A 1-year-old girl was referred to us for evaluation of some small painless papules on the scalp. The first lesion was noted by her mother in the first few days after the birth, but other similar lesions progressively appeared and significantly increased in size.
She was the third child, born at term through a vaginal delivery that did not require instrumentation after an uncomplicated pregnancy. There was no history of trauma. Her medical and family histories were unremarkable.
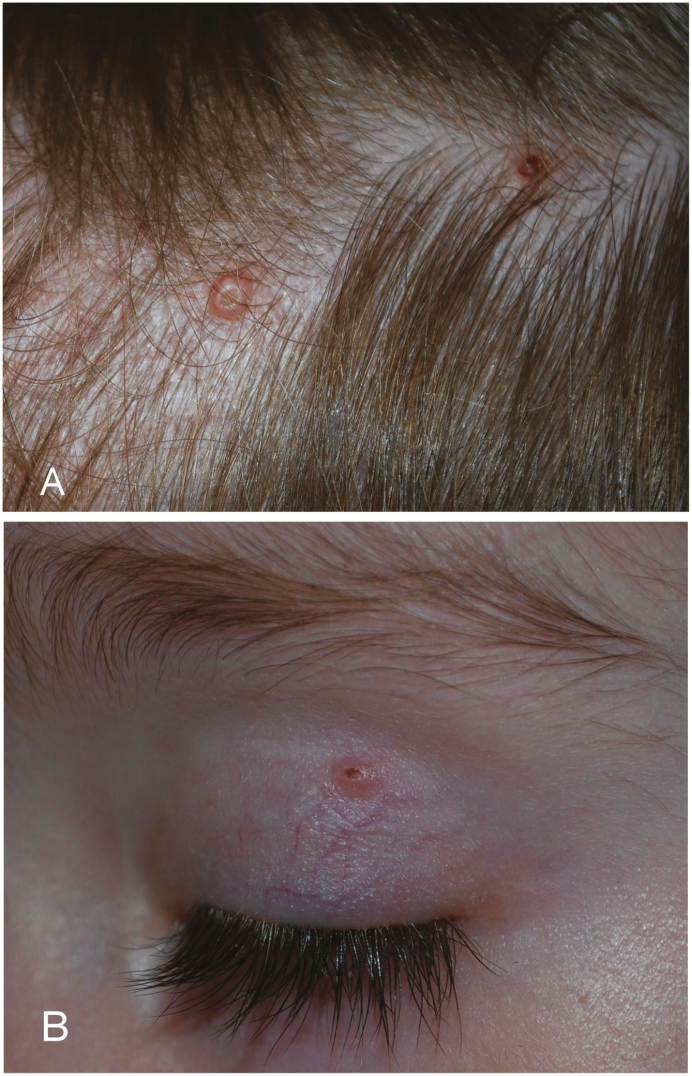
Physical examination revealed three translucent, glossy, dome-shaped papules, ranging from 2 mm to 3 mm, localized on the parietal (Figure 1A) and temporal region and another one on her left eyelid (Figure 1B). This latter appeared some weeks after the other lesions.
Figure 1.
Clinical appearance of molluscum contagiosum infection: two translucent, glossy, dome-shaped papules on the parietal (A) and one on her left eyelid (B)
DISCUSSION
Clinical examination suggested the diagnosis of molluscum contagiosum (MC), histologically confirmed after a curettage. Nobody else in her family presented MC and the mother did not remember having had similar lesions.
MC infection is a common cutaneous viral infection caused by a double-stranded DNA virus of the pox virus family that can affect skin and mucous membranes (1). It is very frequent in school-age children (1). The congenital or early-onset MC appearance is unusual and only a few cases have been previously reported (1,2). Usually MC occurs from person-to-person transmission and self-inoculation is common. Vertical transmission in utero or through the birth canal must be considered in congenital or early-onset MC even if the mother is asymptomatic (1,2). In cases of congenital MC, the lesions typically appear on the scalp. Prolonged rupture of membranes and protracted labour may be factors in transmission. More fragile skin or atopic dermatitis with an altered barrier function may be more susceptible to infection (1). Considering the incubation period ranging from 2 to 8 weeks (2), the lesions may be congenital or may appear in the first 2 to 3 months of life. Dermatologists and paediatricians should be aware that MC infection can be congenital and a proper diagnosis is useful to a timely treatment and to avoid parental concerns.
CLINICAL PEARLS
The congenital onset of molluscum contagiosum is an unusual but reported presentation of a common skin infection.
A vertical transmission in utero or through the birth canal must be considered, even if the mother is asymptomatic.
More fragile skin or atopic dermatitis with an altered barrier function may be more susceptible to infection.
Acknowledgement
The authors have no conflict of interest to disclose.
References
- 1. Berbegal-DeGracia L, Betlloch-Mas I, DeLeon-Marrero FJ, Martinez-Miravete MT, Miralles-Botella J. Neonatal molluscum contagiosum: Five new cases and a literature review. Australas J Dermatol 2015;56:e35–8. [DOI] [PubMed] [Google Scholar]
- 2. Ujiie H, Aoyagi S, Hirata Y, Osawa R, Shimizu H. Linear congenital molluscum contagiosum on the coccygeal region. Pediatr Dermatol 2013;30:e83–4. [DOI] [PubMed] [Google Scholar]