Abstract
Study Objectives:
To describe sleep duration patterns of adults over a 20-year period; to compare sociodemographic, lifestyle, and health characteristics across these patterns; and to relate the patterns to sleep quality.
Methods:
The study population consisted of 3695 adults aged 20 to 59 years at baseline. Five measurements of self-reported sleep duration were used to compose seven patterns from 1987 to 2012: persistent short (≤6 hours), moderate (7–8 hours), or long (≥9 hours) sleep duration and several changing patterns (varying and became short, moderate, or long sleepers). Multinomial logistic regression analyses were used to compare characteristics across sleep duration patterns.
Results:
About 56% of the adults had persistent moderate sleep duration over 20 years. This group had a better sleep quality than the other groups. Of the adults who changed in their sleep duration (40%), 43% became a short sleeper. Sleep duration patterns that deviate from persistent moderate sleep duration were associated with physical inactivity during leisure time (odds ratios [ORs] and 95% confidence intervals [95% CIs] varied between 1.26 [1.04–1.53] and 1.58 [1.06–2.37]) and with poor self-rated health (ORs [95% CIs] varied between 1.50 [1.20–1.87] and 2.15 [1.48–3.12]).
Conclusions:
Nearly half of the adults did not have persistent moderate sleep duration over a 20-year period and more than one-sixth became short sleeper. This is reason for concern considering the adverse health status associated with short and long sleep duration. Leisure-time physical activity is a potential important target to prevent unfavorable changes in sleep duration over the life course.
Keywords: sleep duration, sleep quality, population-based cohort study, epidemiology.
Statement of Significance
Short and long sleep duration have been associated with adverse health status. However, little is known about how adults actually sleep over their life course. The present study provides quantitative data on sleep in adults over a 20-year period. The results show that almost half of the adults did not maintain moderate sleep duration over their life course and that these adults had more often sleep quality complaints than persistent moderate sleepers. By comparing sociodemographic, lifestyle, and health characteristics, the present study contributes to the identification of potential targets for prevention. Our findings suggest that, in particular, leisure-time physical activity may be important. Further research is recommended to examine the role of such modifiable factors to prevent unfavorable sleep patterns.
INTRODUCTION
It is commonly thought that the amount of sleep has declined during the past few decades along with the transition to modern 24/7 societies.1 This has provoked claims of an epidemic of sleep deprivation in the general population.2 Simultaneously, there is growing evidence for an association of sleep duration deviating from the moderate range (ie, 7–8 hours) with adverse health status, such as obesity, coronary heart disease, diabetes, depression, and all-cause mortality.3–9 A meta-analysis by Cappuccio et al. showed that compared to adults who slept 7 to 8 hours per night, adults who slept shorter and longer had a 12% and 30% higher risk of premature death, respectively.7
Sleep duration of adults is not always persistent over time.10–12 For example, Ferrie et al. showed that the sleep duration of half of the adults aged 45–69 at baseline changed over a 5-year period.12 Since also changes (increases and decreases) in sleep duration have been associated with negative health conditions (eg, cognitive dysfunction, diabetes, and mortality), it is relevant to study the course of sleep duration over a long period.7,10–13 The study by Gilmour et al. examined sleep duration among adults at five time points over 8 years while other studies that have assessed sleep duration longitudinally often used only two measurement moments and/or specific study populations, such as children and adolescents.10–12,14,15 Thus, still little is known about the stability or change of sleep duration in the adult general population over a long period.
In addition, it is important to characterize the adults who are more likely to follow an unfavorable course of sleep duration over a long period. The identification of characteristics of adults associated with unfavorable sleep duration patterns could provide potential targets for prevention. Cross-sectional studies have shown that factors, such as gender, age, marital status, level of education, work status, smoking status, alcohol consumption, coffee consumption, physical activity, and both general and specific measures of health status are determinants of sleep duration among adults.13,16–22 However, it is unclear whether these factors also characterize adults with different courses of sleep duration over a long period.15 Furthermore, poor sleep quality has been associated with short and long sleep duration, adverse health status, and with a decrease in sleep duration over 8 years.9,15,16,23 To increase our understanding of the relationship between sleep and health, more research is needed in a longitudinal setting. Using existing longitudinal data, it was possible to explore individual patterns of sleep duration.
The specific research questions were: (1) what are the different sleep duration patterns among adults over 20 years? and (2) how can adults in different sleep duration patterns be characterized by sociodemographic factors, lifestyle factors, health characteristics, and sleep quality?
METHODS
Study Design and Sample
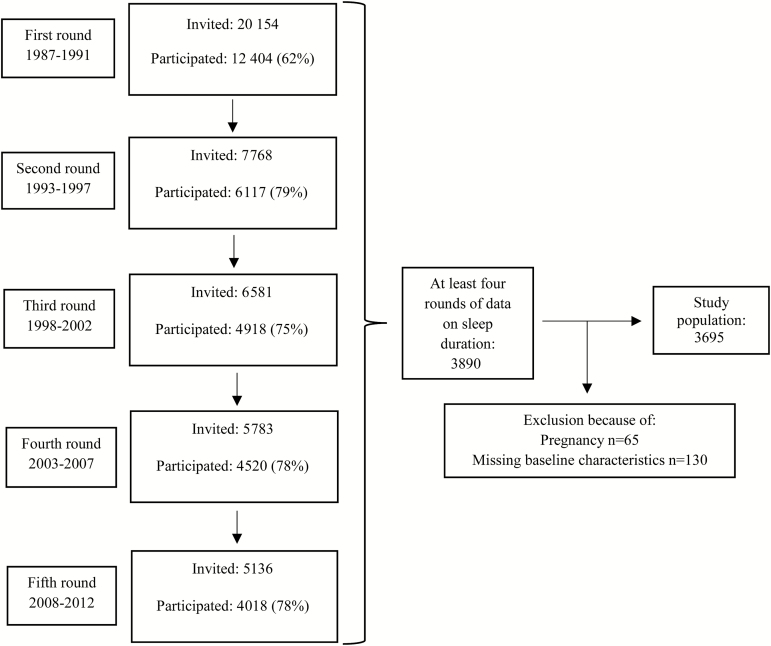
The Doetinchem Cohort Study (DCS) is an ongoing study that started in 1987–1991 and aimed to investigate the impact of sociodemographic, lifestyle, and biological risk factors on health among adults over the life course.24 The first DCS round (1987–1991) was carried out among 12,404 (initial response rate 62%) men and women aged 20 to 59 years from Doetinchem, which is a small provincial town in the Netherlands (Figure 1). Due to budget constraints, a random sample of these adults (n = 7768) was reinvited to participate in the second round of which 6117 (79%) participated. In the third round, 4918 (75%) of the invited inhabitants participated, in the fourth 4520 (78%), and in the fifth 4018 (78%). All participating adults gave written informed consent, and the study was approved by a Medical Ethics Committee.24
Figure 1.
Flowchart of participation in the Doetinchem Cohort Study. Note: in the second round a random sample (n = 7768) of the 12,404 adults who initially participated was reinvited because of budgetary reasons. In subsequent rounds, adults dropped out due to, for instance, emigration, death, and active withdrawal. Common reasons for active withdrawal were no time or interest to participate and participation in other medical investigations.
The present study included adults with complete information on sleep duration in the first round, the fifth round, and at least two of the three remaining rounds (n = 3890). Adults were excluded if they had incomplete information on relevant baseline characteristics (n = 130). Pregnant women were only excluded if there was no complete information on sleep duration in the other four rounds (n = 65). This resulted in a study population of 3695 adults.
Sleep
Adults were asked to answer the following question in all five rounds: “On average, how many hours do you sleep over a 24-hour period?”3 The first round included an open question on the number of hours of sleep over a 24-hour period. From the second to the fifth round, the answer options were: “5 hours or less,” “6 hours,” “7 hours,” “8 hours,” and “9 hours or more.” Adults sleeping 6 hours or less were defined as short sleepers, adults sleeping 7 or 8 hours as moderate sleepers, and adults sleeping 9 hours or more as long sleepers. This was in accordance with previous studies and with the consensus recommendations of The American Academy of Sleep Medicine.3,5,7,25
Five measurements of self-reported sleep duration were used to compose sleep duration patterns over a 20-year period from 1987 to 2012 (Table 2). One missing value or one deviating value in sleep duration in the second to fourth round was allowed to classify adults into these patterns. For example, participants with moderate sleep duration at round one, two, four, and five, but with missing data on sleep duration at round three or with short or long sleep duration at round three were classified as persistent moderate sleepers. Hence, the classification was based on the sleep duration measurements of the first round, the fifth round, and at least two of the three remaining rounds. Seven sleep duration patterns were defined because a wider subdivision resulted in a low number of adults in some patterns. Adults who slept the same amount of hours in at least four rounds were defined as either (1) persistent moderate, (2) persistent short, or (3) persistent long sleepers. Adults who had a consequent change in their sleep duration were defined as either (4) became moderate, (5) became short, or (6) became long sleepers. All adults who had other variations in sleep duration over time were defined as (7) varying sleepers.
Table 2.
Definition and Frequencies of Seven Sleep Duration Patterns Over a 20-Year Period in the Total Study Population (n = 3695) Based on Five Rounds (1987–2012) of the Doetinchem Cohort Study.
| Sleep duration patterns | First round (1987–1991) | Second to fourth round (1993–2007) | Fifth round (2008–2012) | N (%) |
|---|---|---|---|---|
| Persistent moderate sleepers | 7–8 hours | 7–8 hours in ≥2 rounds | 7–8 hours | 2065 (55.9%) |
| Became moderate sleepers | ≤6 hours |
Remaining ≤6 hours and/or a consequent increase in sleep duration in ≥2 rounds |
7–8 hours |
132 (3.6%) |
| ≥9 hours | Remaining ≥9 hours and/or a consequent decrease in sleep duration in ≥2 rounds | 7–8 hours | 230 (6.2%) | |
| Persistent short sleepers | ≤ 6 hours | ≤ 6 hours in ≥2 rounds | ≤6 hours | 115 (3.1%) |
| Became short sleepers | 7–8 hours |
Remaining 7–8 hours and/or a consequent decrease in sleep duration in ≥2 rounds |
≤6 hours |
607 (16.4%) |
| ≥ 9 hours | Remaining ≥9 hours and/or a consequent decrease in sleep duration in ≥2 rounds | ≤6 hours | 28 (0.8%) | |
| Persistent long sleepers | ≥ 9 hours | ≥ 9 hours in ≥2 rounds | ≥9 hours | 39 (1.0%) |
| Became long sleepers | ≤ 6 hours |
Remaining ≤6 hours and/or a consequent increase in sleep duration in ≥2 rounds |
≥9 hours |
9 (0.3%) |
| 7–8 hours | Remaining 7–8 hours and/or a consequent increase in sleep duration in ≥2 rounds | ≥9 hours | 134 (3.6%) | |
| Varying sleepers | Any pattern that is not included in the patterns above because of other variations in sleep duration over time (336 [9.1%]) | |||
Sociodemographic, Lifestyle, and Health Characteristics
Self-reported and objectively measured data of the baseline and fifth round were used in this study.24 Most data were collected in a standardized way over all DCS rounds; the most relevant exceptions are described.
Sociodemographic characteristics include age, which was classified into 10-year categories. Marital status was dichotomized as married or cohabitant and other. Level of education was categorized as follows: low (intermediate secondary education or less), moderate (intermediate vocational or higher secondary education), and high (higher vocational education or university). Adults were asked for their work status (employed vs. unemployed). Only at baseline, type of job was subsequently categorized as white collar job, blue collar job, unknown job, housewife/man, and other (eg, retirement, occupational disability).26
Lifestyle characteristics include smoking status, which was classified as current smoker and nonsmoker. Alcohol consumption was dichotomized as low (≤2 glasses/day for males and ≤1 glasses/day for females) and high alcohol consumption.27 Coffee consumption was dichotomized as coffee (with caffeine) consumption and no coffee consumption. Occupational physical activity was categorized into the categories: low active (mainly sedentary occupations), moderate active (sedentary, standing, and walking occupations), high active (walking and intense physical occupations), and not applicable (in case of unemployment). At baseline, leisure-time physical activity was measured by asking adults whether they were physically active for at least 4 hours per week. In the fifth round, several items on self-reported time spent on at least moderate intensity physical activities were combined and the conventional cutoff point at 3.5 hours per week was used to dichotomize adults as physically active and physically inactive during leisure time.28 This was based on the physical activity guidelines for adults and the known overestimation of self-reported physical activity.29,30
Health characteristics include self-rated general health, which was dichotomized as good (excellent to good) and poor (moderate to poor).31 Body mass index (BMI) was assessed using objectively measured body height and body weight and was dichotomized as normal weight <25 kg/m2 and overweight/obesity ≥25 kg/m2.32 Hypertension was defined as having a systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg and/or using antihypertensive medication.19 Dyslipidemia was defined as having a total cholesterol/HDL ratio ≥6.0 and/or using cholesterol-lowering medication.33,34 Having chronic conditions was categorized as having no and having ≥1 of the following self-reported chronic conditions: cardiovascular disease, stroke, cancer, and diabetes mellitus.
Sleep Quality
At baseline, sleep quality was examined by asking adults about recent poor sleep. Questions on difficulty falling asleep, awakening during the night, difficulty falling asleep after awakening, awakening early in the morning, feeling unrested after a usual night, and needing a nap during the day were asked in the fifth round. These questions were based on elements of the Pittsburgh Sleep Quality Index.35 The answer options “seldom or never” and “now and then” were combined and defined as infrequent and the answer options “often” and “always” as frequent.
Statistical Analyses
Baseline sociodemographic factors, lifestyle factors, and health characteristics were compared across the sleep duration patterns using multinomial logistic regression analyses, with persistent moderate sleepers as the reference category. To get an indication of whether potential baseline associations persisted over time, the same analyses were repeated using fifth round characteristics. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were reported. The analyses were not adjusted for self-rated health and chronic conditions because of their expected mediating role in the examined associations. To relate the sleep duration patterns to sleep quality, chi-square tests with Bonferroni–Holm correction were performed separately for each sleep quality question and sleep duration pattern with persistent moderate sleepers as the reference category.36 The persistent long sleep duration pattern was excluded from the analyses because of the low number of adults (n = 39) with this sleep duration pattern. SAS software version 9.4 was used, and a two-sided p-value of < .05 was considered statistically significant.
RESULTS
The study population consisted of 1909 women and 1786 men aged 38.8 ± 9.6 years on average at baseline (Table 1). Adults who were excluded from our study were slightly older, lower educated, more often smoker, less healthy, less often moderate sleeper, and reported more often poor sleep quality compared to included adults.
Table 1.
Sociodemographic, Lifestyle, Health, and Sleep Characteristics at Baseline for the Total Study Population and for the Adults Who Were Excluded From Our Study.
| Characteristics | Total study population n = 3695 |
Excluded adults n = 4073* |
|---|---|---|
| Sociodemographic | ||
| Female | 1909 (51.7%) | 2219 (54.5%) |
| Age (years) | 38.8 (9.6) | 40.4 (10.9) |
| Not married or cohabitant | 534 (14.5%) | 786 (19.3%) |
| Level of education | ||
| Low | 2086 (56.5%) | 2839 (70.3%) |
| Moderate | 885 (24.0%) | 752 (18.6%) |
| High | 724 (19.6%) | 450 (11.1%) |
| Work status | ||
| Employed | ||
| White collar job | 1560 (42.2%) | 1082 (28.1%) |
| Blue collar job | 761 (20.6%) | 838 (21.7%) |
| Unknown job | 138 (3.7%) | 157 (4.1%) |
| Unemployed | ||
| Housewife/man | 954 (25.8%) | 1209 (31.4%) |
| Other | 282 (7.6%) | 571 (14.7%) |
| Lifestyle | ||
| Smoker | 1075 (29.1%) | 1733 (42.7%) |
| High alcohol consumption | 798 (21.6%) | 881 (21.6%) |
| Coffee consumer | 2949 (79.8%) | 3289 (81.2%) |
| Occupational physical activity | ||
| Low active | 706 (19.1%) | 569 (14.0%) |
| Moderate active | 1530 (41.4%) | 1631 (40.2%) |
| High active | 1199 (32.5%) | 1372 (33.7%) |
| Not applicable | 260 (7.0%) | 490 (12.1%) |
| Physically inactive during leisure-time | 1104 (29.9%) | 1396 (34.3%) |
| Health | ||
| Poor self-rated health | 814 (22.0%) | 1176 (29.2%) |
| Body mass index (kg/m2) | 24.6 (3.3) | 25.5 (4.0) |
| Hypertension | 544 (14.7%) | 963 (23.6%) |
| Dyslipidemia | 569 (15.4%) | 893 (22.0%) |
| ≥1 Chronic conditions | 72 (2.0%) | 171 (4.2%) |
| Sleep | ||
| Sleep quality | ||
| Recent poor sleep | 541 (14.6%) | 748 (18.4%) |
| Short sleepers | 292 (7.9%) | 450 (11.0%) |
| Moderate sleepers | 3067 (83.0%) | 3087 (76.0%) |
| Long sleepers | 336 (9.1%) | 527 (13.0%) |
Frequencies (percentages) for categorical variables and mean (standard deviation) for continuous variables are presented.
*This number varies per characteristic because of missing data.
Sleep Duration Over 20 Years
About 56% of the adults had persistent moderate sleep duration over 20 years (Table 2). The patterns of persistent short and persistent long sleep duration were observed in 3% and 1% of the adults, respectively. Change in sleep duration over time was observed among 40% of the adults: 17% became short sleeper, 10% became moderate sleeper, 9% was a varying sleeper, and 4% became long sleeper. Nine of these adults abruptly changed from short to long sleep duration or vice versa between two subsequent rounds.
Characteristics of Adults and Sleep Duration Patterns
Multivariable-adjusted analyses showed that adults with patterns different from persistent moderate sleep duration were more often physically inactive during leisure time (ORs [95% CIs] varied between 1.26 [1.04–1.53] and 1.58 [1.06–2.37]) and had more often poor self-rated health (ORs [95% CIs] varied between 1.50 [1.20–1.87] and 2.15 [1.48–3.12]) compared to persistent moderate sleepers (Table 3).
Table 3.
Associations of Baseline Sociodemographic, Lifestyle, and Health Characteristics With Five Sleep Duration Patterns.
| Characteristics | Became moderate sleepers (n=362) | Persistent short sleepers (n=115) | Became short sleepers (n=635) | Became long sleepers (n=143) | Varying sleepers (n=336) | Overall p-value |
|---|---|---|---|---|---|---|
| Sociodemographic | ||||||
| Female | 1.33 (1.02–1.73) | 0.56 (0.35–0.88) | 0.99 (0.80–1.22) | 0.84 (0.56–1.27) | 0.77 (0.58–1.01) | <.01 |
| Age | ||||||
| 20–29 years | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 30–39 years | 0.62 (0.44–0.87) | 2.52 (1.22–5.22) | 1.06 (0.81–1.39) | 1.50 (0.72–3.13) | 0.96 (0.67–1.38) | <.01 |
| 40–49 years | 0.80 (0.57–1.13) | 2.48 (1.17–5.25) | 0.85 (0.64–1.14) | 3.76 (1.88–7.54) | 1.00 (0.68–1.45) | <.01 |
| 50–59 years | 0.88 (0.59–1.31) | 4.23 (1.95–9.17) | 0.77 (0.54–1.08) | 5.59 (2.69–11.60) | 1.05 (0.68–1.61) | <.01 |
| Not married or cohabitant | 1.47 (1.08–2.00) | 2.63 (1.62–4.29) | 1.09 (0.83–1.44) | 1.25 (0.73–2.13) | 1.13 (0.79–1.60) | <.01 |
| Level of education | ||||||
| Low | 1,18 (0.86–1.62) | 1.41 (0.83–2.41) | 1.19 (0.92–1.52) | 1.19 (0.75–1.91) | 1.17 (0.84–1.63) | .53 |
| Moderate | 0.89 (0.62–1.29) | 1.18 (0.64–2.18) | 0.95 (0.71–1.26) | 1.19 (0.69–2.05) | 0.95 (0.65–1.39) | .93 |
| High | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Unemployed | 1.07 (0.81–1.42) | 1.48 (0.91–2.41) | 1.28 (1.02–1.60) | 1.05 (0.68–1.64) | 1.51 (1.13–2.03) | .04 |
| Work status | ||||||
| Employed | ||||||
| White collar job | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Blue collar job | 1.03 (0.73–1.45) | 0.79 (0.45–1.37) | 1.39 (1.08–1.81) | 1.33 (0.81–2.17) | 1.07 (0.76–1.50) | .13 |
| Unknown job | 2.33 (1.42–3.83) | 0.62 (0.14–2.64) | 1.00 (0.58–1.72) | 2.35 (1.06–5.05) | 1.25 (0.65–2.40) | <.01 |
| Unemployed | ||||||
| Housewife/man | 0.98 (0.70–1.38) | 1.69 (0.89–3.22) | 1.35 (1.03–1.78) | 1.01 (0.58–1.76) | 1.38 (0.96–1.99) | .11 |
| Other | 1.78 (1.18–2.70) | 1.04 (0.48–2.23) | 1.51 (1.04–2.19) | 1.80 (0.96–3.37) | 1.95 (1.26–3.00) | <.01 |
| Lifestyle | ||||||
| Smoker | 1.25 (0.97–1.60) | 0.83 (0.53–1.30) | 1.07 (0.88–1.31) | 1.29 (0.88–1.89) | 1.57 (1.22–2.01) | <.01 |
| High alcohol consumption | 1.01 (0.76–1.34) | 1.45 (0.94–2.24) | 0.99 (0.79–1.24) | 1.16 (0.78–1.74) | 0.92 (0.69–1.24) | .57 |
| Coffee consumer | 0.76 (0.58–0.99) | 1.08 (0.65–1.79) | 0.84 (0.67–1.04) | 0.79 (0.52–1.19) | 0.97 (0.72–1.31) | .24 |
| Occupational physical activity | ||||||
| Low active | 0.72 (0.50–1.04) | 0.98 (0.54–1.79) | 0.77 (0.58–1.02) | 0.82 (0.49–1.36) | 1.17 (0.83–1.67) | .17 |
| Moderate active | 1.07 (0.82–1.40) | 1.31 (0.82–2.09) | 1.10 (0.89–1.36) | 0.69 (0.46–1.05) | 1.00 (0.75–1.33) | .34 |
| High active | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Not applicable | 1.17 (0.74–1.85) | 0.95 (0.40–2.22) | 0.62 (0.41–0.95) | 1.07 (0.53–2.17) | 1.20 (0.76–1.90) | .20 |
| Physically inactive during leisure time | 1.14 (0.89–1.45) | 1.58 (1.06–2.37) | 1.26 (1.04–1.53) | 1.46 (1.01–2.11) | 1.38 (1.07–1.76) | <.01 |
| Health | ||||||
| Poor self-rated health | 2.11 (1.63–2.73) | 2.07 (1.37–3.14) | 1.50 (1.20–1.87) | 2.15 (1.48–3.12) | 1.69 (1.29–2.22) | <.01 |
| Overweight/obesity | 1.30 (1.02–1.66) | 1.03 (0.69–1.55) | 1.11 (0.91–1.35) | 0.85 (0.59–1.23) | 1.39 (1.08–1.78) | .05 |
| Hypertension | 1.24 (0.91–1.70) | 1.22 (0.75–2.01) | 1.10 (0.85–1.44) | 0.75 (0.45–1.26) | 1.16 (0.84–1.60) | .47 |
| Dyslipidemia | 1.32 (0.95–1.83) | 1.28 (0.77–2.12) | 1.13 (0.87–1.48) | 0.85 (0.52–1.38) | 0.89 (0.64–1.26) | .35 |
| ≥1 Chronic conditions | 0.92 (0.38–2.22) | 1.25 (0.37–4.19) | 1.32 (0.69–2.53) | 1.83 (0.75–4.50) | 1.35 (0.61–2.97) | .76 |
Odds ratios (95% confidence intervals) and overall p-values obtained by multinomial logistic regression analyses are presented. Reference category: persistent moderate sleepers (n = 2065). All odds ratios were adjusted for gender, age, marital status, level of education, work status, smoking status, alcohol consumption, leisure-time physical activity, and BMI at baseline. Statistically significant results are highlighted in bold (p < .05).
Gender, age, marital status, work status, smoking status, coffee consumption status, and BMI were also significantly associated with some sleep duration patterns in comparison with the persistent moderate sleep duration pattern. For example, compared to persistent moderate sleepers, those who became moderate sleepers were more often female, unmarried, overweight/obese, and coffee nonconsumers. Persistent short sleepers were more often male, 30 years or over, and unmarried. Adults who became short sleepers were more often unemployed and blue collar worker. Those who became long sleepers were more often 40 years or over at baseline. Varying sleepers were more often unemployed, smoking, and overweight/obese.
Most associations between the characteristics of adults and the sleep duration patterns were similar at baseline and the fifth round (Supplementary Table S1). With the exception that those who became long sleepers were more often unemployed than persistent moderate sleepers in the fifth round (OR [95% CI]: 5.52 [3.07–9.94]).
Sleep Quality and Sleep Duration Patterns
Sleep quality complaints were more often reported by adults who did not have a persistent moderate sleep duration pattern (Table 4). This was in particular the case for persistent short sleepers: more than half of the persistent short sleepers (51%) reported poor sleep at baseline while 11% of the persistent moderate sleepers reported poor sleep at baseline. In the fifth round, persistent short sleepers and adults who became short sleepers reported more sleep quality complaints than persistent moderate sleepers. For example, 8% of the persistent moderate sleepers reported frequent awakening early in the morning while 47% and 40% of the persistent short sleepers and those who became short sleepers frequently awaked early in the morning, respectively.
Table 4.
Distribution of Baseline and Fifth Round Self-Reported Sleep Quality Complaints for Each Sleep Duration Pattern.
| Self-reported sleep quality complaints | Persistent moderate sleepers | Became moderate sleepers | Persistent short sleepers | Became short sleepers | Became long sleepers | Varying sleepers |
|---|---|---|---|---|---|---|
| First round | ||||||
| Recent poor sleep | 217 (10.5%) | 70 (19.3%) | 59 (51.3%) | 102 (16.1%) | 28 (19.6%) | 62 (18.5%) |
| Fifth round* | ||||||
| Frequent difficulty falling asleep | 105 (5.2%) | 43 (12.0%) | 48 (42.5%) | 148 (23.9%) | 12 (8.8%) | 46 (13.9%) |
| Frequent awakening during the night | 561 (27.6%) | 112 (31.3%) | 66 (58.4%) | 321 (51.9%) | 49 (36.0%) | 116 (35.2%) |
| Frequent difficulty falling asleep after awakening | 159 (7.8%) | 41 (11.5%) | 50 (44.3%) | 197 (31.8%) | 15 (11.0%) | 50 (15.2%) |
| Frequent awakening early in the morning | 167 (8.2%) | 47 (13.1%) | 53 (46.9%) | 248 (40.1%) | 11 (8.1%) | 60 (18.2%) |
| Frequent feeling unrested after a usual night | 133 (6.6%) | 40 (11.2%) | 39 (34.5%) | 146 (23.6%) | 23 (16.9%) | 48 (14.6%) |
| Frequent needing a nap during the day | 315 (15.5%) | 70 (19.6%) | 25 (22.1%) | 127 (20.5%) | 55 (40.4%) | 77 (23.3%) |
Frequencies (percentages) are presented.
*Numbers after excluding 69 adults because of missing data on fifth round self-reported sleep quality complaints.
Reference category: persistent moderate sleepers. Statistically significant results after Bonferroni-Holm correction obtained by chi-square tests are highlighted in bold (p < .05). All overall p-values were < .01.
DISCUSSION
Main Findings
Nearly half of the adults did not have persistent moderate sleep duration over time and more than one-sixth became short sleeper. Adults with patterns different from persistent moderate sleep duration were more often physically inactive during leisure time and had more often poor self-rated health compared to persistent moderate sleepers. Sleep quality complaints occurred least often in persistent moderate sleepers and most often in persistent short sleepers and in those who became short sleepers.
Comparison with Literature
A study that examined sleep duration over 8 years found that the sleep duration of adults remained nearly stable over time.15 In contrast, our results show that a substantial part of the study population changed between short, moderate, and long sleep duration over 20 years. Particularly noteworthy is our finding that more than one-sixth of all adults became short sleeper. This decline in sleep duration might be attributable to developments in the modern 24/7 society.3 For instance, Ford et al. found in a repeated cross-sectional study a significant age-adjusted 31% increase in the number of adults sleeping ≤6 hours between 1985 and 2012.37 Over the last decades, the use of technology has increased and particularly the use of interactive technological devices is associated with sleep problems.38 Besides, in the modern 24/7 society, work schedules have become longer and include more shiftwork.2,3,17 Blue collar workers are generally more exposed to shiftwork.26 Our finding that adults who became short sleepers were more often blue collar workers than white collar workers compared to persistent moderate sleepers may reflect this change in work schedules. The decline in sleep duration might also be partly attributable to the fact that sleep duration becomes shorter with increasing age due to age-related changes in the homeostatic process that underlies sleeping and regulates the sleep–wake cycle.39,40 Due to the extended follow-up period of 20 years, our study might have been able to capture this effect of aging. Our findings certainly suggest that adult sleep duration becomes shorter with aging and that several biological processes and environmental developments may play a role, which warrant further investigation.
Our study extends the findings of Gilmour et al., who found that gender and age were associated with sleep duration patterns, by examining an extensive number of characteristics beyond gender and age.15 Of particular interest are our findings that leisure-time physical inactivity and poor self-rated health were consistently associated with nearly all patterns different from persistent moderate sleep duration. This corresponds with the results of cross-sectional studies, which have found that physical inactivity and poor self-rated health are related to both short and long sleep duration.16,21,22 Several mechanisms may explain the association between physical activity and sleep, such as increased body temperature, alteration of endocrine functions (eg, levels of melatonin), and improvement of mood.41 Poor health status might affect sleep through pain and fatigue, for example.13,40 Thus, a negative effect of physical inactivity and poor health status on long-term sleep duration patterns seems plausible.
Previous cross-sectional research has associated poor sleep quality with short and long sleep duration.16,23 Gilmour et al. found a relationship between poor sleep quality and sleep duration over time; poor sleep quality was significantly associated with a decrease in sleep duration over time.15 This is consistent with our finding that those who became short sleepers reported more sleep quality complaints compared to persistent moderate sleepers. Moreover, our study suggests that there might also be a link between poor sleep quality and the other patterns that are different from persistent moderate sleep duration.
Strengths and Limitations
A main strength of this study is its longitudinal data collection over an extended follow-up period. This provided the opportunity to study sleep duration patterns among adults over a 20-year period. Data were collected in a large sample of the adult general population with a broad age range and with response rates comparable to other cohort studies that investigated sleep duration over time.15,42 Furthermore, most associations between characteristics of adults and sleep duration patterns were similar at baseline and the fifth round, which suggests that characteristics of adults with a particular long-term sleep duration pattern remain mostly the same over time.
While interpreting the results, some limitations of the present study should be taken into account. Sleep duration was measured using a self-reported item with a limited number of fixed response categories. Although more detailed information about sleep duration at each round could not be provided, we think the categorical measure is able to distinguish between the important sleep duration categories and to classify adults into the often used categories “short,” “moderate,” and “long” sleep duration.3,5,7,25 Short and long sleep duration have been associated with adverse health status, and our study also showed that short and long sleepers had a worse sleep quality.3–9 As in most previous large-scale studies, it was not feasible to measure sleep duration objectively and in more detail.3,5 Self-reported sleep duration might represent time spent in bed instead of the actual sleeping time.9 Lauderdale et al. and Cespedes et al. showed that the degree of overestimation and the correlation between self-reported sleep and objectively measured sleep varied by personal factors.43,44 Their results suggested that personal factors, such as gender, age, and BMI may cause these variations. Therefore, differential misclassification may have affected our findings. Differences in overestimation of sleep duration by age and gender were small and not significant in the study of Lauderdale et al., but nonobese adults overestimated sleep duration by approximately 17 minutes more than obese adults.43 Consequently, nonobese adults might have been more often misclassified as relatively longer sleepers than obese adults in our study. Since such misclassification may also apply to other personal factors, part of the adults may have been wrongly classified in baseline sleep duration patterns. This may have attenuated some of the reported associations between characteristics of adults and sleep duration patterns. For the study of long-term sleep duration patterns, we now have to rely on suboptimal assessment methods. With the use of objective sleep duration measurements, such as actigraphy, we will have better data in the future.44 Compared to the Dutch adult general population, our study population was slightly higher educated and slightly healthier, which is a common feature of cohort studies.45 Adults who were excluded from our study were less often moderate sleeper and reported more often poor sleep quality compared to included adults. This selection bias may have led to an underestimation of the number of short and long sleepers in our study, which may have decreased the statistical power.
Practical Implications and Future Research
Our finding that nearly half of the adults did not have a persistent moderate sleep duration pattern over their adult life course implies a potential public health problem. Based on a single measurement, both short and long sleep duration have been associated with adverse health status, such as obesity, coronary heart disease, diabetes, depression, and all-cause mortality.3–9 These associations may even be stronger for those sleeping persistently short or long. With respect to changes in sleep duration, increasing and decreasing sleep duration have also been associated with negative health conditions (eg, cognitive dysfunction, diabetes, and mortality).10–12 Nonetheless, future research is needed to study the relationship between short- and long-term sleep duration and adverse health status, in order to provide more insight into which sleep duration patterns are most unfavorable and should be targeted with preventive interventions.15 Our results suggest that, in particular, leisure-time physical activity might be a potential target for prevention because of its modifiable nature. Future studies should investigate whether increasing physical activity benefits the course of sleep duration over a long period. Furthermore, characteristics, such as being unmarried, unemployed, overweight/obese, and having poor self-rated health may be useful to identify adults at risk for unfavorable sleep duration patterns. Besides the numerous characteristics that were investigated in our study, it is interesting to investigate family structure and mental health in future research, as these factors have previously been associated with sleep duration.42,46
CONCLUSION
This study, which used data over a 20-year period, showed that nearly half of the adults did not have persistent moderate sleep duration over time and that more than one-sixth became short sleeper. As short and long sleep duration have been associated with adverse health status, the present findings imply a potential public health problem. Several characteristics of adults were associated with patterns different from persistent moderate sleep duration, of which leisure-time physical activity is a potential important target to prevent unfavorable changes in sleep duration over the life course.
SUPPLEMENTARY MATERIAL
Supplementary material is available at SLEEP online.
INSTITUTION AT WHICH THE WORK WAS PERFORMED
National Institute for Public Health and the Environment, Bilthoven, the Netherlands.
DISCLOSURE STATEMENT
None declared.
Supplementary Material
ACKNOWLEDGEMENTS
The Doetinchem Cohort Study is funded by the National Institute for Public Health and the Environment, which works under the authority of the Ministry of Health, Welfare, and Sport of the Netherlands. The authors would like to thank the epidemiologists and fieldworkers of the Municipal Health Service in Doetinchem for their contribution to the data collection for this study.
REFERENCES
- 1. Youngstedt SD, Goff EE, Reynolds AM et al. . Has adult sleep duration declined over the last 50+ years? Sleep Med Rev. 2016; 28: 69–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kronholm E, Partonen T, Laatikainen T et al. . Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: a comparative review and re-analysis of Finnish population samples. J Sleep Res. 2008; 17(1): 54–62. [DOI] [PubMed] [Google Scholar]
- 3. Ferrie JE, Kumari M, Salo P, Singh-Manoux A, Kivimäki M. Sleep epidemiology—a rapidly growing field. Int J Epidemiol. 2011; 40(6): 1431–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010; 71(5): 1027–1036. [DOI] [PubMed] [Google Scholar]
- 5. Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011; 32(12): 1484–1492. [DOI] [PubMed] [Google Scholar]
- 6. Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 2015; 32(9): 664–670. [DOI] [PubMed] [Google Scholar]
- 7. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010; 33(5): 585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rechtschaffen A, Bergmann BM, Everson CA, Kushida CA, Gilliland MA. Sleep deprivation in the rat: X. Integration and discussion of the findings. Sleep. 1989; 12(1): 68–87. [PubMed] [Google Scholar]
- 9. Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. 2011; 34(11): 1487–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cespedes EM, Bhupathiraju SN, Li Y, Rosner B, Redline S, Hu FB. Long-term changes in sleep duration, energy balance and risk of type 2 diabetes. Diabetologia. 2016; 59(1): 101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ferrie JE, Shipley MJ, Cappuccio FP et al. . A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007; 30(12): 1659–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ferrie JE, Shipley MJ, Akbaraly TN, Marmot MG, Kivimäki M, Singh-Manoux A. Change in sleep duration and cognitive function: findings from the Whitehall II study. Sleep. 2011; 34(5): 565–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stranges S, Dorn JM, Shipley MJ et al. . Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008; 168(12): 1353–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hayley AC, Skogen JC, Øverland S et al. . Trajectories and stability of self-reported short sleep duration from adolescence to adulthood. J Sleep Res. 2015; 24(6): 621–628. [DOI] [PubMed] [Google Scholar]
- 15. Gilmour H, Stranges S, Kaplan M et al. . Longitudinal trajectories of sleep duration in the general population. Health Rep. 2013; 24(11): 14–20. [PubMed] [Google Scholar]
- 16. Kronholm E, Härmä M, Hublin C, Aro AR, Partonen T. Self-reported sleep duration in Finnish general population. J Sleep Res. 2006; 15(3): 276–290. [DOI] [PubMed] [Google Scholar]
- 17. Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010; 33(1): 37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009; 169(9): 1052–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014; 15(1): 42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shilo L, Sabbah H, Hadari R et al. . The effects of coffee consumption on sleep and melatonin secretion. Sleep Med. 2002; 3(3): 271–273. [DOI] [PubMed] [Google Scholar]
- 21. Ohayon MM. Interactions between sleep normative data and sociocultural characteristics in the elderly. J Psychosom Res. 2004; 56(5): 479–486. [DOI] [PubMed] [Google Scholar]
- 22. Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med. 2011; 12(4): 346–350. [DOI] [PubMed] [Google Scholar]
- 23. Mesas AE, López-García E, León-Muñoz LM, Graciani A, Guallar-Castillón P, Rodríguez-Artalejo F. The association between habitual sleep duration and sleep quality in older adults according to health status. Age Ageing. 2011; 40(3): 318–323. [DOI] [PubMed] [Google Scholar]
- 24. Verschuren WM, Blokstra A, Picavet HS, Smit HA. Cohort profile: the Doetinchem cohort study. Int J Epidemiol. 2008; 37(6): 1236–1241. [DOI] [PubMed] [Google Scholar]
- 25. Watson NF, Badr S, Belenky G et al. . Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015; 11(6): 591–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ilo.org. International Standard Classification of Occupations http://www.ilo.org/public/english/bureau/stat/isco/isco88/index.htm. Accessed March 24, 2016.
- 27. Health.gov. 2015–2020 Dietary Guidelines for Americans http://health.gov/dietaryguidelines/2015/guidelines/appendix-9/. Accessed April 1, 2016.
- 28. Picavet HS, Wendel-vos GC, Vreeken HL, Schuit AJ, Verschuren WM. How stable are physical activity habits among adults? The Doetinchem Cohort Study. Med Sci Sports Exerc. 2011; 43(1): 74–79. [DOI] [PubMed] [Google Scholar]
- 29. Who.int. Global Strategy on Diet, Physical Activity and Health: recommended levels of physical activity for adults aged 18–64 years http://www.who.int/dietphysicalactivity/factsheet_adults/en/. Accessed April 1, 2016.
- 30. Wilcox S, King AC. Self-favoring bias for physical activity in middle-aged and older adults. J Appl Soc Psychol. 2000; 30(9): 1773–1789. [Google Scholar]
- 31. DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006; 21(3): 267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Who.int. Body mass index http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed March 24, 2016.
- 33. Hulsegge G, Smit HA, van der Schouw YT, Daviglus ML, Verschuren WM. Quantifying the benefits of achieving or maintaining long-term low risk profile for cardiovascular disease: The Doetinchem Cohort Study. Eur J Prev Cardiol. 2015; 22(10): 1307–1316. [DOI] [PubMed] [Google Scholar]
- 34. Claudi T, Midthjell K, Holmen J, Fougner K, Krüger O, Wiseth R. Cardiovascular disease and risk factors in persons with type 2 diabetes diagnosed in a large population screening: the Nord-Trøndelag Diabetes Study, Norway. J Intern Med. 2000; 248(6): 492–500. [DOI] [PubMed] [Google Scholar]
- 35. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2): 193–213. [DOI] [PubMed] [Google Scholar]
- 36. Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979; 6(2): 65–70. [Google Scholar]
- 37. Ford ES, Cunningham TJ, Croft JB. Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep. 2015; 38(5): 829–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, Czeisler CA. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. J Clin Sleep Med. 2013; 9(12): 1291–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004; 27(7): 1255–1273. [DOI] [PubMed] [Google Scholar]
- 40. Pandi-Perumal SR, Seils LK, Kayumov L et al. . Senescence, sleep, and circadian rhythms. Ageing Res Rev. 2002; 1(3): 559–604. [DOI] [PubMed] [Google Scholar]
- 41. Chennaoui M, Arnal PJ, Sauvet F, Léger D. Sleep and exercise: a reciprocal issue? Sleep Med Rev. 2015; 20: 59–72. [DOI] [PubMed] [Google Scholar]
- 42. Hagen EW, Mirer AG, Palta M, Peppard PE. The sleep-time cost of parenting: sleep duration and sleepiness among employed parents in the Wisconsin Sleep Cohort Study. Am J Epidemiol. 2013; 177(5): 394–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Sleep duration: how well do self-reports reflect objective measures? The CARDIA sleep study. Epidemiology. 2008; 19(6): 838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cespedes EM, Hu FB, Redline S et al. . Comparison of self-reported sleep duration with actigraphy: results from the hispanic community health study/study of latinos sueño ancillary study. Am J Epidemiol. 2016; 183(6): 561–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Van Loon AJ, Tijhuis M, Picavet HS, Surtees PG, Ormel J. Survey non-response in the Netherlands: effects on prevalence estimates and associations. Ann Epidemiol. 2003; 13(2): 105–110. [DOI] [PubMed] [Google Scholar]
- 46. Luca A, Luca M, Calandra C. Sleep disorders and depression: brief review of the literature, case report, and nonpharmacologic interventions for depression. Clin Interv Aging. 2013; 8: 1033–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.