Abstract
Background
Foreign body aspiration refers to the inhalation of an object into the respiratory system and is a serious and potentially fatal event. A distinct group of patients has recently been recognized among Muslim nations. These patients include women who wear headscarves and place the safety pin in their mouth prior to securing the veils, leading to accidental foreign body aspiration. The aim of this study was to analyze the main presentation, diagnosis, treatment, and outcome of patients with scarf pin aspiration.
Methods
This prospective study involved patients with a history of scarf pin aspiration admitted to a single center during an 18-month period. Their main presentation, diagnosis, treatment, and outcome were analyzed.
Results
In total, 27 patients were included. The needle was extracted by flexible bronchoscopy in 12 (44.4%) patients, rigid bronchoscopy in 13 (48.1%), and thoracotomy in 2 (74%). One patient died during rigid bronchoscopy. All remaining 26 patients were satisfied with the postsurgical outcome at a mean follow-up of 1 week.
Conclusions
Scarf pin aspiration differs from other types of foreign body aspiration considering the specific population affected, and its management algorithm may thus differ from that of other foreign bodies. The left main bronchus is the most common site of pin impaction. Rigid bronchoscopy is the most commonly performed procedure for successful retrieval.
Keywords: Foreign body aspiration, scarf pin, hijab syndrome, bronchoscopy
Key messages
The hazards of a special type of scarf pin used on a wide scale are herein reported, and a new name for scarf pin aspiration is proposed for better communication and a more accurate description.
Introduction
Foreign body aspiration (FBA) refers to the inhalation of an object into the respiratory tract and is a serious and potentially fatal event.1 Asphyxiation secondary to FBA is a leading cause of accidental death among children younger than 4 years.2 The inherent tendency of children to place new objects into their mouths with immature posterior dentition and neuromuscular mechanisms puts them at great risk of FBA.3 Although FBA is rare in adults, risk factors in this population include neurologic dysfunction, dental trauma, and aspiration of larger-than-normal pieces of food.4 Most aspirated foreign bodies are organic materials, primarily nuts and seeds.2 However, a distinct group of patients has recently been recognized among Muslim nations. These patients include women who wear headscarves and place the safety pin in their mouth prior to securing the veils. Aspiration of these pins occurs with talking, laughing, and coughing.5 Although inhaled foreign bodies commonly lodge in the right bronchial tree, scarf pins more often settle in the left tree. Numerous authors have attributed this finding to the Bernoulli phenomenon, which states that coughing, laughing, or speaking creates stronger negative pressure in the narrow left bronchus than in the wide right bronchus.5 In contrast to usual FBA, which has a variety of clinical presentations, scarf pin aspiration is usually either asymptomatic or presents with a cough and/or dyspnea in spite of a clear history.6
Posteroanterior and lateral chest radiographs are efficient tests with which to diagnose and localize the pins, which appear as linear metallic opacities.7 Foreign body extraction is usually performed through a rigid or flexible scope. Patients with scarf pin aspiration require thoracotomy more often than do patients with other forms of FBA. This may be due to distal migration of the pin to subsegmental bronchi because of its small size.5
In this prospective study, we analyzed the main presentation, diagnosis, treatment, and outcome of patients with scarf pin aspiration. In this report, we highlight the potential danger of these pins to the health of veiled women.
The key questions are how this type of FBA presents and how to prevent its occurrence. We believe that scarf pin FBA is common in Muslim communities; therefore, the main goal of this report is to add more clinical information about this subject to the literature.
Patients and methods
This prospective study involved patients with a history of scarf pin aspiration admitted to a single center during an 18-month period. Only patients with a history of scarf pin aspiration were included. Scarf pin aspiration was diagnosed by obtaining a detailed history including the onset time, duration of time from aspiration to presentation, and size and shape of the scarf pin. A detailed physical examination was performed in all patients to identify any cardiorespiratory abnormalities. Posteroanterior and lateral chest radiographs were obtained for all patients to determine the exact anatomical location and alignment of the pin. The same surgeon performed therapeutic flexible fiberoptic bronchoscopy (FOB) (Olympus CV-180 Evis Exera II Endoscopy System) for all patients with the aid of topical anesthesia. In cases of failed extraction by FOB, the patient was transferred to the operation room. Rigid bronchoscopy (Karl Storz Endoskope system) was performed under general anesthesia. When extraction with rigid bronchoscopy failed, posterolateral thoracotomy was performed. Patients who underwent FOB were observed for a couple of hours after the procedure. Patients who underwent successful rigid bronchoscopy were hospitalized for 24 hours. Those who underwent classic thoracotomy were discharged from the hospital after total expansion of both lungs and removal of the chest tubes.
Descriptive statistics (means, numbers, and percentages) were calculated for all variables by IBM SPSS Statistics 2015 (IBM Corp., Armonk, NY).
Results
This study included 27 female patients ranging in age from 8 to 30 years (mean age, 15.74 years). The main presenting symptoms were coughing and shortness of breath. Almost all patients with scarf pin aspiration reported that the event had been induced by talking, laughing, or coughing while the pin was being held in the mouth between the upper and lower teeth. The most common symptom was coughing. Almost all cases were diagnosed using posteroanterior and lateral chest radiographs. Table 1 shows the signs and symptoms according to the location of the needle. FOB bronchoscopy was successful in removing the pins in 12 (44.4%) patients; rigid bronchoscopy was required in 13 (48.1%) patients, and thoracotomy was required in 2 (7.0%). No morbidities occurred among the patients who underwent thoracotomy, and one death occurred during rigid bronchoscopy.
Table 1.
Signs and symptoms according to pin location
| Location of the needle | Signs and symptoms |
Total | |
|---|---|---|---|
| Cough | Dyspnea and cough | ||
| LBPT | 9 (33.3%) | 7 (25.9%) | 16 (59.2%) |
| RBPT | 7 (25.9%) | 1 (3.7%) | 8 (29.6%) |
| Trachea | 1 (3.7%) | 2 (7.4%) | 3 (11.1%) |
| Total | 17 (62.9%) | 10 (37.0%) | 27 (100.0%) |
LBPT, left bronchopulmonary tree; RBPT, right bronchopulmonary tree.
Discussion
FBA remains a common but largely preventable problem.8 Most patients with FBA are children younger than 3 years.2 Patients with aspirated headscarf pins comprise a different age group. Our literature review showed that the mean age of this population is 13 to 20 years.5,6,7,9 In the present series, the patients’ ages ranged from 8 to 30 years with a mean age of 15.74 years. The occurrence of scarf pin aspiration in older patients compared with other types of FBA can be explained by the fact that this accident occurs mostly in young Muslim girls who have newly started wearing hijabs.
A general male predominance for FBA has been reported by many authors, while scarf pin aspiration occurs uniquely in female patients; no reports have described male patients.5–15 Our study was consistent with this finding in that all patients were female.
Children with FBA typically present with symptoms of coughing, dyspnea, wheezing, cyanosis, or stridor.2 In the current study, the main presenting symptoms were coughing and shortness of breath. Almost all patients with scarf pin aspiration reported that the event had been induced by talking, laughing, or coughing while the pin was being held in the mouth between the upper and lower teeth.10,12 We reported the same event in all patients. This indicates the same pathophysiological mechanism of the disease.
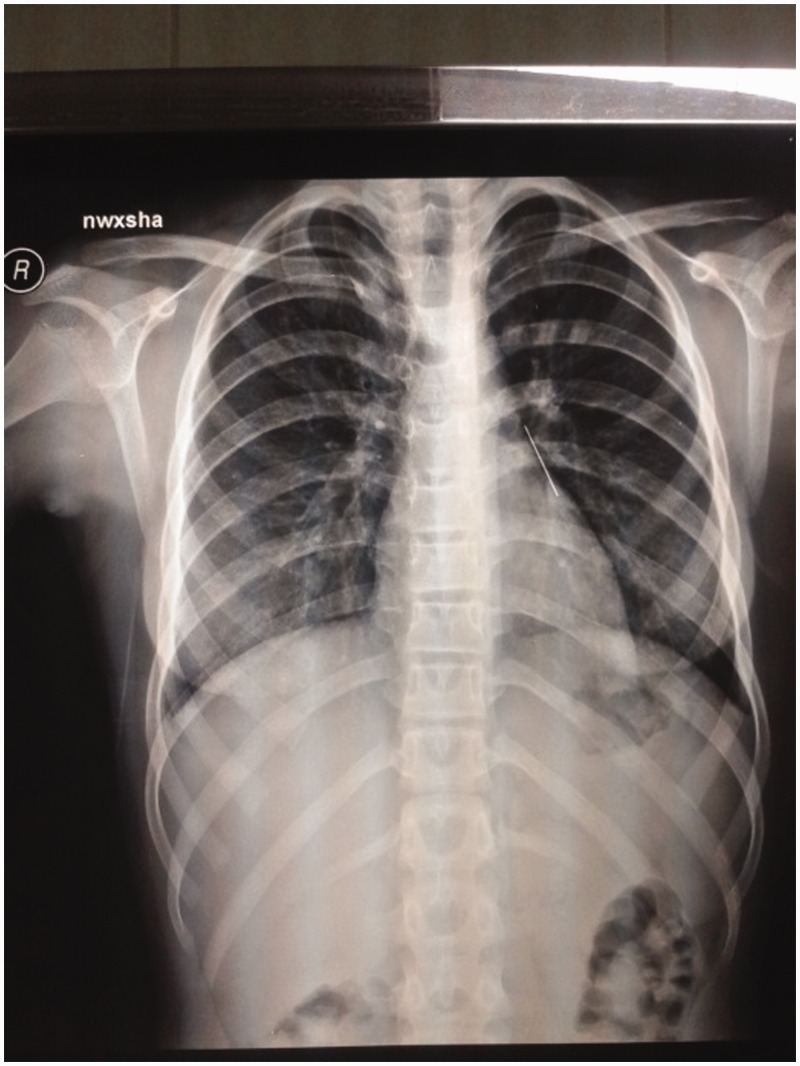
Difficulty in diagnosis is a common problem when dealing with FBA.16 FBA may not be suspected in some cases, leading to chronic lung problems involving asthma-like symptoms, recurrent pulmonary infections, atelectasis, and bronchiectasis.17 However, diagnosis of scarf pin aspiration is less challenging because the needle is metallic and easily recognized due to its characteristic shape on plain chest radiographs in addition to the patient’s obvious history (Figures 1 and 2).17 In the present study, almost all cases were diagnosed using posteroanterior and lateral chest radiographs. In infants and young children, the occurrence of left- and right-side foreign bodies is comparable,18 while in patients with scarf pin aspiration, the left main bronchus is the most common site followed by the right main bronchus and trachea.5–7 In the present study, the pin was found on the left side in 16 (59.3%) patients, on the right side in 8 (29.6%), and in the trachea in 3 (11.1%). The left-side predominance may be explained by the narrow lumen of the left main bronchus; this leads to the production of stronger negative pressure during inhalation.
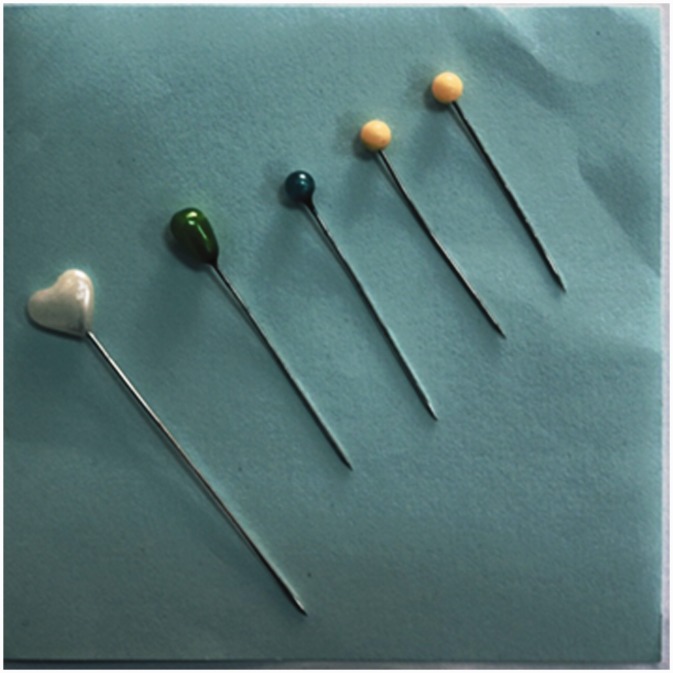
Figure 1.
Scarf pins of different sizes
Figure 2.
Chest radiographs showing a headscarf pin: posteroanterior view of the left lower lobe
Rigid bronchoscopy is the most common procedure used to manage FBA in infants and young children, while FOB is a safe and successful first method for retrieval of aspirated scarf pins.19 In our study, FOB was successful in removing the pins in 12 (44.4%) patients, while 13 (48.1%) needed rigid bronchoscopy and 2 (7.0%) needed thoracotomy. In comparing our findings with other published studies, we observed that our results are more practical because both FOB and rigid bronchoscopy were effective in scarf pin extraction, but the effectiveness was determined by patient-related factors and the operator’s ability. The incidence of FBA-related mortality reportedly ranges from 1% to 12% according to the type of foreign body; the highest incidence is associated with sharp objects.14 In the present study, one (3.7%) patient died of scarf pin aspiration. This death was due to massive endobronchial bleeding associated with extraction during rigid bronchoscopy despite all measures taken to save the patient’s life.
Our literature review, which included the present study, indicates that the pathophysiology, presentation, and management of scarf pin aspiration are specific and consistent among young Muslim girls and women who wear a hijab. Therefore, we propose calling this condition “hijab syndrome” for easier communication and because it symbolically represents the entire disease course from start to end. This is the first study to name this condition as such. Table 2 shows the most recent reports describing scarf pin aspiration.
Table 2.
Most recent publications on scarf pin aspiration
| Authors | Country of study | Year of publication | No. of cases | Method of extraction |
||
|---|---|---|---|---|---|---|
| FOB | RB | Thoracotomy | ||||
| Fenane et al.7 | Morocco | 2015 | 28 | 28* | ||
| Rizk et al.5 | Egypt | 2014 | 83 | 78 | 5 | |
| Taha13 | Iraq | 2013 | 5 | 3 | 1 | 1 |
| Al-Azzawi10 | Iraq | 2013 | 20 | 19 | 1 | |
| Hamad et al.6 | Egypt | 2010 | 73 | 71 | 2 | |
Patients requested surgical treatment after repeated unsuccessful bronchoscopic removal.
FOB, fiberoptic bronchoscopy; RB, rigid bronchoscopy.
Conclusions
Scarf pin aspiration should ideally be called “hijab syndrome” because this name encompasses all details of the event and enables easier communication among health care professionals. Scarf pin aspiration occurs in young Muslim girls and women who wear a hijab. A history of pin inhalation is the most important part of the diagnosis, and the condition is confirmed by plain chest X-ray examination. Rigid bronchoscopy is the most commonly performed procedure for successful retrieval. Hijab syndrome is an important cause of morbidity among young Muslim girls and women. We therefore recommend the outright banning of this pin from Muslim countries with the singular aim of discouraging its use.
Acknowledgements
The authors acknowledge all personnel who assisted in caring for the patients.
Authors’ contributions
Aram Baram: Performed the surgeries, designed the study, and performed the follow-up, data collection, and statistical analysis. Fahmi H. Kakamad: Assisted with the surgeries, follow-up, study design, data collection, and drafting of the manuscript. Delan Ahmed Bakir: Assisted with the surgeries, follow-up, study design, data collection, and drafting of the manuscript.
Declaration of Conflicting Interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Baharloo F, Veyckemans F, Francis C, et al. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest 1999; 115: 1357–1362. [DOI] [PubMed]
- 2.Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 Cases. AnesthAnalg 2010; 111: 1016–1025. [DOI] [PubMed] [Google Scholar]
- 3.Ozguner IF, Buyukyavuz BI, Savas C, et al. Clinical experience of removing aerodigestive tract foreign bodies with rigid endoscopy in children. Pediatr Emerg Care 2004; 20: 671–673. [DOI] [PubMed] [Google Scholar]
- 4.Shields T, LoCicero J, Reed C, et al. General thoracic surgery, Seventh Edition Philadelphia: Lippincott Williams &Wilkins, 2009. [Google Scholar]
- 5.Rizk N, Gwely N, Biron V, et al. Metallic hairpin inhalation: a healthcare problem facing young Muslim females. J Otolaryngol Head Neck Surg 2014; 43: 21–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamad AM, Elmistekawy EM, Ragab SM. Headscarf pin, a sharp foreign body aspiration with particular clinical characteristics. Eur Arch Otorhinolaryngol 2010; 267: 1957–1962. [DOI] [PubMed] [Google Scholar]
- 7.Fenane H, Bouchikh M, Bouti K, et al. Scarf pin inhalation: clinical characteristics and surgical treatment. J Cardiothorac Surg 2015; 10: 61–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Sarraf N, Jamal-Eddine H, Khaja F, et al. Headscarf pin tracheobronchial aspiration: a distinct clinical entity. Interact Cardiovasc Thorac Surg 2009; 9: 187–190. [DOI] [PubMed] [Google Scholar]
- 9.Apilliogulları B, Duzgun N, Esme H, et al. Headscarf pin localized in the right main bronchus and two pins in the abdomen. Eur J Gen Med 2015; 12: 82–85. [Google Scholar]
- 10.Al-Azzawi A. utility of fiberoptic bronchoscopy for retrieval of aspirated headscarf pins. European Scientific Journal March 2013 edition vol.9, No.9 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431.
- 11.Wood R. The diagnostic effectiveness of the flexible bronchoscope in children. Pediatr Pulmonol 1985; 1: 188–192. [DOI] [PubMed] [Google Scholar]
- 12.Kakunje A, MD, Angri S, Kakkilaya S. Headscarf (hijab) pin aspiration: effects of fashion phenomenon in Islam girls. P J Psychol Med 2014; 15: 179–180. [Google Scholar]
- 13.Taha A. The use of fiberoptic bronchoscope to remove aspirated tracheobronchial foreign bodies: Our experience. Case Reports in Clinical Medicine 2013; 2: 285–290. [Google Scholar]
- 14.Elmustafa OM, Osman WN. A clinical experience with sharp bronchial foreign bodies in Sudanese patients. SJPH 2009; 4: 256–258. [Google Scholar]
- 15.Tanriverdi F, Kurtoglu Celik G, Pamukcu Gunaydin G. The lucky patient who aspirated a needle. Turk J Emerg Med 2015; 15: 142–144. doi: 10.5505/1304.7361.2015.26937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karakoc F, Cakir E, Ersu R, et al. Late diagnosis of foreign body aspiration in children with chronic respiratory symptoms. Int J Pediatr Otorhinolaryngol 2007; 71: 241–246. [DOI] [PubMed] [Google Scholar]
- 17.Kiyan G, Gocmen B, Tugtepe H. Foreign body aspiration in children: the value of diagnostic criteria. Int J Pediatr Otorhinolaryngol 2009; 73: 963–967. [DOI] [PubMed] [Google Scholar]
- 18.Stool SE, Manning SC. Foreign bodies of the pharynx and esophagus. In: Blueston CD, Stool SE, Kenna MA. (eds). Pediatric otolaryngology, 3rd ed Philadelphia: W.B. Saunders, 1996, pp. 1169–1169. [Google Scholar]
- 19.Lan RS, Lee CH, Chiang YC, et al. Use of fiberoptic bronchoscopy to retrieve bronchial for- eign bodies in adults. Am Rev Respir Dis 1989; 140: 1734–1737. doi:10.1164/ajrccm/140.6.1734. [DOI] [PubMed] [Google Scholar]