Abstract
Background
We describe a pediatric patient who suffered from critical abdominal distention caused by a combination of humidified, high-flow nasal cannula (HHFNC) oxygen therapy and nasal airway.
Case presentation
A 21-month-old boy with a history of chronic lung disease was admitted to the intensive care unit (ICU). Immediately after admission, his airway was established using a tracheal tube and mechanical ventilation was started. Five days after the commencement of mechanical ventilation, finally, his trachea was extubated. Immediately after extubation, HHFNC therapy at 20 L/min with an FiO2 of 0.35 was applied. However, severe stridor was observed, then a nasal airway was placed in the left nostril. However, he became restless. Critical abdominal distention was observed. A subsequent chest X-ray revealed that the nasal airway was placed too deeply, and the gastrointestinal air was severely accumulated. Immediately, the nasal airway was removed, and HHFNC flow was reduced to 10 L/min. Frequent suctioning and continuous gastric drainage were required, which achieved gradual improvement of respiratory condition.
Conclusions
We need to recognize that HHFNC therapy is one of the positive pressure ventilation system. Therefore, HHFNC therapy might cause the similar adverse events to noninvasive pressure ventilation.
Keywords: Humidified, High-flow nasal cannula, Abdominal distention, Nasal airway, Complication, Pediatric patient
Background
Humidified, high-flow nasal cannula (HHFNC) oxygen therapy has allowed optimal humidification of inspired gas at high flows, which could create a distending pressure-like nasal continuous positive airway pressure (CPAP) [1]. There is a small but growing body of information from clinical trials that support the use of HHFNC as an alternative oxygen interface for critically ill patients across the entire age spectrum, from premature neonates to adults [2–4]. In addition, it has been reported that HHFNC is equivalent to more traditional non-invasive ventilation support, such as continuous or bi-level positive airway pressure (CPAP or BiPAP) [3, 4]. Therefore, HHFNC has become a popular and easy respiratory option for pediatric patients despite the lack of clear practical guidance for safety operation. We describe a pediatric patient who suffered from critical abdominal distention caused by a combination HHFNC therapy and nasal airway.
Case presentation
The consent of patient’s next of kin was obtained; however, institutional review board approval was exempted because neither the ethical problem nor the description to identify the patient was included in this case report. A 21-month-old boy with acute or chronic lung disease was admitted to the intensive care unit (ICU). He was 63 cm in height and weighed 7.9 kg. He was bone on the 24th week of gestation and weighed 645 g and had been provided with home oxygen therapy with 3 L/min oxygen administration. His chest computed tomography showed several giant bullae in the bilateral lungs (Fig. 1). He had gastroesophageal reflux and an intestinal feeding tube (6.5 F) and a gastric drainage tube (6 F) indwelled.
Fig. 1.
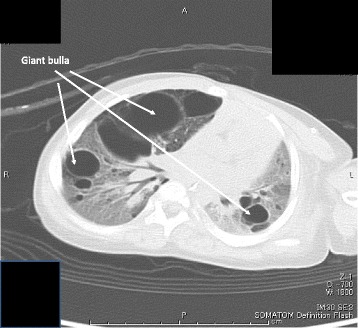
A chest CT at healthy status. Several giant bullae in the bilateral lungs were observed
He had been suffering from upper respiratory infection and fever for a couple of days. He gradually developed hypoxia (SpO2 < 90%) with oxygen administration. Immediately after admission, his airway was established using a cuffed 3.5-mm tracheal tube. Immediately after the beginning of mechanical ventilation, 10-cm H2O positive end-expiratory pressure (PEEP) combined with moderate pressure support (8 cm H2O) was applied.
His respiratory status gradually improved. Five days after the commencement of mechanical ventilation, finally, his trachea was extubated. Immediately after extubation, HHFNC therapy at 20 L/min with an FiO2 of 0.35 (Optiflow system™, MR850 heated humidified RT202 delivery tubing; Fisher and Paykel Healthcare Ltd., Auckland, New Zealand) was applied through nasal cannula (Optiflow™ Junior Nasal Cannula Infant; Fisher & Paykel, Auckland, New Zealand).
However, severe stridor because of upper airway obstruction was observed, then a 10-cm-long 3.5-mm hand-made nasal airway (Portex™, Smith Medical, Kent, UK) was placed in the left nostril (10 cm depth). It was not confirmed whether or not inserting the tube too deeply because he violently resisted being checked with a laryngoscopy. But, stridor or retractive breathing was not observed. Therefore, HHFNC therapy was restarted with this airway position.
HHFNC was conducted smoothly for a while; however, he became restless and then started agonizing heavily with SpO2 reduction down to 70%. Critical abdominal distention was observed, and forced gastric drainage was started through a gastric tube. However, the critical situation was not improved. A subsequent chest X-ray revealed that the nasal airway was placed too deeply (Fig. 2), and the gastrointestinal air was severely accumulated (Fig. 3).
Fig. 2.
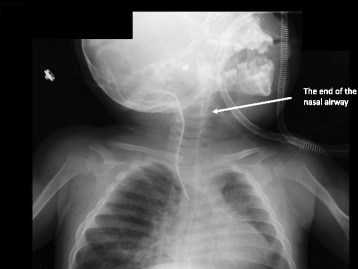
A cervical X-ray at deteriorated respiratory status. A subsequent cervical X-ray revealed that the nasal airway was placed too deeply
Fig. 3.
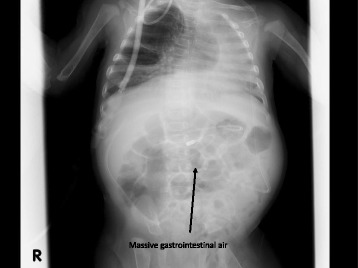
A chest-abdominal X-ray at deteriorated respiratory status. A subsequent chest-abdominal X-ray revealed that gastrointestinal air was severely accumulated
Immediately, the nasal airway was removed and HHFNC flow was reduced to 10 L/min. Frequent suctioning and continuous gastric drainage were required, which achieved gradual improvement of respiratory condition. Finally, HHFNC therapy was successfully terminated.
Conclusions
It is supposed that the deeply inserted nasal airway caused critical abdominal distention by insufflating the HHFNC flow into the gastrointestinal rather than the respiratory tract. In the early stage before the development of critical abdominal distention, the HHFNC flow might have partially supported his breathing; however, it is likely that the HHFNC flow gradually became ineffective for supporting his breathing because of aerophagia. In addition, his gastroesophageal reflux might have worsened the situation because aerophagia is possibly accelerated by noninvasive positive airway pressure in patients with gastroesophageal reflux [5]. Abdominal compartment syndrome related to noninvasive ventilation was also reported [6]. In a pediatric model, a linear relationship between flow and pressures measured in the pharynx (pressure = − 0.375 + 0.138 × flow) with the closed-mouth condition was reported. According to this model, 2.4 cm H2O of positive pressure was generated in our patient at that time. This low level of pressure might unusually force air into the stomach; however, the positive pressure drastically increased with a high nasal prong-to-nares ratio and mouth closed status [7]. Therefore, it might be a little wonder that a positive pressure high enough to open the esophageal sphincter was generated according to the circumstances, which caused the gastrointestinal overdistention. To confirm the location of the tip of the nasal airway, we could have used a fine fiberoptic bronchoscopy as an option. We should have carefully monitored the patient considering the development of this adverse event.
In conclusion, we need to recognize that HHFNC therapy is one of the positive pressure ventilation system. Therefore, HHFNC therapy might cause the similar adverse events to noninvasive pressure ventilation. This time, we would like to underline that critical abdominal overdistention could happen by HHFNC therapy.
Acknowledgements
None
Funding
This study was supported only by the department.
Availability of data and materials
Not applicable
Abbreviations
- BiPAP
Bi-level positive airway pressure
- CPAP
Continuous positive airway pressure
- HHFNC
Humidified, high-flow nasal cannula
- ICU
Intensive care unit
- PEEP
Positive end-expiratory pressure
Authors’ contributions
All authors were involved in the treatment of the patient. SI and YT collected the patient’s data, drafted the manuscript, and obtained the consent for publication from the patient’s next of kin. SS, JE, and MK revised and edited the manuscript. All authors contributed and approved the final version of this manuscript.
Ethics approval and consent to participate
The consent of patient’s next of kin was obtained; however, institutional review board approval was exempted because neither the ethical problem nor the description to identify the patient was included in this case report.
Consent for publication
The consent for publication was obtained from the patient’s next of kin.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC. Observational study of humidified high-flow nasal cannula compared with nasal continuous positive airway pressure. J Pediatr. 2009;154:177–182. doi: 10.1016/j.jpeds.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 2.Kepreotes E, Whitehead B, Attia J, Oldmeadow C, Collison A, Searles A, Goddard B, Hilton J, Lee M, Mattes J. High-flow warm humidified oxygen versus standard low-flow nasal cannula oxygen for moderate bronchiolitis (HFWHO RCT): an open, phase 4, randomised controlled trial. Lancet. 2017;389:930–939. doi: 10.1016/S0140-6736(17)30061-2. [DOI] [PubMed] [Google Scholar]
- 3.Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard JC, Brochard L, Robert R, FLORALI Study Group; REVA Network High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 4.Kotecha SJ, Adappa R, Gupta N, Watkins WJ, Kotecha S, Chakraborty M. Safety and efficacy of high-flow nasal cannula therapy in preterm infants: a meta-analysis. Pediatrics. 2015;136:542–553. doi: 10.1542/peds.2015-0738. [DOI] [PubMed] [Google Scholar]
- 5.Shepherd K, Hillman D, Eastwood P. Symptoms of aerophagia are common in patients on continuous positive airway pressure therapy and are related to the presence of nighttime gastroesophageal reflux. J Clin Sleep Med. 2013;9:13–17. doi: 10.5664/jcsm.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Keulenaer BL, De Backer A, Schepens DR, Daelemans R, Wilmer A, Malbrain ML. Abdominal compartment syndrome related to noninvasive ventilation. Intensive Care Med. 2003;29:1177–1181. doi: 10.1007/s00134-003-1806-z. [DOI] [PubMed] [Google Scholar]
- 7.Sivieri EM, Gerdes JS, Abbasi S. Effect of HFNC flow rate, cannula size, and nares diameter on generated airway pressures: an in vitro study. Pediatr Pulmonol. 2013;48:506–514. doi: 10.1002/ppul.22636. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable


