Abstract
Background
General emergency department crowding negatively impacts patient care, and increases patient morbidity.
Objectives
This study seeks to determine if markers of paediatric emergency department (PED) flow are independently associated with negative outcomes and increased health care utilization.
Methods
We conducted a retrospective cohort study of PED visits from 2008 to 2012. Data were pulled from an electronic administrative database. Using multivariate logistic regression models, we measured the association between odds of adverse outcomes (hospital/paediatric intensive care unit [PICU] admission, unscheduled return visits and mortality) with markers of PED flow (shift mean length of stay [LOS] and daily rate of patients leaving without being seen [LWBS]).
Results
We found an association between the daily LWBS proportion and the odds of being admitted to the hospital (odds ratio [OR]: 2.1; 95% confidence interval [CI]: 1.2, 3.7), as well as admission to the PICU (OR: 8.9; 95% CI: 1.1, 71.3). We found a statistically significant increase in the odds of admission if seen during shifts in the third or fourth quartile mean shift LOS. We observed lower odds of returning to the PED with increased daily LWBS proportions (OR: 0.4; 95% CI: 0.2, 0.7), but found no association between the odds of returning to the PED and mean shift LOS.
Conclusion
While we found an association between our pre-defined measures of adverse outcomes and markers of PED flow (or crowding), further studies are needed to determine whether PED overcrowding is the cause or effect of increased hospital and PICU admissions.
Keywords: Crowding, Emergency, Paediatric
Emergency department (ED) crowding has become an increasing problem. General ED studies show crowding reduces quality and access to care and increases patient morbidity (1–4). Guttman et al. (5) completed the largest study to date and found that ED patients who had been treated and released during periods of increased crowding had an increased risk of being admitted or dying within the next 7 days.
In the paediatric ED (PED), the impact of crowding is less clear. Studies in the PED have shown increases in the time to administration of antibiotics in sepsis, and trends to delayed treatment in asthma and fracture care as a result of crowding (6–9). However, other paediatric specific studies have suggested that crowding significant enough to divert ambulances did not influence mortality and that crowding conditions did not increase 48-h return visits (10,11). Only mixed studies of adult and paediatric centres have demonstrated a trend toward increased mortality, but these studies were strongly influenced by predominantly adult populations (1,5,12). Cha et al. (12) did look at the paediatric subgroup seen within a mixed adult-paediatric ED and found that crowding in this environment was associated with increased hazard of hospital mortality for those paediatric patients who required admission.
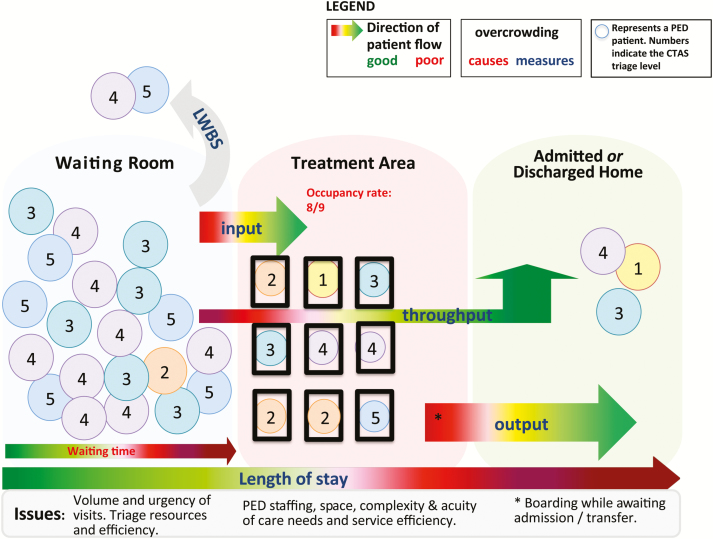
Markers of adult ED crowding have included the number of admitted patients boarding in the ED, the number of intubated patients in the ED, and mean ED length of stay (LOS) (13). Some of these markers are not relevant in Canadian PEDs as boarded patients—although an increasing phenomenon—are uncommon in PEDs, and intubated patients are rare in the paediatric population. Consequently, the paediatric literature has focused on variables such as ED LOS, PED occupancy, and proportion of patients who left without being seen (LWBS), as measures of PED crowding (5,14–16). A model of PED flow and conceptual determinants of overcrowding: input factors (volume of visits), throughput factors (the process of care from door to door and their associated resources) and output factors (ED disposition) is depicted in Figure 1, which highlights the factors which contribute to crowding.
Figure 1.
A conceptual model of paediatric emergency department flow, with factors involved in congestion
In this study, we sought to determine if markers of PED crowding are independently associated with adverse patient outcomes defined by admission to the hospital, admission to the paediatric intensive care unit (PICU), mortality, or return visit within 7 days of the index visit.
METHODS
We conducted a retrospective cohort study using an administrative database of British Columbia Children’s Hospital (BCCH) PED visit from January 2008 to December 2012, obtained from the Provincial Health Service Authority Performance Measurement and Reporting Office. Individual patient charts were not reviewed. BCCH is a level one trauma centre and tertiary care academic hospital located in Vancouver, and accepts referrals from across the province, with an annual PED census of approximately 40,000 patients a year during the study period. All patient visits to the BCCH PED from January 2008 and December 2012 for 21 years of age and younger were included for analysis. The age cut off of 21 years was used to include the group of paediatric patients who have not yet transitioned to adult care, and are still followed by paediatric subspecialties. The majority of patients were under 18 years of age, and those older than 21 were excluded as they are typically transferred to local adult centres per hospital policy. Ethics approval was obtained from the University of British Columbia.
Our study objective was to measure the association between markers of PED crowding and adverse patient outcomes. Our measures of PED crowding included the mean shift LOS and daily proportion of patients who left without being seen (LWBS). LOS stay was defined as the total time spent in the PED, from arrival to disposition (transferred to a ward or discharged home). Both of these measures have been used in other studies of ED crowding as markers for ED flow or proxies for ED overcrowding (5,15–23). In our analyses, mean shift LOS was calculated from the average LOS for all other patients arriving during the same shift, with the same acuity level as measured by the paediatric Canadian Triage and Acuity Scale (CTAS). The index visit’s own LOS was excluded from the mean shift LOS thereby evaluating the effect of the PED’s overall state of crowding, without allowing for the index visit’s own LOS to contribute to the shift mean LOS. Shifts were defined as (1) 08:00–15:59, (2) 16:00–23:59 and (3) 00:00–07:59. The daily proportion LWBS was analyzed as a continuous variable as a marker of PED overcrowding, rather than the patient-level dichotomous LWBS variable which has been used as an outcome of ED crowding in other studies (23).
Our primary predefined adverse patient outcome was admission to hospital, and secondary outcomes were admission to PICU, unscheduled return visits to the PED within 7 days, and death. While admission to hospital or PICU are often necessary for the management of severe illness, we isolated the incremental number of admissions to hospital or PICU after controlling for a measure of severity of ED presentation as described in analyses below. We used 7-day return to ED (RTED) visit based on unpublished data from our institution, which demonstrated that use of a shorter time period significantly underestimates the number of children returning for the same illness. A patient’s death was included if the patient died anytime in the visit or admission following initial ED registration.
We used descriptive statistics to summarize PED visit characteristics included in the analyses. Multivariable logistic regression models were used to determine the odds of an adverse outcome in relation to markers of ED crowding. Adverse outcome measures were dichotomous: (1) admission to hospital (yes or no), (2) admission to the PICU (yes or no), (3) unscheduled return visits within the next 7 days (yes or no) and (4) mortality (yes or no). The exposure variables of interest include (1) mean shift LOS which was categorical using quartiles of mean shift LOS; and (2) daily proportion LWBS which was continuous reflecting the proportion of LWBS that day. Covariates controlled for in the regression model included visit acuity (as measured by CTAS, as this is associated with admission risk), patient age, gender, the shift during which the visit was made, and calendar year (24).
RESULTS
Between January 2008 and December 2012, there were 208,585 patient visits to the PED with a mean annual visit volume of 41,717; 149 visits were excluded for age >21. While presenting CTAS score proportions, admission and mortality rates remained constant through the study period, there was a small increase in the rate of admission to the PICU (0.4–0.7%) and a small decrease in return visits to the PED (11.8–9.6%) across the study period. Table 1 summarizes the demographics of the study population. Increasing mean shift LOS was associated with increased rates of both hospital and PICU admission, but decreased rates of return ED visits (Table 2). As expected, the odds of hospitalization and PICU admissions both increased with increasing triage acuity. With regard to hospitalization, compared to CTAS 5, odds ratio (OR) for CTAS 3, CTAS 2 and CTAS 1 were respectively: 8.2, 28.6 and 75.3 (all with P < 0.05). With regard to PICU admission, the OR for CTAS 1 compared to CTAS 2 was 22.9 (P < 0.05). No PICU admissions occurred among CTAS 3–5. The odds of hospitalization were also highest with overnight shift presentations compare to day or evening shifts (ORs ranging from 1.1 to 1.3, P < 0.05). A similar association was observed between overnight shift arrivals and RTED (ORs ranging from 1.1 to 1.2, P < 0.05). Adjusted ORs for other covariates were not statistically significant for any of our outcomes.
Table 1.
Demographics
| Demographics | Year | ||||
|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | |
| Total number seen | 41,128 | 42,812 | 40,111 | 44,069 | 40,465 |
| CTAS 1, N (%) | 124 (0.3) | 191 (0.4) | 247 (0.6) | 216 (0.5) | 197 (0.5) |
| CTAS 2, N (%) | 3286 (8.0) | 3714 (8.7) | 4619 (11.5) | 5021 (11.4) | 5065 (12.5) |
| CTAS 3, N (%) | 13,765 (33.5) | 13,701 (32.0) | 13,496 (33.6) | 15,048 (34.1) | 14,116 (34.8) |
| CTAS 4, N (%) | 21,661 (52.7) | 21,909 (51.2) | 19,031 (47.4) | 21,373 (48.5) | 19,626 (48.5) |
| CTAS 5, N (%) | 2070 (5.0) | 2640 (6.2) | 2718 (6.8) | 1865 (4.2) | 1343 (3.3) |
| Missing CTAS, N (%) | 222 (0.5) | 657 (1.5) | 0 (0) | 546 (1.2) | 118 (0.3) |
| Median age (interquartile range) | 3.9 (1.4, 9.0) | 4.3 (1.6, 9.5) | 4.1 (1.5, 9.4) | 4.2 (3.0, 9.0) | 4.4 (1.6, 9.5) |
| Male % (95% CI) | 55.9 (55.5, 56.4) | 56.6 (56.1, 57.0) | 56.3 (55.9,56.8) | 56.1 (55.6, 56.5) | 56.9 (56.4, 57.4) |
| Admission % (95% CI) | 8.2 (7.9, 8.4) | 7.8 (7.5, 8.1) | 8.9 (8.64, 9.20) | 8.8 (8.5, 9.0) | 9.2 (9.0, 9.5) |
| PICU admission % (95% CI) | 0.4 (0.32, 0.45) | 0.4 (0.34, 0.47) | 0.6 (0.50, 0.65) | 0.6 (0.49, 0.63) | 0.7 (0.59, 0.75) |
| Mortality/1000 (95% CI) | 0.1 (0.1, 0.3) | 0.3 (0.1, 0.5) | 0.3 (0.2, 0.6) | 0.3 (0.1, 0.5) | 0.3 (0.1, 0.5) |
| RTED % (95% CI) | 11.8 (11.5, 12.2) | 10.4 (10.1, 10.7) | 10.2 (9.9, 10.4) | 10.3 (10.0, 10.6) | 9.6 (9.3, 9.9) |
| LWBS % (95% CI) | 2.3 (2.1, 2.4) | 3.9 (3.7, 4.1) | 2.9 (2.7, 3.0) | 5.1 (4.9, 5.3) | 4.8 (4.6, 5.0) |
| Median LOS (min) (interquartile range) | 157 (103, 243) | 174 (114, 264) | 168 (110, 260) | 191 (125–285) | 234 (123–296) |
CI confidence interval; CTAS Canadian Triage and Acuity Scale; LOS length of stay; LWBS leaving without being seen; PICU paediatric intensive care unit; RTED return to emergency department
Table 2.
Distribution of outcomes per shift LOS quartiles
| Shift LOS | 1st Quartile (<2.6 h) | 2nd Quartile (2.6–3.4 h) | 3rd Quartile (3.5–4.4 h) | 4th Quartile (>4.5 h) |
|---|---|---|---|---|
| % Admission (95% CI) | 2.8 (2.6, 2.9) | 4.8 (4.6, 5.0) | 9.0 (8.8, 9.3) | 16.9 (16.6, 17.2) |
| % PICU admission (95% CI) | 0.1 (0.1, 0.2) | 0.2 (0.2, 0.2) | 0.3 (0.3, 0.4) | 1.3 (1.2, 1.4) |
| % Mortality/1000 (95% CI) | 0.0 (0, 0.1) | 0.1 (0, 0.2) | 0.1 (0, 0.3) | 0.8 (0.6, 0.1) |
| % RTED (95% CI) | 11.0 (10.7, 11.2) | 10.7 (10.4, 11.0) | 10.4 (10.1, 10.7) | 9.8 (9.6, 10.1) |
CI confidence interval; LOS length of stay; PICU paediatric intensive care unit; RTED return to emergency department
The multivariable regression showed an association between the daily proportion LWBS and the odds of admission to hospital (OR: 2.1; 95% confidence interval [95% CI]: 1.2, 3.7) or PICU (OR: 8.9; 95% CI: 1.1, 71.3). The odds of returning to the PED within 7 days was significantly decreased if the initial visit was on a day with higher LBWS rate (OR: 0.4; 95% CI: 0.2, 0.7).
Overall, there were few associations between mean shift LOS and adverse outcomes (Table 2). There was a statistically significant increased odds of admission to the hospital if visiting the PED during shifts in the third or fourth quartile for longest mean shift LOS compared to the lowest quartile, but no significant association between mean shift LOS and the odds of admission to the PICU or returning to the ED (Table 3).
Table 3.
Odds ratios (ORs)
| Markers of crowding | Admission to hospital, OR (95% CI) | Admission the PICU, OR (95% CI) | RTED within 7 days (95% CI) |
|---|---|---|---|
| Daily proportion LWBS | 2.1 (1.2, 3.7) | 8.9 (1.1, 71.3) | 0.4 (0.2, 0.7) |
| Mean shift LOS (referent: 1st quartile: <2.6 h) | |||
| 2nd Quartile: 2.6–3.4 h | 1.1 (1.0, 1.1) | 1.0 (0.7, 1.3) | 1.0 (1.0, 1.0) |
| 3rd Quartile: 3.5–4.4 h | 1.1 (1.1, 1.3) | 0.8 (0.6, 1.1) | 1.0 (1.0, 1.1) |
| 4th Quartile: >4.5 h | 1.2 (1.1, 1.3) | 0.9 (0.7, 1.2) | 1.0 (0.9, 1.0) |
CI confidence interval; LOS length of stay; LWBS leaving without being seen; PICU paediatric intensive care unit; RTED return to emergency department
Throughout our study period, there were approximately 10 mortalities per year, precluding statistical testing of the association between mortality and measures of crowding.
DISCUSSION
Our study of PED crowding and adverse outcomes found a statistically significant association between both of our measures of PED crowding. While the OR of 2.1 for admission as a function of daily proportion LWBS was both clinically and statistically significant, the association with mean shift LOS was less definitive. With an overall admission rate of about 8%, the calculated OR of 1.2 associated with the longest shift mean LOS quartile represents less than a 2% increase to the baseline admission rate.
It is possible that poor ED flow leads to delays in ED treatment of time-sensitive conditions such as asthma or serious infection and such delays may lead to worsening patient condition necessitating hospital admission. Alternatively, ED crowding may alter the threshold for hospital admission due to reluctance to keep patients in the crowded department to assess response to ongoing interventions.
Current literature in this area is not only limited but also conflicting. Several small paediatric studies show that crowding increases time to interventions potentially resulting in sicker patients, although they have not shown an increase in admissions due to these practices (6–8). Michelson et al. (11) reported a trend in the opposite direction, proposing that ED occupancy rates may reflect hospital occupancy and that during times of overcrowding, ED practitioners may try to avoid hospital admission due to a lack of inpatient bed availability.
The only measure of crowding associated with PICU admission was the daily proportion of LWBS. For every percent increase in this proportion on a given day, there was an almost nine-fold increase in odds of being admitted to the PICU after adjusting for age, sex and CTAS level. There are two opposing possible explanations for this observation: it is possible that ED crowding as measured by proportion of LWBS negatively affects patient outcomes as suggested by Guttman’s primarily adult study, leading to patient deterioration and admission to PICU; alternatively, shifts with sicker patients (requiring PICU admission) may devote significant resources to those patients leading to ED overcrowding and patient decision to leave without being seen, especially those with lower acuity presentation. The fact that PICU admission was only associated with proportion of LWBS and not mean LOS raises questions about the directionality of the association and highlights the need for more refined measures of ED crowding and flow.
Contrary to our hypothesis, we found the odds of returning to the ED were inversely associated with the daily proportion of LWBS. Previous studies have shown conflicting relationships between overcrowding and ED return visits: some paediatric studies have found an increase in ED returns if the index visit was overcrowded, while other adult studies found trends similar to ours, with decreased returns following an experience with overcrowding (11,25). As we only measured return visits to our own PED, we may underestimate the true number of ED returns, had alternate hospitals been captured. It is likely, however, that a family experiencing a crowded PED may be discouraged from returning to the same site for their current concerns.
LIMITATIONS
By its nature, the retrospective design has inherent limitations; it is only generalizable to other centres with similar patient volumes, acuity distribution and hospital admission policies and practices. Of note, there were no changes in our department number of beds, staffing ratios or protocols that would have significantly changed flow during the study period, lessening the threat to internal validity due to period effect.
The more important limitation is related imperfect measures of PED crowding. Stang et al. (15) in their study of expert opinion of measures of PED crowding point out that ‘research on overcrowding is hampered by the lack of a universally accepted definition or measure tool’. The authors, however, cite a number of examples in which LWBS is used as a marker of crowding and suggest that in the PED, this measure is a reasonable marker of ED throughput; moreover, studies in adult or mixed EDs show good correlation between LWBS and other markers of ED crowding such as ED occupancy rates (17,18,20,26,27). As PED occupancy is not a tracked metric in our centre, we used the daily proportion of LWBS as a proxy for system’s level crowding or congestion. Nevertheless, our finding of an association between this measure and an increased odds of PICU admission may represent reverse causality as previously mentioned; and the observed inverse association with ED return visits may reflect patient dissatisfaction more generally, with crowding as only one of a number of factors that play into the decision to leave prior to ED care (16).
Similarly, our use of hospitalization as an outcome measure does not discriminate between necessary admissions related to the patient’s underlying condition and those that may result from deterioration of delayed ED care or errors associated with a crowded PED environment. We, however, attempted to control for underlying severity of ED presentation using CTAS score, but a larger prospective study is necessary to further clarify our observed associations.
CONCLUSIONS
We observed an association between odds of hospitalization and markers of PED flow. While causality or directionality cannot be determined through these analyses, provider awareness of the potential impact of conditions of crowding on admission rates provides a potential opportunity to mitigate patient safety risks. The Canadian Patient Safety Institute’s (CPSI) ‘Safety Competencies’ framework identifies six domains of patient safety, and we hope that our findings will contribute to two of these domains: Domain 4, ‘Manage Safety Risks’ and emphasizes ‘risk awareness, including situational awareness’ as a key element of Domain 4, as well as Domain 5 key competency by helping providers to ‘… evaluate the impact of organizational resource allocation, policies and procedures and culture’ (28).
Beyond the implications for patient safety within the CPSI framework, this study highlights the complex relationship between accepted measures of PED crowding and patient outcomes and the need for further definition and refinement of measures of flow and overcrowding in a PED. Perhaps this will serve as a starting point for future investigations using alternate methodologies and frameworks including quality improvement to better understand the observed associations between crowding and patient outcomes. Finally, given the lower rates of mortality and critical illness in PEDs compared to primarily adult centres, multicentre PED studies are needed to allow more meaningful analyses of the effect of overcrowding on these rare but important outcomes.
Acknowledgements
The Innovative Acute Care and Technologies Cluster Clinical Investigator Trainee Seed Grant, from the Child and Family Research Institute at BC Children’s Hospital, funded this project. Dr Doan is supported through a Michael Smith Foundation for Health Research Scholar’s Award.
References
- 1. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 2006;184:213–6. [DOI] [PubMed] [Google Scholar]
- 2. Hoot NR, Aronsky D. Systematic review of emergency department crowding: Causes, effects, and solutions. Ann Emerg Med 2008;52:126–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miró O, Antonio MT, Jiménez S et al. Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med 1999;6:105–7. [DOI] [PubMed] [Google Scholar]
- 4. Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via western Australian emergency departments. Med J Aust 2006;184:208–12. [DOI] [PubMed] [Google Scholar]
- 5. Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: Population based cohort study from Ontario, Canada. BMJ 2011;342:d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kennebeck SS, Timm NL, Kurowski EM, Byczkowski TL, Reeves SD. The association of emergency department crowding and time to antibiotics in febrile neonates. Acad Emerg Med 2011;18:1380–5. [DOI] [PubMed] [Google Scholar]
- 7. Sills MR, Fairclough D, Ranade D, Kahn MG. Emergency department crowding is associated with decreased quality of care for children with acute asthma. Ann Emerg Med 2011;57:191–200.e1–7. [DOI] [PubMed] [Google Scholar]
- 8. Sills MR, Fairclough DL, Ranade D, Mitchell MS, Kahn MG. Emergency department crowding is associated with decreased quality of analgesia delivery for children with pain related to acute, isolated, long-bone fractures. Acad Emerg Med 2011;18:1330–8. [DOI] [PubMed] [Google Scholar]
- 9. Sills MR, Fairclough D, Ranade D, Kahn MG. Emergency department crowding is associated with decreased quality of care for children. Pediatr Emerg Care 2011;27:837–45. [DOI] [PubMed] [Google Scholar]
- 10. Shenoi RP, Ma L, Jones J, Frost M, Seo M, Begley CE. Ambulance diversion as a proxy for emergency department crowding: The effect on pediatric mortality in a metropolitan area. Acad Emerg Med 2009;16:116–23. [DOI] [PubMed] [Google Scholar]
- 11. Michelson KA, Monuteaux MC, Stack AM, Bachur RG. Pediatric emergency department crowding is associated with a lower likelihood of hospital admission. Acad Emerg Med 2012;19:816–20. [DOI] [PubMed] [Google Scholar]
- 12. Cha WC, Shin SD, Cho JS, Song KJ, Singer AJ, Kwak YH. The association between crowding and mortality in admitted pediatric patients from mixed adult-pediatric emergency departments in korea. Pediatr Emerg Care 2011;27:1136–41. [DOI] [PubMed] [Google Scholar]
- 13. Weiss SJ, Derlet R, Arndahl J et al. Estimating the degree of emergency department overcrowding in academic medical centers: Results of the National ED Overcrowding Study (NEDOCS). Acad Emerg Med 2004;11:38–50. [DOI] [PubMed] [Google Scholar]
- 14. Graham J, Aitken ME, Shirm S. Correlation of measures of patient acuity with measures of crowding in a pediatric emergency department. Pediatr Emerg Care 2011;27:706–9. [DOI] [PubMed] [Google Scholar]
- 15. Stang AS, McGillivray D, Bhatt M et al. Markers of overcrowding in a pediatric emergency department. Acad Emerg Med 2010;17:151–6. [DOI] [PubMed] [Google Scholar]
- 16. Pines JM. The left-without-being-seen rate: An imperfect measure of emergency department crowding. Acad Emerg Med 2006;13:807; author reply 807–8. [DOI] [PubMed] [Google Scholar]
- 17. Hsia RY, Asch SM, Weiss RE et al. Hospital determinants of emergency department left without being seen rates. Ann Emerg Med 2011;58:24–32.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hwang U, McCarthy ML, Aronsky D et al. Measures of crowding in the emergency department: A systematic review. Acad Emerg Med 2011;18:527–38. [DOI] [PubMed] [Google Scholar]
- 19. Sinclair D. Emergency department overcrowding—Implications for paediatric emergency medicine. Paediatr Child Health 2007;12:491–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goldman RD, Macpherson A, Schuh S, Mulligan C, Pirie J. Patients who leave the pediatric emergency department without being seen: A case–control study. CMAJ 2005;172:39–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kulstad EB, Hart KM, Waghchoure S. Occupancy rates and emergency department work index scores correlate with leaving without being seen. West J Emerg Med 2010;11:324. [PMC free article] [PubMed] [Google Scholar]
- 22. Doan Q, Genuis ED, Yu A. Trends in use in a Canadian pediatric emergency department. CJEM 2014;16:405–10. [DOI] [PubMed] [Google Scholar]
- 23. Timm NL, Ho ML, Luria JW. Pediatric emergency department overcrowding and impact on patient flow outcomes. Acad Emerg Med 2008;15:832–7. [DOI] [PubMed] [Google Scholar]
- 24. Gravel J, Fitzpatrick E, Gouin S et al. Performance of the Canadian triage and acuity scale for children: A multicenter database study. Ann Emerg Med 2013;61:27–32.e3. [DOI] [PubMed] [Google Scholar]
- 25. Goldman RD, Ong M, Macpherson A. Unscheduled return visits to the pediatric emergency department-one-year experience. Pediatr Emerg Care 2006;22:545–9. [DOI] [PubMed] [Google Scholar]
- 26. Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med 2010;28:304–9. [DOI] [PubMed] [Google Scholar]
- 27. Bond K, Ospina MB, Blitz S et al. Frequency, determinants and impact of overcrowding in emergency departments in Canada: A national survey. Healthc Q 2007;10:32–40. [DOI] [PubMed] [Google Scholar]
- 28. Frank JR, Brien S (eds) on behalf of The Safety Competencies Steering Committee. The Safety Competencies: Enhancing Patient Safety Across the Health Professions. Ottawa, Canada: Canadian Patient Safety Institute, 2008. [Google Scholar]