Abstract
Aims
Although the number of hospitals performing cardiac surgery has increased rapidly in China, information regarding the trends in coronary artery bypass grafting (CABG) outcomes remains unknown.
Methods and results
We used data from the Chinese Cardiac Surgery Registry, the largest registry system that accounts for nearly 50% of total annual CABG volume in China, to assess trends of in-hospital mortality and major complication rates for patients receiving isolated CABG in 102 urban teaching hospitals in China from 25 January 2004 through 31 December 2013 (except 2006 and 2009). Using a mixed effects model, we estimated annual trends in each of these two outcomes overall and by age groups (18–64 and 65 years or older), adjusted for patient characteristics. We also assessed the trends in pre-operative, post-operative, and total length of stay (LOS). The study included 40 652 patients across 102 hospitals. Between 2004 and 2013, patients' mean age decreased from 62.7 to 61.4 years, in-hospital mortality decreased from 2.8% to 1.6% (difference, 1.3%, 95% CI: 0.70–1.85), and major complication rates decreased from 7.8% to 3.8% (difference, 4.0%; 95% CI: 3.05–4.90). The reduction in mortality and major complication rates were consistent across age groups. Between 2004 and 2013, the median (inter-quartile range) pre-operative LOS remained unchanged, post-operative LOS declined from 12.0 (8.0) to 10.0 (7.0) days, and total LOS declined from 22.0 (13.0) to 20.0 (12.0) days.
Conclusion
Isolated CABG-related in-hospital mortality, major complication rates, and LOS have improved in urban teaching hospitals in China over the last decade.
Keywords: Quality and outcomes of care, Coronary artery bypass graft
Introduction
Coronary artery disease (CAD) has become one of the most prevalent diseases in China. From 1980 to 2011, the number of CAD related hospitalizations increased by 11.6% annually, ranking second after stroke in terms of growth rate.1 Between 1985 and 2010, CAD-related mortality increased from 24.2 to 86.3 per 100 000 person-years,1,2 and in 2012, there were approximately 4.5 million CAD-related hospitalizations.3 During the same period, cardiac surgery developed rapidly in China; the number of cardiac surgery centres increased from fewer than 500 in 2003 to approximately 750 in 2013.4 Coronary artery bypass grafting (CABG) was carried out in more than 55% of those centres and more than 40 centres had an annual CABG volume of over 100. Overall, isolated CABG procedures were carried out in approximately 28 000 Chinese adults in 2012.4,5
With the rapid increase in CABG volume in China, national efforts have been initiated to monitor and improve the care and outcomes of CABG. Patients, healthcare providers, insurance companies, and the government are increasingly interested in the results achieved and whether there are changes over time.1,6,7 Previous studies on CABG outcomes in China were cross-sectional and limited to single institutions or regions,5,6 which are important, however they have not shown trends of outcomes at the national level. Information from a diverse group of institutions regarding the temporal changes in CABG outcomes, including mortality, post-operative major complications, and length of stay (LOS), remains unknown. As the CAD population continually increases in China, it is important to identify gaps in CABG outcomes to inform future healthcare planning to enhance the future care of the CAD population in China. Additionally, identifying a reduction of outcomes provides the opportunity to learn what processes may be responsible for the success.
Accordingly, we used data from the Chinese Cardiac Surgery Registry,8,9 the largest multi-hospital CABG registry in China, to evaluate isolated CABG outcomes and to assess trends of CABG outcomes through investigation of in-hospital mortality, major complication rates, and LOS for a large sample of urban and teaching hospitals in which CABG surgery is carried out.9
Methods
Study sample
The Chinese Cardiac Surgery Registry recruited hospitals on a voluntary basis. All the hospitals are located in urban areas and are designated by the Chinese government as tertiary hospitals. All of them are teaching hospitals as defined by being associated with a medical school and being engaged in training doctors. Participating hospitals received detailed information on data collection requirements and definitions of variables. Specifically, they used a Standardized Case Report Form to collect patient information, including demographics, pre-operative risk factors, operative information, post-operative treatment course, and surgical outcomes. All the data were collected by trained clinical research staff and were subsequently double-entered into databases. Data quality measures have been reported elsewhere.8 Demographics, clinical characteristics, and in-hospital events following cardiac surgery, were complete for all patients involved in the study. All patients signed informed consent forms when they were admitted for CABG. The study sample was restricted to patients who were aged 18 years or older and underwent an isolated CABG from 1 January 2004 through 31 December 2013 (except 2006 and 2009 in which no data were collected) across 102 hospitals. Some hospitals were not repeated in every year. Patients receiving other surgeries (e.g. valve surgery, aortic surgery, ventricular aneurysm repair) with CABG were also excluded from the study.
Patient characteristics and outcomes
Patient characteristics included age, gender, body mass index (BMI), smoking status, diabetes, hypertension, hyperlipidaemia, renal failure, history of acute myocardial infarction (AMI), peripheral vessel diseases, and history of CABG. We divided patients into two age groups: 18–64 years of age and 65 years or older to compare with younger and older patients.
The outcomes were in-hospital total post-operative mortality, in-hospital 7-day post-operative mortality, in-hospital post-operative major complication, and LOS. In-hospital post-operative mortality was defined as any death during the hospitalization after CABG, and in-hospital 7-day post-operative mortality was defined as any death within 7 days during the hospitalization after CABG. A major complication was defined as the occurrence of any of the following major post-operative events: death, reoperation for bleeding, stroke, re-intubation, AMI, and renal failure (see Supplementary material online, Table S1). For LOS, we assessed the changes in pre-operative LOS (Pre-LOS), defined as the difference in dates between operation and admission; post-operative length of stay (Post-LOS), defined as the difference in dates between discharge and operation; and total LOS, defined as the difference in dates between discharge and admission; if the date of operation was the same as the date of admission, Pre-LOS was counted as 0; if the date of discharge was the same as the date of operation, Post-LOS was counted as 0.
Statistical analysis
To facilitate data presentation, we reported patient characteristics and observed outcomes in 2-year interval periods: 2004–2005, 2007–2008, 2010–2011, and 2012–2013. We examined patient demographics, clinical characteristics, and outcomes across these four biannual intervals. Rates of in-hospital mortality and in-hospital major complications were expressed as percentages and LOS as a median (interquartile range [IQR]). We used the Cochran–Armitage trend test to determine the statistical significance of changes in outcomes over time. We fitted a mixed effects model with a logit link function and hospital-specific random intercepts, adjusting for patient characteristics, to evaluate the trend in mortality rates. We included an ordinal time variable, corresponding to each year of the study period, after the visual inspection of crude rates revealed a linear pattern in the model, in which the odds ratio of this variable represents the annual change in mortality rates. We fitted the same model to evaluate the trend in major complications as well. We repeated each model for the two age subgroups (18–64 and 65 years or older) to assess whether the trends were consistent among both younger and older patient groups. We quantified the variation in outcomes over time by calculating the population-weighted quartile coefficient of dispersion. Decreases in the dispersion imply less heterogeneity in hospital-specific outcomes.
To address the possibility of different hospitals being included over time, we conducted a sensitivity analysis by identifying hospitals that were in each of the four bi-interval periods (2004–2005, 2007–2008, 2010–2011, and 2012–2013). These hospitals accounted for 66.7% of total patients in the sample. We then fitted the mixed models based on this subset of patients, who underwent a CABG procedure from hospitals that were repeated in the whole study period. All statistical testing was two-sided at a significance level of 0.05 and all analyses were conducted with SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Study sample
The final study sample included a total of 40 652 consecutive patients who underwent an isolated CABG surgery across 102 hospitals from 2004 to 2013, except 2006 and 2009 (see Supplementary material online, Table S2). The mean age of patients was 62.2 ± 9.4 years, 22.4% were females, and 34.6% patients had an on-pump CABG surgery. Patient characteristics varied slightly by measure periods (Table 1). Between 2004–2005 and 2012–2013, the patients' age decreased slightly from 62.7 to 61.4 years, and the percentage of patients with a history of MI also decreased, while the proportions of patients with high BMI, and active smoking habits increased (Table 1).
Table 1.
Pre-operative characteristics and outcomes
| Measure | Overall (n = 40 652) | 2004–2005 (n = 8082) | 2007–2008 (n = 8739) | 2010–2011 (n = 10 046) | 2012–2013 (n = 13 785) | P-value |
|---|---|---|---|---|---|---|
| Patient characteristics | ||||||
| Age, mean (SD), years | 62.2 ± 9.4 | 62.7 ± 9.2 | 62.2 ± 9.2 | 62.0 ± 9.2 | 61.4 ± 8.8 | <0.001 |
| Age group | <0.001 | |||||
| 18–64 years old (%) | 60.7 | 55.4 | 58.1 | 61.3 | 65.1 | |
| 65 years or older (%) | 39.3 | 44.6 | 41.9 | 38.7 | 34.9 | |
| Female (%) | 22.4 | 20.9 | 21.6 | 23.6 | 23.1 | <0.001 |
| BMI, Mean (SD), kg/m2 | 25.1 ± 3.7 | 25.1 ± 2.9 | 25.2 ± 2.8 | 25.3 ± 3.2 | 25.6 ± 10.5 | 0.701 |
| Current smoker (%) | 58.0 | 48.0 | 49.0 | 51.8 | 57.9 | <0.001 |
| Diabetes (%) | 29.2 | 28.2 | 31.3 | 31.6 | 26.9 | 0.003 |
| Hypertension (%) | 59.8 | 65.3 | 65.8 | 62.9 | 51.2 | <0.001 |
| Hyperlipidaemia (%) | 62.0 | 55.9 | 64.3 | 61.4 | 62.7 | <0.001 |
| Renal failure (%) | 0.7 | 0.7 | 1.1 | 0.5 | 0.5 | <0.001 |
| History of MI (%) | 35.5 | 44.4 | 40.5 | 38.0 | 37.2 | 0.01 |
| PVD (%) | 2.3 | 2.5 | 1.3 | 3.3 | 2.2 | <0.001 |
| Previous CABG (%) | 0.4 | 0.4 | 0.2 | 0.4 | 0.6 | 0.0042 |
| Post-operative outcomes | ||||||
| In-hospital mortality (%) | 1.77 | 2.66 | 2.15 | 1.15 | 1.44 | <0.001 |
| Myocardial infarction (%) | 0.4 | 0.5 | 0.4 | 0.4 | 0.4 | 0.2168 |
| Reoperation for bleeding (%) | 2.25 | 3.56 | 2.9 | 2.27 | 1.06 | <0.001 |
| Stroke (%) | 0.44 | 0.46 | 0.39 | 0.56 | 0.38 | 0.6402 |
| Reintubation (%) | 0.35 | 0.37 | 0.65 | 0.54 | <0.01 | <0.001 |
| Renal failure (%) | 1.87 | 2.26 | 3.28 | 1.21 | 1.21 | <0.001 |
| One or more above events (%) | 5.47 | 7.32 | 7.32 | 4.95 | 3.58 | <0.001 |
| Median length of stay, (interquartile range [IQR]) days | ||||||
| Pre-operative stay | 9.0 (8.0) | 9.0 (9.0) | 10.0 (9.0) | 8.0 (8.0) | 9.0 (8.0) | 0.0601 |
| Post-operative stay | 10.0 (7.0) | 12.0 (8.0) | 11.0 (7.0) | 9.0 (6.0) | 9.0 (6.0) | <0.001 |
| Total stay | 20.0 (13.0) | 22.0 (14.0) | 22.0 (14.0) | 19.0 (11.0) | 19.0 (12.0) | <0.001 |
All of the 102 hospitals were teaching hospitals, 11.8% were CVD-specific hospitals, and 11.8% were military hospitals that treated non-military patients (see Supplementary material online, Table S3). Overall, the Chinese Cardiac Surgery Registry had 32.4% of participating hospitals from Eastern China, 7.8% from Southern China, 16.7% from Western China, 30.4% from Northern China, and 12.7% from Central China (see Supplementary material online, Table S3). Between 2004 and 2013, the number of individual hospitals in the Chinese Cardiac Surgery Registry increased from 32 to 85 and the median (IQR) annual hospital volume of CABG decreased from 70 (41 to 119) to 40 (16 to 85); but the maximum annual volume of an individual hospital increased from 1107 to 3822 (see Supplementary material online, Table S2). The aggregated mean (SD) CABG volume for the 102 hospitals was 398.5 (1702.6) over the study period (see Supplementary material online, Table S3).
Trends in mortality and major complication rates
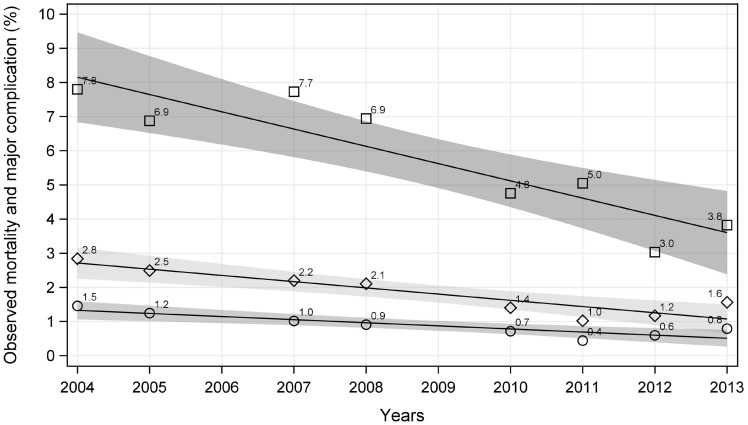
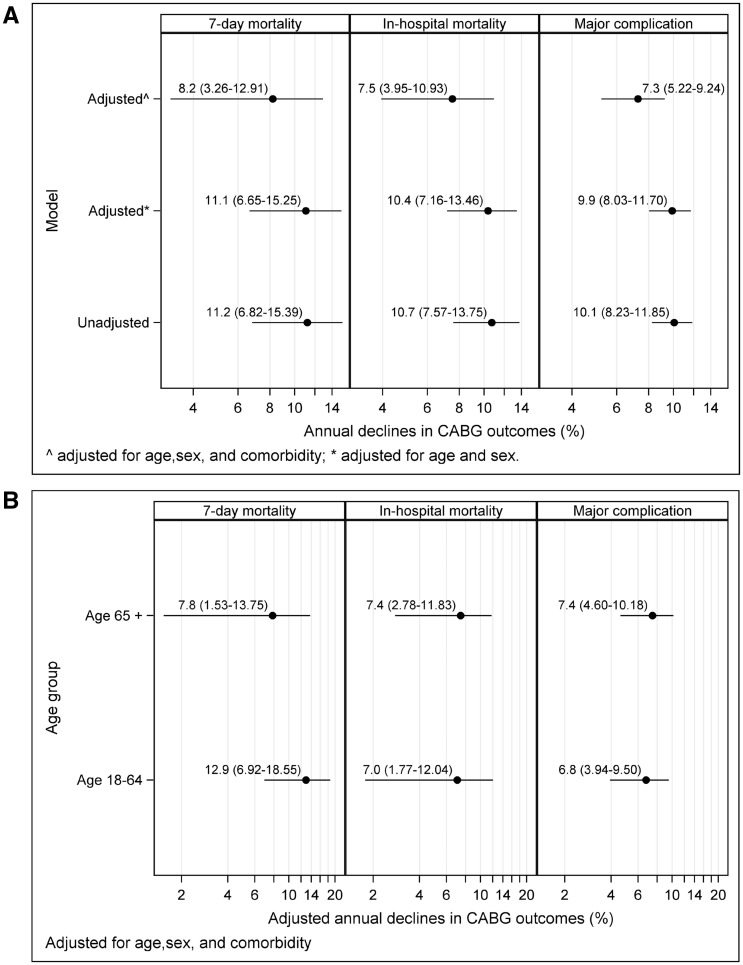
The aggregated in-hospital total mortality, 7-day mortality, and complication rates during the study period were 1.8, 0.9, and 5.5%, respectively. Patients undergoing CABG surgeries in recent years had significantly lower mortality and major complication rates than previous years. Between 2004 and 2013, the in-hospital total mortality rate decreased from 2.8% (95% CI: 2.32–3.36) to 1.6% (95% CI: 1.31–1.81), with a difference of 1.28 percentage points (95% CI: 0.70–1.85), and 7-day in-hospital mortality rate decreased from 1.5% (95% CI: 1.11–1.88) to 0.8% (95% CI: 0.62–0.99), with a difference of 0.7 percentage points (95% CI: 0.25–1.08). The major complication rate decreased from 7.8% (95% CI: 6.96–8.64) to 3.8% (95% CI: 3.44–4.21), with a difference of 4.0 percentage points (95% CI: 3.05–4.90) (Figure 1, Table 1). These findings did not change substantially after accounting for patients’ demographic and clinical characteristics. After adjusted for age, sex, and comorbidities, annual declines were 7.5 percentage points (95% CI: 3.95–10.93), 8.2 percentage points (95% CI: 3.26 to 12.91), and 7.3 percentage points (95% CI: 5.22–9.24) for in-hospital total mortality, 7-day mortality, and major post-operative complication rates, respectively (Figure 2A); age and sex adjusted annual declines were 10.4 percentage points (95% CI: 3.95–10.93), 11.1 percentage points (95% CI: 3.26 to 12.91), and 9.9 percentage points (95% CI: 5.22–9.24) for in-hospital total mortality, 7-day mortality, and major post-operative complication rates, respectively (Figure 2A). The age-specific subgroup analysis illustrates that elderly patients had a greater decline in rates than the younger group for both mortality and complication rates (Figure 2B).
Figure 1.
Observed in-hospital total mortality, in-hospital 7-day mortality, and complication rate from 2004 through 2013.
Figure 2.
Adjusted annual reduction of in-hospital total mortality in-hospital 7-day mortality, and complication rate. (A) Adjusted annual reduction of in-hospital total mortality in-hospital 7-day mortality, and complication rate (overall); (B) adjusted annual reduction of in-hospital total mortality in-hospital 7-day mortality, and complication rate (in different age intervals).
The sensitivity analysis included 13 hospitals that were repeated in each of the 2-year periods (2004–2005, 2007–2008, 2010–2011, and 2012–2013). These hospitals accounted for 27 130 patients, which is 66.7% of the total number of patients in the whole sample. Supplementary material online, Figures S1 and S2 show that the patterns of trends in mortality and complication rates between this subsample and the full sample are similar, but the reductions from these hospitals were much larger than all other hospitals.
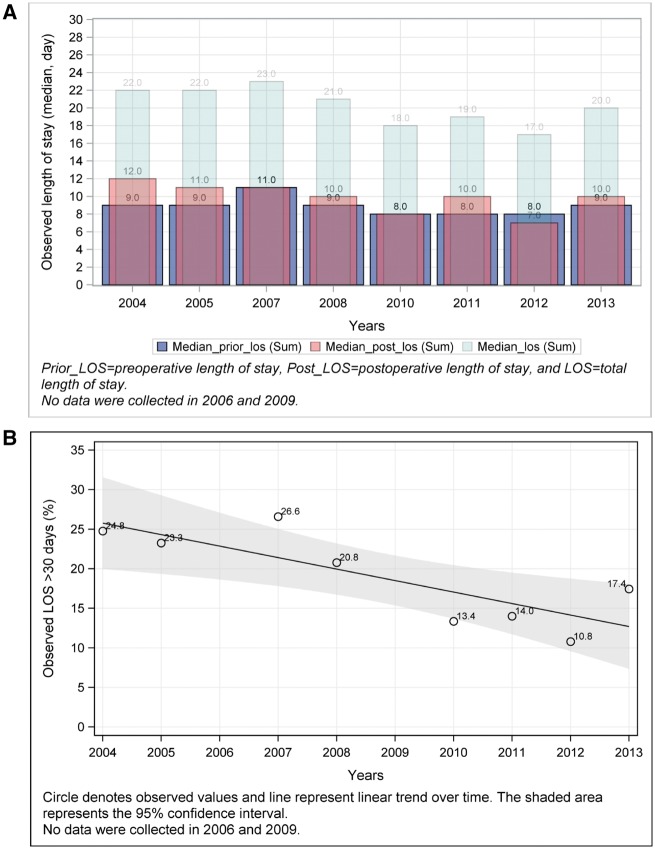
Trends in length of stay
Between 2004 and 2013, the median (IQR) Pre-LOS remained unchanged from 9.0 (9.0) to 9.0 (8.0) days, Post-LOS declined from 12.0 (8.0) to 10.0 (7.0) days, and total LOS declined from 22.0 (13.0) to 20.0 (12.0) days (Figure 3A, Table 1). Supplementary material online, Figure S3 shows the trends in median LOS among hospitals included in the sensitivity analysis. Nevertheless, the proportion of patients who had an overall LOS for more than 30 days declined remarkably from 24.8% in 2004 to 17.4% in 2013 (P < 0.001, Figure 3B).
Figure 3.
Length of stay (LOS). (A) Observed pre-operative LOS, post-operative LOS, and total LOS; (B) Observed LOS over 30 days.
Trend variations at hospital level
Between 2004–2005 and 2012–2013, the quartile coefficients of dispersion changed from 0.49 to 0.33, 0.30 to 0.16, and 0.46 to 0.50 for in-hospital mortality, major complication, and length of stag greater than 30 days, respectively.
Discussion
In this comprehensive analysis of the trends in CABG outcomes in urban teaching hospitals in China, there were marked reductions in mortality and major complication rates. Improvements in the length of hospital stay were observed, but the hospital stays were quite long by international standards. During the study period, the absolute reductions were 1.3% for the in-hospital total mortality, 0.7% for the in-hospital 7-day mortality, and 4.0% for the major complication rate. The risk of in-hospital death was approximately 40% lower in patients undergoing CABG in 2013 than those in 2004 despite a shortened LOS. The degree of reductions was similar between patients who were 18–64 years old, and those who were 65 years or older. According to the most recently reported annual isolated CABG volume of approximately 30 000 cases,4,5 these decreases translate to nearly 400 annual additional patients discharged alive and 1200 annual additional patients discharged free from major complications. In contrast to our findings, McNeely et al. found, in a series involving 1, 264, 265 US Medicare patients over a 12-year period (2000–2012), a decline in CABG volume with slightly higher in-hospital mortality (from 4.2% in 2000 to 2.7% in 2012) and much shorter total median LOS (8 days in the USA vs. 20 days in China).10 Different demographic characteristics, epidemiological changes, and varied health policies might underline the differences in results between the two registries.
There are numerous possible explanations for our findings. First, the trends may be due to Chinese surgeons having acquired more experience with CABG procedures over the past decade. Unlike in the USA where CABG rates have declined rapidly,11–13 CABG volume, as a whole, in China has increased, most likely due to the great increase in the incidence of CAD in the country over the past decade. For example, among the 102 hospitals included in the study, the maximum annual CABG volumes increased from 1107 in 2004 to 3822 in 2013. This is consistent with studies that have shown that higher volumes of cardiac surgeries are associated with better cardiac surgery outcomes.12,14
Second, the trends we observed may, in part, reflect the success of national efforts to improve cardiovascular care. CABG in China was developed during a period of extensive national efforts focused on improving care, processes, and outcomes.6 In the early 2000s, a series of regulations calling attention to patient safety issues were released.7,15 By the end of 2009, legislation for improvements in medical practice and quality control had been established.6 In 2010, the Chinese National Center for Cardiovascular Disease was founded. The Center aims to develop a series of guidelines and conducts evidence-based studies for CVD care in China. Then the Chinese Health Ministry launched a non-communicable disease prevention program aimed to establish a mortality-monitoring network to cover 90% of the Chinese population in 2012.1 Additionally, the Chinese cardiac surgery community has launched numerous national programs to monitor, analyse, and improve outcomes.5,16 It has also conducted various training programs and seminars to help Chinese cardiac hospitals broaden their horizons, and improve surgeons' proficiency with high healthcare standards.17 All of these efforts may have contributed to the improvement in CABG outcomes.
Third, some of the observed improvement in mortality and complication rates may be attributed to the Chinese Cardiac Surgery Registry. In 2004, the Chinese Cardiac Surgery Registry was established to evaluate surgical outcomes in patients undergoing cardiac surgery. The registry included more than 100 urban cardiac surgery centres in 2016. The registry sends annual hospital-specific performance reports, including overall outcomes and ranking information, to its members.9 These reports provide useful information that helps hospitals to identify areas for improvement and understand trajectories of change. The improvements observed in CABG performance within Chinese Cardiac Surgery Registry hospitals may have been motivated by these interventions.
Our study also indicates important areas for improvement. The variations at the hospital level were significant. Notably, variation in complication rates was larger than that observed in mortality rates, suggesting that there is more potential for the rate of complications to improve under the current Chinese healthcare system. Additionally, despite dropping significantly, the absolute lengths of Pre-LOS and Post-LOS are still much longer than those reported in Western countries.18,19 Possible explanation might be that patients too precarious to wait at home, often ‘squeezed’ themselves into hospitals for an extended period before surgery. There are many reasons for this situation, probably including restricted operating room access, lack of ICU beds, or delays due to more urgent cases. What’s more, patients and doctors in China tend to prefer a longer LOS after coronary angiography, percutaneous coronary intervention, and CABG as a precautionary measure. High patient volume and relatively few available operating rooms may also be responsible for higher Pre-LOS because patients must wait until an operating room becomes available. This latter reason for increased Pre-LOS is not unique to China.20 Prolonged LOS, both pre- and post-operatively, has been shown to be associated with higher utilization of hospital resources and decreased quality of life after CABG, most likely due to the increased risk for developing in-hospital adverse events.21 In addition to opening more cardiac surgery centres, China should increase investments in less-developed areas to reduce regional inequalities in resource allocation, build capacity in community hospitals and rehabilitation centres, and alter payment schemes to incentivize higher quality of care.
Our study has several limitations. First, our findings represent only the urban teaching hospitals in China. The Chinese Cardiac Surgery Registry recruits its members on a voluntary basis and all of the participating hospitals in the Chinese Cardiac Surgery Registry are urban teaching hospitals. Thus, they may exhibit better performance than would be seen in hospitals that did not participate in the registry because teaching hospitals may have contributed in terms of having environments with continuous learning and improvements embedded in patient care. The recent growth of percutaneous coronary intervention in China may also have resulted in fewer high-risk patients receiving CABG,22 which could also be partially responsible for lower CABG mortality and complication rates. The lack of national percutaneous coronary intervention data in China precluded our ability to assess this factor in our analysis. However, because patient characteristics did not change remarkably over the study period, the impact of this factor should be small. Finally, our mortality and complication rates were measured as in-hospital outcomes rather than 30-day outcomes. Nevertheless, these in-hospital outcomes provide important information about CABG quality and outcomes in China. Because the scope of our study did not allow us to address these limitations in depth, future studies are warranted to elucidate them.
In conclusion, we found that isolated CABG-related in-hospital mortality, major complication rate, and LOS have improved in urban teaching hospitals in China over the last decade. Despite these important improvements, our findings also suggest that there is ample opportunity for further improvement in CABG care in China.
Supplementary material
Supplementary material is available at European Heart Journal – Quality of Care and Clinical Outcomes online.
Acknowledgements
We thank all the hospitals that participated in the China Cardiovascular Surgery Registry for their contributions to this work. We also thank Maliha Tariq, B.A. Research Assistant and Paul Horak, B.S., Postgraduate Associate in Medicine (Cardiology), both from the Center for Outcomes Research and Evaluation, Yale-New Haven Hospital and Yale University, for their valuable editorial comments. The content of the publication does not necessarily reflect the views or policies of the Chinese government. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
Funding
Projects in the National Science & Technology Pillar Program during the 12th 5-year plan period (2011BAI11B21); National Key Research and Development Program (2016YFC1302001); Hospital for Cardiovascular Outcomes Research at Yale University (1U01HL105270-02); and National Heart, Lung, and Blood Institute to H.M.K. in part.
Conflict of interest: Dr Krumholz reports other from Johnson & Johnson (Janssen) and Medtronic, personal fees from UnitedHealth, other from Hugo, personal fees from IBM Watson, personal fees from Element Science, grants from FDA and Medtronic, personal fees from Aetna, other from Centers for Medicare & Medicaid Services, outside the submitted work. None of the rest authors declared.
Supplementary Material
References
- 1. National Center for Cardiovascular Disease. Chinese Cardiovascular Disease Report 2012. Beijing: Encyclopedia of China Publishing House; 2013. p145–152. [Google Scholar]
- 2. Yang G. Deaths and Their Risk Factors Among Chinese Population. Beijing: Union Medical University Press of China; 2005. [Google Scholar]
- 3. Ministry of Health, the People's Republic of China. Vital Statistics Annual Reports. People's Medical Publishing House; 2012.
- 4. Zhu D, Long C, Hei F.. National cardiac surgery and extracorporeal circulation data: 2013 white book. Chin J Extracorporeal Circ 2014;12:129–133. [Google Scholar]
- 5. Hu S. History of Chinese coronary surgery. J Med Res 2013;42:4–6. [Google Scholar]
- 6. Liu JT. Historical review and basic features for medical quality research in the past three decades in China. Chin Hosp Manage 2010;30:11–13. [Google Scholar]
- 7. Hao R, Wang F.. The gold-standard measurement for quality management for modern hospitals: “satisfaction rate by patients”. Hosp Qual 2003;7:29–31. [Google Scholar]
- 8. Rao C, Zhang H, Gao H, Zhao Y, Yuan X, Hua K, Hu S, Zheng Z.. The Chinese cardiac surgery registry: design and data audit. Ann Thorac Surg 2016;101:1514–1520. [DOI] [PubMed] [Google Scholar]
- 9. Hu S, Zheng Z, Yuan X, Wang Y, Normand SL, Ross JS, Krumholz HM.. Coronary artery bypass graft: contemporary heart surgery center performance in China. Circ Cardiovasc Qual Outcomes 2012;5:214–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McNeely C, Markwell S, Vassileva C.. Trends in patient characteristics and outcomes of coronary artery bypass grafting in the 2000 to 2012 Medicare population. Ann Thorac Surg 2016;102:132–138. [DOI] [PubMed] [Google Scholar]
- 11. Mack MJ, Brown PP, Kugelmass AD, Battaglia SL, Tarkington LG, Simon AW, Culler SD, Becker ER.. Current status and outcomes of coronary revascularization 1999 to 2002: 148,396 surgical and percutaneous procedures. Ann Thorac Surg 2004;77:761–766; discussion 766–768. [DOI] [PubMed] [Google Scholar]
- 12. Post PN, Kuijpers M, Ebels T, Zijlstra F.. The relation between volume and outcome of coronary interventions: a systematic review and meta-analysis. Eur Heart J 2010;31:1985–1992. [DOI] [PubMed] [Google Scholar]
- 13. Riley RF, Don CW, Powell W, Maynard C, Dean LS.. Trends in coronary revascularization in the United States from 2001 to 2009: recent declines in percutaneous coronary intervention volumes. Circ Cardiovasc Qual Outcomes 2011;4:193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Glance LG, Dick AW, Osler TM, Mukamel DB.. The relation between surgeon volume and outcome following off-pump vs on-pump coronary artery bypass graft surgery. Chest 2005;128:829–837. [DOI] [PubMed] [Google Scholar]
- 15. Zheng Y. Healthcare procedure and outcomes evaluation. Chin Health Qual Manage 2005;12:70–72. [Google Scholar]
- 16. Meng X, Bai T, Jiang Y, Zhang Z.. Establishment and application of cardiac surgery database. Chin J Hosp Adm 2003;19:755–756. [Google Scholar]
- 17. Zhang G, Han L, Xu Z, Li B, Wang B, Zhao Z, Shen H, Shen X.. Reflection on standardized training programs for residents of cardiac surgery. Northwest Med Educ 2012;20:403–406. [Google Scholar]
- 18. Bhamidipati CM, LaPar DJ, Fonner E Jr, Kern JA, Kron IL, Ailawadi G.. Outcomes and cost of cardiac surgery in octogenarians is related to type of operation: a multiinstitutional analysis. Ann Thorac Surg 2011;91:499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cserep Z, Losoncz E, Toth R, Toth A, Juhasz B, Balog P, Vargha P, Gal J, Contrada RJ, Falger PR, Szekely A.. Self-rated health is associated with the length of stay at the intensive care unit and hospital following cardiac surgery. BMC Cardiovasc Disord 2014;14:171.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fidelman C. Cardiac Patients Living in Fear Montreal Gazette; 2011. http://scholar.google.com/scholar_lookup?title=Cardiac%20Patients%20Living%20in%20Fear.%20Montreal%20Gazette&author=C.%20Fidelman&publication_year=2011 (14 February 2011).
- 21. Cowper PA, Peterson ED, DeLong ER, Jollis JG, Muhlbaier LH, Mark DB.. Impact of early discharge after coronary artery bypass graft surgery on rates of hospital readmission and death. The Ischemic Heart Disease (IHD) Patient Outcomes Research Team (PORT) Investigators. J Am Coll Cardiol 1997;30:908–913. [DOI] [PubMed] [Google Scholar]
- 22. Morrison DA, Sethi G, Sacks J, Henderson W, Grover F, Sedlis S, Esposito R, Ramanathan K, Weiman D, Saucedo J, Antakli T, Paramesh V, Pett S, Vernon S, Birjiniuk V, Welt F, Krucoff M, Wolfe W, Lucke JC, Mediratta S, Booth D, Barbiere C, Lewis D.. Percutaneous coronary intervention versus coronary artery bypass graft surgery for patients with medically refractory myocardial ischemia and risk factors for adverse outcomes with bypass: a multicenter, randomized trial. Investigators of the Department of Veterans Affairs Cooperative Study #385, the Angina With Extremely Serious Operative Mortality Evaluation (AWESOME). J Am Coll Cardiol 2001;38:143–149. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.