Abstract
Background:
Hyperbilirubinemia is a common neonatal condition requiring timely management to prevent acute bilirubin encephalopathy. Management protocols allow nonphysicians to initiate designated actions prior to physician assessment.
Objective:
To assess the effectiveness of a nurse-initiated neonatal jaundice management protocol for serum bilirubin sampling and phototherapy for neonates presenting with hyperbilirubinemia to the Paediatric Emergency Department (PED).
Methods:
A health records review was performed for jaundiced neonates 12 months prior to the introduction of the management protocol (control period) and 12 months after (intervention period). Randomly selected charts were evaluated for time to serum bilirubin sampling, phototherapy initiation, ED length of stay, admission rate, completion of direct antiglobulin test and nursing documentation.
Results:
Two hundred and sixty-six neonates (131 control and 135 intervention) were included. Median time to serum bilirubin sampling was reduced by 22% (36 min versus 28 min; P<0.001) with 34 min difference at the 90th percentile (94 min [95% confidence interval (CI) 63.7 to 116.9] versus 60 min [95% CI 49.0 to 78.2]). Statistically significant improvements were found in time to phototherapy initiation (127 min [95% CI 72.0 to 160.7] versus 65 min [95% CI 50.0 to 72.4] at 90th percentile), ED length of stay (267 min [95% CI 180.9 to 292.9] versus 216 min [95% CI 171.1 to 247.4] at 90th percentile) and hospital admissions (36% versus 17%; P<0.001). Improvements were also observed in direct antiglobulin test measurement (P<0.001) and nursing documentation (P=0.017)
Conclusions:
Implementation of a PED neonatal jaundice management protocol was associated with improved timeliness and standardization of care for this common and important condition.
Keywords: Emergency department, Hyperbilirubinemia, Infant, Jaundice, Management protocol.
Many of the two-thirds of neonates who develop jaundice in the first weeks of life present to the Paediatric Emergency Department (PED) for management (1,2). Though the majority of jaundice cases are benign and self-limited, acute bilirubin encephalopathy still occurs in approximately 1 in 10,000 live births (1,3,4).
National and international neonatal hyperbilirubinemia practice guidelines have emphasized timely interventions for prevention of neurological complications (1–3). PED overcrowding may contribute to delayed assessments, serum bilirubin sampling and phototherapy initiation for neonates with severe hyperbilirubinemia (4). Clinical pathways operationalize best evidence guidelines into accessible bedside formats for health care provider teams (5). Management protocols, also known as standing orders or medical directives, further improve the effectiveness of clinical pathways by delegating authority for nonphysician implementers to perform designated actions prior to physician assessment, thus facilitating timely care (6). Studies evaluating PED nurse-initiated clinical pathways and management protocols have demonstrated significant outcome improvements for acutely ill patients (5,7–9).
A study evaluating a PED neonatal jaundice clinical pathway demonstrated improved times to phototherapy, bloodwork and decreased length of stay (4). The median time from triage to serum bilirubin sampling and phototherapy in this study was greater than 1 h. The authors noted that additional improvements could be accomplished by implementing a management protocol to permit nurse-initiated bloodwork and phototherapy prior to physician assessment (4).
The goal of our study was to assess the impact of a nurse-initiated management protocol for jaundiced neonates in the PED. We hypothesized that a protocol authorizing serum bilirubin sampling and phototherapy initiation prior to physician assessment would be associated with a 20% reduction in time to serum bilirubin sampling. We further hypothesized that this would be associated with decreased time to phototherapy and ED length of stay (LOS).
METHODS
Study setting and population
This study was performed in the Children’s Hospital of Eastern Ontario (CHEO) ED, a tertiary care centre with 68,000 visits and approximately 400 neonatal jaundice cases annually. Eligibility criteria included neonates of any gestational age, 0 to 28 days, on first presentation with the chief complaint of jaundice or hyperbilirubinemia identified by primary care provider, parental report or triage assessment. Neonates were excluded if they required resuscitation (Pediatric Canadian Triage and Acuity Scale [PaedCTAS] 1) or had serum bilirubin level measured by a primary care provider immediately prior to PED presentation (10).
Existing standard of care (control period)
Prior to the protocol, neonatal jaundice management was variable in our PED. Verbal orders were commonly employed and phototherapy was initiated either at the time of serum bilirubin sampling or after bilirubin results were known. Medical trainees often performed initial assessments followed by staff physician review, potentially leading to management delays.
Development of neonatal jaundice management protocol
Our PED supports the expansion of the nursing role through nurse-initiated management protocols (11,12). As a patient safety initiative to standardize quality of care for jaundiced neonates, a multidisciplinary team of ED nurses and physicians developed the management protocol (available from the corresponding author by request). Previously published institutional guidelines for management protocol implementation were followed (11).
The management protocol instructs the triage nurse to assign a triage level of ‘PaedCTAS 2 – Emergent’ (10). Within 15 minutes of patient arrival, the bedside nurse provides parental education, obtains consent and blood via heelstick for serum bilirubin and direct antiglobulin test (DAT) and initiates high-intensity phototherapy (Olympic Bili-Bassinet; 30 to 35 µW/cm2/nm). Neonates remain under phototherapy with continuous temperature monitoring and eye shielding until the serum bilirubin level is resulted and reviewed by the physician. For febrile, jaundiced neonates, the Jaundice Management Protocol was used in conjunction with our institution’s Febrile Neonate/Rule Out Sepsis Management Protocol.
Study design
Health record reviews were performed for eligible neonates over a 25-month period: 12 months prior to management protocol initiation (control period, October 1, 2010 to September 30, 2011) and 12 months after (intervention period, November 1, 2011 to October 31, 2012). The study periods were separated by a ‘training period’ (October 2011). Twelve-month study periods were chosen to minimize seasonal variation in PED volumes.
Relevant charts were identified using ICD-10-A coding for neonatal jaundice and hyperbilirubinemia. One reviewer screened the charts for inclusion/exclusion criteria and abstracted relevant data using a standardized data collection form. Ten per cent of the charts were reviewed by a second reviewer. Data were entered into a customized database created in REDCap, a secure, web-based application for data capture in research studies (13). Ethics approval was obtained through the CHEO Research Ethics Board.
Measures
The primary outcome was median and 90th percentile time from triage assessment to serum bilirubin sampling documented in the electronic health record. Secondary outcomes included median and 90th percentile times from triage assessment to phototherapy initiation, total ED LOS, admission rate, rate of DAT sampling and completion of nursing documentation for time of bilirubin sampling and phototherapy initiation. If phototherapy initiation was not documented, we classified the patient as having not received phototherapy. DAT sampling was included to identify patients with isoimmune hemolytic disease in order to classify risk of kernicterus.
Sample size estimation
The ideal time to bloodwork and phototherapy initiation for jaundiced neonates is undefined in the literature; thus a 20% time reduction to these interventions was deemed to be clinically significant based on expert opinion. A prestudy chart audit examining 100 randomly selected charts (50 control and 50 intervention) was performed to inform our sample size calculation. Median time to serum bilirubin sampling in the pilot intervention sample was 31 minutes compared to 39 minutes in the control period, a 20.5% reduction. Since the time to serum bilirubin sampling was skewed, a log transformation was used, resulting in an approximate Gaussian distribution with a standard deviation of 0.61. In order to have 80% power to detect this reduction, with probability of type-I error fixed at 5%, a minimum of 119 charts from control and intervention periods were required. We randomly selected 140 charts from all eligible neonatal jaundice visits during the control and intervention periods using a computer-generated random sample.
Data analysis
Patient characteristics were examined using descriptive statistics. For categorical variables, frequencies and percentages were computed. For continuous variables, mean (standard deviation), median (interquartile range [IQR]) and range were computed. To test for patient differences between the control and intervention periods in categorical variables, the chi-square or Fisher’s exact test was used. The continuous variable of age was compared using the Student’s t test.
Times from triage to serum bilirubin sampling, phototherapy initiation and ED LOS were summarized using median and IQR. For the primary and secondary outcome analyses, times from triage to serum bilirubin sampling, phototherapy initiation and discharge were compared using the Mann–Whitney U test. Two-sided P values less than 0.05 were considered statistically significant. Because time from triage to serum bilirubin sampling was skewed, the difference in the 90th percentile in the control and intervention periods was further used to describe group differences in times at the upper end of the distribution. Completeness of documentation was compared using Pearson’s chi-square test.
Serum bilirubin levels according to postnatal age in hours and kernicterus risk factors were used to determine qualification for exchange transfusion (ET) (2). Neonates were classified as low risk (>38 weeks and well), medium risk (>38 weeks and risk factors or 35 to 37 6/7 weeks and well) or high risk (35 to 37 6/7 weeks and risk factors). A Fisher’s exact test was used to determine whether the number of neonates meeting ET criteria differed between control and intervention periods. Postnatal age in hours was calculated by taking the difference between triage date/time and birth date/time, rounding to the nearest 6 h. When birth time was not available, the baby was considered born at 12:00 in order to provide an estimate of age in hours.
All statistical analyses were performed using SPSS 22.0 (SPSS, Inc., Chicago, IL).
RESULTS
Patient characteristics
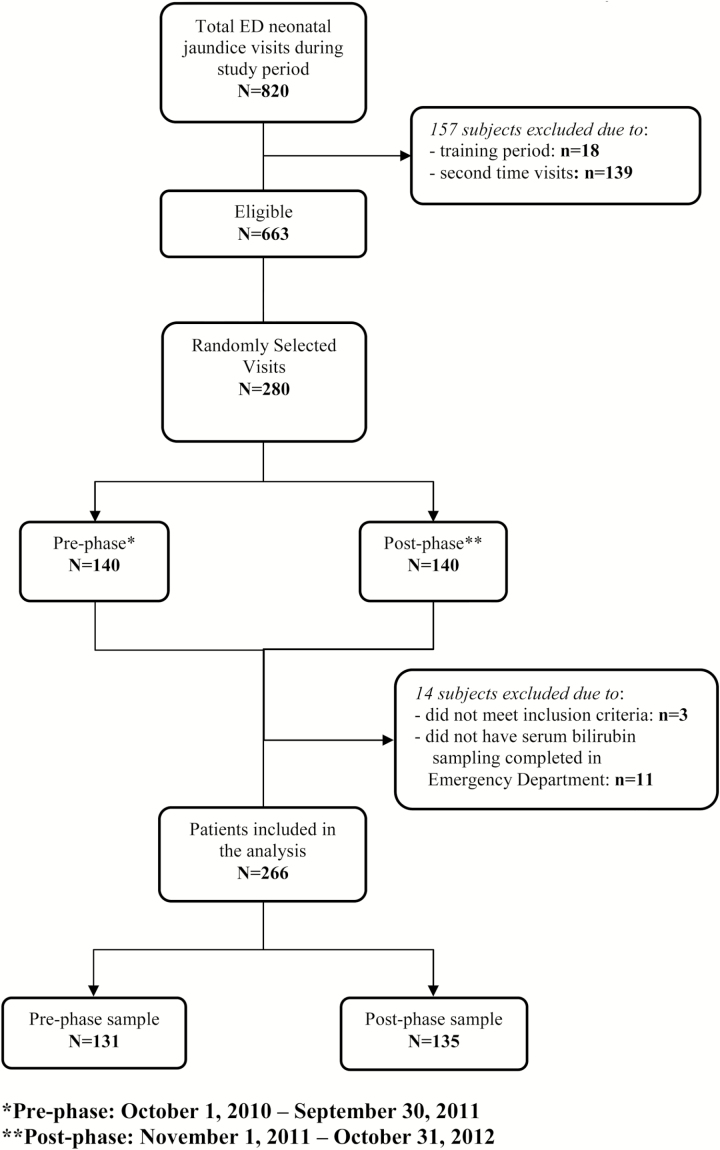
During the study periods, 820 jaundiced neonates were seen in the PED of which 280 were randomly selected for review. Of these, 266 neonates were included in the study (131 neonates in the control group and 135 in the intervention group, Figure 1). Patient characteristics are described in Table 1. There was a statistically significant difference in the serum bilirubin levels in the control group (277 µmol/L, IQR: 231 to 309 µmol/L) compared to the intervention group (247 µmol/L, IQR: 206 to 288 µmol/L) (P<0.001). After adjusting for ‘home-initiated’ versus ‘referred’ visit types in the control and intervention groups with a two-way Analysis of Variance (ANOVA), a statistically significant decreased serum bilirubin level was still present. There was 100% agreement between reviewers for gender, disposition, dates of visit, triage assessment, documentation of phototherapy initiation and serum bilirubin sampling. Inter-rater reliability was almost perfect for time of triage assessment (κ=0.85) and time of serum bilirubin sampling (κ=0.88) and substantial for time of discharge (κ=0.67) and time of phototherapy initiation (κ=0.75).
Figure 1.
Flow diagram of participants recruited into the study.
Table 1.
Demographic characteristics
| Pre (N=131) | Post (N=135) | P value | |
|---|---|---|---|
| N (%) | |||
| Age (days) (mean±SD) | 6.07 ± 4.18 | 6.12 ± 4.28 | 0.92a |
| Gender | |||
| Female | 58 (44.3) | 50 (37.0) | 0.23b |
| Male | 73 (55.7) | 85 (63.0) | |
| Gestational age | |||
| 35–37 + 6 days | 29 (26.1) | 23 (20.5) | 0.32b |
| >38 weeks | 82 (73.9) | 89 (79.5) | |
| PaedCTAS code | |||
| 1 | 0 (0.0) | 0 (0.0) | 0.37b |
| 2 | 129 (98.5) | 132 (97.8) | |
| 3 | 1 (0.8) | 3 (2.2) | |
| 4 | 1 (0.8) | 0 (0.0) | |
| 5 | 0 (0.0) | 0 (0.0) | |
| Visit type | |||
| Home initiated | 53 (40.5) | 67 (49.6) | 0.25b |
| Referred | 77 (58.8) | 66 (48.9) | |
| Not documented | 1 (0.8) | 2 (1.5) | |
| Feeding type | |||
| Breast fed | 79 (60.3) | 97 (71.9) | 0.13b |
| Formula fed | 9 (6.9) | 6 (4.4) | |
| Both breast fed and formula fed | 28 (21.4) | 16 (11.9) | |
| Not documented | 15 (11.5) | 16 (11.9) | |
| Phototherapy initiation | |||
| Yes | 75 (58.1) | 101 (74.8) | 0.004*,b |
| No | 54 (41.9) | 34 (25.2) | |
| First physician assessment | |||
| Medical student | 6 (4.6) | 7 (5.2) | 0.66b |
| Resident | 42 (32.1) | 43 (31.9) | |
| Fellow | 12 (9.2) | 9 (6.7) | |
| Staff | 39 (29.8) | 50 (37.0) | |
| Not documented | 32 (24.4) | 26 (19.3) | |
| Kernicterus risk zone | |||
| Low-risk | 83 (64.3) | 89 (66.4) | 0.92b |
| Medium-risk | 41 (31.8) | 36 (26.9) | |
| High-risk | 5 (3.9) | 9 (6.7) | |
aT test. bChi-square test. *P<0.05
Primary outcome
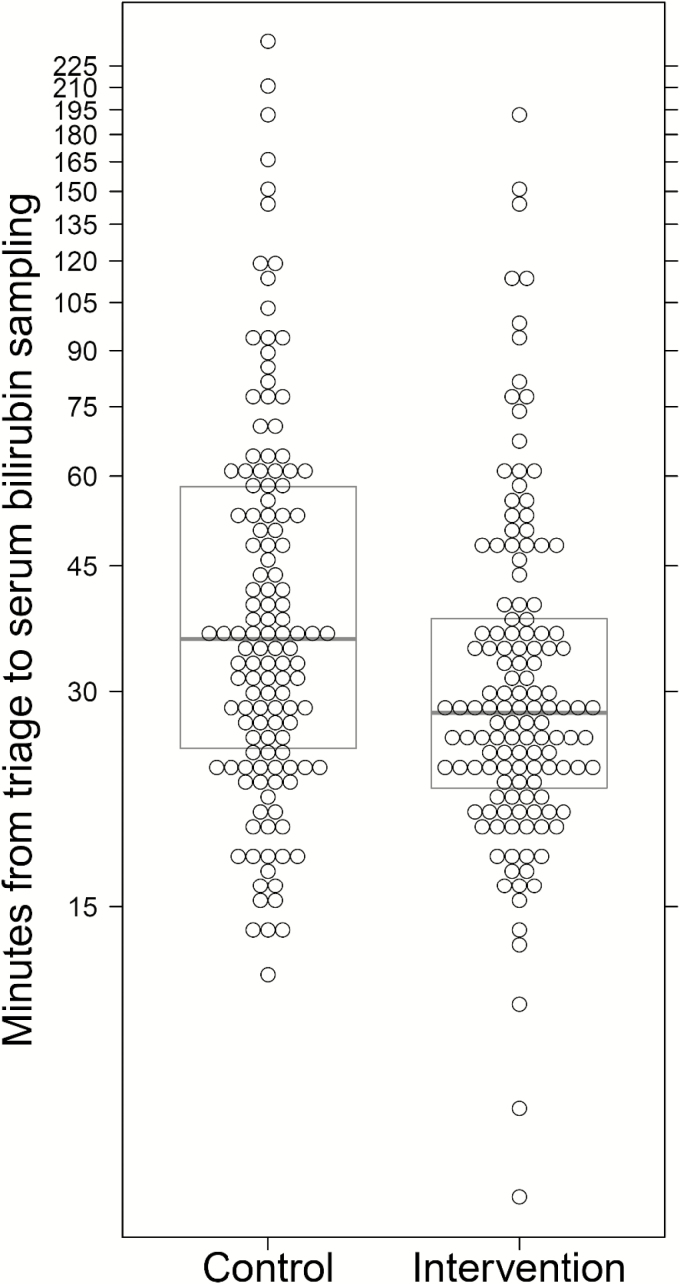
Clinical outcomes are described in Table 2. The intervention group had improved median time from triage to serum bilirubin sampling (36 minutes [IQR: 25 to 59] versus 28 minutes [IQR: 22 to 38], a 22.2% reduction [P=0.001], Figure 2). The 90th percentile of time from triage to serum bilirubin sampling was 94 minutes in the control group (95% confidence interval [CI] 63.7 to 116.9 minutes) compared to 60 minutes in the intervention group (95% CI 49.0 to 78.2 minutes).
Table 2.
Clinical outcomes
| Pre (N=131) | Post (N=135) | P value | |
|---|---|---|---|
| N (%) or median (IQR) | |||
| Serum bilirubin levels (µmol/L) | 277 (231–309) | 247 (206–288) | <0.001*,a |
| Disposition | |||
| Admitted | 47 (35.9) | 23 (17.0) | |
| Discharged | 84 (64.1) | 112 (83.0) | <0.001*,b |
| Serum bilirubin levels categorized by disposition (µmol/L) | |||
| Admitted | 314 (283–359) | 306 (266–377) | 0.68a |
| Discharged | 254 (223–289) | 240 (2001–264) | 0.014*,a |
| DAT completed | |||
| Yes | 45 (34.4) | 94 (69.6) | <0.001*,b |
| No | 86 (65.6) | 41 (30.4) | |
| DAT result | |||
| Positive | 2 (4.8) | 4 (4.4) | 0.94b |
| Negative | 40 (95.2) | 86 (95.6) | |
| Number of patients admitted to: | |||
| Ward | 41 (87.2) | 22 (95.7) | 0.27b |
| Neonatal Intensive Care Unit | 6 (12.8) | 1 (4.3) | |
| Pediatric Intensive Care Unit | 0 (0.0) | 0 (0.0) | |
| Patients meeting exchange | |||
| transfusion criteria | |||
| Yes | 7 (5.4) | 3 (2.2) | 0.21c |
| No | 122 (94.6) | 131 (97.8) | |
DAT direct antiglobulin test; IQR interquartile range.
aMann–Whitney U test. bChi-square test. cFisher’s exact test. *P<0.05
Figure 2.
Time from triage to serum bilirubin sampling in control and intervention periods. The vertical axis uses a log scaling. Individual times are represented by circles. For each period, the median (dark horizontal line) and 25th and 75th percentiles (top and bottom of the box) have been superimposed.
Secondary outcomes
Phototherapy initiation documentation was improved in the intervention group (101 [74.8%] versus 75 [57.2%]; P=0.004). Median time to phototherapy was 42 minutes (IQR: 26 to 70) in the control group compared to 34 minutes (IQR: 26 to 45) in the intervention group (P=0.032) with a decrease of 62 minutes at the 90th percentile (127 minutes [95% CI 72.0 to 160.7 minutes] versus 65 minutes [95% CI 50.0 to 72.4 minutes]).
While there was no significant difference in ED LOS between control and intervention periods (129 min [IQR: 99 to 179] versus 128 min [IQR: 94 to 184]; P=0.669), there was a statistically significant decrease in ED LOS for discharged neonates in the intervention period, with a median difference of 17 min (135 min [IQR 108 to 176] versus 118 min [IQR: 91 to 155]; P=0.011). The difference in 90th percentile ED LOS for discharged patients was 51 min (267 min [95% CI 180.9 to 292.9 min] versus 216 min [95% CI 171.1 to 247.4 min]). There were significantly fewer admissions to hospital in the intervention group compared to the control group (17% versus 35.9%; P<0.001). There was no significant difference between the number of neonates meeting ET criteria between the control and intervention periods (5.4% versus 2.2%; P=0.21).
DAT measurement significantly increased after management protocol initiation (34.4% versus 69.6%; P<0.001). Nursing documentation of therapies was significantly higher following management protocol implementation (54.6% versus 68.9%; P=0.017). There were no parental complaints, safety incidents or adverse events in regards to the protocol identified through the institutional Safety Reporting System during the study period.
DISCUSSION
A novel PED nurse-initiated neonatal jaundice management protocol was associated with reduced time to bloodwork, phototherapy, ED LOS for discharged patients and improved nursing documentation. These results are consistent with previous studies demonstrating the effectiveness of nurse-initiated treatments (5,8,9,11). Standardization of care and improved adherence to practice guidelines with protocol implementation may account for the decreased time to jaundice management.
Although most patients received timely bilirubin sampling and phototherapy prior to protocol implementation, there were a proportion of ‘outliers’ who experienced delays due to factors including physician availability, daily census and acuity in the PED. Protocol implementation was associated with a reduction in the 90th percentile times to bilirubin sampling and phototherapy by more than half an hour and an hour, respectively. We found a smaller decrease in median time to bilirubin sampling and phototherapy than Wolff et al. did postprotocol implementation (4). Time to these interventions at our institution in the control period was already substantially less than in Wolff’s study intervention period, likely reflecting the use of verbal orders.
ED overcrowding may lead to delayed treatment and prolonged ED LOS (6). Despite a 3.9% increase in patient census at our institution over the study period (with no concomitant increase in staffing), our time to serum bilirubin sampling and phototherapy initiation improved with the use of the management protocol. Admitted patients’ ED LOS may be impacted by bed availability and staffing. Excluding admitted patients, discharged neonates in the intervention period had a statistically significant decreased ED LOS. Use of the protocol was associated with a clinically significant reduction in ED LOS for patients at the 90th percentile by almost an hour.
Despite randomization, the intervention group had a significantly lower median serum bilirubin level and a lower admission rate. Since our management protocol only impacts initial PED care and the decision to admit is primarily based on the initial bilirubin level, this was an unexpected and interesting finding. Adjusting for visit type did not account for the difference in serum bilirubin levels. To our knowledge, there is no literature on how quickly serum bilirubin levels rise in untreated neonates with hyperbilirubinemia. Future prospective studies are required to investigate this association.
The possibility of over-diagnosis and treatment was carefully considered when creating the management protocol. Our intervention did not lead to more aggressive hyperbilirubinemia screening since only neonates presenting with jaundice qualified for the protocol. Prompt phototherapy initiation for every jaundiced neonate reduces the risk of severe hyperbilirubinemia. The known minimal risks associated with a brief period of phototherapy for neonates whose bilirubin levels do not require treatment is outweighed by the potential benefit of rapid initiation of phototherapy for neonates who do (4).
Limitations
Our study has several limitations. First, incomplete documentation impacted the full assessment of certain outcomes. Ideally, time to phototherapy initiation would have been used as our primary outcome; however, documentation of this measure was infrequent, particularly in the control period when phototherapy was initiated either with or after serum bilirubin sampling. After management protocol implementation, phototherapy was initiated at the time of bloodwork. Time to serum bilirubin sampling thus served as an accurate proxy for phototherapy initiation in the intervention period and underestimates the time to phototherapy during the control period. The full clinical impact of this management protocol on decreasing time to phototherapy is therefore likely underestimated in our study. Second, if phototherapy initiation was not documented in the chart, we classified the patient as having not received phototherapy. This incomplete documentation explains why phototherapy initiation was not seen in 100% of the neonates in the intervention group as expected and likely underestimates the number of infants started on phototherapy. Finally, our study was conducted at a single site and may not be generalizable to other centres. Further prospective studies should be undertaken to further assess the impact of this intervention.
CONCLUSIONS
Implementation of a neonatal jaundice management protocol for nurse-initiated serum bilirubin sampling and phototherapy initiation was associated with statistically significant improved time to interventions, with clinically significant improved times for patients at the 90th percentile. Jaundice management protocols for neonates presenting to PEDs have the potential to improve standardization and quality of care for this common and important condition.
Conflict of Interest
The authors have no conflicts of interest to disclose. The authors have no financial relationships relevant to this article to disclose.
Acknowledgements
Funding sources: Children’s Hospital of Eastern Ontario Research Institute, Resident Research Grant (internal funding), $2500.
References
- 1. Barrington KJ, Sankaran K; Canadian Paediatric Society. Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants. Paediatr Child Health. 2007;12(Suppl B): 1B-12B. [Google Scholar]
- 2. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297–316. [DOI] [PubMed] [Google Scholar]
- 3. National Collaborating Centre for Womens’ and Childrens’ Health. Recognition and Treatment of Neonatal Jaundice (NICE Clinical Guideline) 2012. <http://www.ncbi.nlm.nih.gov/pubmed/22132434>. Accessed October 18, 2014.
- 4. Wolff M, Schinasi DA, Lavelle J, Boorstein N, Zorc JJ. Management of neonates with hyperbilirubinemia: Improving timeliness of care using a clinical pathway. Pediatrics 2012;130:e1688–94. [DOI] [PubMed] [Google Scholar]
- 5. Jayaram A, Nagel RW, Jasty R. Impact of clinical pathway on quality of care in sickle cell patients. J Pediatr Hematol Oncol 2010;32:537–9. [DOI] [PubMed] [Google Scholar]
- 6. Qazi K, Altamimi SA, Tamim H, Serrano K. Impact of an emergency nurse-initiated asthma management protocol on door-to-first-salbutamol-nebulization-time in a pediatric emergency department. J Emerg Nurs 2010;36:428–33. [DOI] [PubMed] [Google Scholar]
- 7. Browne GJ, Giles H, McCaskill ME, Fasher BJ, Lam LT. The benefits of using clinical pathways for managing acute paediatric illness in an emergency department. J Qual Clin Pract 2001;21:50–5. [DOI] [PubMed] [Google Scholar]
- 8. Cheney J, Barber S, Altamirano L et al. A clinical pathway for bronchiolitis is effective in reducing readmission rates. J Pediatr 2005;147:622–6. [DOI] [PubMed] [Google Scholar]
- 9. Johnson KB, Blaisdell CJ, Walker A, Eggleston P. Effectiveness of a clinical pathway for inpatient asthma management. Pediatrics 2000;106:1006–12. [PubMed] [Google Scholar]
- 10. Warren DW, Jarvis A, LeBlanc L, Gravel J; CTAS National Working Group; Canadian Association of Emergency Physicians; National Emergency Nurses Affiliation; Association des Médecins d’Urgence du Québec; Canadian Paediatric Society; Society of Rural Physicians of Canada Revisions to the Canadian Triage and acuity scale paediatric guidelines (paedctas). CJEM 2008;10:224–43. [PubMed] [Google Scholar]
- 11. Zemek R, Plint A, Osmond MH et al. Triage nurse initiation of corticosteroids in pediatric asthma is associated with improved emergency department efficiency. Pediatrics 2012;129:671–80. [DOI] [PubMed] [Google Scholar]
- 12. Dixon A, Clarkin C, Barrowman N, Correll R, Osmond MH, Plint AC. Reduction of radial-head subluxation in children by triage nurses in the emergency department: A cluster-randomized controlled trial. Cmaj 2014;186(9):E317–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (redcap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]