Abstract.
The lentil lectin glycoprotein enzyme-linked immunoelectrotransfer blot (LLGP EITB, reported sensitivity 99% and specificity 100%) is used as a serologic marker of exposure to Taenia solium in pigs. However, only a limited number of parasites have been evaluated for cross reactivity. Pigs may host other related cestode infections, including Taenia hydatigena, which have not been formally evaluated for cross-reactions. We investigated a corral in Tumbes, Peru, a region where a cysticercosis elimination demonstration project was completed in 2012. In this corral, 14/19 (73.7%) 6–8-week-old piglets were reactive to GP50 on LLGP EITB, and all had circulating Taenia sp. antigens. From eight necropsied piglets; four were infected with T. hydatigena metacestodes whereas none had evidence of T. solium infection. Two resident dogs were subsequently confirmed to have T. hydatigena taeniasis. These results suggest GP50 cross-reactivity in T. hydatigena-infected pigs, although controlled experimental infection is needed to confirm this hypothesis.
INTRODUCTION
Taenia solium is a zoonotic cestode that causes seizures in humans and agricultural losses due to contaminated pork. Serologic testing for the metacestode stage of the parasite in pigs plays an important role in understanding transmission and in monitoring control interventions.1–6 One commonly used diagnostic assay for this purpose is the lentil lectin glycoprotein enzyme-linked immunoelectrotransfer blot assay (LLGP EITB), which uses a semipurified fraction that contains seven native T. solium glycoprotein antigens (GP50, GP42-39, GP24, GP21, GP18, GP14, and GP13, the number indicating the molecular weight in kDa).7 Reaction to one or more of these diagnostic bands indicates the presence of circulating antibodies resulting from infection with or exposure to T. solium metacestode. The test was initially reported to be 100% specific to T. solium metacestode stage in pigs, although only a small number of sera from pigs with other helminth infections (Ascaris, Trichuris, Trichinella, Echinococcus granulosus, and Fasciola hepatica) have been tested.8 Pigs may host other related cestode infections, including T. hydatigena, which have not been formally evaluated for cross-reactions.
In an ongoing study in Tumbes, Peru, we purchase seronegative piglets from community corrals to use as sentinels in an experiment evaluating environmental egg contamination.9 Tumbes is unique because in 2012, we completed a successful project which eliminated cysticercosis from all 107 rural villages in this region. To ensure that the sentinel pigs have not been exposed to T. solium, we use both LLGP EITB and the monoclonal antibody–based B158/B60 Ag-detection enzyme-linked immunosorbent assay (ELISA) to screen the piglets before purchase.8,10,11 In 2016, we encountered a corral in which 14/19 (73.7%) tested piglets were seropositive on LLGP EITB, all of which were reactive only to the GP50 diagnostic band. All 19 piglets were also positive to the Ag-ELISA suggesting active Taenia sp. metacestode infection. This was in stark contrast with other corrals in the area in which sporadic reactivity to GP50 had been noted, but usually not in association with the presence of circulating antigens. In this manuscript, we describe the result of an investigation to evaluate the potential source of seropositivity in this corral.
MATERIALS AND METHODS
This investigation took place in the district of Zarumilla, Tumbes, Peru. The owners of the land maintain their own pigs in a discrete corral with concrete floors and walls, and rent space for others to build separate corrals to raise pigs and goats. In October 2016, we took a blood sample from all 19 piglets present in the owner’s corral that were between the ages of 6–8 weeks. Pig sera were analyzed by LLGP EITB for the presence of antibodies against T. solium metacestodes and by B158/B60 Ag-ELISA for the presence of Taenia sp. antigens as previously described.8,10
After reviewing the results of the LLGP EITB and Ag-ELISA, we returned to the corral 6 weeks later and offered to purchase all piglets that had been tested. Those purchased were transferred to the animal facilities at the Center for Global Health Tumbes where they were anesthetized using intramuscular ketamine (5 mg/kg)/xylazine (0.1 mg/kg) and then euthanized by intravenous sodium pentobarbital (100 mg/kg). The entire carcass was inspected for the presence of metacestode infection. All skeletal muscle tissue was systematically dissected using fine cuts less than 0.5 cm to detect viable, degenerating, or calcified cysts; organs including heart, liver, lungs, esophagus, and intestines were also examined.
We arranged collection and screening of stool for humans residing near the corral in accordance with the Tumbes Regional Directorate of Health postelimination surveillance guidelines. Whole stool samples were inspected visually for the presence of tapeworm segments or proglottids. Ten milliliter fecal aliquots in phosphate buffered saline 5% formaldehyde were then evaluated by light microscopy for the presence of Taenia sp. eggs before and after concentration, and by ELISA for the detection of coproantigens as previously described.12 Resident dogs were restrained and administered 4 mg/kg of arecoline hydrobromide purgative, with a second dose of 2 mg/kg given if there was no purgative effect after 30 minutes.13 Postpurgative fecal samples were mixed with saline 5% formaldehyde, passed through a sieve, and examined visually for the presence of helminths. Cestodes were preserved in 70% ethanol. We used various morphologic parameters, including characteristics of rostellar hooks, to identify the species of the adult-stage cestodes. For confirmation, we used polymerase chain reaction to amplify a 392-bp fragment of the cytochrome c oxidase subunit 1 gene (cox1) using primers JB3 and JB4.5, then sequenced the PCR products using an ABI 3100 automated sequencer (Applied Biosystems, Foster City, CA).14,15 The genetic identity was determined based on the alignment of the nucleotide sequences of the cox1 gene.16
The protocol was approved by the Institutional Committee for the Ethical Use of Animals at Universidad Peruana Cayetano Heredia and at Universidad Nacional Mayor de San Marcos. Treatment of animals adhered to the Council for International Organizations of Medical Sciences International Guiding Principles for Biomedical Research Involving Animals. Screening of human stool was conducted in accordance with the Tumbes Regional Directorate of Health postelimination guidelines for surveillance of taeniasis and porcine cysticercosis.
RESULTS
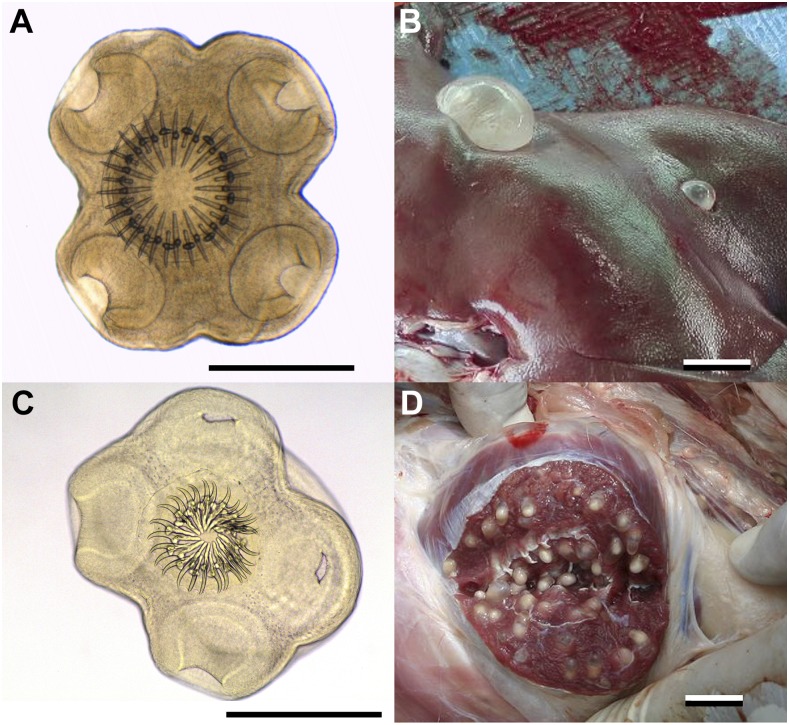
We were able to purchase nine of the original 19 piglets, including seven that were reactive to GP50 and two that were nonreactive to GP50. The other 10 had been sold and were no longer available. One piglet died of presumed viral infection and was not evaluated further. The remaining eight piglets underwent necropsy and none had evidence of T. solium infection (Table 1). However, 4/6 (66.7%) GP50-reactive piglets and 0/2 (0%) GP50-nonreactive piglets were found to be infected with T. hydatigena metacestodes (Figure 1).
Table 1.
Serologic and necropsy results of nine piglets from Zarumilla, Tumbes, Peru
| Pig | LLGP-EITB, number of bands | GP50 | Ag-ELISA | Optical density ratio | Necropsy |
|---|---|---|---|---|---|
| 1 | 0 | Nonreactive | Positive | 49.27 | Normal |
| 2 | 0 | Nonreactive | Positive | 22.78 | Normal |
| 3 | 1 | Reactive | Positive | 2.97 | Normal |
| 4 | 1 | Reactive | Positive | 8.80 | Normal |
| 5 | 1 | Reactive | Positive | 67.80 | Taenia hydatigena |
| 6 | 1 | Reactive | Positive | 67.80 | T. hydatigena |
| 7 | 1 | Reactive | Positive | 66.66 | T. hydatigena |
| 8 | 1 | Reactive | Positive | 64.76 | T. hydatigena |
| 9 | 1 | Reactive | Positive | 15.93 | Not done |
LLGP-EITB = Lentil lectin glycoprotein enzyme-linked immunoelectrotransfer blot.
Figure 1.
(A) Scolex of Taenia hydatigena collected from dog feces. Scale bar = 500 μm. (B) Taenia hydatigena metacestode collected from a GP50-positive pig during necropsy. Scale bar = 2 cm. (C) Scolex of Taenia solium. Scale bar = 500 μm. (D) Taenia solium metacestode in a naturally infected pig. Scale bar = 2 cm. This figure appears in color at www.ajtmh.org.
There were four people who cared for the pigs in the corral; the fecal samples were tested from all four, and none had taeniasis. There were eight resident dogs near the corral. We were able to capture five dogs and two were found to harbor adult-stage T. hydatigena tapeworms, including one with six worms and one with four worms. The scoleces had a globular form 765 to 1,085 μm in diameter and six suckers of 361–370 μm at maximum width. The rostella were 377–408 μm in diameter and had two rows of hooks; large hooks were 193–207 μm in length whereas small hooks were 125–152 μm in length. The nucleotide sequences were more than 99% similar to sequences of T. hydatigena that had been previously published and registered in the GenBank.
DISCUSSION
This investigation suggests that T. hydatigena metacestode infection in pigs can provoke an antibody response against the GP50 diagnostic band on LLGP EITB. Although controlled experimental infection is required for definitive confirmation of this hypothesis, our findings are strongly suggestive of cross-reactivity to this parasite. Taenia hydatigena metacestodes were confirmed in the 4/6 (66.7%) pigs reactive to GP50 whereas T. solium metacestodes were not found. Since the completion of the elimination demonstration project 4 years prior there have not been reports of porcine cysticercosis in this area. In addition, a probable source of exposure to T. hydatigena eggs was confirmed in two dogs that lived nearby the corral and were infected with T. hydatigena taenaiasis. On the contrary, no T. solium taeniasis was found among nearby humans.
The LLGP EITB assay in pigs is often used in epidemiologic studies to identify regions where T. solium transmission occurs and in trials to monitor the progress of control interventions.1–6 Seropositivity has also been used to select pigs with increased likelihood of detecting viable T. solium cyst infection for necropsy.9 The high reported specificity of the LLGP EITB in pigs has been viewed as an advantage over the use of antigen detection assays as these are known to cross-react with the metacestode stage of other Taenia sp. that infect pigs.17,18 This is particularly important for T. hydatigena which is frequently coendemic to T. solium and often more prevalent.19 It is important to note that in this investigation, there was no evidence of cross-reaction to any of the other diagnostic glycoprotein antigens. However, until the specificity of the different glycoprotein antigens used in LLGP EITB can be verified, the results of the LLGP EITB in pigs should be interpreted with caution. It is important to note that although necropsy is the gold standard, it is possible that small cysts may escape detection, which could explain the lack of cysts in four pigs that were positive to Ag-ELISA. Finally, it is also important to stress that T. hydatigena is not known to infect humans, so these findings cannot be generalized to the interpretation of the LLGP EITB in the diagnosis of human neurocysticercosis.
REFERENCES
- 1.Gonzalez AE, Gilman R, Garcia HH, McDonald J, Kacena K, Tsang VC, Pilcher JB, Suarez F, Gavidia C, Miranda E, 1994. Use of sentinel pigs to monitor environmental Taenia solium contamination. The Cysticercosis Working Group in Peru (CWG). Am J Trop Med Hyg 51: 847–850. [DOI] [PubMed] [Google Scholar]
- 2.García HH, et al. Cysticercosis Working Group in Perú, 2003. Hyperendemic human and porcine Taenia solium infection in Perú. Am J Trop Med Hyg 68: 268–275. [PubMed] [Google Scholar]
- 3.O’Neal SE, Moyano LM, Ayvar V, Rodriguez S, Gavidia C, Wilkins PP, Gilman RH, Garcia HH, Gonzalez AE; Cysticercosis Working Group in Peru, 2014. Ring-screening to control endemic transmission of Taenia solium. PLoS Negl Trop Dis 8: e3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gavidia CM, Verastegui MR, Garcia HH, Lopez-Urbina T, Tsang VC, Pan W, Gilman RH, Gonzalez AE; Cysticercosis Working Group in Peru, 2013. Relationship between serum antibodies and Taenia solium larvae burden in pigs raised in field conditions. PLoS Negl Trop Dis 7: e2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohan VR, Tharmalingam J, Muliyil J, Oommen A, Dorny P, Vercruysse J, Vedantam R, 2013. Prevalence of porcine cysticercosis in Vellore, South India. Trans R Soc Trop Med Hyg 107: 62–64. [DOI] [PubMed] [Google Scholar]
- 6.Sikasunge CS, Phiri IK, Phiri AM, Siziya S, Dorny P, Willingham AL., 3rd, 2008. Prevalence of Taenia solium porcine cysticercosis in the eastern, southern and western provinces of Zambia. Vet J 176: 240–244. [DOI] [PubMed] [Google Scholar]
- 7.Tsang VC, Brand JA, Boyer AE, 1989. An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium). J Infect Dis 159: 50–59. [DOI] [PubMed] [Google Scholar]
- 8.Tsang VC, Pilcher JA, Zhou W, Boyer AE, Kamango-Sollo EI, Rhoads ML, Murrell KD, Schantz PM, Gilman RH, 1991. Efficacy of the immunoblot assay for cysticercosis in pigs and modulated expression of distinct IgM/IgG activities to Taenia solium antigens in experimental infections. Vet Immunol Immunopathol 29: 69–78. [DOI] [PubMed] [Google Scholar]
- 9.Garcia HH, et al. 2016. Elimination of Taenia solium transmission in northern Peru. N Engl J Med 374: 2335–2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brandt JR, Geerts S, De Deken R, Kumar V, Ceulemans F, Brijs L, Falla N, 1992. A monoclonal antibody-based ELISA for the detection of circulating excretory-secretory antigens in Taenia saginata cysticercosis. Int J Parasitol 22: 471–477. [DOI] [PubMed] [Google Scholar]
- 11.Nguekam A, Zoli AP, Vondou L, Pouedet SM, Assana E, Dorny P, Brandt J, Losson B, Geerts S, 2003. Kinetics of circulating antigens in pigs experimentally infected with Taenia solium eggs. Vet Parasitol 111: 323–332. [DOI] [PubMed] [Google Scholar]
- 12.Guezala MC, Rodriguez S, Zamora H, Garcia HH, Gonzalez AE, Tembo A, Allan JC, Craig PS, 2013. Development of a species-specific coproantigen ELISA for human Taenia solium taeniasis. Am J Trop Med Hyg 81: 433–437. [PubMed] [Google Scholar]
- 13.Gemmell MA, 1973. Surveillance of Echinococcus granulosus in dogs with arecoline hydrobromide. Bull World Health Organ 48: 649–652. [PMC free article] [PubMed] [Google Scholar]
- 14.Liu GH, Lin RQ, Li MW, Liu W, Liu Y, Yuan ZG, Song HQ, Zhao GH, Zhang KX, Zhu XQ, 2011. The complete mitochondrial genomes of three cestode species of Taenia infecting animals and humans. Mol Biol Rep 38: 2249–2256. [DOI] [PubMed] [Google Scholar]
- 15.Bowles J, McManus DP, 1994. Genetic characterization of the Asian Taenia, a newly described taeniid cestode of humans. Am J Trop Med Hyg 50: 33–44. [PubMed] [Google Scholar]
- 16.Zhan G, Chen J, Yang Y, Liu N, Jiang W, Gu S, Wang X, Wang Z, 2014. Utility of DNA barcoding in distinguishing species of the family Taeniidae. J Parasitol 100: 542–546. [DOI] [PubMed] [Google Scholar]
- 17.Dorny P, Phiri IK, Vercruysse J, Gabriel S, Willingham AL, 3rd, Brandt J, Victor B, Speybroeck N, Berkvens D, 2004. A Bayesian approach for estimating values for prevalence and diagnostic test characteristics of porcine cysticercosis. Int J Parasitol 34: 569–576. [DOI] [PubMed] [Google Scholar]
- 18.Cheng RWK, Ko R, 1991. Cross-reactions between crude antigens of larval Taenia solium (Cysticercus cellulosae) and other helminths of pigs. Vet Parasitol 39: 161–170. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen MT, Gabriël S, Abatih EN, Dorny P, 2016. A systematic review on the global occurrence of Taenia hydatigena in pigs and cattle. Vet Parasitol 226: 97–103. [DOI] [PubMed] [Google Scholar]