has been studied in Iranian people (20).
Procedure
To investigate the inter-rater reliability of the KI, all samples were assessed by two experienced raters in one session (21). To determine the intra-rater reliability of the KI, all subjects in the first assessment were evaluated in the second assessment (i.e. 14 days later) by one experiencedrater. Results of first assessment of the first rater were used to examine the internal consistency reliability, criterion and construct validity. In order to examine the criterion and construct validity of the KI, BI and factor analysis was used; respectively.
Statistical Analysis
Normal distribution of data was tested by Kolmogorov-Smirnov test. Inter-rater reliability and intra-rater reliability for total item of KI were calculated by Intraclass Correlation Coefficients (ICC2,1) (22). The ICC value≥0.8 and between 0.6-0.8 indicates excellent and moderate reliability; respectively (23). Standard Error of Measurement (SEM), SEM%, Minimum Detectable Change (MDC) and MDC% were calculated for both of inter-rater & intra-rater reliability with the following formula: SEM=SD and MDC=SEM(24). Internal consistency was assessed using cronbach's α coefficient (α). The minimum acceptable value for α was 0.7 (23). Ceiling and floor effects are described as the number of patients obtaining the highest and lowest possible scores on the used test; respectively. Ceiling/ floor effects less than 15% are generally considered acceptable (25,26). Criterion validity was assessed by measuring the correlation between Persian KI scores and BI (Self-care/ Motion) using Spearman’s Correlation Coefficient (ρ). Spearman values between 0.90-1.00 indicate excellent correlation (21). Confirmatory Factor Analysis (CFA) and Exploratory Factor Analysis (EFA) with Varimax rotation were conducted to investigate the construct validity of the Persian KI version (23). In order to investigate the goodness-of-fit of the model with the given dataset, several model fit indices and their criteria were used including Goodness-of-Fit Index (GFI), Adjusted Goodness-of-Fit Index (AGFI), Normed Fit Index (NFI), Tucker-Lewis Index (TLI), Comparative Fit Index (CFI), and Root Mean Square Error of Approximation (RMSEA). EFA and CFA were conducted with SPSS for Windows (version 13.0) and AMOS (version 24.0); respectively. The level of statistical significance were considered at P-value<0.005.
Results
Descriptive Statistics: No case was omitted from the analyses due to the missing data. The mean age of participants was 61 (SD=12.46) years. The score of Mini-Mental Status Examination was 18 to 26 (mean±SD=20.9±2.84). Minimum and maximum numbers of medications per day were 1 and 5; respectively. Seventy-five participants (86.2%) took their medications in the morning. Table 1 illustrates the detailed participants’ descriptive data. The mean (SD) total score of KI for motion, self-care and, total scores of BI were 3.66 (1.99), 29.12 (14.23), 41.9. (17.26), and 67.87 (29.74), respectively. The result of Kolmogorov-Smirnov showed that total scores of KI and BI have no normal distribution (p<0.001).
Table 1. Characteristics of study participants .
| Variable | Number | % |
| Gender | ||
| Male | 56 | 64.4 |
| Female | 31 | 35.6 |
| Education level | ||
| Under diploma | 60 | 69 |
| Diploma | 19 | 21.8 |
| Collage | 8 | 9.2 |
| Family status | ||
| Single | 7 | 8 |
| Married | 67 | 77 |
| Widow/divorce | 13 | 15 |
| Living arrangement | ||
| Alone | 7 | 8 |
| With spouse/relative | 80 | 92 |
| High risk factors | ||
| Hypertension (from 87 subjects) | 44 | 50.6 |
| Cholesterol (from 87 subjects) | 22 | 25.3 |
| Diabetes (from 87 subjects) | 21 | 24.1 |
| Smoking (from 87 subjects) | 12 | 13.8 |
| Poly pharmacy≥4 (from 87 subjects) | 78 | 89.7 |
| Use assistive devise | ||
| Yes | 35 | 40.2 |
| No | 52 | 59.8 |
| Rehab service | ||
| Yes | 37 | 42.5 |
| No | 50 | 57.5 |
| Number of stroke | ||
| 1 | 67 | 77.1 |
| 2 | 18 | 20.7 |
| 3 | 1 | 1.1 |
| >3 | 1 | 1.1 |
Reliability: Inter-rater reliability for total score of KI items indicated excellent reliability (ICC2,1=0.93, p<0.001, 95%CI: 0.89-0.95). The SEM, SEM%, MDC, and MDC% values were 0.51, 13.8%, 1.42, and 38.2%; respectively. Intra-rater reliability of total items indicated excellent reliability (ICC2.1=0.83, p<0.001, 95%CI: 0.70-0.90). The SEM, SEM%, MDC, and MDC% values were 0.79, 20.3%, 2.19, and 56.3%; respectively.
Internal consistency of the total score in Persian KI was good (cronbach’s α=0.79). The range of cronbach's α with deletions of each item was 0.77 to 0.85. Correlation between each item of Persian KI and its total score was 0.48-0.88 (Table 2). The ceiling and floor effects of Persian KI were 28.74% and 5.75%; respectively.
Table 2. Factor analysis and internal consistency of Persian Katz Index in stroke .
| Items | Mean (SD) | Factor Loading | Community |
Cronbach’s α If item deleted |
Correlation Item to total |
|
| Factor 1 | Factor 2 | |||||
| Bathing | 0.39 (0.49) | 0.80 | -0.07 | 0.68 | 0.78 | 0.81 |
| Dressing | 0.45 (0.50) | 0.43 | 0.45 | 0.54 | 0.81 | 0.73 |
| Toileting | 0.52 (0.50) | 0.95 | -0.02 | 0.88 | 0.77 | 0.88 |
| Transferring | 0.56 (0.50) | 0.97 | 0.10 | 0.87 | 0.77 | 0.84 |
| Bowel & Bladder Control | 0.87 (0.33) | -0.16 | 0.95 | 0.81 | 0.85 | 0.48 |
| Feeding | 0.86 (0.35) | 0.29 | 0.55 | 0.51 | 0.82 | 0.62 |
| Total | 3.66 (1.99) | 0.84 | 1 | |||
| Eigen value | 3.27 | 1.03 | ||||
Validity: Criterion validity was calculated by evaluating the correlation between Persian KI and BI. An excellent correlation (ρ=0.92, p<0.001) was found. Also, there were an excellent (ρ=0.93) and high (ρ=0.88) correlations between the Persian KI with self-care and motion scores of BI; respectively.
Value of the “Kaiser-Meyer-Olkin” measure of sampling adequacy used to verify the data set suitability for factor analysis was 0.713. The “Bartlett’s Test of Sphericity” value was significant (א2=277.63, p<0.001). Two components (Motion: bathing, toileting, transferring; and Self-care: dressing, bowel & bladder control, feeding) were extracted based on Eigen values greater than one (Table 2). These components explained 71.65% of the total variance. Two-factor model from the results of this study for CFA is depicted in Figure 1. The model fit indices were: GFI=0.97, AGFI=0.91, NFI=0.76, TLI=0.90, CFI=0.95 and RMSEA=0.04.
Fig. 1.
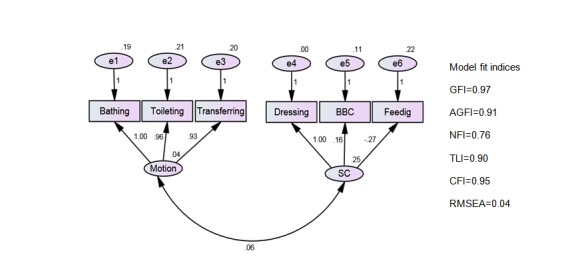
Results of Confirmatory Factor Analysis of the Persian Katz Index for stroke
(BBC: Bowel & Bladder Control; SC: Self-Care; GFI: Goodness-of-Fit Index; AGFI: Adjusted Goodness-of-Fit Index; NFI: Normed Fit Index,
TLI: Tucker-Lewis Index; CFI: Comparative Fit Index; RMSEA: Root Mean Square Error of Approximation)
Discussion
The present study assessed the psychometric properties of the Persian KI in Iranian patients with acute stroke. Results indicated that the Persian KI has excellent reliability and acceptable validity in assessing basic ADL in patients with acute stroke.
Reliability: Inter-rater reliability for total score indicated excellent reliability. Similarly, Alvarez et al. (27), Spector & Takada (28), Hulter Asberg & Sonn (29), and Katz et al. (10) reported excellent inter-rater reliability. Also, EK et al. (30) stated moderate to good inter-observer reliability (Kappa=0.56), but Brosson & Asberg (31) reported low inter-rater reliability. Possible explanation for different results compared to the results of the current study could be the different methods used for training the raters. Katz et al. (10) explained that the inter-rater reliability was greater after tool training in the scoring of each item. Another possible reason for this result may be cultural differences such as the concepts of shame and religious beliefs. Intra-rater reliability for total items indicated excellent reliability. Similarly, Alizadeh-Khoei et al. (8), Mystakidou & Tsilika (12), and Alvarez et al. (27) reported excellent intra-rater reliability with correlation coefficients range of 0.83 to 0.94. A possible explanation for this result might be that the KI is a large scale measure and it is unlikely that patients score on this measure change markedly in 14 days interval for a retest (32). Values of the MDC% in total scores of Persian KI for the intra-rater after two weeks and inter-rater were 56.3% and 38.2%; respectively. This implies that for clinical users, 56.3% and 38.2% or higher change of KI score for intra-rater and inter-rater, indicates that real improvement has occurred.
Internal consistency of all items of Persian KI was acceptable. Similarly, Alizadeh-Khoei et al. (8) and Mystakidou & Tsilika (12) reported an acceptable internal consistency in patients with cancer. Other studies such as Rodgers & Miller (33) (cronbach’s α=0.89), Sonn (34) (α range=0.84-0.9), and Spector et al. (35) (α range=0.73-0.78) also stated acceptable internal consistency in all items of KI in elderly.
Results of correlation between each item and total Persian KI score indicated a statistically significant association, but only item 5 (bowel & bladder control) had a relatively low correlation with the total score. The same findings were observed by Mystakidou & Tsilika (12), Spector et al. (35) and Spector & Fleischman (36), suggested reasons for this finding include: shame, fear of mortality, receiving another medication or operation, the belief that there is no effective remedy, reduction of self-esteem, self-neglect, and feeling of social incompetence (6,37).
Validity: Criterion validity was assessed by the association of the Persian KI and motion, self-care and total score of BI; asignificant correlation was found. Results demonstrated that higher Katz scores were associated with better motion and good mobility. In other words, it showed that KI could be a good criteria measure in predicting mobility problem of stroke patients. Also, the results demonstrated higher total KI score was correlated with independence in self-care activities. Similarly, Harting et al. (38), Wade & Hewer (39), and Gresham et al. (40) have reported a high correlation between KI and BI.
The criteria of the various model fit indices were considered to discuss the model fit of CFA. It has been proposed that RMSEA values less than 0.05 are good, values between 0.05 and 0.08 are acceptable, values between 0.08 and 0.1 are marginal, and values greater than 0.1 are poor (41). Therefore, the RMSEA value of 0.04 in this study shows a good fit. The GFI as well as AGFI value of 0.9 or over indicates a good fit. So, the GFI value of 0.97 and AGFI value of 0.91 in this sample indicates a good fit of the model (42). Also, CFI value of 0.95 shows a good fit (43). NFI and TLI should be equal or over 0.9 for a good fit (43), but in this study, the NFI is little below the criteria. Based on these indices, this sample has a good fit to the 2-factor model. The factor analysis of Persian KI in stroke patients depicted two major factors, including Motion (bathing, toileting, transferring) and Self-care (dressing, bowel & bladder control, feeding). Also, a strong correlation was observed between the items and the two extracted components. Similarly, Alizadeh-Khoei et al. (8) found two factors in elderly subjects with cancer. Since culture significantly affects daily activities of living through its important role in shaping our behavior, cultural norms and values (44), the similar extracted factor in the current study and the study of Alizadeh-Khoei et al. may be explained by the fact that both studies were conducted in Iranian subjects. Mystakidou & Tsilika (12), Spector & Fleischman (36), and Kempen & Surrmeijer (45) reported one factor, while Cumming et al. (46) and Fitzgerlad et al. (47) have reported three factors. The KI factors found in this study is consistent with the conceptual framework of this measure that assesses motion and self-care of activity daily living.
The result of this study indicated that the KI have a ceiling effect in the assessment of ADL in acute stroke patients. Ceiling effect means that some patients obtain the highest score with the used test (25,48). If the test items are not challenging enough for some individuals due to inappropriate item selection or a limited number of difficult items, ceiling effects will occur (25,49,50). Since most of the participants in this study have the ability to walk independently, with or without assistive devices, therefore the items of KI may be not challenging enough for these patients. Another possible explanation for this result may be the small number of items in KI (51).
A number of limitations need to be noted regarding the present study. The convenience sampling method may limit the generalization of the results of this study. Given the ceiling effect of the KI, as observed in this study, further studies to investigate the ceiling effect of KI in patients with stroke is warranted. Moreover, the type of stroke was not considered in the current study which is recommended to be addressed in future investigations.
Conclusion
In conclusion, the Persian version of KI is a reliable and valid clinical instrument for assessing the ADL among Iranian acute stroke patients.
Acknowledgements
We would like to appreciate all patients and their families for their co-operation. The authors are also grateful to Dr. Anita Emrani, Ph.D. for the kind assistance and insightful comments in English language editing of this article.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Azad A, Mohammadinezhad T, Taghizadeh Gh, Lajevardi L. Clinical assessment of activities of daily living in acute stroke: Validation of the Persian version of Katz Index. Med J Islam Repub Iran. 2017(3 June 2017);31:30. https://doi.org/10.18869/mjiri.31.30
References
- 1.Hsueh IP, Wang CH, Liou TH, Lin CH, Hsieh CL. Test-retest reliability and validity of the comprehensive activities of daily living measure in patients with stroke. J Rehabil Med. 2012;44(8):637–41. doi: 10.2340/16501977-1004. [DOI] [PubMed] [Google Scholar]
- 2.Cabanero-Martınez MJ, Cabrero-Garcıa J, Richart-Matinez M, Munoz-Mendoza CL. The Spanish versions of the Barthel Index (BI) and the Katz Index (KI) of activities of daily living (ADL): A structured review. Arch Gerontol Geriatr. 2009;49(1):e77–e84. doi: 10.1016/j.archger.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 3. Fawcus R. Stroke rehabilitation: A collaborative approach. UK: Blackwell Science Ltd; 2008.pp.80-8.
- 4.Hartigan I. A comparative review of the Katz ADL and the Barthel Index in assessing the activities of daily living of older people. Intern J Older People Nurs. 2007;2(3):204–12. doi: 10.1111/j.1748-3743.2007.00074.x. [DOI] [PubMed] [Google Scholar]
- 5.Indsay P, Bayley M, Hellings C, Hill M, Woodbury E, Phillips S. Canadian best practice recommendations for stroke care. Canada Med Assoc J. 2008;179(12):S1–25. doi: 10.1503/cmaj.081536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen ME, Marino RJ. The tools of disability outcomes research functional status measures. Arch Phys Med Rehabil. 2000;81(12):S21–9. doi: 10.1053/apmr.2000.20620. [DOI] [PubMed] [Google Scholar]
- 7.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the Index of ADL. Gerontologist. 1970;10(1):20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 8.Alizadeh-Khoei M, Akbar ME, Sharifi F, Fakharzadeh H, Larijani B. Translation and validation of the activities of daily living scale with Iranian elderly cancer patients treated in an oncology unit. Asian Pacific J Cancer Prevention (APJCP) 2013;14(5):2731–7. doi: 10.7314/apjcp.2013.14.5.2731. [DOI] [PubMed] [Google Scholar]
- 9.Wallace M, Shelkey M. Katz Index of independence in activity of daily living. Assisted Living Consult. 2008;108(4):21–2. [Google Scholar]
- 10.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: The Index of ADL: A standardized measure of biological and psychosocial functions. J Am Med Assoc. 1963;185(12):914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 11.Eloah R, Alencar M. Validity of the Katz Index to assess activities of daily living by informants in neuropath logical studies. Rev Esc Enferm USP. 2015;49(6):944–50. doi: 10.1590/S0080-623420150000600010. [DOI] [PubMed] [Google Scholar]
- 12.Mystakidou K, Tsilika E, Parpa E, Mitropoulou E, Galanos A, Gouliamos A. Activities of daily living in Greek cancer patients treated in a palliative care unit. Support Care Cancer. 2013;21(1):97–105. doi: 10.1007/s00520-012-1497-5. [DOI] [PubMed] [Google Scholar]
- 13.Nasser R, Doumit J. Validity and reliability of the Arabic version of activities of daily living. BMC Geriatr. 2009;9:11. doi: 10.1186/1471-2318-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reijneveld AC, Spijker J, Dijkshoorn H. Katz’ ADL Index assessed functional performance of Turkish, Moroccan and Dutch elderly. J Clin Epidemiol. 2007;60(4):382–8. doi: 10.1016/j.jclinepi.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Bouffioulx E, Amould C, Vandevelde L, Thonnard JL. Change in satisfaction with activities and participation between acute, post-acute, and chronic stroke phases: A responsiveness study of the SATIS-stroke questionnaire. J Rehabil Med. 2010;42(10):944–8. doi: 10.2340/16501977-0635. [DOI] [PubMed] [Google Scholar]
- 16.Schmid AA, Rittman M. Consequences of post stroke falls: Activity limitation, increased dependence, and the development of fear of falling. AJOT. 2009;63(3):310–16. doi: 10.5014/ajot.63.3.310. [DOI] [PubMed] [Google Scholar]
- 17.Aaronson NK, Acquadre C, Alonso J, Apolone G, Bucquet D, Bullinger M. et al. International quality of life assessment (IQOLA) project. Quality Life Res. 1992;1:349–51. doi: 10.1007/BF00434949. [DOI] [PubMed] [Google Scholar]
- 18.Westergren A, Karlsson S, Andersson P, Ohlsson O, Hallberg IR. Eating difficulties, need for assisted eating, nutritional status and pressure ulcers in patients admitted for stroke. J Clin Nurs. 2001;10(2):257–69. doi: 10.1046/j.1365-2702.2001.00479.x. [DOI] [PubMed] [Google Scholar]
- 19.Patricia P. Measures of adult general functional status. Arthritis Care Res. 2003;49:15–27. [Google Scholar]
- 20.Oveisgharan S, Shirani S, Ghorbani A, Soltanzade A, Baghaei A, Hosseni S. et al. Barthel Index in a Middle-East country: Translation, validity and reliability. Cerebrovasc Dis. 2006;22(5-6):350–4. doi: 10.1159/000094850. [DOI] [PubMed] [Google Scholar]
- 21. Domholdt E. Rehabilitation research: Principles and applications. 3rded. Philadelphia: Saunders; 2005.pp.274-6.
- 22.Shrout PE, Fleiss JL. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychol Bull. 1979;86(2):420–8. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 23.Hsueh I, Lee M, Hsieh C. Psychometric characteristics of the Barthel: Activities of daily living Index in stroke patients. J Formo Med Assoc. 2001;100(8):526–32. [PubMed] [Google Scholar]
- 24.Chou CY, Chien CW, Hsueh IP, Sheu CF, Wang CH, Hsieh CL. Developing a short from of the Berg Balance Scale for people with stroke. J Phys Ther. 2006;86(2):195–204. [PubMed] [Google Scholar]
- 25.Hamilton DF, Giesinger IM, MacDonald DJ, Simpson AH, Howie CR, Giesinger K. Responsiveness and ceiling effects of the forgotten joint score-12 following total his arthroplasty. Bone Joint Res. 2016;5(3):87–91. doi: 10.1302/2046-3758.53.2000480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Justicia-Grande AS, Pardo-Seco J, Cebey-Lopez M, Vilanovar-Trillol Vilanovar-Trillol, Gomez-Carballa A, Rivero-Calle I. et al. Development and validation of a new clinical scale for infant with acute respivatory infection: The ReSVinet Scale. PLOS ONE. 2016:1–15. doi: 10.1371/journal.pone.0157665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alvarez M, Alaiz AT, Bru E, Cabaneros JJ, Calzon M, Cosio I. et al. Capacidad funcional de pacientes mayores de 65 anos, segunel Indice de Katz Fiabilidad delmetodo Aten. Primaria. 1992;10:812–16. (Abstract in English). [PubMed] [Google Scholar]
- 28.Spector WD, Takada HA. Characteristics of nursing homes that resident outcome. J Aging Health. 1991;3(4):427–54. doi: 10.1177/089826439100300401. [DOI] [PubMed] [Google Scholar]
- 29.Hulter-Asberg K, Sonn U. The cumulative structure of personal and instrumental ADL. Scand J Rehabil Med. 1989;21(4):171–7. [PubMed] [Google Scholar]
- 30.Ek AC, Unosson M, Larsson J, Ganowiak W. Inter-rater variability in subjective nutritional assessment of elderly patients. Scand J Caring Sci. 1996;10(3):163–8. doi: 10.1111/j.1471-6712.1996.tb00330.x. [DOI] [PubMed] [Google Scholar]
- 31.Brorsson B, Asberg Asberg, KH KH. Katz Index of independence in ADL Reliability and validity in short-term care. Scand J Rehabil Med. 1984;16(3):125–32. [PubMed] [Google Scholar]
- 32.Salavati M, Mazaheri M, Negahban H, Ebrahimi I, Jafari AH, Kazemnjad A. et al. Effect of dual-tasking on postural control in subjects with nonspecific low back pain. Spine. 2009;34(13):1415–21. doi: 10.1097/BRS.0b013e3181a3a917. [DOI] [PubMed] [Google Scholar]
- 33.Rodger W, Miller B. A Comparative analysis of ADL questions in survey of older people. J Gerontol B. 1997;52B(Special Issue):21–36. doi: 10.1093/geronb/52b.special_issue.21. [DOI] [PubMed] [Google Scholar]
- 34.Sonn U. Longitudinal studies of dependence in daily life activities among elderly persons. Scand J Rehabil Med Suppl. 1996;34:1–35. [PubMed] [Google Scholar]
- 35.Spector WD, Katz S. , Murphy JB, Fulton JP The hierarchical relationship between activities of daily living and instrumental activities of daily living. J Chronic Dis. 1987;40(6):481–9. doi: 10.1016/0021-9681(87)90004-x. [DOI] [PubMed] [Google Scholar]
- 36.Spector WD, Fleischman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. J Gerontol. 1998;53(1):S46–57. doi: 10.1093/geronb/53b.1.s46. [DOI] [PubMed] [Google Scholar]
- 37.Wilson MM. Urinary incontinence: A treatise on gender, sexuality and culture. Clin Geriatric Med. 2004;20(3):565–70. doi: 10.1016/j.cger.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 38.Harting MT, Engle VF. Geraney MJ Accuracy of nurse aides' functional health assessment of nursing home residents. J Gerontol. 1997;52A(3):M142–8. doi: 10.1093/gerona/52a.3.m142. [DOI] [PubMed] [Google Scholar]
- 39.Wade D, Hewer R. Motor loss and swallowing difficulty after stroke: Frequency, recovery and prognosis. Acta Neurol Scand. 1987;76(10):50–4. doi: 10.1111/j.1600-0404.1987.tb03543.x. [DOI] [PubMed] [Google Scholar]
- 40.Gersham GE, Phillips TF, Labi ML. ADL statues in stroke: Relative merits of three standard indexes. Arch Phy Med Rehabil. 1980;61(8):355–8. [PubMed] [Google Scholar]
- 41.Fabrigar LR, MacCallum RC, Wegener DT, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999;4(3):272–99. [Google Scholar]
- 42.Mulaik SA, James LR, Van Alstine J, Bennett N, Lind S, Stilwell CD. Evaluation of goodness-of-fit indices for structural equation models. Psychological Bulletin. 1989;105(3):430–45. [Google Scholar]
- 43.Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–46. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 44.Arik G, Varan HD, Yavuz BB, Karabulut E, Kara O, Kilic MK, Kizilarslanoglu MC. et al. Validation of Katz Index of independence in activities of daily living in Turkish older adults. Arch Gerontol Geriatr. 2015;61(3):344–50. doi: 10.1016/j.archger.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 45.Kempen GI, Surrmeijer TP. The development of a hierarchical polychotomous ADL-IADL scale for non-institutionalized elders. J Gerontol. 1990;30(4):497–502. doi: 10.1093/geront/30.4.497. [DOI] [PubMed] [Google Scholar]
- 46.Cumming SM, Neff JA, Ban H. Functional impairment as a predictor of depressive symptomatology: The role of race, religiosity and social support. Health Soc Work. 2003;28(1):23–32. doi: 10.1093/hsw/28.1.23. [DOI] [PubMed] [Google Scholar]
- 47.Fitzgerlad JF, Smith DM, Martin DK, Freedman JA, Wolinsky FD. Replication of the multidimensionality of activities of daily living. J Gerontol. 1993;48(1):S28–31. doi: 10.1093/geronj/48.1.s28. [DOI] [PubMed] [Google Scholar]
- 48.Trewee CB, Bot SD, de Boer MR, van der Windt DA, Dekker J, Bouter LM. et al. Quality criteria were proposed fof measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 49.MCHorney CA, Tarlor AR. Individual-patient monitoring in clinical practice: Are available health status surveys adequate? Qual Life Res. 1995;4(4):293–307. doi: 10.1007/BF01593882. [DOI] [PubMed] [Google Scholar]
- 50.Lai SM, Perea S, Duncan PW, Bode R. Physical and social functioning after stroke: Comparison of the stroke impact scale and short form-36. Stroke. 2003;34(2):488–93. doi: 10.1161/01.str.0000054162.94998.c0. [DOI] [PubMed] [Google Scholar]
- 51.Zhaeentan S, Legeby M, Ahlstrom S, Stark A, Salomonsson B. A validation of the Swedish version of the WORC index in the assessment of patients treated by surgery for subacromial disease including rotator cuff syndrome. BMC Muscuskeletal Disorders. 2016;17:165–73. doi: 10.1186/s12891-016-1014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


