Abstract.
Schools convene many people together for a prolonged time, facilitating spread of respiratory pathogens and amplifying epidemics. Crowded Bangladeshi schools lack the infrastructure to support optimal cough etiquette behaviors. We collected formative data on current practices from four elementary schools, and developed and piloted a low-cost cough etiquette intervention, promoting coughing and sneezing into upper sleeves at four additional schools. We trained teachers to lead behavior change sessions during regular hygiene classes for 4 weeks. We evaluated intervention acceptability, feasibility, and potential for sustainability at 1 month and at 14 months after the intervention commenced. At baseline, among 63 observed students, 58 (92%) coughed/sneezed into open air, five (8%) covered coughs/sneezes with their hands, which were not subsequently washed with soap and water as they judged this infeasible. After 4 weeks, among 70 observed students, 27 (39%) coughed/sneezed into upper sleeves, 33 (47%) into open air, and 10 (12%) covered with hands. After 14 months, among 230 observed students, 13 (6%) used upper sleeves, 154 (67%) coughed/sneezed into open air, and 59 (26%) covered with hands. Students reported that coughing/sneezing into upper sleeves was simple and protected them and their classmates from germs. This school-based intervention was acceptable and feasible, and resulted in short-term reductions in coughing/sneezing into open air, but these habits of comparatively new behavior were not sustained as teachers ceased behavior change session delivery. Strategies to support longer-term adoption of habits should be considered.
INTRODUCTION
Schools are efficient settings for the spread of infectious respiratory diseases, facilitating outbreaks and expanding epidemics by bringing many individuals together in a limited area for prolonged periods.1–4 Studies conducted both in high- and low-income countries including Bangladesh5 suggested that close proximity interaction in schools and within students’ social network enhances the transmission of infectious disease, particularly influenza, in schools, households, and communities.6–15 Focused research on coughing and sneezing behaviors and habits, however, has been rare.16–18
To prevent the spread of respiratory pathogens, the U.S. Centers for Disease Control and Prevention recommends 1) covering the nose and mouth using tissues when coughing and sneezing, and disposing of used tissues in the nearest waste container; 2) washing hands with soap and water, alcohol-based hand rub, or antiseptic hand wash after contact with respiratory secretions and contaminated objects; and 3) if tissues are unavailable, using the upper sleeves or elbow, not hands, to cover coughs and sneezes.19
Several intervention trials in low- and middle-income countries concluded that intensive handwashing promotion in school settings can reduce diarrheal and respiratory disease incidence and significantly reduce student absenteeism.20–27 Handwashing with soap can reduce the risk of respiratory infection by 16–23% and reduce laboratory-confirmed influenza by 50% among school-aged children.16,24,28 A study of respiratory hygiene practices among school-aged children in urban and rural Bangladesh in 2009 did not observe any handwashing with soap and water after coughing and sneezing and found that 85% of school children coughed or sneezed into the open air.17
Barriers to ensuring hand hygiene or using tissues to cover coughs and sneezes in most Bangladeshi schools include lack of access to running water and the cost of supplying hand cleansing agents and tissues, which are not affordable for a large segment of the population living below the poverty line of US$ < 1 per day.17,29 In addition, coughing and sneezing occurs frequently, and it is not feasible for school children to wash their hands after each event. Using upper sleeves or elbows to cover coughs and sneezes might be a feasible method to promote cough etiquette behaviors in Bangladeshi schools.17,30,31 Students offer a unique opportunity to communicate public health messages to the family and larger community,25,32 which might be a useful strategy for wider prevention efforts, especially during epidemics. School-based hygiene programs and provision of take home packs also resulted in students acting as health change agents; subsequently, transferring knowledge in the home, resulting in an increase in family and siblings’ hygiene practices.32–34
The objectives of the paper were to describe 1) school children’s current practices and perceptions of respiratory hygiene; 2) the effectiveness of an intervention to increase the frequency of appropriate cough etiquette practices among school children; and 3) the acceptability, feasibility, and potential for sustainability of this intervention.
METHODS AND MATERIALS
Study setting and participants.
We conducted this study among elementary school students in urban and rural Bangladesh from May 2011 to September 2013. We collected a list of schools in rural areas from the United Nations Children’s Fund (UNICEF) and a list of urban schools from the Divisional Education Department and subdistrict education officers. Fieldworkers then visited 110 schools, and we purposively selected eight schools to ensure a range of settings. The four urban schools were located in Dhaka, and the four rural schools were located in Mymensingh, in north-central Bangladesh. Half were government schools and half were nongovernment schools; all enrolled both boys and girls.
Step 1: formative study.
Out of eight schools, two urban and two rural schools participated in this formative study in September–November 2011. We structured our study questionnaires and synthesis of findings using the Integrated Behavioral Model for Water, Sanitation, and Hygiene (IBM-WASH) adapted for school WASH interventions (see Supplemental Table 1).35 The model, widely adapted for the design of WASH behavior change interventions,36–39 theorizes that the adoption of new WASH behavior and technologies is influenced by 1) contextual dimension–the social and physical environment in which the WASH behaviors and technologies are implemented; 2) a psychosocial dimension–social and psychological factors that affect WASH practices; and 3) a technological dimension factors affecting adoption of WASH technologies.
We examined contextual factors related to school policies, allocation of responsibilities, teacher skills, experience and workload, classroom size and crowding, socioeconomic status of the students, and organization of the school day (Supplemental Table 2). We examined psychosocial factors including leadership from school system, shared goals, descriptive and injunctive norms, self-efficacy, and knowledge (Supplemental Table 2).35,40
Notably, our intervention only addressed psychosocial factors influencing coughing and sneezing into upper sleeves during the behavior change communication sessions.
Structured observations.
Similar to Nasreen et al.,17 we conducted 4-hour-long observations in schools. We prepared a standard cough etiquette behavior assessment tool to observe and record coughing and sneezing events once per student. Fieldworkers informed school administrators, but not individual students, about the purpose of the visit. Fieldworkers placed themselves in classrooms and in a convenient place at each school compound and noted any cough etiquette behavior–related events on a precoded structured observation form for cough etiquette behavior practices. Fieldworkers recorded the grade level of the student that had one of the events of interest and also whether the student coughed/sneezed into the open air or upper sleeves, covered his/her mouth while coughing/sneezing, or used any material to cover cough/sneezes including handkerchief, tissue paper, or scarf. Fieldworkers conducted observations in each of the four schools on three consecutive days.
Baseline student survey.
A previous study conducted in urban and rural Bangladesh found 0% of school children coughed and sneezed into their upper sleeves. A sample of 88 students would provide 80% power and 95% confidence if after the intervention 20% of students coughed or sneezed on their upper sleeve. We increased the targeted number of students to 200 to provide greater power given clustering by school and class. We selected 50 students from each school. Fieldworkers prepared a list of all students from grades 4 and 5 using class register books and then randomly drew 25 student names from an envelope from each grade.
Qualitative interviews.
We purposively selected participants for in-depth interviews and focus group discussions based on their enrolment in grade 4 or 5 and availability and willingness to participate. Fieldworkers conducted 16 in-depth interviews: one each with the head and science teacher, and with the school management committee and parent–teacher association members from each school. They facilitated 12 focus group discussions: one each with the male students, female students, and with the assistant teachers and school management committee members from each school to gather information related to perceptions on hygiene-related topics, suggestions for the design and content of the set of interventions, and the process of implementation. We crosschecked findings from different methods to increase validity.
Step 2: intervention development.
We systematically designed the intervention. Based on findings from Step 1, we concluded that handwashing after every cough and sneeze would be neither feasible nor practical. We organized an intervention development workshop in January 2012 with teachers, school management committee and parent–teacher association members, study staff, and a co-investigator. We shared findings from Step 1 and sought feedback regarding acceptability and feasibility of coughing and sneezing into upper sleeves.
Development of behavior change communication materials.
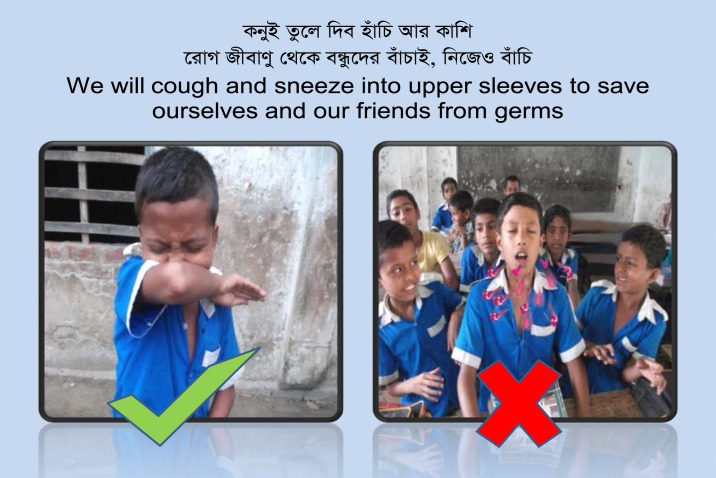
Based on feedback, we developed pictorial flipcharts and cue cards to address 1) skills and self-efficacy of coughing and sneezing into upper sleeves; 2) perceived susceptibility and severity of sickness; and 3) perceived benefits and barriers for cough etiquette behaviors. The materials depicted the potential consequences of poor cough etiquette practices and both health and nonhealth benefits of coughing and sneezing into upper sleeves. Figure 1 display two pictures that encouraged coughing and sneezing into upper sleeves, not to open air. We trained teachers to complement pictures with messages that 1) coughing and sneezing into open air can transmit disease to others, and this is disgusting; 2) use of upper sleeve is an easy method to protect yourself and others from germs; and 3) if you do so, your friends will approve of you. We also developed short entertaining songs to encourage students to cough and sneeze into their upper sleeves. We pretested these materials in schools and conducted four focus group discussions with teachers and four with the students to assess appropriateness, feasibility, and acceptability of materials.
Figure 1.
Cue card with English translation to promote respiratory hygiene practices in schools in urban Dhaka and rural Mymensingh, Bangladesh, 2013. This figure appears in color at www.ajtmh.org.
Step 3: piloting the intervention.
We piloted the intervention in the remaining four schools in June 2012 by demonstrating to students how to cough and sneeze into upper sleeves, and training teachers to lead, deliver, and continue behavior change communication sessions in conjunction with the existing weekly hygiene classes. We invited school teachers to International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) and held a 1 day training on how to conduct sessions and deliver messages using flipcharts. This training of teachers aimed to create a resource person in schools to promote cough etiquette practices, to deliver communication sessions, and to ensure ownership of the project for long-term sustainability of cough etiquette behavior change.
We assessed the intervention 4 weeks after commencement of the sessions in July 2012. We provided schools with 12 × 17 inch (31 × 43 cm) cue cards (Figure 1) and placed them inside the classrooms to remind students to cough and sneeze into their upper sleeves. We formed a hygiene committee of 18 members: 10 students of grade 4 and 5 (as members), one head and two assistant teachers (as secretary and assistant secretary), two education officials (as advisor and co-advisor), one janitor (as supportive staff), and one school management committee and one parent–teacher association members (as chair and co-chair) in each school. Teachers were responsible to conduct cough etiquette classes using the behavior change communication materials (flipcharts and cue cards). Students were responsible to monitor peers and encourage the recommended practices.
Structured observations.
Fieldworkers monitored the intervention for 1 month when they conducted structured observations on six occasions (days 1, 2, 3, 7, 14, and 30 after the first class on respiratory hygiene). Fieldworkers identified “doers” (students who practiced the promoted behavior) and “non-doers” (students who did not practice the promoted behavior). One month after the intervention commenced, we conducted an assessment with the doers and non-doers (from grade 4 and 5), parents, and teachers. Based on availability and willingness to participate, fieldworkers selected participants for 12 focus group discussions: four with students of grades 4 and 5 who had been observed as cough etiquette behavior “doers” and four with “non-doers” from the structured observations, and with the teachers, school management committee, and parent–teacher association members.
Pocket voting.
Fieldworkers also conducted four anonymous pocket voting exercises with a subset sample of 96 students of grades 4 and 5 to understand their reported knowledge and practices.41,42 This was a participatory tool to assess hygiene and sanitation particularly for handwahsing practices.41 This approach allowed students to communicate their perspective by voting confidentially.
Using class register books, fieldworkers prepared a list of all students and then drew 24 student names randomly from an envelope for each school. After selection, fieldworkers gave each student a numerical identification to facilitate the session and analysis, introduced the session, and explained the process of voting. We structured the pocket voting questions based on the IBM-WASH model35 to assess students’ knowledge of respiratory diseases; their use of upper sleeves at school and at home; their feelings of vulnerability to respiratory diseases; their subjective, descriptive, and injunctive norms; and their self-efficacy to cough or sneeze into their upper sleeves.
Step 4: 14-month follow-up assessment.
To explore the potential for sustainability of the targeted behaviors, fieldworkers revisited schools in August 2013, 14 months after the intervention commenced and 13 months after the study staff withdrew. Fieldworkers conducted structured observations of all students in each intervention school on three consecutive school days. They then conducted 12 focus group discussions with the students of grades 4 and 5 classified during this round of observations as “doers” and “non-doers” and with the teachers, school management committee, and parent–teacher association members to understand their perceptions, perceived benefits, and barriers regarding the use of upper sleeves when coughing or sneezing.
Research design and analysis.
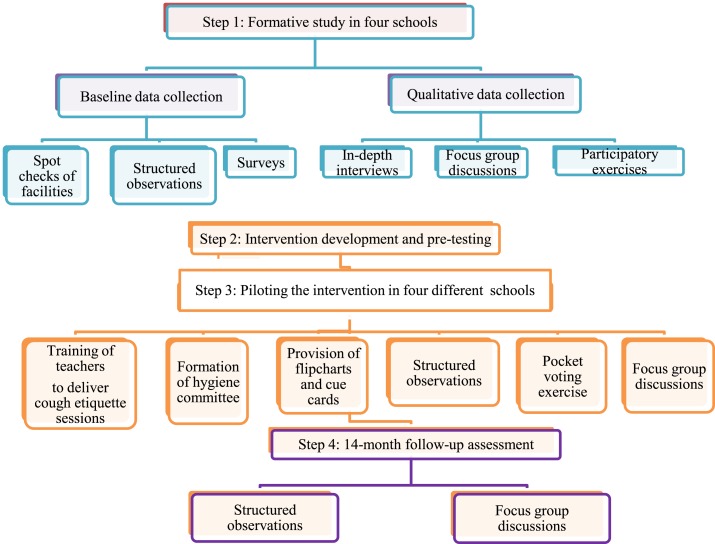
In this pilot study, we collected both qualitative and quantitative data using a baseline survey, follow-up observations of uptake, and qualitative assessments (Figure 2).We conducted the interviews in Bengali. We determined frequencies for the quantitative and pocket voting data. For comparison of behaviors at three time points (baseline, pilot, and 14-month assessment), we performed the difference of proportion test. For the qualitative data analysis, trained fieldworkers transcribed the audio-recorded focus group discussion and in-depth interview data and then translated it into English. We prepared the interview guideline based on research objectives and conducted thematic content analysis to provide descriptive and systematic results. We analyzed each in-depth interview and each focus group discussion separately; however, we have drawn inferences collectively from both types of data and presented these in the results.
Figure 2.
Piloting cough etiquette practices in schools in urban Dhaka and rural Mymensingh, Bangladesh, 2011–2013 study phases and activities. This figure appears in color at www.ajtmh.org.
Ethics.
We obtained permission from the Government of Bangladesh Divisional Primary Education Office, Dhaka, to work in specific schools in Dhaka and Mymensingh districts for research purposes. All teachers provided written consent, and students assented to participate before we collected data from them. The icddr,b Ethical Review Committee reviewed and approved the study protocol.
RESULTS
Formative study of current perception, practices, and barriers.
Table 1 shows the physical environment of the study schools. Students had limited access to toilets. Table 2 describes the study participants; most were students of grade 4 and 5 with a mean age of 10.1 years old (standard deviation [SD] 1.3). Fieldworkers observed 63 students coughing and sneezing; 58 (92%) coughed and sneezed into the open air, and the remaining five (8%) covered their coughs and sneezes with their hands, but did not wash hands with soap and water afterward (Table 3).
Table 1.
Physical environment in elementary schools in urban Dhaka and rural Mymensingh, Bangladesh, 2011–2013
| Indicators | Urban govt. schools | Urban registered schools | Rural govt. schools | Rural registered schools |
|---|---|---|---|---|
| Baseline formative study schools | ||||
| No. of students | 1,089 | 640 | 468 | 335 |
| No. of toilets | 2 | 1 | 1 | 1 |
| Source of water | Piped water supply | Deep tube–well | Shallow tube–well | Shallow tube–well |
| Pilot and 14-month follow-up assessment study schools | ||||
| No. of students | 1,047 | 341 | 475 | 296 |
| No. of toilets | 4 | 1 | 1 | 1 |
| Source of water | Piped water supply | Deep tube–well | Shallow tube–well | Shallow tube–well |
Table 2.
Socio demographic characteristics of study respondents in urban Dhaka and rural Mymensingh, Bangladesh, 2011–2013
| Indicators | Formative study n (%) | Pilot n (%) | 14-month follow-up assessment n (%) |
|---|---|---|---|
| Type | |||
| Student | 248 (89) | 144 (87) | 27 (55) |
| Teachers and school management committee members | 30 (11) | 22 (13) | 22 (45) |
| Sex | |||
| Female | 146 (53) | 87 (52) | 29 (59) |
| Education | |||
| Grade IV | 124 (45) | 72 (43) | 13 (27) |
| Grade V | 124 (44) | 72 (43) | 14 (29) |
| Elementary | 6 (2) | 6 (4) | 4 (8) |
| Secondary | 9 (3) | 0 | 3 (6) |
| Higher secondary | 7 (3) | 8 (5) | 5 (10) |
| Graduation | 8 (3) | 8 (5) | 10 (20) |
| Occupation of student guardian | |||
| Farmer | 49 (20) | 19 (13) | 2 (7) |
| Salaried government job | 39/(16) | 26 (18) | 7 (26) |
| Small trader | 36 (15) | 22 (15) | 3 (11) |
| Small business | 32 (13) | 33 (23) | 9 (33) |
| Non-agri labor | 27 (11) | 24 (17) | 6 (22) |
| Van/rickshaw operator | 23 (9) | 12 (8) | – |
| Other* | 42 (17) | 8 (6) | – |
| Monthly income of teachers and school management committee members in US$ | |||
| No income | 3 (10) | 3 (14) | 4 (18) |
| 63–125 | 11 (37) | 10 (45) | 7 (32) |
| 126–188 | 10 (30) | 5 (23) | 9 (41) |
| Above 189 | 7 (23) | 3 (14) | 2 (9) |
Carpenter, driver, maid, and boatman.
Table 3.
Differences in observed cough etiquette practices after coughing and sneezing at baseline, pilot, and follow-up in urban Dhaka and rural Mymensingh, Bangladesh, 2011–2013
| Formative study N = 63 n (%) | Pilot intervention N = 70 n (%) | 14-month follow-up assessment N = 230 n (%) | |
|---|---|---|---|
| Covered with disposable tissues | 0 | 0 | 0 |
| Covered with hands | 5 (8) | 10 (12) | 59 (26)*† |
| Washed hands with water and soap | 0 | 0 | 0 |
| Washed hands with water only | 0 | 0 | 0 |
| Into upper sleeves | 0 | 27 (39)* | 13 (6)*† |
| Covered with dopatta (scarf) | 0 | 0 | 4 (2) |
| Into open air | 58 (92) | 33 (47)* | 154 (67)*† |
Significant difference compared with formative (P ≤ 0.05).
Significant difference compared with pilot (P ≤ 0.05).
In the 200-student baseline survey (Table 4), one student reported that coughing and sneezing without covering the mouth and nose with hands or handkerchief causes flu, 88 (44%) reported that they never knew about the recommendation to wash hands with soap after covering coughs or sneezes with hands, 36 (18%) reported handwashing after coughing and sneezing as unimportant, and 28 (14%) judged it to be infeasible.
Table 4.
Reported knowledge, practice, and barriers related to cough etiquettes using closed-ended questions during the baseline formative study in urban Dhaka and rural Mymensingh, Bangladesh, 2011–2013
| Indicators | N = 200% (n) |
|---|---|
| Believe that coughing and sneezing without covering the mouth and nose by hands or handkerchief causes flu | 0.5 (1) |
| Believe that washing hands after coughing, sneezing, or nose picking is not feasible/practical practice | 14 (28) |
| Believe that bathing in the pond or cold water causes flu | 44 (88) |
| Practice handwashing with soap and water after coughing, sneezing, or nose picking | 2 (5) |
| Never heard about the requirement of handwashing with soap after covering coughs or sneezes with hands | 44 (88) |
| Believe that handwashing with soap and water after coughing, sneezing, or nose picking is not important | 18 (36) |
| Believe that handwashing with soap and water after coughing, sneezing, or nose picking is not feasible | 14 (28) |
| Believe that not washing hands with water and soap after coughing and sneezing may have high chance of causing disease | 36 (72) |
| Believe that covering coughs and sneezes among friends and family is not necessary | 16 (32) |
During the baseline qualitative exploration with 48 students and 30 teachers and school management committee members, most (52/78) of them thought that it would be safer if respiratory events were covered with hands, tissues, or a handkerchief. However, none thought that if they covered their coughs or sneezes with hands, and/or tissues, that they needed to wash their hands with soap and water afterward, and dispose used tissues in a waste container. A male student of grade 5 at an urban school said “Covering mouth with hands while coughing and sneezing is enough to reduce the transmission. We never heard of people washing hands after such events.”
Respondents reported that they could not practice optimal cough etiquette as they had no access to soap in schools; tissues or handkerchiefs because of the cost; and that the use of soap for coughing and sneezing, and disposing used tissues in waste container were not perceived as social norms. None of the students were familiar with the term “respiratory illnesses” and more than three quarters (40/48) of them incorrectly identified the route of transmission of respiratory illness by relating it to an “evil wind” and failure to take preventive measures. One male student of grade 4 at a rural school explained “Evil wind (aoula batas) makes us ill for which we catch fever, colds, coughs, sneezes and others. Thus we shall behave well, and visit indigenous doctors for treatment.” After the study team defined the term, some of the students identified respiratory illnesses correctly as “communicable” and the mode of transmission as “airborne.”
All teachers, school management committee members, and students perceived that using upper sleeve would be more practical than carrying a handkerchief or tissues, or washing hands with soap. Students mentioned that their motivations/drivers of coughing and sneezing into upper sleeves included perceived threats of catching a cold, cough and sneeze, and perceived health benefits of not catching or early recovery from those illnesses. One female student of grade 5 at an urban school said: “If I cough and sneeze into upper sleeves, I will remain healthy and thus my father can save treatment and medicine costs also! I can also come to school regularly and eat whatever I want.”
Piloting the intervention for acceptability and feasibility.
Table 3 shows that during the 1-month pilot intervention period, 70 student coughing and sneezing events were observed at three intervention schools and none were observed at one urban school. Of these 70, 39% (27) of students coughed or sneezed into their upper sleeve, none used a handkerchief or tissue, 47% (33) coughed and sneezed into the open air, and 14% (10) covered their coughs and sneezes with their hands, but did not wash their hands with soap and water afterward.
During the pocket voting exercise, 79% (76) of students reported that coughing and sneezing directly on others’ faces transmits respiratory diseases. Regarding injunctive norms (perception that others want you to practice a given behavior), 80% (77) of students reported that their teachers wanted them to cough and sneeze into their upper sleeves, 69% (66) reported that their friends wanted them to cough and sneeze into their upper sleeves and 76% (73) reported that they had a strong desire to cough and sneeze into their upper sleeves. Regarding descriptive norms (perception of usual practices among others in the group), 81% (78) of students reported that their friends coughed and sneezed into their upper sleeves. Regarding perceived risk, 86% (83) of the students reported that chances of getting flu was higher if they did not use upper sleeves to cover their cough and sneezes. Regarding self-efficacy, 83% (80) of them mentioned that they were confident on how to use the upper sleeves properly.
During the qualitative assessment of the pilot intervention with 48 (24 doers and 24 non-doers) students, and 22 teachers and school management committee members, “the doers” explained that they adopted the practice because it was easy to comply with, would keep them and other students healthy, and they feared that teachers or other students, who saw them coughing and sneezing into their hands or into the open air, would feel disgusted. “Doer” students mentioned their motivation to cough and sneeze into the upper sleeve was to protect the spreading of germs into the air, to keep the school environment healthy, and to protect themselves and their friends from germs and disease transmission. A female science teacher at an urban school explained the benefits of the new behavior in this way “This is a totally new and effective method that we had not heard of before. We like to use upper sleeves because it is easy to practice and is free.”
Students who were observed coughing and sneezing into the open air or into their hands without subsequent handwashing reported that they had not become habituated to the behavior during the 30-day intervention. However, they tended to report themselves as “doers” during the interviews. A female student in grade 5 at a rural school explained that “I always try to use upper sleeves, but I can’t remember after each event because I am not habituated yet.”
All students, teachers, school management committee, and parent–teacher association members reported that the idea of using upper sleeves for coughing and sneezing was acceptable and feasible because of its innovativeness, ease, and zero cost. They also reported that this practice had created a norm for positive behavior change in the school compound in which both teachers and students monitored each other and reminded “non-doers” to use upper sleeves. They felt that over time this practice would become a habit and there would be more and more “doers”. A male assistant teacher at a rural school reported “This (coughing and sneezing into the upper sleeves) is something new that the students enjoy practicing, which also motivates other students and teachers as well. Once in the classroom, I sneezed in the open air and some of the students told me to use my upper sleeves.”
Both students and teachers disseminated information and acted as role models for their family members, relatives, and neighbors that could lead to broad and sustained adoption of this practice in the wider community. Some (16/70) teachers and students shared that promoting the use of upper sleeves could be enforced and encouraged if all students had to obey a rule. One female head teacher at an urban school said “I included some questions on promoted behaviors in our existing physical exercise exams to explore the level of respiratory hygiene knowledge and practices among students and I found all of them answered all questions properly.”
Follow-up assessment at 14 months to explore sustainability.
Fieldworkers again observed hygiene practices 14 months after the pilot intervention commenced. Out of 230 students’ coughing and sneezing events, 13 (6%) students used their upper sleeves after coughing (5) and after sneezing (8), and 4 (2%) covered their coughs and sneezes with a dopatta (scarf). However, 154 (67%) students coughed and sneezed into the open air, and 59 (26%) covered their coughs and sneezes with hands and did not wash them with water and soap afterward (Table 3).
During focus group discussions convened 14 months after the intervention with 27 (13 “doer” and 14 “non-doer”) students and 22 teachers and school management committee members, the “doers” reported that coughing and sneezing into upper sleeves was a fun and easy method that protected them and their classmates from germs and disease transmission. The “non-doer” students who did not use their upper sleeves reported that they could not become habituated to the new recommended behavior, and therefore, did not adopt it. Lack of practice among family or community members was also reported as a barrier for habit formation. Teachers and school management committee members reported the previous habitual practice of coughing and sneezing into the open air or into hands, which was practiced for many years, likely acted as a barrier toward the use of upper sleeves. However, teachers reported that they reminded students to cough and sneeze into upper sleeves both during the regular textbook classes and hygiene classes, and when they observed a student cough/sneeze into open air or covered with hands. Students reported that the behavior was comparatively new for them to remember and continue practices. A female teacher at a rural school said “We have also newly learned about the use of upper sleeves, though we have been coughing and sneezing into open air for decades. This is a new idea to adopt that we teachers even forget, so I guess it is difficult for students to remember and continue practicing. Therefore, I believe such interventions should be prolonged to make students habituated.”
Half (11/22) of the teachers and school management committee members reported that they stopped the behavior change communication sessions 6 months after commencing the intervention because they perceived that the students had acquired adequate knowledge about the use of upper sleeves. They added that coughing and sneezing are rare events; therefore, continuing weekly sessions on cough etiquette behavior change was not necessary. A male assistant teacher at an urban school explained that “Students rarely suffer from coughing and sneezing; therefore, we don’t emphasize this during hygiene classes.”
DISCUSSION
Formative study.
Cough etiquette practice was suboptimal and not common among school children in Bangladesh, with handwashing after respiratory events almost nonexistent. Previously in Bangladesh, Nasreen et al.17 reported that the majority (> 90%) of students coughed and sneezed into the open air. An observational study among all ages in a high-income country during an influenza pandemic also found low prevalence (1.3%) of using elbows or arms to cover coughs.16
Although the teachers and students at both urban and rural schools knew that using a tissue to cover coughs and sneezes could prevent the spread of germs, they did not know that if they coughed or sneezed into their hands that they should wash them afterward and judged this as an infeasible practice. Similarly, our previous formative study found people were not aware that their behavior could affect their health and the health of others.30 The major barriers were lack of knowledge about germ theory and proper cough etiquette, and limited access to soap, tissues, or handkerchiefs.
Piloting the intervention.
After 1 month of intervention, the proportion of students seen coughing and sneezing into their upper sleeve increased from 0% to 39% and there was a 45% reduction of coughing and sneezing into the open air. We attributed this success to the novelty and simplicity of the intervention. Students found the target behaviors fun and were comfortable reminding friends and even teachers to practice the recommended cough etiquette behaviors, suggesting that it might be worth adding an additional intervention focus on reminding peers, elders, and those in authority.43,44 This intervention met basic criteria of a sustainable program including 1) acceptable to schools and teachers; 2) feasible to implement on an ongoing basis with minimal resources; and 3) flexible and adaptable.45
Teachers led sessions using pictorial flipcharts and cue cards as part of the regular hygiene class curriculum. School hygiene committees monitored and reminded students to encourage habit formation, and contributed to improvements in students’ cough etiquette behavior change. The intervention increased knowledge and also established a norm reinforced by the hygiene committee, peers, and teachers. Students appreciated the health benefits of coughing and sneezing into upper sleeves. Role modeling to disseminate information and feelings of disgust were among the apparent drivers for behavior change. Schools offer a unique opportunity to communicate messages regularly with students and so has the potential for sustainability.46,47
Follow-up assessment at 14-months.
The markedly improved cough etiquette behaviors observed at 30 days were not sustained. Coughing and sneezing into upper sleeves declining from 39% to 6%, although 6% was still somewhat more common than at baseline (0%). Coughing and sneezing into the open air was 67%, which was higher than the 47% observed at 1 month after intervention, but still marked an improvement from baseline practices (92%).
We did not design the study from the outset to assess sustained behavior change. Nevertheless, the falloff in cough etiquette practices suggests that habits had not fully formed (Table 5). Habit formation develops through cues and repetition.48–50 The intervention exposure time was short; longer exposure may have led to more common sustained practices and longer-term habit adoption; thus, the lack of practice was an important barrier. Although the intervention encouraged teachers to continue weekly session using the behavior change communication materials, the teachers reported that after 6 months of inclusion in classroom instruction, they no longer emphasized cough etiquette behaviors as they felt students already understood the recommendations. For approximately 8 months there was no behavior change promotion for coughing and sneezing into upper sleeves. This break in promotion may have interrupted the process of habit adoption. Previous habits of coughing and sneezing into the open air or hands likely created barriers to change and to adopting the new behavior of using upper sleeves.48 In addition, the lack of practice among family or community members also interrupted the process of habit adoption for the school children to remember, practice, and become habituated with this comparatively new recommendation.
Table 5.
Theory-of-Change model of the cough etiquette intervention in urban Dhaka and rural Mymensingh, Bangladesh, 2011–2013
| Activities | Target | Outputs | Short-term outcomes | Long-term outcomes |
|---|---|---|---|---|
| Formative study to develop cough etiquette intervention | Children demonstrated high self-efficacy to practice coughing and sneezing into upper sleeves | Cough etiquette practices increased by 39% | ||
| Provision of behavior change communication materials (pictorial flipcharts) and placement cue cards at school grounds | School children received (and understand) intervention messages | Cue cards worked as reminder and call for action to practice cough etiquette | Increased level of changes in cough etiquette knowledge and attitudes | |
| Training of teachers to deliver cough etiquette behavior change communication sessions | Teachers played vital role to encourage, monitor, and promote regular cough etiquette practices and worked as agents to disseminate skills and knowledge | Children reflected social norms with regard to feelings of disgust when coughing or sneezing in open air | Habit formation did not sustain because of short time intervention exposure, lack of practice, and cessation of weekly cough etiquette sessions | |
| Weekly cough etiquette sessions | Availability of trained cough etiquette resource teachers and behavior change communication session delivery personnel in schools | Teachers conducted weekly sessions | ||
| Formation of school-based hygiene committee to promote and monitor cough etiquette practices | Hygiene committee members supported habit adoption | Teachers acted as role models, and children worked as agents for cough etiquette behavior change at home and community |
Future interventions might include a range of new activities incorporated into a schedule to ensure variability to engage student and teacher interest beyond 6 months. The intervention encouraged students to practice a previously unknown and unobserved behavior17,30; that two-thirds of the students did not continue to practice suggests they would need longer duration and repeated message delivery. Students described sneezing and coughing into the upper sleeve as a fun behavior. Compared with affecting all decision-makers in the home environment, schools offer substantial environmental control for behavior change because of the opportunities to positively impact peer pressure with teachers’ influence and leadership to create and manage changes. Therefore, a progressive next step would be to iteratively develop interventions to create a supportive school environment to promote longer-term habit adoption.22
Additional strategies, such as integration of cough etiquette information in the science and health curriculum, promoting cough etiquette as entertaining and fun, and including questions on cough etiquette practices during school hygiene examinations, may also support sustained habit adoption. Future research can explore the potential of using low-cost microscopes in teaching germ theory.51 Teachers might also place signs in each classroom showing someone coughing and sneezing into their upper sleeve with a message that describes this behavior as a rule. Teachers could introduce and explain the sign at the beginning of the school year and refer to it periodically to promote the behavior, especially during winter when colds and coughs are more common. Teachers are in a position of authority to act as community role models and can influence behavior change. Activities, such as singing motivational songs at daily school assemblies reminding students of hygiene practices, have the potential to create a new social norm of coughing and sneezing into upper sleeves to maintain a habit that could spill over to home and community to reduce the transmission of respiratory pathogens. Establishing school rules of coughing and sneezing into upper sleeves during the daily assembly, including handwashing practices after coughing and sneezing as a key time in other handwashing programs and effective message delivery with key motivations of disgust, social acceptance, and peer pressure, can bring sustained behavior change.
Similar to Seimetz et al.,36 systematic analysis of our findings using the IBM-WASH model indicated that contextual and psychosocial factors are important to improve intervention design, and schools can address 1) a supportive context (by the formation of hygiene committees that contributed to continued intervention activities and habit adoption); and 2) Psychosocial factors at both the individual level (perceived benefits, self-efficacy, and behavioral cues or nudges) and also the community level (social norms).35
The presence of fieldworkers to evaluate the students may have altered their behavior during the pilot testing period and thus exaggerated the impact of the intervention. Nevertheless, structured observation is a more valid method in assessing hygiene practices than using questionnaires for self-reported behaviors.41,52 Although we piloted the interventions in only a few schools, the overall environment of the study schools was similar to other schools in Bangladesh. All students would likely underestimate the impact because the grade one students did not receive the intervention; however, when prevalence of coughing and sneezing into the upper sleeve was calculated for only grade 5 children who were exposed to the intervention in the previous year, practices were no better (data not shown).
Research on promotion of cough etiquette is limited.16 The 2009 influenza pandemic caused an estimated 200,000 deaths from respiratory disease globally; 51% of the deaths occurred in southeast Asia and Africa suggesting efforts to prevent influenza need to effectively target these regions in future pandemics. Crowded schools in low- and middle-income countries amplify the risk of disease spread. Public health agencies, including centers for disease control and prevention (CDC), World Health Organization (WHO), and the Committee on Infectious Diseases of the American Academy of Pediatrics (CIDAAP) recommend cough etiquette practices to reduce the risk of transmission17,53,54 and have made explicit calls for additional research on effectiveness of such interventions.55 Schools are both high-risk sites for infectious disease transmission and ideal places to adopt habits that have the potential to impact public health.16 Childhood is a good time to develop habits that are practiced throughout life as children are receptive to new ideas.25,33,49,56–58 Therefore, school settings have the potential to provide an opportunity for encouraging hygiene-related behavior change at a large scale and can put in place key elements necessary for formation of long-term habits.
Improved cough etiquette practices among school children could decrease transmission of respiratory pathogens,18 improve school attendance, and reduce transmission to family members at home. The recommended practice of coughing and sneezing into the upper sleeve was feasible and acceptable, although further research should focus on identifying strategies for sustaining the habit.18 Integrating cough etiquette behaviors into school text books that address other issues of hygiene might help sustained habit adoption at a very low cost.
Supplementary Material
Acknowledgments:
We are grateful for icddr,b’s Environmental Interventions Unit, Training Support Group, and acknowledge Meghan Scott for her thoughtful guidance on the scientific writing, Carrie Read for her review of the high-level outline, Kishor Kumar Das for quantitative data analysis, and Probir Kumar Gosh for his statistical support. We also acknowledge our fieldworkers, study participants, the school communities, and Mahfuzul Islam, Deputy Director from the Directorate of Primary Education for their support throughout the study period. icddr,b is thankful to the Governments of Australia, Bangladesh, Canada, Sweden, and the United Kingdom for providing core/unrestricted support.
Note: Supplemental tables appear at www.ajtmh.org.
Disclaimer: The opinions expressed by the authors do not necessarily reflect the opinions of the Centers for Disease Control and Prevention (CDC), the U.S. Agency for International Development (USAID), or the U.S. Government.
REFERENCES
- 1.Stebbins S, Downs JS, Vukotich CJ, Jr, 2009. Using nonpharmaceutical interventions to prevent influenza transmission in elementary school children: parent and teacher perspectives. J Public Health Manag Pract 15: 112–117. [DOI] [PubMed] [Google Scholar]
- 2.Neuzil KM, Hohlbein C, Zhu Y, 2002. Illness among schoolchildren during influenza season: effect on school absenteeism, parental absenteeism from work, and secondary illness in families. Arch Pediatr Adolesc Med 156: 986–991. [DOI] [PubMed] [Google Scholar]
- 3.Xue Y, Kristiansen I, de Blasio B, 2012. Dynamic modelling of costs and health consequences of school closure during an inflienza pandemic. BMC Public Health 12: 962 (1–17). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization , 2009. Water, Sanitation and Hygiene Standards for Schools in Low-Cost Settings. Adams J, Bartram J, Chartier Y, Sims J, eds. Geneva, Switzerland: WHO Press. [Google Scholar]
- 5.Haque F, et al. 2016. Influenza B virus outbreak at a religious residential school for boys in northern Bangladesh, 2011. Influenza Other Respi Viruses 11: 165–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma R, Joshi P, Tiwari K, Katyal R, Gill KS, 2005. Outbreak of dengue in national capital territory of Delhi, India during 2003. J Vector Ecol 30: 337–338. [PubMed] [Google Scholar]
- 7.Gurav YK, Pawar SD, Chadha MS, Potdar VA, Deshpande AS, Koratkar SS, Hosmani AH, Mishra AC, 2010. Pandemic influenza A (H1N1) 2009 outbreak in a residential school at Panchgani, Maharashtra, India. Indian J Med Res 132: 67–71. [PubMed] [Google Scholar]
- 8.Singh KP, Jain P, Prakash O, Khan DN, Gupta S, Prakash S, Singh DD, Jain A, 2014. Outbreaks of measles and chickenpox in eastern Uttar Pradesh, India. Clin Epidemiol Glob Health 2: 3–9. [Google Scholar]
- 9.Dumre SP, Sapkota K, Adhikari N, Acharya D, Karki M, Bista S, Basanyat SR, Joshi SK, 2009. Asymptomatic throat carriage rate and antimicrobial resistance pattern of Streptococcus pyogenes in Nepalese school children. Kathmandu Univ Med J 7: 392–396 (KUMJ). [DOI] [PubMed] [Google Scholar]
- 10.Lessler J, Reich NG, Cummings DA, 2009. Outbreak of 2009 pandemic influenza A (H1N1) at a New York city school. N Engl J Med 361: 2628–2636. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control Prevention , 2009. Performance of rapid influenza diagnostic tests during two school outbreaks of 2009 pandemic influenza A (H1N1) virus infection-Connecticut, 2009. MMWR Morb Mortal Wkly Rep 58: 1029–1032. [PubMed] [Google Scholar]
- 12.Zhao H, Joseph C, Phin N, 2007. Outbreaks of influenza and influenza-like illness in schools in England and Wales, 2005/06. Euro Surveill 12: E3–E4. [DOI] [PubMed] [Google Scholar]
- 13.Jackson C, Vynnycky E, Hawker J, Olowokure B, Mangtani P, 2013. School closures and influenza: systematic review of epidemiological studies. BMJ Open 3: e002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salathé M, Kazandjieva M, Lee JW, Levis P, Feldman MW, Jones JH, 2010. A high-resolution human contact network for infectious disease transmission. Proc Natl Acad Sci USA 107: 22020–22025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cauchemez S, Bhattarai A, Marchbanks TL, Fagan RP, Ostroff S, Ferguson NM, Swerdlow D, Sodha SV, Moll ME, Angulo FJ, 2011. Role of social networks in shaping disease transmission during a community outbreak of 2009 H1N1 pandemic influenza. Proc Natl Acad Sci USA 108: 2825–2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barry T, Manning S, Lee MS, Eggleton R, Hampton S, Kaur J, Baker MG, Wilson N, 2011. Respiratory hygiene practices by the public during the 2009 influenza pandemic: an observational study. Influenza Other Respi Viruses 5: 317–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nasreen S, Azziz‐Baumgartner E, Gurley E, Winch P, Unicomb L, Sharker M, Southern D, Luby S, 2010. Prevalent high‐risk respiratory hygiene practices in urban and rural Bangladesh. Trop Med Int Health 15: 762–771. [DOI] [PubMed] [Google Scholar]
- 18.Berry TD, Fournier AK, 2014. Examining university students’ sneezing and coughing etiquette. Am J Infect Control 42: 1317–1318. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention , 2013. Respiratory Hygiene/Cough Etiquette in Healthcare Settings Available at: http://www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm. Accessed October 13, 2013.
- 20.Freeman MC, Greene LE, Dreibelbis R, Saboori S, Muga R, Brumback B, Rheingans R, 2012. Assessing the impact of a school‐based water treatment, hygiene and sanitation programme on pupil absence in Nyanza province, Kenya: a cluster‐randomized trial. Trop Med Int Health 17: 380–391. [DOI] [PubMed] [Google Scholar]
- 21.Ejemot RI, Ehiri JE, Meremikwu MM, Critchley JA, 2008. Hand washing for preventing diarrhoea. Cochrane Database Syst Rev, Cd004265. [DOI] [PubMed] [Google Scholar]
- 22.Lopez-Quintero C, Freeman P, Neumark Y, 2009. Hand washing among school children in Bogotá, Colombia. Am J Public Health 99: 94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waddington H, Snilstveit B, White H, Fewtrell L, 2009. Water, Sanitation and Hygiene Interventions to Combat Childhood Diarrhoea in Developing Countries. Delhi, India: International Initiative for Impact Evaluation. [Google Scholar]
- 24.Rabie T, Curtis V, 2006. Handwashing and risk of respiratory infections: a quantitative systematic review. Trop Med Int Health 11: 258–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bowen A, Ma H, Ou J, Billhimer W, Long T, Mintz E, Hoekstra RM, Luby S, 2007. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Am J Trop Med Hyg 76: 1166–1173. [PubMed] [Google Scholar]
- 26.Master D, Hess Longe SH, Dickson H, 1997. Scheduled hand washing in an elementary school population. Fam Med 29: 336–339. [PubMed] [Google Scholar]
- 27.Nicholson JA, Naeeni M, Hoptroff M, Matheson JR, Roberts AJ, Taylor D, Sidibe M, Weir AJ, Damle SG, Wright RL, 2014. An investigation of the effects of a hand washing intervention on health outcomes and school absence using a randomised trial in Indian urban communities. Trop Med Int Health 19: 284–292. [DOI] [PubMed] [Google Scholar]
- 28.Talaat M, Afifi S, Dueger E, El-Ashry N, Marfin A, Kandeel A, Mohareb E, El-Sayed N, 2011. Effects of hand hygiene campaigns on incidence of laboratory-confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerg Infect Dis 17: 619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization , 2008. World Health Statistics 2008 Geneva, Switzerland: World Health Organization Press, 1–110. [Google Scholar]
- 30.Nizame FA, Nasreen S, Unicomb L, Southern D, Gurley ES, Arman S, Kadir MA, Azziz-Baumgartner E, Luby SP, Winch PJ, 2011. Understanding community perceptions, social norms and current practice related to respiratory infection in Bangladesh during 2009: a qualitative formative study. BMC Public Health 11: 901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tellier R, 2006. Review of aerosol transmission of influenza A virus. Emerg Infect Dis 12: 1657–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blanton E, Ombeki S, Oluoch GO, Mwaki A, Wannemuehler K, Quick R, 2010. Evaluation of the role of school children in the promotion of point-of-use water treatment and handwashing in schools and households—Nyanza province, western Kenya, 2007. Am J Trop Med Hyg 82: 664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Onyango-Ouma W, Aagaard-Hansen J, Jensen B, 2005. The potential of schoolchildren as health change agents in rural western Kenya. Soc Sci Med 61: 1711–1722. [DOI] [PubMed] [Google Scholar]
- 34.O’reilly C, Freeman M, Ravani M, Migele J, Mwaki A, Ayalo M, Ombeki S, Hoekstra R, Quick R, 2008. The impact of a school-based safe water and hygiene programme on knowledge and practices of students and their parents: Nyanza province, western Kenya, 2006. Epidemiol Infect 136: 80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dreibelbis R, Winch PJ, Leontsini E, Hulland KR, Ram PK, Unicomb L, Luby SP, 2013. The integrated behavioural model for water, sanitation, and hygiene: a systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure-restricted settings. BMC public health 13: 1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seimetz E, Boyayo A-M, Mosler H-J, 2016. The influence of contextual and psychosocial factors on handwashing. Am J Trop Med Hyg 94: 1407–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hulland KR, Leontsini E, Dreibelbis R, Unicomb L, Afroz A, Dutta NC, Nizame FA, Luby SP, Ram PK, Winch PJ, 2013. Designing a handwashing station for infrastructure-restricted communities in Bangladesh using the integrated behavioural model for water, sanitation and hygiene interventions (IBM-WASH). BMC Public Health 13: 877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Najnin N, Arman S, Abedin J, Unicomb L, Levine DI, Mahmud M, Leder K, Yeasmin F, Luoto JE, Albert J, 2015. Explaining low rates of sustained use of siphon water filter: evidence from follow‐up of a randomised controlled trial in Bangladesh. Trop Med Int Health 20: 471–483. [DOI] [PubMed] [Google Scholar]
- 39.Bresee S, Caruso BA, Sales J, Lupele J, Freeman MC, 2016. ‘A child is also a teacher’: exploring the potential for children as change agents in the context of a school-based WASH intervention in rural eastern Zambia. Health Educ Res 31: 521–534. [DOI] [PubMed] [Google Scholar]
- 40.Cialdini RB, Reno RR, Kallgren CA, 1990. A focus theory of normative conduct: recycling the concept of norms to reduce littering in public places. J Pers Soc Psychol 58: 1015–1026. [Google Scholar]
- 41.Biran A, Rabie T, Schmidt W, Juvekar S, Hirve S, Curtis V, 2008. Comparing the performance of indicators of hand-washing practices in rural Indian households. Trop Med Int Health 13: 278–285. [DOI] [PubMed] [Google Scholar]
- 42.Cairncross S, Shordt K, Zacharia S, Govindan BK, 2005. What causes sustainable changes in hygiene behaviour? A cross-sectional study from Kerala, India. Soc Sci Med 61: 2212–2220. [DOI] [PubMed] [Google Scholar]
- 43.Damerell P, Howe C, Milner-Gulland EJ, 2013. Child-orientated environmental education influences adult knowledge and household behaviour. Environ Res Lett 8: 015016. [Google Scholar]
- 44.Jenkins RL, 1979. The influence of children in family decision-making: parents’ perceptions. Adv Consum Res 6: 413–418. [Google Scholar]
- 45.Han SS, Weiss B, 2005. Sustainability of teacher implementation of school-based mental health programs. J Abnorm Child Psychol 33: 665–679. [DOI] [PubMed] [Google Scholar]
- 46.Petersen PE, Hunsrisakhun J, Thearmontree A, Pithpornchaiyakul S, Hintao J, Jürgensen N, Ellwood R, 2015. School-based intervention for improving the oral health of children in southern Thailand. Community Dent Health 32: 44–50. [PubMed] [Google Scholar]
- 47.Barry MM, Clarke AM, Jenkins R, Patel V, 2013. A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC Public Health 13: 835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verplanken B, 2006. Beyond frequency: habit as mental construct. Br J Soc Psychol 45: 639–656. [DOI] [PubMed] [Google Scholar]
- 49.Wood W, Neal DT, 2007. A new look at habits and the habit-goal interface. Psychoanal Rev 114: 843–863. [DOI] [PubMed] [Google Scholar]
- 50.Wood W, Tam L, Witt MG, 2005. Changing circumstances, disrupting habits. J Pers Soc Psychol 88: 918–933. [DOI] [PubMed] [Google Scholar]
- 51.Cybulski JS, Clements J, Prakash M, 2014. Foldscope: origami-based paper microscope. PLoS One 9: e98781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Biran A, et al. 2009. The effect of a soap promotion and hygiene education campaign on handwashing behaviour in rural India: a cluster randomised trial. Trop Med Int Health 14: 1303–1314. [DOI] [PubMed] [Google Scholar]
- 53.Aledort JE, Lurie N, Wasserman J, Bozzette SA, 2007. Non-pharmaceutical public health interventions for pandemic influenza: an evaluation of the evidence base. BMC Public Health 7: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stebbins S, et al. 2011. Reduction in the incidence of influenza A but not influenza B associated with use of hand sanitizer and cough hygiene in schools: a randomized controlled trial. Pediatr Infect Dis J 30: 921–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zayas G, Chiang MC, Wong E, MacDonald F, Lange CF, Senthilselvan A, King M, 2013. Effectiveness of cough etiquette maneuvers in disrupting the chain of transmission of infectious respiratory diseases. BMC Public Health 13: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scott B, Curtis V, Rabie T, Garbrah-Aidoo N, 2007. Health in our hands, but not in our heads: understanding hygiene motivation in Ghana. Health Policy Plan 22: 225–233. [DOI] [PubMed] [Google Scholar]
- 57.Vivas A, Gelaye B, Aboset N, Kumie A, Berhane Y, Williams MA, 2010. Knowledge, attitudes, and practices (KAP) of hygiene among school children in Angolela, Ethiopia. J Prev Med Hyg 51: 73–79. [PMC free article] [PubMed] [Google Scholar]
- 58.Curtis V, Schmidt W, Luby S, Florez R, Touré O, Biran A, 2011. Hygiene: new hopes, new horizons. Lancet Infect Dis 11: 312–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.