Abstract
Background:
We recently reported an encouraging decline in the prevalence of overweight (OW) or obesity (OB) in Canadian children from 31% to 27% with stabilization in OB rates at ~13% using national survey data between 2004 and 2013. Although rates were lower for toddlers, girls and those of European (White) race-ethnicity, secular trends persisted after adjustment. In this follow-up study, we explored the ability of socioeconomic status to explain or modify these relationships using the same data set.
Methods:
We analyzed a decade of anthropometric data from 14,014 children aged 3 to 19 years. We explored the influence of income adequacy, education, immigration status, family type (e.g., single-parent) and geographic region by multivariable logistic regression. Data sets included Canadian Community Health Survey cycle 2.2 and Canadian Health Measures Surveys cycles 2 and 3.
Results:
Children from higher-income families fared better than their lower-income counterparts in each survey era and demonstrated a significant decline in OW/OB from 29.1% (95% confidence interval [CI]: 27.3 to 30.8) in 2004 to 2005 to 22.2% (95% CI: 19.8 to 24.6) in 2012 to 2013, P<0.001. Regression models confirmed the effects of time, age, sex, race, income, education, immigration and region. Although single-parent families did less well in univariate analyses, this effect vanished after adjustment for other socioeconomic status variables, such as income and education. Regional variations persisted, with lower rates of OB and OW/OB in British Columbia and higher rates in Atlantic Canada.
Conclusions:
These results confirm that progress is possible against this important public health challenge, underline the need to better understand sociodemographic risk factors and identify groups at higher risk for possible interventions.
Keywords: Obesity, Overweight, Socioeconomic status
Although lack of progress against high rates of obesity (OB) and overweight (OW) is a global concern (1), we recently analyzed a decade of growth in 14,014 Canadian children aged 3 to 19 years and reported a 15% decline in the prevalence of ‘OW or OB’ (OW/OB). OW or OB was 30.7% (29.7% to 31.6%) in 2004 and declined to 27.0% (25.3% to 28.7%, P<0.001) in 2013, with stabilization in OB rates at ~13% (2). The data were derived from three national surveys between 2004 and 2013. As detailed in the Methods section, OB for children aged 5 to 19 years refers to body mass index (BMI=weight/height2) above the 97th percentile (%) for age and sex. In toddlers (≤5 years), the corresponding cut-point is > 99.9%. Similarly, OW refers to BMI>85% and ≤97% (5 to 19 years) or > 97 and ≤99.9% (≤5 years). The combined designation of ‘overweight or obesity’ (OW/OB) pools these categories to identify children outside the healthy range, who experience a graded risk (3).
Although rates were lower for younger children, girls and those of European (White) race-ethnicity, temporal trends persisted after adjustment for age, sex and race. While declining, median Z-scores for BMI, weight and height were consistently positive, with higher values than the World Health Organization (WHO) reference population (2), further underlining the need for studies in different national jurisdictions.
While our work to date has focused primarily on the biological determinants of OW and OB, it is clear that socioeconomic status (SES) also influences prevailing rates and temporal trends through a complex interplay of financial resources, educational background, family supports, regional programs and cultural expectations (4,5). For this reason, we hypothesized that lower SES would be associated with higher rates of ‘OW or OB’. In this follow-up study, we therefore examine the ability of socioeconomic and regional variables to explain rates of OW and OB in the same data sets.
METHODS
As described elsewhere, Health Canada and Statistics Canada restored directly measured heights and weights in 2004 as part of the Canadian Community Health Survey (CCHS) cycle 2.2, a representative, cross-sectional, national survey designed to collect information about the nutritional status of Canadians aged 2 to 79 years (6). After 2007, the Canadian Health Measures Survey (CHMS) continued to measure height, weight and waist circumference on Canadian children aged 3 to 19 years. Both surveys systematically targeted over 96% of the Canadian population, excluding residents of Indian Reserves and some remote regions, full-time members of the regular Canadian Forces and institutions, with participation rates > 75% (7,8). To permit detailed comparisons over time, we analyzed a decade of anthropometric data from 14,014 children aged 3 to 19 years from CCHS cycle 2.2 (2004 to 2005) and CHMS cycles 2 (2009 to 2011) and 3 (2012 to 13). CHMS cycle 1 (2007 to 2008) was excluded, since it did not include children < 6 years. By restricting analysis to a comparable age range (3 to 19 years) across survey cycles, we could apply poststratification, inverse-probability survey weights with sample-specific standardization to account for nonresponse and under-coverage and generalize results to the population as a whole (9). For anthropometric measurements, trained staff measured heights to the nearest 0.5 cm and weights to the nearest 0.1 kg. Parents consented for children to be measured as part of the CCHS and CMHS surveys; children over 12 years (CCHS) or 14 years (CHMS) provided assent.
Approval was granted by the Research Ethics Board at the University of Manitoba. All statistical analyses were performed in R (10).
Obesity was defined according to the WHO criteria, with BMI > 97th percentile between the ages of 5 and 19 years (child) and > 99.9th percentile for 2 to 5 years (toddler). Similarly, overweight was defined as BMI > 85th and ≤ 97th percentile (5 to 19 years) or > 97th and ≤ 99.9th percentile (2 to 5 years). As a result, age groups were designated as toddler (≤5 years) or child (5 to 19 years) (11). The three survey eras included 8976 (CCHS 2.2), 2578 (CHMS 2) and 2460 (CHMS 3) children aged 3 to 19 years evenly split by gender, with 1622 toddlers and 2781 non-Whites.
We utilized four socioeconomic variables from all three surveys. Household income adequacy (‘income’) takes into consideration the number of individuals within a household who share the total income, providing a fairer comparison between families of different sizes over time. For each survey, Statistics Canada groups families into low (~9.8% of the Canadian population in 2004 to 2005), low-middle (21.1%), upper-middle (34.8%) and high-income adequacy (34.3%) categories (12). For example, the high-income category included families with incomes > $60,000 with 1 to 2 family members or larger families (>2) with incomes >$80,000. Similarly, household educational achievement was categorized as less than high-school (ltHS), high-school (HS) and any postsecondary (PS) education. Families were identified as couple-led (couple), single-parent (single) or other. Immigration status was defined as immigrant versus nonimmigrant. Provinces of origin were grouped as Ontario, Quebec, British Columbia, Prairies (Manitoba, Saskatchewan and Alberta) and Atlantic (Nova Scotia, Prince Edward Island, New Brunswick and Newfoundland) regions, representing between 12% (British Columbia) and 29% (Ontario) of the total sample. Race-ethnicity categories were pooled as White (European-American) versus non-White to ensure adequate numbers and consistency across survey cycles.
Logistic regression was used to assess the association of all predictors on rates of OB or OW/OB, with reference categories assigned to survey era = 2004 to 2005, age group = child, sex = male, race-ethnicity = White, income adequacy = high, education = postsecondary, family = couple-led and region = Ontario. A model using era, age, sex and race-ethnicity was considered the ‘unadjusted’ model for these additional analyses (2). All analyses were planned a priori and no correction for multiple comparisons was applied. P values are denoted by †<0.05, *<0.001.
RESULTS
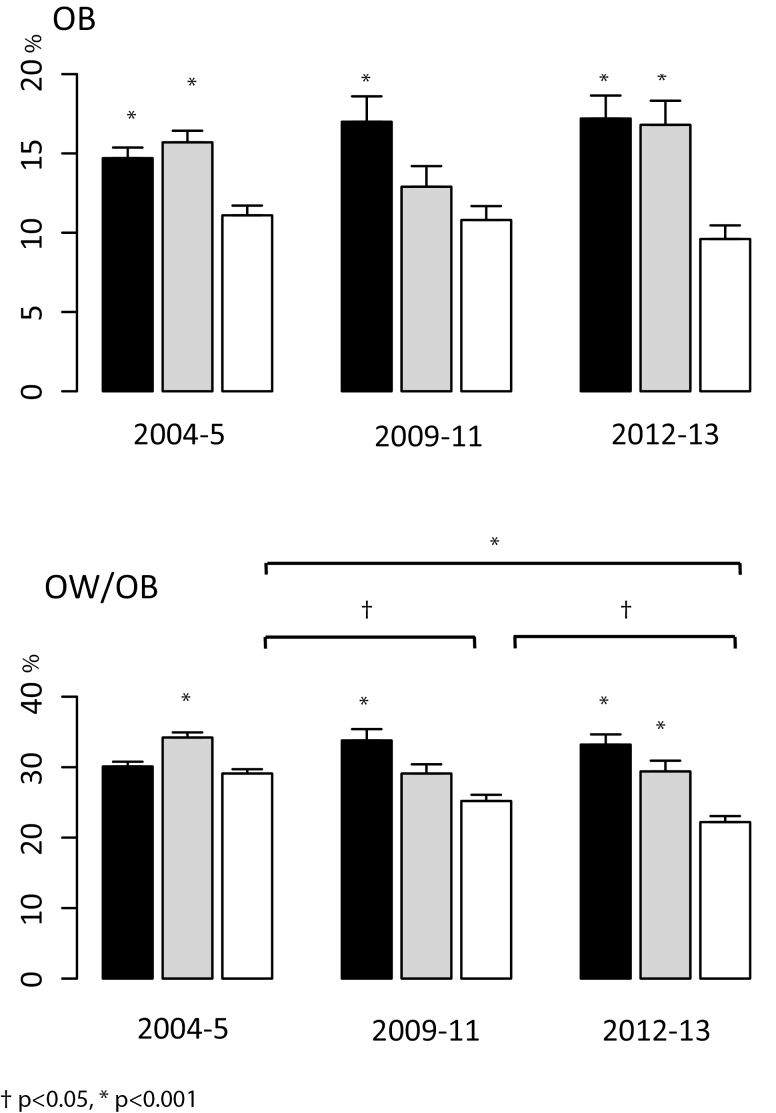
Figure 1 illustrates the association between income adequacy and the prevalence of OB (A) and OW/OB (B) by survey era, weighted to reflect the national population. Within each survey era, rates of OB or OW/OB were consistently lower with higher-income adequacy. While OB rates were stable across time, rates of OW/OB declined significantly within the highest income category from 2004 to 2005 (29.1% [95% confidence interval (CI): 27.3 to 30.8] to 2009 to 2011 (25.2% [95% CI: 22.8 to 27.8], P=0.02) and 2009 to 2011 to 2012 to 2013 (22.2% [95% CI: 19.8 to 24.6], P=0.03), without significant changes in the lowest category. Similar patterns were observed when income adequacy was replaced by survey-specific tertiles for total household income (not shown).
Figure 1.
Weighted prevalence (+SE) of OB (A) and OW/OB (B) by survey and income adequacy. To respect Statistics Canada privacy regulations for reporting prevalences, low- and low–middle-income categories were pooled for the lowest category (black bars); grey bars = upper middle income and white bars = high income. Asterisks above the vertical bars denote statistical significance compared to the reference category for each survey (high-income adequacy). The horizontal lines identify pairwise differences across survey eras in the highest income adequacy category. P values are marked as *P<0.001, †P<0.05.
Table 1 reports the results of the multivariable logistic regression in the form of odds ratios for OW/OB, beginning with the previously reported ‘unadjusted’ base model, which confirms a significant decline over time (2). Socioeconomic variables were then added individually to assess their impact on the biological determinants, which were largely unaffected. OW/OB rates were higher in those from lower incomes, lower education and single-parent families but were lower in immigrants even after accounting for temporal trends, age, sex and race. Regional differences were variable, with the highest levels in Atlantic Canada and the lowest in British Columbia and Quebec. The fully adjusted model includes both biological and socioeconomic determinants, which confirms the effects of time, age, sex, race-ethnicity, income, education, immigration and geographic region. Higher rates in single-parent families vanished with adjustment for other SES variables. Variance inflation factors (VIF<1.2) excluded multicollinearity as the explanation (when collinear predictor variables inflate the standard errors or variances of the parameter estimates, they may be associated with type II errors and loss of statistical significance).
Table 1.
Odds ratios (95% CI) for overweight/obese with and without adjustment for sociodemographic features
| Unadjusted | Income adequacy | Education | Family type | Immigrant status | Geographic region | Fully adjusted | |
|---|---|---|---|---|---|---|---|
| Age Group Toddler 11.6%, ref=88.4% | 0.27* (0.23, 0.32) | 0.27* (0.23, 0.31) | 0.28* (0.24, 0.33) | 0.28* (0.23, 0.32) | 0.27* (0.23, 0.31) | 0.27* (0.23, 0.32) | 0.27* (0.23, 0.32) |
| Survey 2009–2011 18.4%, ref=64.0% | 0.87‡ (0.79, 0.95) | 0.90† (0.82, 0.99) | 0.88‡ (0.80, 0.96) | 0.86‡ (0.79, 0.95) | 0.87‡ (0.79, 0.95) | 0.87‡ (0.79, 0.95) | 0.90† (0.81, 0.98) |
| Survey 2012–2013 17.6% | 0.82* (0.74, 0.89) | 0.84* (0.76, 0.92) | 0.81* (0.74, 0.89) | 0.82* (0.74, 0.89) | 0.82* (0.75, 0.90) | 0.82‡ (0.74, 0.90) | 0.81* (0.74, 0.90) |
| Sex Female 50.0%, ref=50.0% | 0.78* (0.73, 0.84) | 0.79* (0.73, 0.85) | 0.78* (0.72, 0.84) | 0.79* (0.73, 0.85) | 0.78* (0.72, 0.84) | 0.78* (0.73, 0.84) | 0.79* (0.73, 0.85) |
| Race Non-White 19.8%, ref=80.2% | 1.15* (1.06, 1.25) | 1.07 (0.98, 1.17) | 1.14‡ (1.05, 1.24) | 1.14‡ (1.05, 1.25) | 1.22* (1.11, 1.33) | 1.16* (1.06, 1.26) | 1.13† (1.02, 1.24) |
| Low income 9.2%, ref=80.2% | 1.50* (1.29, 1.73) | 1.39* (1.18, 1.64) | |||||
| Low-middle income 19.8% | 1.36* (1.23, 1.51) | 1.32* (1.18–1.48) | |||||
| Middle income 32.4% | 1.31* (1.20, 1.44) | 1.22* (1.10, 1.35) | |||||
| Education less than high school 5.6%, ref=76.4% | 1.26‡ (1.06, 1.50) | 1.04 (0.87, 1.25) | |||||
| Education high school 18.0% | 1.24* (1.12, 1.38) | 1.14† (1.02–1.28) | |||||
| Family Other 2.6%, ref=78.1% | 1.19 (0.91, 1.54) | 1.19 (0.89, 1.59) | |||||
| Family Single 19.4% | 1.22* (1.11, 1.34) | 1.05 (0.95, 1.17) | |||||
| Immigrant 6.2%, ref=93.8% | 0.79* (0.68, 0.89) | 0.82‡ (0.71, 0.95) | |||||
| Region Atlantic 17.0%, ref=28.6% | 1.21† (1.04, 1.40) | 1.13 (0.96, 1.32) | |||||
| Region Quebec 18.2% | 0.88‡ (0.79, 0.97) | 0.81* (0.73, 0.90) | |||||
| Region Prairies 23.6% | 0.95 (0.86, 1.06) | 0.91 (0.81, 1.01) | |||||
| Region British Columbia 12.6% | 0.82‡ (0.73, 0.93) | 0.78* (0.68, 0.88) |
Multivariable logistic regression as odds ratios (95% CIs) for overweight or obesity, beginning with the unadjusted model for survey era, age group, sex and race-ethnicity. Socioeconomic variables were then added individually to assess their impact.
Percentages in the first column refer to the proportion of respondents represented by the corresponding level of each categorical variable and ‘ref’ is the proportion represented by the reference level. The final column is the fully adjusted model, including both biological and socioeconomic predictors. Reference categories are survey = 2004–2005 (CCHS 2.2), age group = child (5–19 years), sex = male, race = White, income adequacy = high, education = postsecondary, family = couple-led and region = Ontario. Odds ratios that do not cross 1 are statistically significant, specifically marked as *P<0.001, ‡P≤0.01, †P<0.05
CI Confidence interval
OB prevalence is assessed in Table 2. Although no temporal trend was demonstrated, univariate results are otherwise similar to those for combined OW/OB in Table 1. In the fully adjusted model, the odds of obesity in lower-income classes were significantly increased by a factor of 1.38 to 1.73 compared with families in the high-income category.
Table 2.
Odds ratios (95% CI) for obesity with and without adjustment for sociodemographic features
| Unadjusted | Income adequacy | Education | Family type | Immigrant status | Geographic region | Fully adjusted | |
|---|---|---|---|---|---|---|---|
| Age group Toddler | 0.47* (0.38, 0.56) | 0.45* (0.37, 0.55) | 0.48* (0.39, 0.58) | 0.47* (0.39, 0.57) | 0.46* (0.37, 0.55) | 0.46* (0.38, 0.56) | 0.46* (0.37, 0.56) |
| Survey 2009–2011 | 0.91 (0.81, 1.03) | 0.97 (0.86, 1.10) | 0.93 (0.82, 1.05) | 0.91 (0.81, 1.03) | 0.92 (0.81, 1.03) | 0.91 (0.80, 1.02) | 0.96 (0.84, 1.09) |
| Survey 2012–2013 | 0.97 (0.86, 1.09) | 1.01 (0.89, 1.14) | 0.96 (0.85, 1.09) | 0.97 (0.86, 1.09) | 0.97 (0.86, 1.10) | 0.96 (0.85, 1.09) | 0.98 (0.86, 1.11) |
| Sex Female | 0.65* (0.59, 0.72) | 0.65* (0.58, 0.72) | 0.66* (0.60, 0.73) | 0.66* (0.59, 0.72) | 0.65* (0.58, 0.71) | 0.65* (0.59, 0.72) | 0.66* (0.59, 0.73) |
| Race Non-White | 1.17‡ (1.05, 1.30) | 1.07 (0.96, 1.20) | 1.19‡ (1.06, 1.32) | 1.16‡ (1.04, 1.29) | 1.28* (1.14, 1.44) | 1.25* (1.11, 1.39) | 1.26* (1.12, 1.43) |
| Low income | 1.92* (1.59, 2.30) | 1.73* (1.40, 2.12) | |||||
| Low middle income | 1.51* (1.32, 1.73) | 1.38* (1.18, 1.60) | |||||
| Middle income | 1.51* (1.33, 1.70) | 1.39* (1.22, 1.58) | |||||
| Education less than high school | 1.70* (1.39, 2.08) | 1.32† (1.05, 1.63) | |||||
| Education high school | 1.31* (1.15, 1.50) | 1.12 (0.97, 1.29) | |||||
| Family Other | 1.29 (0.91, 1.78) | 1.20 (0.82, 1.70) | |||||
| Family Single | 1.32* (1.17, 1.49) | 1.08 (0.94, 1.23) | |||||
| Immigrant | 0.64* (0.53, 0.78) | 0.67* (0.54, 0.81) | |||||
| Region Atlantic | 1.43* (1.18, 1.73) | 1.26† (1.03, 1.54) | |||||
| Region Quebec | 1.13 (1.00, 1.29) | 0.98 (0.86, 1.13) | |||||
| Region Prairies | 1.04 (0.90, 1.20) | 1.03 (0.89, 1.19) | |||||
| Region British Columbia | 0.78‡ (0.66, 0.93) | 0.71* (0.59, 0.85) |
Multivariable logistic regression as odds rations (95% CIs) for obesity. Otherwise, as in Table 1.
CI Confidence interval
DISCUSSION
Our study finds that rates of OB and OW/OB are substantially lower in Canadian children from higher-income families in all survey eras and in these families, there was also greater improvement with time, with OW/OB declining from 29.1% (95% CI: 27.3 to 30.8) (2004 to 2005) to 22.2% (95% CI: 19.8 to 24.6) (2012 to 2013, P<0.001). The multivariable analyses confirm our earlier report on the declining prevalence of OW/OB among Canadian children, which was largely unaffected by further adjustment for SES variables (2). Therefore, the decline over time is not explained by differences in income adequacy, education levels, immigration status or regional variations. However, children from families with lower incomes, lower levels of parental education, nonimmigrant status and from selected regions of Canada have increased odds of OW/OB or OB. As in the USA, even middle-income families appear to be at increased risk (13).
Previous cross-sectional studies have reported higher rates of OW/OB in children from families with lower income and education levels (5). Only one other manuscript has used multiyear administrative data to show a declining prevalence of OB in adolescents (12 to 17 years) with high SES: In a recent comparison of data from the 1988 to 2010 National Health and Nutrition Examination Surveys and the 2003 to 2011 National Survey of Children’s Health, Frederick et al. did not find significant differences in obesity prevalence by family income or education among children aged 2 to 5 years or 6 to 11 years. However, they identified a divergence in trends for children aged 12 to 17 years based on parental education levels, with rates increasing in families with at most a high-school education and declining in families with at least a 4-year postsecondary degree (14).
Although not adjusted for other socioeconomic factors, previous studies have also reported higher rates of OB or OW/OB in both children and adults in Atlantic Canada, with lower rates in British Columbia (5,15,16). Perhaps, surprisingly, the regional variations observed here persisted after regression adjustment for income, education, race and immigration, which speaks to additional sociodemographic or cultural factors. These may not have been captured consistently in these surveys and might include such factors as food and exercise habits, community attitudes or educational programs.
Although single-parent families have been associated with higher rates in other jurisdictions, not all such studies controlled for differences in family income and education levels (17). A previous report of data on Canadian adolescents in the CCHS (2000 to 2008) documented lower rates of OW/OB (18%) in immigrant children compared with nonimmigrants (22%). This contrasts with the rise of OB in many developing countries (18,19). Unfortunately, immigrant youth gain BMI with time spent in this country, as BMI z-scores increase by 0.02 for each year in Canada (19), which provides an opportunity to target this population with primary prevention measures.
This study benefits from a large and systematic sample from national surveys that include anthropometric measurements by trained professionals. In terms of limitations, Statistics Canada privacy regulations mean that we cannot report detailed cross-tabulations for all variables of interest (e.g., race, province). Despite a common sampling frame and target population, CCHS and CHMS were based on different designs. Notwithstanding the use of survey weights, nonresponder biases may still be present. Moreover, First Nations reserves and remote northern communities were not included. Additionally, data are cross-sectional and cannot be used to infer causality.
Moreover, using only national survey data, we are unable to explain mechanistically the observed decline in rates of OW/OB or the effects of socioeconomic determinants on prevalence. Although we might speculate that the introduction of BMI charts in 2000 (20) encouraged health care providers to more openly discuss OW/OB, and numerous regional/national weight management programs may have increased media scrutiny and public awareness. Families with higher education and income adequacy may benefit more readily from such programs, with more resources for follow-up and less food insecurity.
CONCLUSIONS
Childhood OW and OB represent an important public health challenge and a significant disease burden in terms of adult diabetes, heart disease and premature mortality. The results described here confirm that progress is possible in terms of reducing rates of overweight and stabilizing obesity rates. In addition, these findings highlight the importance of socioeconomic risk factors that may hinder progress and identify significant disparities in how that progress is shared across socioeconomic strata. Moreover, the observed associations with lower income, lower education and specific geographic regions identify potential candidates for targeted interventions, such as education and treatment programs.
Acknowledgements
This work was generously supported by Children’s Hospital Research Institute of Manitoba (CHRIM) and performed in the Statistics Canada Research Data Centre at the University of Manitoba.
References
- 1. Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr 2014;168:561–6. [DOI] [PubMed] [Google Scholar]
- 2. Rodd CJ, Sharma AK. Recent progress in the prevalence of overweight and obesity in Canadian children. CMAJ. 2016;188:E313–20. [DOI] [PMC free article] [PubMed]
- 3. Sharma AK, Metzger DL, Daymont C, Hadjiyannakis S, Rodd CJ. LMS tables for waist-circumference and waist-height ratio Z-scores in children aged 5-19 y in NHANES iii: Association with cardio-metabolic risks. Pediatr Res 2015;78:723–9. [DOI] [PubMed] [Google Scholar]
- 4. Datar A, Chung PJ. Changes in socioeconomic, racial/ethnic, and sex disparities in childhood obesity at school entry in the United States. JAMA Pediatr 2015;169:696–7. [DOI] [PubMed] [Google Scholar]
- 5. Shields M. Measured obesity: Overweight Canadian children and adolescents. Statistics Canada Catalogue. 2005;82-620-MWE(001): 1–34. [Google Scholar]
- 6. Statistics Canada. Canadian Community Health Survey Cycle 2.2, Nutrition Focus 2012 [cited October 29, 2015] <http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/cchs_focus-volet_escc-eng.php - p4>.
- 7. Health Canada. Canadian Community Health Survey (CCHS) Ottawa, Canada: Health Canada; 2012 [updated April 23, 2012; July 17, 2015] <http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/index-eng.php>.
- 8. Health Canada. Canadian Health Measures Survey (CHMS) Ottawa, Canada: Health Canada; 2015 [updated July 15, 2015; cited 2015 July 17, 2015] <http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5071>.
- 9. Statistics Canada. Appendix 4 normalizing weights. The Research Data Centres Information and Technical Bulletin. 2014;6:69–70. [Google Scholar]
- 10. R Core Team, R Foundation for Statistical Computing. R: A language and Environment for Statistical Computing <http://www.R-project.org/>. 2014. (accessed Jan 2015).
- 11. Corby L, Secker D. Growth monitoring of infants and children using the 2006 World Health Organization [WHO] Child Growth Standards and 2007 WHO Growth References. PEN: The Global Resource for Nutrition Practice [Internet]. 2012. https://www.dietitians.ca/Downloads/Public/Growth_Charts_backgrounder_eng.aspx. [Google Scholar]
- 12. Statistics Canada. CCHS Cycle 2.2 Data Dictionary for the Public Use Microdata File. Ottawa, ON: Statistics Canada, 2005:118. [Google Scholar]
- 13. Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in children and adolescents: United States, 2005-2008. NCHS Data Brief. 2010;51:1–8. [PubMed] [Google Scholar]
- 14. Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci USA 2014;111:1338–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Public Health Agency of Canada and the Canadian Institute for Health Information. Obesity in Canada: A joint report from the Public Health Agency of Canada and the Canadian Institute for Health Information. Ottawa: Public Health Agency of Canada, 2011:1–62. [Google Scholar]
- 16. Roberts KC, Shields M, de Groh M, Aziz A, Gilbert J-A. Overweight and obesity in children and adolescents: Results from the 2009 to 2011 Canadian Health Measures Survey. Statistics Canada Health Reports 2012;23:3–7. [PubMed] [Google Scholar]
- 17. Biehl A, Hovengen R, Grøholt EK, Hjelmesæth J, Strand BH, Meyer HE. Parental marital status and childhood overweight and obesity in norway: A nationally representative cross-sectional study. BMJ Open 2014;4:e004502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: A systematic review. Obes Rev 2012;13:1067–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wahi G, Boyle MH, Morrison KM, Georgiades K. Body mass index among immigrant and non-immigrant youth: Evidence from the canadian community health survey. Can J Public Health 2014;105:e239–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for disease control and prevention 2000 growth charts for the United States: Improvements to the 1977 national center for health statistics version. Pediatrics 2002;109:45–60. [DOI] [PubMed] [Google Scholar]