Abstract
Family-based treatment (FBT) has emerged as a promising approach for medically stable youth with anorexia nervosa (AN). While there is evidence that therapists embrace the core principles of FBT, most face barriers in implementing the model with fidelity. Little research has been conducted to determine whether adhering to the core methods of placing parents in charge are sufficient in restoring weight in youth with AN. This study involved a chart review of youth under 16 years of age, treated by a Canadian tertiary care health centre-based eating disorders team (EDT). The purpose was to compare the weight gain of youth treated before and after the team was trained in FBT and shifted to empowering parents to be in charge of weight gain. As predicted, youth who participated in family sessions adhering to the ‘parents in charge’ approach (PIC, N=32) made greater gains in percentage of ideal body weight (%IBW) and were more likely to reach body weights within a healthy range as compared with youth (N=14) who participated in a ‘non-specific therapy’ (NST) involving expert driven psycho-educational family sessions. Youth whose parents were placed in charge of weight gain were also significantly less likely to be hospitalized on the psychiatry unit for weight restoration, had significantly shorter mean duration of stays on this unit, and required tube-feeding less frequently than youth who participated in NST. Collectively, the results suggest that placing parents in charge of refeeding promotes efficient weight gain, while decreasing the need for more intensive intervention.
Keywords: Adolescent, Anorexia Nervosa, Child, Eating disorders, Family therapy.
Anorexia nervosa (AN) is a serious mental illness characterized by a refusal to maintain a healthy body weight, leading to a malnourished body and brain. Family-based therapy, in which parents are placed in a leadership role in renourishing their child, has gained an increasing amount of evidence-based support as treatment for AN in adolescents (1). The widely disseminated family-based treatment (FBT) is now endorsed by The Canadian Paediatric Society for the treatment of children and adolescents with AN (2). FBT was developed at the Maudsley Hospital in London, England, and has been manualized by Lock and colleagues (3). It is an intensive, outpatient-based treatment in which parents are placed in charge of refeeding their child or adolescent with AN. Parents are viewed as the solution to the problem of AN, rather than its cause, and are empowered to stand up to AN, which is treated as an externalized illness. Compared to individual therapy for AN, FBT has been found to result in higher rates of weight gain and remission (1). FBT has also been found to have high acceptability ratings by youth and their family members (4,5).
Despite growing support, there is evidence that Canadian therapists are not practicing FBT with fidelity to the manualized model (6). Couturier and colleagues (6) found that most therapists endorse the core features of FBT, such as placing the parents in charge of refeeding, externalizing the illness and making weight restoration the initial focus. However, there was less agreement and adherence among clinicians on other features of FBT, such as the family meal and including siblings in sessions. As well, most clinicians endorsed the importance of involving a dietitian as part of their treatment team. Concern has been expressed that the lack of fidelity to the whole model of FBT might be compromising care (6); however, there has been little research reflecting the reality of clinical practice to examine whether partial FBT is effective. One study provided evidence that the core objective of uniting parents in the role of renourishing their child in an uncritical fashion is most predictive of greater weight gain, while sibling support may not contribute to weight gain (7). Moreover, other forms of delivering family therapy that have been shown to be effective, such as Behavioural Family Systems Therapy (8), share the core feature of placing parents in charge but do not share all other elements of FBT.
After receiving training and consultation with Drs Lock and Le Grange in June 2002 and reading the manualized treatment for FBT (3), the eating disorders team (EDT) shifted its philosophy from a focus on expert driven family psycho-education and support (with hospitalization for significant weight restoration when needed) to an approach which empowers parents to take the lead in refeeding their child, consistent with the principles of FBT. While the core FBT principles of placing parents in charge, externalizing the eating disorder and keeping the focus on weight gain were implemented, barriers (e.g., time, space) precluded the implementation of the family meal and having siblings at each session. Given that the team was not certified in FBT and fidelity to the full FBT approach was not practiced, the treatment provided is referred to as ‘parents in charge’ (PIC). The purpose of the present study was to conduct a chart review to examine whether the shift in philosophy to a PIC approach enhanced weight gain and decreased hospitalization in youth with AN. While weight gain is not the only important outcome measure in youth with AN, it is a significant predictor of eventual recovery (7,9).
METHOD
Study design
Patient information was obtained from the health records of children under age 16 who were diagnosed with AN and who participated in treatment through the specialty eating disorders outpatient team. Clinicians’ reports and tracking sheets were reviewed to obtain information on demographic characteristics and diagnoses, as well as medical information including height, weight, ideal body weight (IBW; based on height age), %IBW, medications, hospitalizations (e.g., unit and length of hospitalizations) and tube-feeding. At each consecutive month following first assessment, data was collected on weight, height, IBW and %IBW. Data was collected up to and including the 12th month of treatment or until the youth completed or terminated treatment with the specialty team. Those assessed and completing treatment between November 1997 and June 2002 fell into the Non-Specific Therapy (NST) group, while those assessed and treated between June 2002 and February 2011 were included in the PIC group. Treatment was primarily provided on an outpatient basis, although some youth did require inpatient hospitalization. Hospitalization occurred on either the medical unit (for medical stabilization) or the psychiatric unit (for weight restoration).
EDT
The eating disorders outpatient team included a psychologist, psychiatrist and a social worker, who were the primary therapists in conducting the PIC treatment; a dietitian and registered nurse were part of the consultation team. While there were some professional staff changes during the course of treatment, the psychologist (team leader) responsible for directing treatment remained the same, ensuring that in 2002 when the PIC approach was adopted new staff were versed in the FBT manual and were supervised in the PIC approach. Weekly clinical team meetings were held to discuss treatment progress for both the NST and PIC groups. The dietitian also had sessions as needed with parents for both treatments, but for the PIC group, the approach was to empower the parents in renourishing their child, and to provide dietetic advice as requested. The EDT remained involved in the treatment of the youth during hospitalizations. This study was approved by the health centre’s Research Ethics Board.
Treatment
Treatment for the PIC group was guided by the basic structure of the FBT manual by Lock and colleagues (3). In phase 1, the weight restoration phase, the parents were given a leadership role in taking charge of refeeding their child and reducing activity level. They were also coached in how to externalize the illness in order to take a united stance against AN, while also demonstrating empathy and support for their child. Youth were weighed at the start of each session and therapists coached parents in determining how to help their child return to health through achieving a healthy weight. While the family meal was not conducted, parents were guided in how to remain calm and supportive yet keep a consistent approach at meals, in which the need to eat was non-negotiable. During phase 2, control over eating was gradually returned to the adolescent. During phase 3, the focus of treatment turned to establishing a healthy adolescent identity and parental boundaries. Parents were invited to involve siblings in treatment but typically, due to competing obligations, families chose to have them come only for specific sibling sessions. Initial treatment sessions occurred on a weekly basis, with a gradual increase in the time between appointments as families progressed through the phases of treatment.
For the NST group, sessions were led weekly to biweekly by professionals on the EDT providing parents, youth and occasionally siblings, with the information, education, support and advice on how to help the youth recover from AN. While the treatment team was experienced in working with families, there was a belief at that time that weight restoration was most often achieved more efficiently and effectively in a controlled hospital setting led by experts on the EDT (10).
Participants
The consecutive charts of 46 youth, from age 9 up to and including age 15, who were assessed and treated for AN by the EDT at a tertiary paediatric health care centre in eastern Canada, were included in this study. The age range was chosen to reduce variability based on age and stage of development. All youth had a diagnosis of AN restricting subtype based on DSM-IV-TR criteria (11) and had at least one parent participate in treatment. Youth were considered to meet the AN restricting subtype as long as they met both criterion B (intense fear of gaining weight or becoming fat) and C (disturbance in the way in which one’s body weight or shape is experienced) and either criterion A (<85% IBW) or D (amenorrhea in postmenarcheal females). It should be noted that all participants would also meet the DSM 5 Criteria for AN restricting type. Fourteen youth qualified for the NST group (0 males, 14 females) and 32 youth qualified for the PIC group (3 males, 29 females). Youth in the PIC group (M=13.07 years, SD=1.89) were younger, on average, than youth in the NST group (M=14.36 years, SD=1.37) at the onset of treatment, t(44)=2.29, P=0.03. Age was not significantly correlated with the outcome variables, and therefore, was not considered further in the analyses. Approximately 44% (N=20) of youth had a comorbid psychiatric diagnosis, the most common being a mood disorder (N=10, 21.7%) or an anxiety disorder (N=9, 19.6%). The percentage of youth with one or more comorbidities did not differ between groups. Approximately 33% (N=15) of the youth were taking psychotropic medications including antidepressant (N=11, 23.9%) or antipsychotic medications (N=3, 6.5%) or both (N=1, 2.2%). The use of psychotropic medications did not differ between groups.
Data analysis
All statistical analyses were conducted using IBM SPSS Statistics 20. Independent-samples t tests and one-way analysis of variances (ANOVAs) were used to test significance in between-group differences for continuous variables (e.g., %IBW, length of hospitalization) and Fisher’s Exact Test was used to test between-group differences for categorical variables (e.g., rate of hospitalization, tube-feeding). Levene’s test was used to test the homogeneity of variance and was nonsignificant in all cases, indicating equal variances for the dependent variables across treatment groups. Cohen’s d (d) and Cramer’s V (φ) were used as measures of effect size. Two patients, both of whom participated in NST and were hospitalized on the psychiatry unit for greater than 200 days, were removed from the analyses on length of hospitalization because they were significant univariate outliers.
RESULTS
Percentage IBW
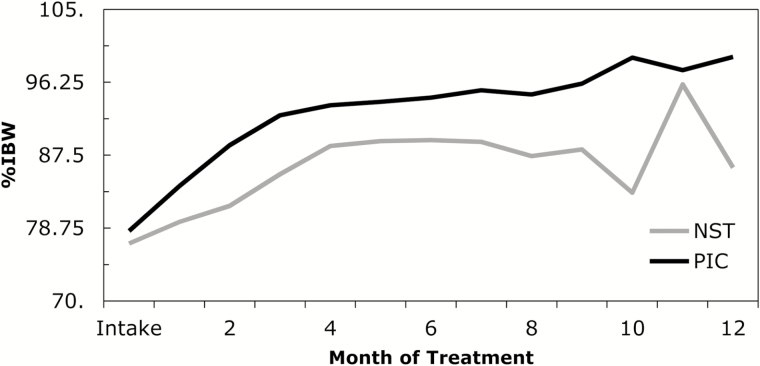
At the outset of treatment, the mean %IBW of youth who participated in NST (M=76.9, SD=6.9) and PIC (M=78.4, SD=7.5) was not significantly different. There was a trend for youth in the PIC group to have a higher %IBW at each month post-first assessment (see Figure 1) and the difference reached significance at 2 (F[1, 42]=12.72, P=0.001, d=1.33), 3 (F[1, 41]=10.56, P=0.002, d=1.17), 6 (F[1, 35]=4.28, P=0.046, d=0.83), 7 (F[1, 34]=5.94, P=0.02, d=0.94), 9 (F[1,23]=6.22, P=0.02, d=1.13) and 10 (F[1,17]=5.59, P=0.03, d=1.83) months post-intake assessment. Those in the PIC group were more likely to be seen for a longer period of time by the EDT (M=10.4 months, SD=2.3) compared to the NST group (M=7.5 months, SD=3.4), t(44)=3.34, P=0.002). Looking at %IBW achieved, youth who participated in PIC reached a higher mean percentage (M=96.4; SD=10.19) versus the NST group (M=90.5; SD=6.8), t(44)=1.98, P=0.05).
Figure 1.
Mean percentage ideal body weight at each month of treatment. PIC= Parents in Charge. IBW= Ideal Body Weight. NST= Non-Specific Therapy.
Hospitalizations
Youth who participated in NST were significantly more likely to require admission on the psychiatry unit for weight restoration during treatment than youth who participated in PIC (71.4% versus 34.4%, respectively), P=0.03, φ=0.34. Youth who participated in NST also had significantly longer admissions to this unit than youth who participated in PIC (M=50.0 versus 19.1 days, respectively), t(42)=2.31, P=0.03, d=0.74. However, youth who participated in either treatment did not differ in terms of rates of admission to the medical unit (21.4% NST versus 34.4% PIC), nor did they differ in length of stay on the medical unit (M=7.67 days NST versus 16.91 days PIC).
Tube-feeding
Youth who participated in NST were significantly more likely to have required tube-feeding while hospitalized (N=6, 42.9%) than youth who participated in PIC (N=2, 6.3%), P=0.006, φ=0.44.
DISCUSSION
While both groups gained weight during treatment, this study suggests that the shift to a philosophy of placing parents in charge of renourishing their child with AN contributed to more efficient weight restoration, with less hospitalization for the purpose of refeeding and minimal need for tube feeding. While the FBT manual was not followed with complete fidelity, the central tenets of the model (i.e., empowering parents to unite and take charge, supporting the child by externalizing AN, keeping the focus on weight gain) were adhered to, and proved to be effective in restoring weight in youth with AN, as in previous research on FBT (12,13). This is in keeping with the findings of Ellison and colleagues (7) who found that parental control is the central predictor of change leading to weight gain in FBT. Weight restoration is a significant predictor of eventual treatment outcome and recovery (9,14). Moreover, given that specialized outpatient treatments account for a relatively small proportion of costs associated with treatment for AN (15), training therapists to deliver an FBT guided approach is more cost-effective for the patient and the health care system, as compared to inpatient hospitalization.
LIMITATIONS
The sample size was small and because data was gathered through chart review, random assignment to either the PIC or NST group was not possible; therefore, causality cannot be inferred. As well, because the two treatments were offered during different time periods, nonspecific factors in the therapeutic situation or temporal factors may have influenced the results. These factors may have been mitigated by the consistency of the treatment team over the two time periods and their involvement in outpatient and inpatient care. The shift in treatment to placing parents in charge was the most significant change over the period of study.
Directions for future research
In 2015, the EDT was expanded and given the mandate to receive training and full supervision to implement the FBT model with fidelity. It will therefore be possible to examine whether the full FBT model enhances outcome over the partial implementation of the model (PIC) in a longer-term study. Given the important role of parents in FBT and the high levels of distress brought on by this disorder (16), future research will need to examine the most effective ways of providing parents with the emotional support and coaching needed to help them feel confident and equipped to play a central role in restoring their child’s weight and well-being (17–19).
Acknowledgements
The authors would like to acknowledge Lisa Parkinson McGraw, Dietitian, Bonny Halket, Administrative Assistant, Judy Ashley LeBlanc, Registered Nurse, Laurie Kennedy, Research Assistant and Dr Gordon Butler, Psychologist, for their respective contributions to this research project.
References
- 1. Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: A systematic review and meta-analysis. Int J Eat Disord 2013;46:3–11. [DOI] [PubMed] [Google Scholar]
- 2. Findlay S, Pinzon J, Taddeo D, Katzman D. Family-based treatment of children and adolescents with anorexia nervosa: Guidelines for the community physician. Paediatr Child Health 2010;15:31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lock J, Le Grange D, Agras WS, Dare C. Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford Press, 2001. [Google Scholar]
- 4. Krautter T, Lock J. Is manualized family-based treatment for adolescent anorexia nervosa acceptable to patients? Patient satisfaction at the end of treatment. J Fam Ther 2004;26:66–82. [Google Scholar]
- 5. Le Grange D, Gelman T. Patients’ perspective of treatment in eating disorders: A preliminary study. S Afric J Psychol 1998;28:182–6. [Google Scholar]
- 6. Couturier J, Kimber M, Jack S, Niccols A, Van Blyderveen S, McVey G. Understanding the uptake of family-based treatment for adolescents with anorexia nervosa: Therapist perspectives. Int J Eat Disord 2013;46:177–88. [DOI] [PubMed] [Google Scholar]
- 7. Ellison R, Rhodes P, Madden S, Miskovic J, Wallis A, Baillie A, Kohn M, Touyz S. Do the components of manualized family-based treatment for anorexia nervosa predict weight gain? Int J Eat Disord 2012;45:609–14. [DOI] [PubMed] [Google Scholar]
- 8. Robin AL, Siegel PT, Moye AW, Gilroy M, Dennis AB, Sikand A. A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. J Am Acad Child Adolesc Psychiatry 1999;38:1482–9. [DOI] [PubMed] [Google Scholar]
- 9. Accurso EC, Ciao AC, Fitzsimmons-Craft EE, Lock JD, Le Grange D. Is weight gain really a catalyst for broader recovery? The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behav Res Ther 2014;56:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kennedy SH, Abbass A. Inpatient treatment for anorexia nervosa and bulimia nervosa. In: Kennedy SH, ed. University of Toronto Handbook of Eating Disorders. Toronto: University of Toronto, 1993:30–6. [Google Scholar]
- 11. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edn, Text Revision. Washington: The Association, 2000. [Google Scholar]
- 12. Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry 2010;67:1025–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Russell GF, Szmukler GI, Dare C, Eisler I. An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry 1987;44:1047–56. [DOI] [PubMed] [Google Scholar]
- 14. Doyle PM, Le Grange D, Loeb K, Doyle AC, Crosby RD. Early response to family-based treatment for adolescent anorexia nervosa. Int J Eat Disord 2010;43:659–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lock J, Couturier J, Steward Agras W. Costs of remission and recovery using family therapy for adolescent anorexia nervosa: A descriptive report. Eat Disord 2008;16:322–30. [DOI] [PubMed] [Google Scholar]
- 16. Treasure J, Murphy T, Szmukler G, Todd G, Gavan K, Joyce J. The experience of caregiving for severe mental illness: A comparison between anorexia nervosa and psychosis. Soc Psychiatry Psychiatr Epidemiol 2001;36:343–7. [DOI] [PubMed] [Google Scholar]
- 17. Hopf RB, Hoste RR, Pariseau C. Parent support as an adjunct to family therapy. In: Loeb KL, Le Grange D, Lock J, eds. Family Therapy for Adolescent Eating and Weight Disorders: New Applications. New York: Routledge, 2015:139–54. [Google Scholar]
- 18. Rhodes P, Baillee A, Brown J, Madden S. Can parent-to-parent consultation improve the effectiveness of the Maudsley model of family-based treatment for anorexia nervosa? A randomized control trial. J Fam Ther. 2008;30:96–108. [Google Scholar]
- 19. Stillar A, Strahan E, Nash P, et al. The influence of carer fear and self-blame when supporting a loved one with an eating disorder. Eat Disord 2016;24:173–85. [DOI] [PubMed] [Google Scholar]