Abstract
Background:
Sickness presenteeism is defined as the act of attending one’s job despite ill-health. Recently, physicians and other health care workers have become the focus of sickness presenteeism research, because presenteeism in this population can put patients at risk of infection. There are currently no data on this topic among physicians in Canada. The aim of this study was to investigate sickness presenteeism in paediatric resident physicians in Canada.
Methods:
We conducted an anonymous, online, cross-sectional survey study in which all paediatric residents in Canada were eligible. Outcomes of interest included prevalences of sickness presenteeism, sickness during the study period and voluntary self-appointed personal protective equipment use when engaging in sickness presenteeism.
Results:
Response rate was 56.5% (N=323). During the previous 2 months, 61% (95% confidence interval [CI] 55.7 to 66.3) of respondents reported having experienced an illness and 59% (95% CI 53.7 to 64.5) of respondents had come to work sick. Of those who reported becoming ill during the study period, 97.0% (95% CI 94.6 to 99.4) reported coming to work while sick. There was no difference in prevalence when comparing across post-graduate year training levels. Extra personal protective equipment was used by 86% (95% CI 82.1 to 91.7) when engaging in sickness presenteeism.
Conclusion:
Sickness presenteeism is a common phenomenon among paediatric resident physicians. Our results should influence residents and supervising staff physicians to encourage appropriate self-care at home, rather than presenteeism.
Keywords: Presenteeism, Absenteeism, Internship and Residency, Sick Role, Physicians/statistics & numerical data, Canada.
Sickness presenteeism (SP) is the act of attending one’s job despite ill-health (1). A number of studies have investigated prevalence of SP and factors associated with coming to work sick in non-health care-related fields (1–4). SP has been associated with loss of productivity (5), future poor general health (6) and the development of depression (7). Recently, physicians and other health care workers have become the focus of SP research as working while sick can put their coworkers and patients at risk of infection (8–11). There are currently no data on SP among Canadian physicians. The aim of this study was to investigate SP in paediatric resident physicians in Canada.
METHODS
Study design
We investigated SP among paediatric residents in Canada through an anonymous, online, cross-sectional survey. We defined SP as: ‘Coming to work with symptoms of a potentially infectious illness including cough, rhinorrhea, sinus pressure or congestion, fever, sore throat, vomiting, and/or diarrhea’. To limit recall bias, we specified the recall period as the preceding 2 months that one had worked.
The primary outcome for this study was overall prevalence of self-reported SP. Secondary outcomes of interest were prevalence of SP among those who became ill during the study period, prevalence of sickness symptoms and use of personal protective equipment (PPE) among physicians engaging in SP with the intention of protecting patients from one’s infectious illness.
Sample size
Sample size determination was performed using statistical software from the University of Iowa, Department of Statistics and Actuarial Science (12). Based on our estimates, the appropriate sample size (N) was deemed to be N=175. As we expected a low response rate, we opted to include all paediatric residents in Canada as eligible for the study (N=644). To encourage an optimal response rate, incentives were offered. A random prize draw was conducted at the end of the study. Each respondent had a chance to win one of ten $10 coffee gift cards, or one of two Apple TV consoles.
Participants
Eligible participants were resident physicians enrolled in a paediatric residency training program in Canada in Post-Graduate Year 1 through 4 (PGY-1 through PGY-4). Paediatric subspecialty residents were not included in the study.
Questionnaire design
A 20-item questionnaire was developed in English and translated into French. The questions and content were designed to address how often residents engaged in SP and why SP was practiced (data regarding reasons for engaging in SP will be analyzed for a future study). Some content was based on a questionnaire used in a similar study assessing SP among 537 American resident physicians from a variety of different specialties (13). The draft questionnaire was tested with a pilot focus group at the investigators’ institution to ensure face validity. The questionnaire was modified and finalized based on feedback from this focus group. The questionnaires in both languages (available on request from the corresponding author) were then hosted online using a Canadian-based survey firm.
Questionnaire send-out and data acquisition
Unique online links to English and French questionnaires were sent to the Canadian Paediatric Program Directors Research Group (CPPD-R) in September 2013. The CPPD is the group of paediatric residency program directors from each of the 17 training programs in Canada. A functional link was required to gain access to the questionnaire. The CPPD-R then forwarded the links to the residents enrolled in their respective programs. A total of four link send-outs with a 2-week period in between each occurred over 2 months. Responses to the survey were anonymous. Demographic information was obtained including PGY level, sex and university/training program. To identify winners of the incentive prize draw, a separate form was located at the end of the questionnaire inviting respondents to submit their e-mail address for inclusion. These e-mail addresses were dissociated from the other questionnaire responses to ensure anonymity. At the completion of the study period, the data were downloaded into Microsoft Excel (14) and stored securely.
Statistical analysis
The data were imported into SPSS Version 22.0 (15) for further analysis. Outcomes of interest included prevalences of SP, sickness symptoms and use of voluntary PPE when attending work while sick (i.e., did the physician wear a mask during patient care which was not mandated by the patient’s isolation status on droplet or airborne precautions). These were reported using 95% confidence intervals (95% CI) for a proportion. Pearson chi-square testing was used to assess statistical significance across PGY levels. Analyses were also undertaken to compare between junior residents (PGY-1 and 2) and senior residents (PGY-3 and 4), as well as between PGY-1 and PGY-2 residents.
Ethics approval
Ethics approval was obtained from the University of Calgary Conjoint Health Research Ethics Board in October 2012. Support for the project was also received from the CPPD-R.
RESULTS
Response rate and demographics
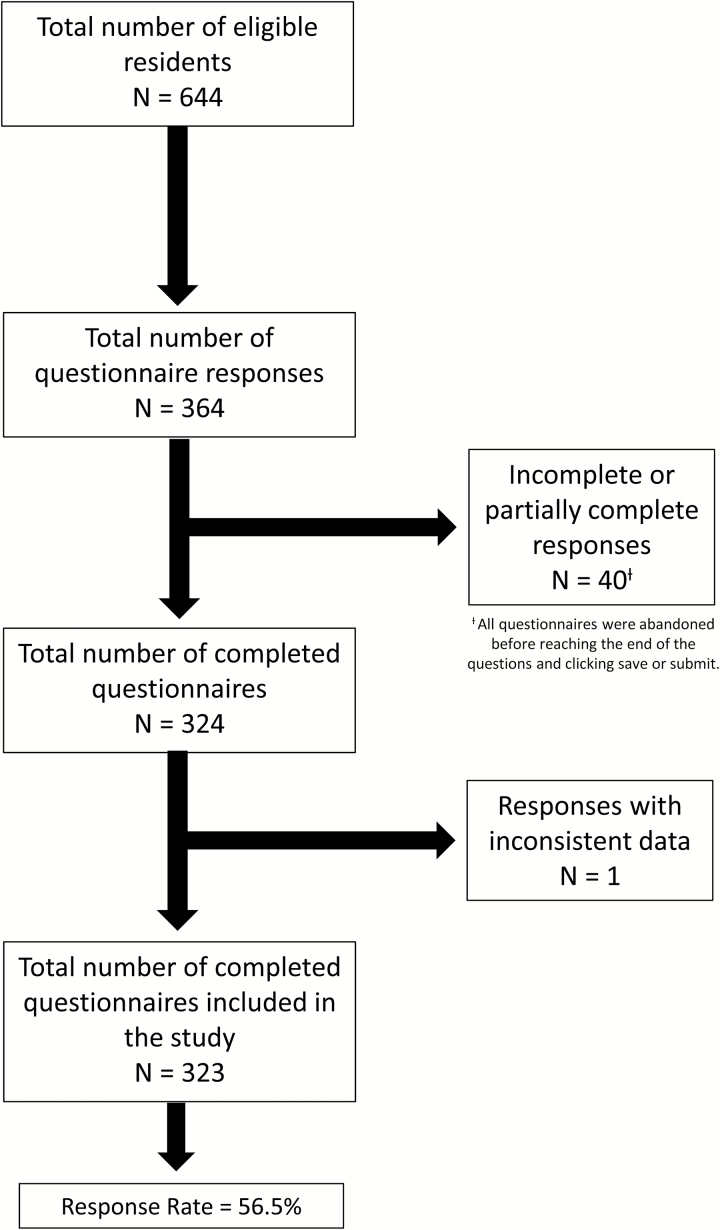
A total of 364 questionnaire responses were received (response rate 56.5%) (Figure 1). The completed questionnaires were reviewed (324). One questionnaire was excluded from the study because of inconsistencies in responses (the responder stated he/she had come to work sick within the study period but then later stated that he/she had not been sick within the study period). The remaining 323 completed questionnaires were included in the final analyses.
Figure 1.
Study response rate and response inclusion/exclusion.
Data related to subject demographics are displayed in Table 1.
Table 1.
Participant demographics
| Number of residents (%) | |
|---|---|
| Sex | |
| Female | 258 (79.9) |
| Male | 65 (20.1) |
| PGY level | |
| 1 | 106 (32.8) |
| 2 | 86 (26.6) |
| 3 | 89 (27.6) |
| 4 | 42 (13.0) |
| Institution | |
| A | 26 (8.0) |
| B | 31 (9.6) |
| C | 9 (2.8) |
| D | 19 (5.9) |
| E | 48 (14.9) |
| F | 19 (5.9) |
| G | 18 (5.6) |
| H | 28 (8.7) |
| I | 15 (4.6) |
| J | 0 (0.0) |
| K | 7 (2.2) |
| L | 30 (9.3) |
| M | 11 (3.4) |
| N | 6 (1.9) |
| O | 9 (2.8) |
| P | 26 (8.0) |
| Q | 21 (6.5) |
PGY Post-graduate year
Prevalence of sickness during the study period
Sixty-one percent (95% CI 55.7 to 66.3) of the respondents reported having experienced sickness symptoms in the preceding 2 months. The proportion of PGY-1 residents reporting sickness symptoms during the study period (69.8% [95% CI 61.1 to 78.5]) was greater than that of the remaining resident groups (P=0.02).
Prevalence of SP
Among the 323 respondents, 59.1% (95% CI 53.7 to 64.5) had come to work sick. The breakdown of PGY training level of the respondents who engaged in SP is displayed in Table 2.
Table 2.
Prevalence of sickness presenteeism among paediatric resident physicians in Canadian training programs
| Number of residents engaging in SP | Percentage (%) of total sample (N=323) responding yes to SP (95% confidence interval) | Percentage (%) within each group responding yes to SP (95% confidence interval) | |
|---|---|---|---|
| All Residents, N=323 | 191 | 59.1 (53.7–64.5) | 59.1 (53.7–64.5) |
| PGY-1, N=106 | 72 | 22.3 (17.8–26.8) | 67.9 (59.0–76.8) |
| PGY-2, N=86 | 43 | 13.3 (9.6–17.0) | 50.0 (39.4–60.6) |
| PGY-3, N=89 | 53 | 16.4 (12.4–20.4) | 59.6 (49.4–69.8) |
| PGY-4, N=42 | 23 | 7.1 (4.3–9.9) | 54.8 (39.7–69.9) |
PGY Post-graduate year; SP Sickness presenteeism
Prevalence of SP among those who became sick during the study period
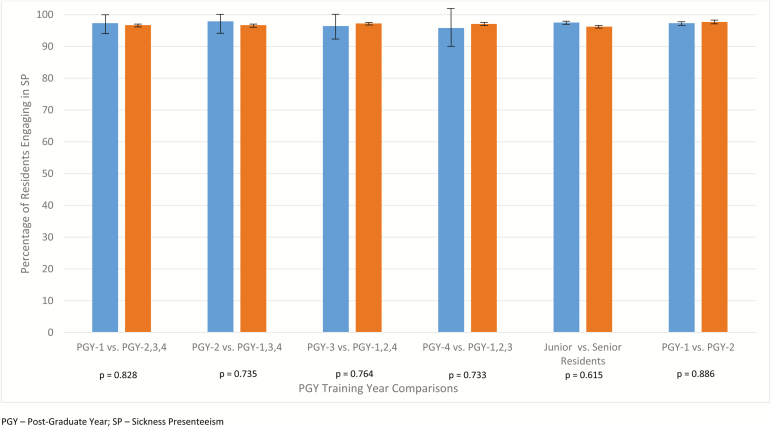
Of the 197 residents who reported becoming ill during the study period, 191 (97.0% [95% CI 94.6 to 99.4]) reported coming to work while sick. This proportion remained consistent across the four PGY levels, ranging from 95.8% to 97.9%. As shown in Figure 2, there was no statistically significant difference when comparing the PGY training levels. There was also no difference noted when comparing junior residents and senior residents and PGY-1s and PGY-2s.
Figure 2.
Comparison between groups of self-reported prevalence of sickness presenteeism among those who had developed sickness symptoms during the study period using Pearson chi-square testing.
Self-reported prevalence of extra PPE use or hygiene practices among those who came to work sick
Of the 191 residents who came to work while sick during the study period, 166 (86.9% [95% CI 82.1 to 91.7]) reported using some form of voluntary PPE. There was no statistically significant difference when comparing the residents by year of training.
DISCUSSION
Cross-sectional survey studies have shown SP prevalence among physicians to range from 51% to 86% (13,16–19). Among the respondents of our study, 59.1% reported coming to work sick during the previous 2 months. This is similar to the prevalence of SP (57.9%) as reported by Jena et al. in their 2010 study (13) although that study had a recall period of 1 year. Among the four specialties surveyed, Paediatrics had the highest incidence of SP with 62.5%. Contrary to that study, we did not find an increased incidence of SP in PGY-2s. In fact, we found that PGY-1 residents came to work sick more often than any of their resident counterparts, most likely due to the finding that PGY-1s were more likely to report having been ill during the study period. The reason for this is unclear. When excluding residents who did not get sick during the study period, there was no difference in SP across the PGY levels. We expected to find a trend of increased presenteeism as the amount of responsibility increased from PGY-1 to PGY-4, but this was not reflected in the data.
The vast majority of residents who came to work while sick reported using some kind of voluntary PPE to reduce the risk of infection transmission. While the purpose of PPE is to protect oneself (the health care provider) from infection (20,21), there is some evidence for specific procedures (specifically lumbar punctures, epidural procedures, and insertion of central vascular catheters) that use of PPE reduces the risk of hospital-acquired infection in patients during the doctor–patient interaction (22,23). There is also evidence supporting the role of physician PPE use in preventing infection transmission between patients (24,25). While the proportion of residents claiming to voluntarily use extra PPE seems encouraging at 86.9%, it is not clear how stringently these precautions were applied or if extra PPE use by residents will protect patients.
A recent study examined self-reported frequency of working while sick among attending physicians and advance practice clinicians (26). More than 95% of the respondents believed that working while sick put patients at risk. Despite this belief, 446 respondents (83.1%) reported working sick at least one time in the past year. Reasons commonly cited included not wanting to let colleagues and/or patients down, staffing concerns, fear of ostracism by colleagues and concern about continuity of care. Other concerns among staff related to perceived difficulty finding coverage, a strong cultural norm to come to work unless remarkably ill and ambiguity around what constitutes ‘too sick to work’ (26). By examining the ‘why’ behind SP, hospital and training program administrators may be able to promote a culture change supporting the idea that a sick health care worker is a risk to his or her patients and colleagues and to support those who decide to stay home rather than endanger the patients for whom they care. A physician may have what he or she considers to be a minor upper respiratory tract infection; however, this infection could be catastrophic for an immunocompromised patient. While one may not want to create more work for their colleagues by taking a ‘sick day’, to ‘first, do no harm’, one must consider that staying home while sick may be the ethically more appropriate decision. Information sessions for attending physicians and hospital administrators may enhance appreciation of SP as a patient safety issue. This would not, however, address the logistical issues that would go with appropriate sickness absenteeism. Possible solutions might include the institution of back-up work schedules and/or the hiring of supplemental attending staff. The practical aspects of such changes would be challenging to enact in the current model for staffing.
Our study has a number of limitations. In selecting only paediatric residents, external validity may be limited in that the results may not reflect the presenteeism habits of paediatric subspecialty residents or non-paediatric residents. That being said, our results were similar to those reported by Jena et al. (13), which included a variety of medical and surgical specialties.
The period of recall was set at 2 months prior to the start of the study, which, while limiting recall bias, might underestimate the prevalence of SP among the paediatric resident population, given that the 57.9% reported in Jena et al.’s study used a recall period of 1 year: It is plausible that the prevalence of SP in our study may have been much higher if we had also used a recall period of 1 year. Additionally, as the recall period was not controlled for all respondents (i.e., September through October), the preceding 2 months of work may have varied among the respondents, with some working during a period of the year that might have a lower incidence of respiratory infections (summer versus winter months). As such, time of response may have affected the results.
While we did specify what symptoms were considered to be suggestive of an infectious illness in the questionnaire, we did not ask the residents to rate the severity of their illness. It is possible that some of the residents may have come to work because they felt that they were not sick enough to warrant staying home. We also did not clarify that cough and rhinorrhea due to seasonal allergies should not be considered ‘sickness symptoms’. It is possible that this may have increased the reported prevalence of SP in our study.
It is difficult to interpret whether ‘social desirability’ of responses might have played a role in the responses chosen by some residents. Participation in our study was anonymous, though there does exist the possibility that residents could have responded in a manner as to choose the most ‘altruistic’ response. This would likely vary from participant to participant in that some residents may feel that to come to work while sick is more altruistic (preventing more work for one’s colleagues), while others may feel the more altruistic response is to stay at home (preventing infection transmission to patients and colleagues). Our results hinge on the assumption that the residents responded truthfully to the questionnaire.
Our study has a number of strengths. This is the first study with Canadian data on resident SP. The study was carried out in both English and French with a validated bilingual questionnaire piloted prior to send-out. The response rate of the study was excellent at 56.5%, given that survey studies targeting residents tend to have lower response rates. A 2008 study examining strategies to increase survey response rate among residents and practicing physicians in Canada had a resident response rate of 27.9% (27).
Another strength of this study is that it identified the self-reported prevalence of SP among those who became sick during the study period. Previous studies have cited overall SP rates without delineating healthy residents not engaging in SP and sick residents not engaging in SP. This suggests that SP is a much more systemic and cultural problem in residency than previously suspected. When lending consideration only to those residents who had symptoms suggestive of an infectious illness, 97.0% (95% CI 94.6 to 99.4) chose to come to work while sick, with only six residents choosing to stay home.
From an alternative perspective, one is also less productive when ill. A 2009 review examined SP and on-the-job productivity losses. The studies included in this review varied significantly in the assessment of presenteeism and the assigned dollar value of those productivity losses (28). Some estimates have placed the cost of presenteeism to US businesses at $150 billion (29) to $260 billion (30), although a recent review of the literature cautioned against the conversion of presenteeism results into monetary figures as the populations and health conditions of workers are variable (28).
CONCLUSION
The primary outcome of this study was the overall self-reported prevalence of SP among paediatric residents in Canadian training programs. This study represents the first available Canadian data on resident SP. The fact that 97.0% of participating residents who were unwell (59.1% overall) continued to work in a health care environment is a key finding and raises concerns about behaviours that may affect patient safety and risks of health care-associated infections. Further efforts are required to understand what factors can help eliminate presenteeism and to what extent this contributes to adverse outcomes for patients.
Acknowledgements
We thank Drs. Kathy Tobler and Deborah Fruitman (Program Directors for the Paediatrics Residency program at the University of Calgary at the time of study onset and completion) as well as the Canadian Paediatric Program Directors Research Group for their support and assistance in sending out the questionnaire links. We also thank Dr. Brent Hagel in the design and statistical analysis phases of the project, as well as Dr. Ijab Khanafer for her assistance in translating the questionnaire into French and Ms. Julie Squires for her administrative support. This work was performed at the University of Calgary, Alberta Children’s Hospital. The ethics board that approved the study is the Conjoint Health Research Ethics Board at the University of Calgary. Funding for this study was provided by the Alberta Children's Hospital, Department of Paediatrics, Infection Prevention Research and Evaluation Fund.
References
- 1. Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. J Epidemiol Community Health 2000;54:502–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hansen C, Andersen J. Going ill to work—what personal circumstances, attitudes and work-related factors are associated with sickness presenteeism? Soc Sci Med 2008;67:956–64. [DOI] [PubMed] [Google Scholar]
- 3. Johansen V, Aronsson G, Marklund S. Positive and negative reasons for sickness presenteeism in Norway and Sweden: A cross-sectional survey. BMJ Open 2014;4:e004123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Perio MA, Wiegand DM, Brueck SE. Influenza-like illness and presenteeism among school employees. Am J Infect Control 2014;42:450–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bramley TJ, Lerner D, Sames M. Productivity losses related to the common cold. J Occup Environ Med 2002;44:822–9. [DOI] [PubMed] [Google Scholar]
- 6. Bergstrom G, Bodin L, Hagberg J, Lindh T, Aronsson G, Josephson M. Does sickness presenteeism have an impact on future general health? Int Arch Occup Environ Health 2009;82:1179–90. [DOI] [PubMed] [Google Scholar]
- 7. Conway PM, Hogh A, Rugulies R, Hansen AM. Is sickness presenteeism a risk factor for depression? A Danish 2-year follow-up study. J Occup Environ Med 2014;56:595–603. [DOI] [PubMed] [Google Scholar]
- 8. Widera E, Chang A, Chen H. Presenteeism: A public health hazard. J Gen Intern Med 2010;25:1244–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Landry M, Miller C. Presenteeism: Are we hurting the patients we are trying to help? J Gen Intern Med 2010;25:1142–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Albrich WC, Harbarth S. Health-care workers: Source, vector, or victim of MRSA? Lancet Infect Dis 2008;8:289–301. [DOI] [PubMed] [Google Scholar]
- 11. Mattner F, Mattner L, Borck HU, Gastmeier P. Evaluation of the impact of the source (patient versus staff) on nosocomial norovirus outbreak severity. Infect Control Hosp Epidemiol 2005;26:268–72. [DOI] [PubMed] [Google Scholar]
- 12. Lenth RV. Java Applets for Power and Sample Size [computer software]. 2006–2009 <www.stat.uiowa.edu/~rlenth/Power> (Accessed December 1, 2011).
- 13. Jena AB, Baldwin DC, Daugherty SR, Meltzer DO, Arora V. Presenteeism among resident physicians. JAMA 2010;304:1166–8. [DOI] [PubMed] [Google Scholar]
- 14. Microsoft Corporation. 2010. Microsoft Excel 2010, Version 14.0.6024.1000. [Google Scholar]
- 15. IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp, 2013. [Google Scholar]
- 16. McKevitt C, Morgan M, Dundas R, Holland WW. Sickness absence and ‘working through’ illness: A comparison of two professional groups. J Public Health Med 1997;19:295–300. [DOI] [PubMed] [Google Scholar]
- 17. Bracewell LM, Campbell DI, Faure PR, et al. Sickness presenteeism in a New Zealand hospital. NZ Med J 2010;123:31–42. [PubMed] [Google Scholar]
- 18. Tan PC, Robinson G, Jayathissa S, Weatherall M. Coming to work sick: A survey of hospital doctors in New Zealand. NZ Med J 2014;127:23–35. [PubMed] [Google Scholar]
- 19. LaVela S, Goldstein B, Smith B, Weaver FM. Working with symptoms of a respiratory infection: Staff who care for high-risk individuals. Am J Infect Control 2006;35:448–54. [DOI] [PubMed] [Google Scholar]
- 20. Jefferson T, Del Mar CB, Dooley L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev 2011;7:CD006207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moore D, Gamage B, Bryce E, Copes R, Yassi A. Protecting health care workers from SARS and other respiratory pathogens: Organizational and individual factors that affect adherence to infection control guidelines. Am J Infect Control 2005;33:88–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725–32. [DOI] [PubMed] [Google Scholar]
- 23. Shewmaker PL, Gertz RE, Jr, Kim CY, et al. Streptococcus salivarius meningitis case strain traced to oral flora of anesthesiologist. J Clin Microbiol 2010;48:2589–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. LeClair JM, Freeman J, Sullivan BF, Crowley CM, Goldmann DA. Prevention of nosocomial respiratory syncytial virus infections through compliance with glove and gown isolation precautions. N Engl J Med 1987;317:329–34. [DOI] [PubMed] [Google Scholar]
- 25. Madge P, Paton JY, McColl JH, Mackie PL. Prospective controlled study of four infection-control procedures to prevent nosocomial infection with respiratory syncytial virus. Lancet 1992;340:1079–83. [DOI] [PubMed] [Google Scholar]
- 26. Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin S, Sammons J. Reasons why physicians and advanced practice clinicians work while sick: A mixed-methods analysis. JAMA Pediatr 2015;169:815–21. [DOI] [PubMed] [Google Scholar]
- 27. Grava-Gubins I, Scott S. Effects of various methodologic strategies: Survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician 2008;54:1424–30. [PMC free article] [PubMed] [Google Scholar]
- 28. Schultz A, Chen C-Y, Edington D. The cost and impact of health conditions on presenteeism to employers: A review of the literature. Pharmacoeconomics 2009;27:365–78. [DOI] [PubMed] [Google Scholar]
- 29. Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: Results from the American Productivity Audit. J Occup Environ Med 2003;45:1234–46. [DOI] [PubMed] [Google Scholar]
- 30. Davis K, Collins SR, Doty MM, Ho A, Holmgren A. Health and productivity among U.S. Workers. Issue Brief (Commonw Fund) 2005;856:1–10. [PubMed] [Google Scholar]