Abstract
As recently as the 1970s, children born with sickle cell disease (SCD) were unlikely to survive into adulthood. With advances in medical care, most patients now survive childhood and live into their forties or beyond [1,2]. A better transition from pediatric- to adult-focused care is therefore increasingly important [3]. Despite recent awareness of the importance of transition by the SCD community, little is known about existing transition programs. We conducted a survey of pediatric sickle cell clinics to describe current transition practices and identify areas for improvement. Survey topics included program demographics, transition logistics, assessment of patient transition readiness and independence, transition preparation, and program evaluation. Twenty-three clinics (77%) report having a transition program, although half have been in place for under 2 years. There is wide variation in specific transition practices. Most centers (97%) have an identified accepting adult provider, however, only 60% routinely transfer their patients to an adult hematologist specializing in SCD. Although there has been a recent effort to establish transition programs in pediatric sickle cell clinics, specific practices vary widely. As anticipated, lack of an accepting adult hematologist with an interest in SCD emerged as a common barrier to transition.
SCD currently affects over 89,000 Americans with 2,000 children born with the disease each year, making it one of the most prevalent inherited chronic diseases of childhood [4,5]. As patients become young adults, disease complications change, with increasing rates of painful episodes, increased health care utilization (including rehospitalization), and cost [6–8]. A recent study showed that an alarming number of deaths occurred shortly after transfer to an adult program [2]. These findings highlight the crucial need to help patients make the transition from pediatric- to adult-focused care [3].
Transition has been defined as a “purposeful, planned” process with a goal of providing continuity of care and preparing young adults for greater independence [9]. It has been proposed that transition planning should begin early and include disease specific knowledge as well as self-management skills. Transition applies to pediatric providers as well as the patient and family and should encompass medical, psychosocial, and educational needs [9,10]. The transition process then culminates in a medical transfer of care which includes finding an accepting adult provider, helping the patient with logistics such as insurance coverage, and ensuring transfer of medical records, including a portable medical summary for the patient [11].
Studies have found that overall adolescents are dissatisfied with their transition experience. Over half of cystic fibrosis (CF) patients expressed concern over the care they will receive as adults [12]. Specific concerns include lack of information about adult facilities, not meeting an adult provider prior to switching care, and poor communication between pediatric and adult teams [13–15]. Adolescents with SCD similarly report wanting more information about what to expect after transfer, uncertainty about how they will pay for medical care, fear of leaving a familiar, trusted provider, and worry that adult providers may not be familiar with managing SCD [13,15,16]. Studies have found worse outcomes following the transition to adult care, such as increased hospitalizations in patients with diabetes mellitus and decreased adherence to immunosupression in liver transplant patients [17,18].
A recent publication provided an excellent conceptual model for transition in SCD, described three current model transition programs as examples, and highlighted areas for future research [19]. However, little is known about transition programs for SCD. Therefore, we sought to characterize current transition practices for SCD and identify areas for improvement.
The response rate to our survey was 67% (30/45). The majority of the centers are large, academic urban clinics associated with a free-standing children’s hospital. Ten programs are located in a combined pediatric/adult hospital. Most centers are located in the South or Northeast. Most respondents (67%) have been working in their clinic for more than 5 years (see Supporting Information Table I).
Just over half of the centers (57%) are in a system with a required age for transition due to “hospital policy,” which ranges from 18–22 years. Transition is first discussed at an average age of 15.7 years (range 13–18) and transfer occurs at a mean age of 19.6 years (range 18–25). One center continues to see adult patients in the pediatric clinic for sickle cell care because of the lack of an adult provider. One-third of centers allow patients to remain in pediatric care past the cut-off age in cases of cognitive or developmental delay, or needing time to complete a transition program, graduate high school, or find an adult provider. The most common criteria used for transferring a patient to adult care are age (100%) and pregnancy (74%) (see Supporting Information Table II).
The majority of centers (97%) have at least one identified adult provider to accept patients from the pediatric clinic; however, only 18 centers (60%) routinely transfer their patients to an adult hematologist specializing in SCD. Ten percent of programs transfer patients to an internist rather than hema-tologist (see Supporting Information Table III). In free text comments, the majority of respondents identified difficulties finding an appropriate adult sickle cell provider as their most significant transition issue.
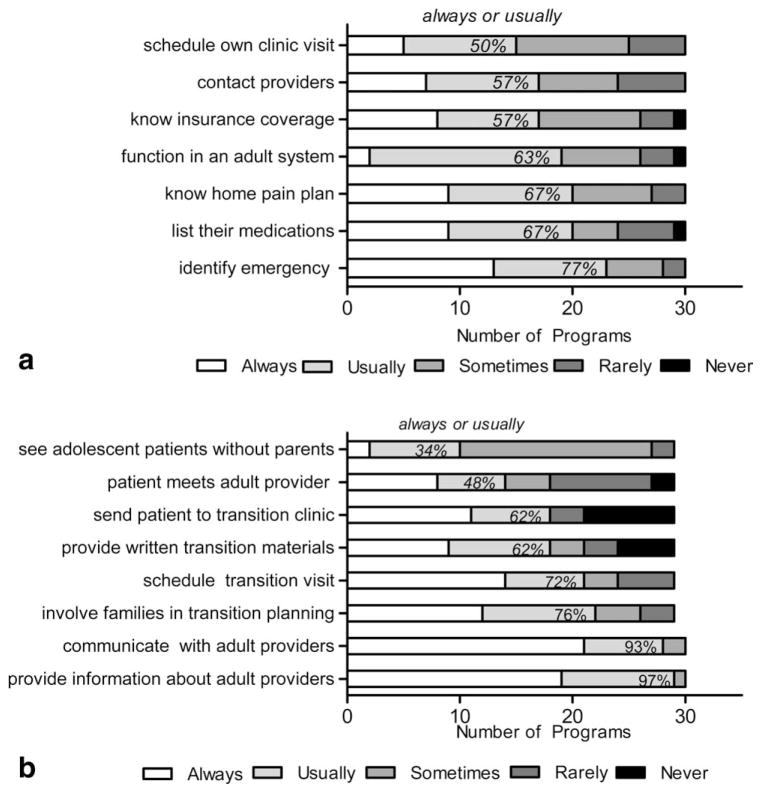
Half of the centers have a written list of desirable self-management skills, 60% have a program to foster patient self-management, and 70% report assessing patient readiness to transition. Most centers report “always” or “usually” reviewing the readiness assessment as a team (73%), discussing it with the patient or family (73%), adding it to the medical record (64%), and making a plan to address an area of need (64%). However, there is substantial variation in specific practices related to assessment of patient transition readiness or independence. Almost all centers report that they communicate with adult providers and provide information about adult providers to their patients. However, surprisingly few centers report seeing adolescent patients without parents, or assessing if a patient is able to independently schedule a clinic visit or contact providers. Even scheduling a visit focused on transition was far from universal (Fig. 1). In open ended, comments providers identified a need for additional transition resources such as “transition program and materials” and “formal/written/checklist/documentation of steps/readiness.”
Figure 1.
A: Number of programs reporting how often their providers assess if a patient is able to complete certain tasks independently. Cumulative percent of programs answering “usually” or “always” is included. B: Number of programs reporting how often their providers complete certain steps in transition preparation. Cumulative percent of programs answering “usually” or “always” is included.
Slightly over half (54%) of centers evaluate their transition program at least annually, with the main area of evaluation being communication between adult and pediatric providers (72%). Few centers assess patient satisfaction (39%) or follow clinical outcomes (33%) or utilization measures (17%). The average self-assessment score was 3.2 on a scale from 1 (weak) to 5 (strong), ranging from 3.0 for patient and provider “satisfaction with transition” to 4.0 for “communication with adult providers.”
This first known study highlighting specific transition practices among a national sample of pediatric sickle cell centers shows a recent move toward developing transition programs with a focus on the medical transfer of patients from pediatric to adult providers, and less emphasis on the patient readiness components of the transition process.
Age and pregnancy are still the primary factors that determine time of transfer, which is problematic in SCD. Pregnancy in adolescents and young adults may not be planned, and therefore, using it as a trigger for transfer is unlikely to allow adequate time for preparation. Using age as a proxy for maturity may be particularly problematic for patients with SCD, who may have neurocognitive delay due to cerebrovascular injury [20]. Even children with SCD but without overt stroke have been shown to have deficits in executive function which may make it more challenging for young adult patients to help with the necessary planning for transition [21].
The fact that finding an appropriate adult provider with expertise in SCD was frequently identified as the most significant transition issue facing pediatric sickle centers is of particular concern given the growing number of young adult patients. Young adulthood is a vulnerable time, when young adults need a provider whom they trust and who can help manage their disease.
Our study has certain limitations. Without a systematic way to identify sickle cell centers, we cannot claim to have a nationally representative sample. However, even this highlights the discrepancy between SCD care and that of other chronic diseases, where national foundations allow identification of accredited centers and collaboration on best practices. Lack of central organization or collaboration between programs remains a problem in SCD, in contrast to CF with a unified organization that drives advocacy, research funding, and clinical care. The Cystic Fibrosis Foundation reviews and accredits over 100 CF Centers annually in the US, which allows centers to be eligible for funding and creates an infrastructure for improved quality of care [22]. Nothing similar exists for SCD, at least in part because of the disparities in both research and funding, as well as less organized activism by patients, families, and advocacy groups compared with the model of CF [23].
We also have not accounted for the fact that most children with SCD are cared for outside of sickle cell centers [24]. Finally, respondents from sites with a transition program may have been more likely to answer the survey, leading to bias in our results. However, these limitations strengthen our results, as the programs we identified may be the best that is going on, and there are still areas for improvement.
Further steps in research must focus on more clearly identifying the spe-cific transition practices that are most effective in preparing pediatric patients to become successful young adult patients and on helping providers develop and implement these practices. Validation of transition checklists would be an important first step in meeting the identified need for transition resources.
The central goal of helping patients achieve independence as they reach young adulthood is one that all pediatricians and pediatric sub-specialists share. With more than 500,000 adolescents with special health care needs reaching an age to transition to adult focused care every year this is an area that all pediatric providers can agree is important [3].
Methods
Overview and study population
Our target population was sickle cell centers in the US that care for pediatric patients and are large enough (~100 pediatric patients) to need a standardized transition program. We sought to describe the practices of the centers, rather than individual practitioners or clinic sites, so there was a single response per center. We anticipated that survey respondents would either be the center director, the sickle cell service director, or someone they designated as knowledgeable about transition practices in their program.
Identification of participants
There is no single national registry of sickle cell centers. We began with a list of potential sickle cell centers with pediatric patients by using disease specific websites (the Sickle Cell Disease Association of America website, the NHLBI Comprehensive Sickle Cell Centers website and the NIH clinical trials website), and professional organizations [25,26]. We looked at the website of each center to verify that it cared for pediatric sickle cell patients and was not part of another identified center. Contact information for the center director was obtained from individual program websites, through membership in a national organization or by personal knowledge. To ensure that we had correctly identified centers as caring for pediatric patients, we included a screening question in the survey, which eliminated three centers that reported not having pediatric patients. The final list consisted of 45 pediatric sickle cell centers.
Survey development
We began with a validated published survey of national CF centers, which had been developed after extensive review of the transition literature [27]. We revised the survey with input from local experts to address specific needs of the pediatric sickle cell population. The final survey was pilot tested by nine clinicians (pediatric hematologists or other pediatric specialists with an interest in transition) and further revisions were made as a result of that work. Survey domains included the following: transition logistics, identifying an adult provider, patient readiness for transition and preparation, transition program and evaluation, and patient and program demographics. The final survey contained 29 close-ended questions (including one screening question) and four open-ended questions. The survey was exempt from review by the Children’s Hospital of Bos-ton Institutional Review Board. See Supporting Information for complete survey.
Survey administration
The survey was constructed and administered electronically using Survey Monkey [28]. Before sending the survey, we sent an introductory e-mail to the directors of each identified center to notify them of the upcoming survey. We asked them to provide an alternate name and contact information if there was someone else they would prefer to respond to the survey. We sent out a personal link to the survey electronically, with two reminder e-mails. For those centers that had still not responded after these reminders, an e-mail invitation to complete the survey was sent to another clinician at that center.
Survey analysis
All surveys were completed online, and the descriptive analysis of responses was done through the SurveyMonkey.com internal data analysis program.
Supplementary Material
Acknowledgments
Contract grant sponsor: AHRQ T32 NRSA; Contract grant number: HS000063; Contract grant sponsor: NIH K24; Contract grant number: HL004184; Contract grant sponsor: Harvard Pediatric Health Services Research Fellowship
Footnotes
Conflict of interest: Nothing to report.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, Klug PP. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994;330:1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- 2.Quinn CT, Rogers ZR, McCavit TL, Buchanan GR. Improved survival of children and adolescents with sickle cell disease. Blood. 115:3447–3452. doi: 10.1182/blood-2009-07-233700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304–1306. [PubMed] [Google Scholar]
- 4.National Institutes of Health, National Heart, Lung, and Blood Institute, Division of Blood Diseases and Resources. The Management of Sickle Cell Disease. 4. Bethesda, MD: National Institutes of Health, National Heart, Lung, and Blood Institute; 2002. [Accessed December 1st, 2010]. NIH Publication No. 02-2117. Available at: www.nhlbi.nih.gov/health/prof/blood/sickle/sc_mngt.pdf. [Google Scholar]
- 5.Brousseau DC, Panepinto JA, Nimmer M, Hoffmann RG. The number of people with sickle-cell disease in the United States: national and state estimates. Am J Hematol. 85:77–78. doi: 10.1002/ajh.21570. [DOI] [PubMed] [Google Scholar]
- 6.Platt OS, Thorington BD, Brambilla DJ, Milner PF, Rosse WF, Vichinsky E, Kinney TR. Pain in sickle cell disease. Rates and risk factors. N Engl J Med. 1991;325:11–16. doi: 10.1056/NEJM199107043250103. [DOI] [PubMed] [Google Scholar]
- 7.Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Hartzema AG. The cost of health care for children and adults with sickle cell disease. Am J Hematol. 2009;84:323–327. doi: 10.1002/ajh.21408. [DOI] [PubMed] [Google Scholar]
- 8.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 303:1288–1294. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- 9.Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, Slap GB. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- 10.Telfair J, Myers J, Drezner S. Transfer as a component of the transition of adolescents with sickle cell disease to adult care: adolescent, adult, and parent perspectives. J Adolesc Health. 1994;15:558–565. doi: 10.1016/1054-139x(94)90139-t. [DOI] [PubMed] [Google Scholar]
- 11.Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005;115:112–120. doi: 10.1542/peds.2004-1321. [DOI] [PubMed] [Google Scholar]
- 12.Brumfield K, Lansbury G. Experiences of adolescents with cystic fibrosis during their transition from paediatric to adult health care: a qualitative study of young Australian adults. Disabil Rehabil. 2004;26:223–234. doi: 10.1080/09638280310001644924. [DOI] [PubMed] [Google Scholar]
- 13.Hauser ES, Dorn L. Transitioning adolescents with sickle cell disease to adult-centered care. Pediatr Nurs. 1999;25:479–488. [PubMed] [Google Scholar]
- 14.McPherson M, Thaniel L, Minniti CP. Transition of patients with sickle cell disease from pediatric to adult care: Assessing patient readiness. Pediatr Blood Cancer. 2009;52:838–841. doi: 10.1002/pbc.21974. [DOI] [PubMed] [Google Scholar]
- 15.Telfair J, Ehiri JE, Loosier PS, Baskin ML. Transition to adult care for adolescents with sickle cell disease: results of a national survey. Int J Adolesc Med Health. 2004;16:47–64. doi: 10.1515/ijamh.2004.16.1.47. [DOI] [PubMed] [Google Scholar]
- 16.Telfair J, Alexander LR, Loosier PS, Alleman-Velez PL, Simmons J. Providers' perspectives and beliefs regarding transition to adult care for adolescents with sickle cell disease. J Health Care Poor Underserved. 2004;15:443–461. doi: 10.1353/hpu.2004.0049. [DOI] [PubMed] [Google Scholar]
- 17.Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124:e1134–1141. doi: 10.1542/peds.2009-0041. [DOI] [PubMed] [Google Scholar]
- 18.Annunziato RA, Emre S, Shneider B, Barton C, Dugan CA, Shemesh E. Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatr Transplant. 2007;11:608–614. doi: 10.1111/j.1399-3046.2007.00689.x. [DOI] [PubMed] [Google Scholar]
- 19.Treadwell M, Telfair J, Gibson RW, Johnson S, Osunkwo I. Transition from pediatric to adult care in sickle cell disease: Establishing evidence-based practice and directions for research. Am J Hematol. doi: 10.1002/ajh.21880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wojciechowski EA, Hurtig A, Dorn L. A natural history study of adolescents and young adults with sickle cell disease as they transfer to adult care: a need for case management services. J Pediatr Nurs. 2002;17:18–27. doi: 10.1053/jpdn.2002.30930. [DOI] [PubMed] [Google Scholar]
- 21.Kral MC, Brown RT, Nietert PJ, Abboud MR, Jackson SM, Hynd GW. Transcranial Doppler ultrasonography and neurocognitive functioning in children with sickle cell disease. Pediatrics. 2003;112:324–331. doi: 10.1542/peds.112.2.324. [DOI] [PubMed] [Google Scholar]
- 22.Cystic Fibrosis Foundation. Bethesda, MD: updated 5/27/2010; cited Dec 1st, 2010. Available from: http://www.cff.org. [Google Scholar]
- 23.Smith LA, Oyeku SO, Homer C, Zuckerman B. Sickle cell disease: a question of equity and quality. Pediatrics. 2006;117:1763–1770. doi: 10.1542/peds.2005-1611. [DOI] [PubMed] [Google Scholar]
- 24.Telfair J, Haque A, Etienne M, Tang S, Strasser S. Rural/urban differences in access to and utilization of services among people in Alabama with sickle cell disease. Public Health Rep. 2003;118:27–36. doi: 10.1093/phr/118.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sickle Cell Disease Association of America. Baltimore, MD: Comprehensive Sickle Cell Centers, Universities & Institutions; updated 2005, cited Dec 1st, 2010. Available from: http://www.sicklecelldisease.org/members/honorary.phtml. [Google Scholar]
- 26.Sickle Cell Disease Information Center. National Heart Lung and Blood Institute, National Institutes of Health; Bethesda, MD: updated Nov 15, 2010, cited Dec 1st, 2010. available from: http://www.nhlbi.nih.gov/new/sicklecell.htm. [Google Scholar]
- 27.McLaughlin SE, Diener-West M, Indurkhya A, Rubin H, Heckmann R, Boyle MP. Improving transition from pediatric to adult cystic fibrosis care: lessons from a national survey of current practices. Pediatrics. 2008;121:e1160–1166. doi: 10.1542/peds.2007-2217. [DOI] [PubMed] [Google Scholar]
- 28.Survey Monkey. Palo Alto, California, USA: SurveyMonkey.com, LLC; www.surveymonkey.com. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.