Abstract
Background:
Accurate skeletal maturity assessment is important to guide clinical evaluation of idiopathic scoliosis, but commonly used methods are inadequate or too complex for rapid clinical use. The objective of the study was to propose a new simplified staging method, called the thumb ossification composite index (TOCI), based on the ossification pattern of the 2 thumb epiphyses and the adductor sesamoid bone; to determine its accuracy in predicting skeletal maturation when compared with the Sanders simplified skeletal maturity system (SSMS); and to validate its interrater and intrarater reliability.
Methods:
Hand radiographs of 125 girls, acquired when they were newly diagnosed with idiopathic scoliosis prior to menarche and during longitudinal follow-up until skeletal maturity (a minimum of 4 years), were scored with the TOCI and SSMS. These scores were compared with digital skeletal age (DSA) and radius, ulna, and small hand bones (RUS) scores; anthropometric data; peak height velocity; and growth-remaining profiles. Correlations were analyzed with the chi-square test, Spearman and Cramer V correlation methods, and receiver operating characteristic curve analysis. Reliability analysis using the intraclass correlation (ICC) was conducted.
Results:
Six hundred and forty-five hand radiographs (average, 5 of each girl) were scored. The TOCI staging system was highly correlated with the DSA and RUS scores (r = 0.93 and 0.92, p < 0.01). The mean peak height velocity (and standard deviation) was 7.43 ± 1.45 cm/yr and occurred at a mean age of 11.9 ± 0.86 years, with 70.1% and 51.4% of the subjects attaining their peak height velocity at TOCI stage 5 and SSMS stage 3, respectively. The 2 systems predicted peak height velocity with comparable accuracy, with a strong Cramer V association (0.526 and 0.466, respectively; p < 0.01) and similar sensitivity and specificity on receiver operating characteristic curve analysis. The mean age at menarche was 12.57 ± 1.12 years, with menarche occurring over several stages in both the TOCI and the SSMS. The growth remaining predicted by TOCI stage 8 matched well with that predicted by SSMS stage 7, with a mean of <2 cm/yr of growth potential over a mean of <1.7 years at these stages. The TOCI also demonstrated excellent reliability, with an overall ICC of >0.97.
Conclusions:
The new proposed TOCI could provide a simplified staging system for the assessment of skeletal maturity of subjects with idiopathic scoliosis. The index needs to be subjected to further multicenter validation in different ethnic groups.
Accurate skeletal maturity assessment is important for prediction of curve progression and clinical management of idiopathic scoliosis, including bracing decisions and counseling about prognosis. Determination of the timing of peak height velocity and growth remaining is of paramount importance for these purposes1-5. However, commonly used clinical or radiographic methods are inadequate or too complex for rapid application in a busy clinic setting6,7.
Sanders et al.6 demonstrated that the Tanner-Whitehouse-3 (TW3)8 radius, ulna, and small bones of the hand (RUS) scores had the highest correlation with the curve acceleration phase among all skeletal maturity parameters in idiopathic scoliosis. The scoring system is, however, time-consuming and requires the use of an atlas with a substantial learning curve3,4,6,7. Sanders et al. simplified the RUS score into a digital skeletal age (DSA) score, by excluding the scoring of the distal aspect of the radius and the ulnar epiphysis, and confirmed that the DSA score had excellent correlation with the curve acceleration phase as well6.
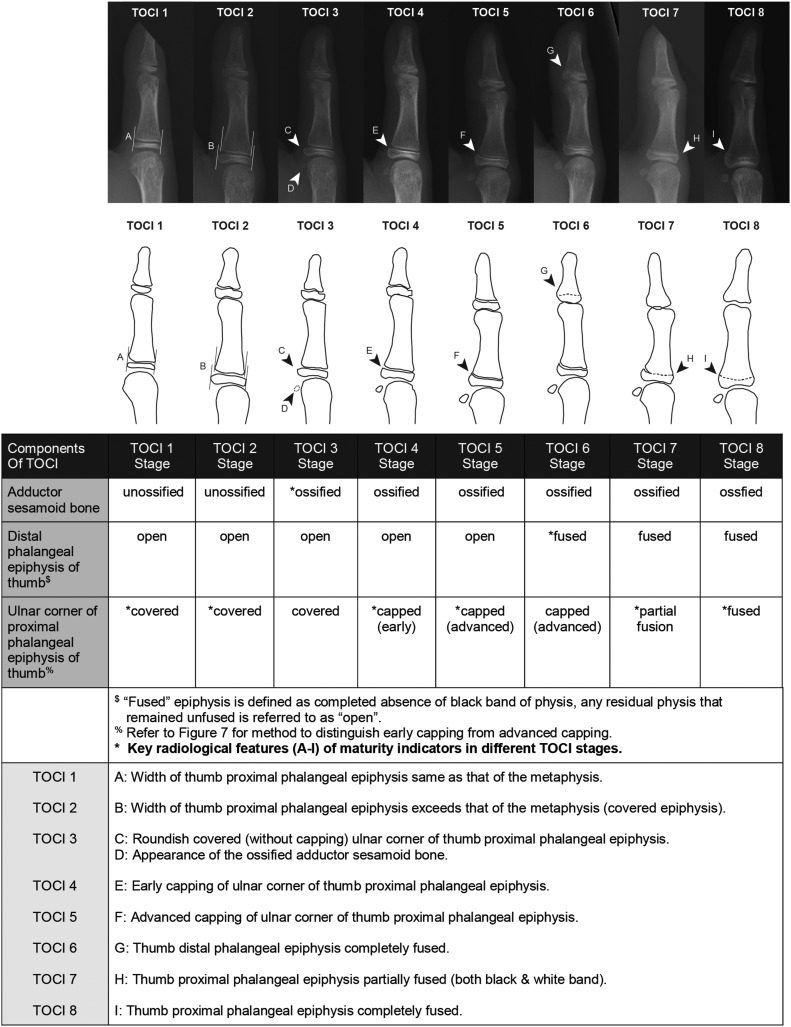
An ideal skeletal maturity assessment system would be simple and reliable with good predictability of peak height velocity and correlation with the standard DSA scoring system. We attempted to further simplify the current skeletal maturity staging system by focusing on the morphology of a minimum number of essential hand ossification centers that we hoped would reliably predict the skeletal maturity information from the whole hand in a quicker and easier manner. Previous studies8,9 had revealed that the epiphyses of the distal and proximal phalanges of the thumb demonstrated radiographic changes that were similar to those of the epiphyses of the ulnar 4 digits during the pubertal period. The adductor sesamoid has also been extensively used to predict pubertal onset for decision-making regarding maxillofacial surgery9-12. After conducting a validation study and confirming the very high concordance rate (71.3%) between TW staging of the thumb epiphyses and that of the ulnar 4 digital epiphyses13, we developed a new thumb classification based on the epiphyses of the distal and proximal phalanges together with the adductor sesamoid bone, which we call the “thumb ossification composite index (TOCI)” (Fig. 1). We hypothesized that this new simpler staging system could reliably predict when skeletal maturity would be reached by a subject in the early peripubertal period.
Fig. 1.
TOCI stages 1 through 8 and the corresponding ossification pattern and sequence of the adductor sesamoid, distal phalangeal epiphysis, and proximal phalangeal epiphysis.
The objective of this study was to compare the TOCI with a current simplified system for prediction of skeletal maturity and validate its interrater and intrarater reliability.
Materials and Methods
Hand radiographs were prospectively collected from a longitudinal cohort of girls with clinically and radiographically confirmed idiopathic scoliosis recruited from a scoliosis clinic in a tertiary hospital. The inclusion criteria were (1) female sex, (2) premenarche, (3) an age of 8 to 12 years at the time of entry into the study, (4) a diagnosis of idiopathic scoliosis, (5) no clinical evidence of neurological abnormality, (6) no abnormalities of skeletal maturation, (7) a Risser sign of zero with open physes in the hand, and (8) completion of at least 6 follow-up visits over a minimum of 4 years. Demographic variables that were collected included the ages when the radiographs were made, standing height, sitting height, body weight, and arm span. Institutional review board approval was obtained (ethics approval reference number 2016.045).
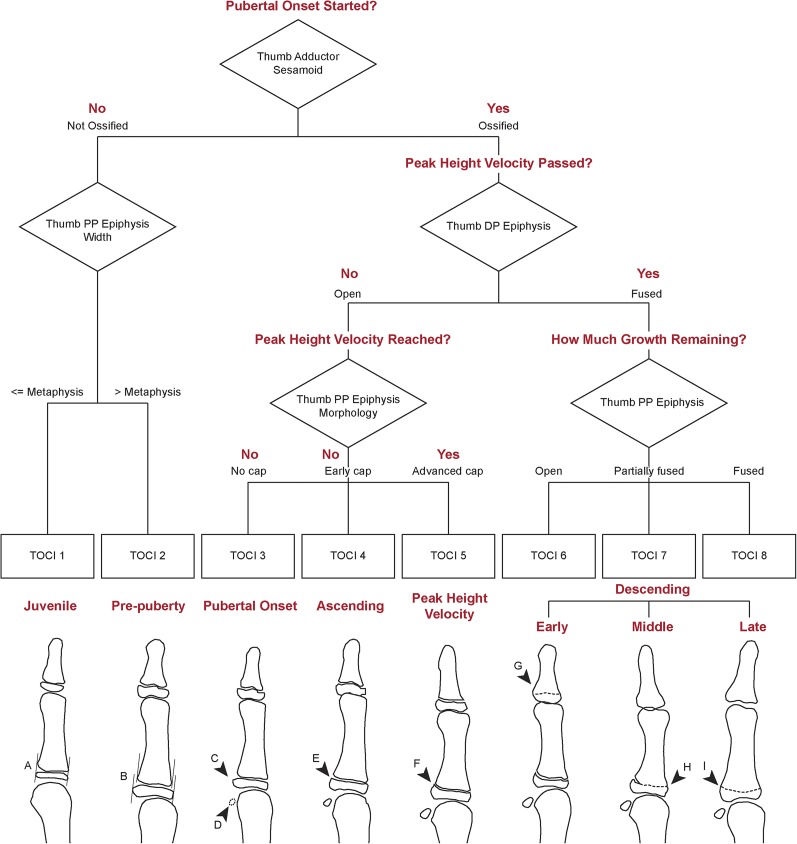
All patients were followed at an average of 6-month intervals starting prior to menarche, with more frequent visits during the early peripubertal growth period to capture accurately the timing of peak height velocity, until skeletal maturity was confirmed by the radiographic appearance of physeal closure of the distal radial epiphysis. In accordance with the original TW3 protocol, posteroanterior radiographs of the left hand were obtained at each visit8. All hand and wrist radiographs were independently reviewed by the principal author and another experienced orthopaedic clinical fellow to establish the stage of skeletal maturity according to (1) the proposed TOCI method algorithm based on the 2 thumb epiphyses and the adductor sesamoid (Fig. 2) and (2) the standard TW method based on the epiphyses of the small bones (distal phalanx, middle phalanx, proximal phalanx, and metacarpal) of the first, third, and fifth digits as well as the radial and ulnar epiphyses. Both investigators were blinded to the chronological age and identity of the patients. The TW stages (E through I) and TOCI stages (1 through 8) were recorded on separate data sheets, which were then collected by a third independent coinvestigator for subsequent analysis. TW-derived RUS and DSA scores were calculated. The Sanders simplified skeletal maturity scoring system (SSMS)4 was included for comparison to determine the accuracy of TOCI staging in predicting the timing of peak height velocity and menarche. Peak height velocity was calculated using the minimum 6-month interval method8,14,15. To define the accuracy in predicting the final growth remaining, the magnitude, time interval, and velocity of the growth occurring after the final TOCI stage (8) were compared with those parameters following a similar SSMS stage (7). All TOCI and SSMS scores were tabulated against the chronological age when the score was obtained and at menarche as well as peak height velocity.
Fig. 2.
Algorithm for TOCI staging. The words in red refer to the clinical decision-making algorithm. PP = proximal phalangeal and DP = distal phalangeal. Also see the short training video on TOCI staging included with this article.
Reliability Test
The principal investigator scored all radiographs using the TOCI method, and another investigator, who was not involved in the study, grouped the radiographs by stage across the whole TOCI spectrum (stages 1 through 8). Nine radiographs were then selected randomly from each TOCI stage, to ensure an equal distribution of test radiographs demonstrating each stage, resulting in 63 radiographs for testing (none were stage 1). One clinical fellow, 2 orthopaedic residents, and 3 non-medical assistants were invited to serve as novices for reliability testing.
An interactive training session (see the instructional video on TOCI staging included with this article [Video 1]) was provided to all 6 reviewers to give the details of the TOCI. For the reliability testing, the reviewers were instructed to view the radiographs on a high-resolution computer monitor and were allowed to refer to the reference materials (Fig. 2). All reviewers were blinded to the chronological age of the patients and performed the ratings independently with no time limit. After 4 weeks, all reviewers repeated the ratings using the same set of radiographs.
Statistical Analysis
Descriptive statistics and Spearman correlation coefficients were calculated for the DSA and RUS scores in comparison with the TOCI staging system. Charts were created to determine the timing of menarche and peak height velocity at different maturity stages in the TOCI and SSMS systems. The chi-square test and Cramer V correlation were used to evaluate the accuracy of the 2 systems in predicting the peak height velocity. The area under the receiver operating characteristic curve was also used to determine the cutoff stages in the 2 systems with the best sensitivity and specificity (highest percentages) to predict peak height velocity. Reliability analysis was tested with Cronbach alpha values. Intraclass correlations (ICCs) in different kinds of comparisons were carried out. The statistical analyses were done with SPSS version-20.0 software (IBM). The significance level was p < 0.05.
Results
In a 5-year period (2007 through 2011), 645 hand and wrist radiographs were collected consecutively from 125 premenarchal girls with adolescent idiopathic scoliosis followed longitudinally until skeletal maturity, so that the patients had an average of 5 follow-up radiographs each. The mean ages (and standard deviations [SDs]) when the first and last radiographs available for analysis were made were 10.9 ± 0.8 and 13.7 ± 1.0 years, respectively. The last radiograph was defined as the earliest radiograph that demonstrated TOCI stage 8. None of the patients in our cohort had TOCI stage 1.
Correlation of TOCI Staging with SSMS System
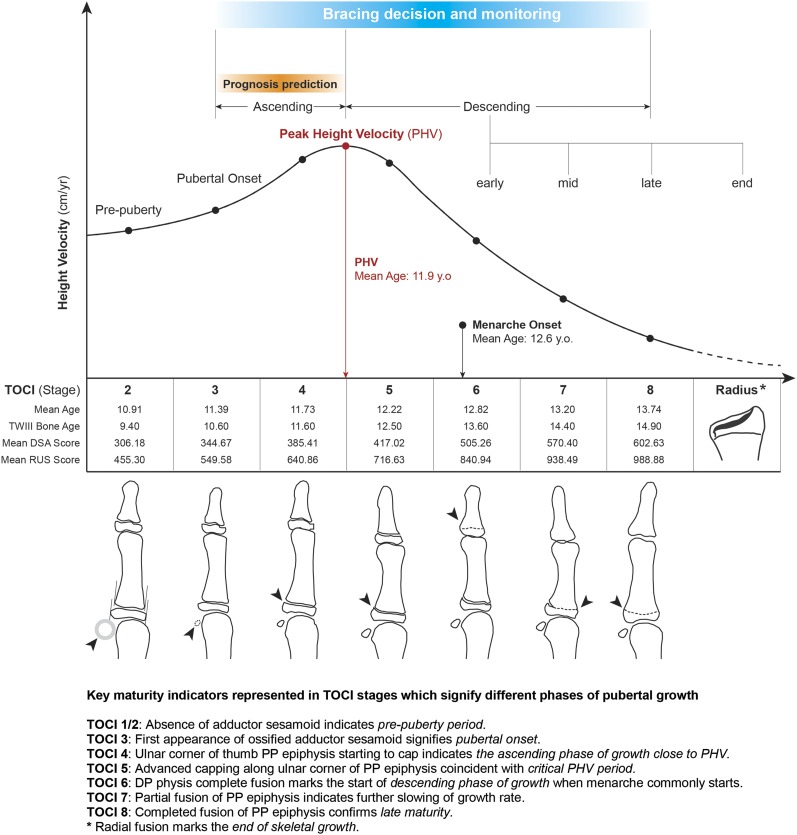
The TOCI stages were found to correlate strongly with both the DSA (r = 0.93, p < 0.01) and the RUS (r = 0.92, p < 0.01) score. The correlations of the TOCI and SSMS stages with chronological age and the DSA and RUS scores are shown in Table I and summarized in the integrated growth chart in Figure 3.
Fig. 3.
Integrated pubertal growth chart showing the crucial phases in the peripubertal growth period until skeletal maturity matched with the corresponding TOCI stages, mean DSA and RUS scores, and chronological and bone ages. PHV = peak height velocity, PP = proximal phalangeal, and DP = distal phalangeal.
TABLE I.
Correlation of TOCI and SSMS Stages with Chronological Age and DSA and RUS Scores
| Age (yr) |
DSA Scores |
RUS Scores |
|||||||
| Mean (SD) | Median | Range | Mean (SD) | Median | Range | Mean (SD) | Median | Range | |
| TOCI stage | |||||||||
| 2 | 10.9 (0.8) | 10.7 | 10.2-12.6 | 306.2 (49.7) | 332.0 | 221.0-363.0 | 455.3 (70.7) | 469.0 | 332.0-573.0 |
| 3 | 11.4 (0.7) | 11.1 | 10.6-13.3 | 344.7 (34.5) | 353.5 | 293.0-397.0 | 549.6 (76.9) | 556.0 | 441.0-683.0 |
| 4 | 11.7 (0.8) | 11.6 | 10.1-13.8 | 385.4 (27.9) | 390.5 | 293.0-429.0 | 640.9 (50.0) | 641.0 | 481.0-748.0 |
| 5 | 12.2 (0.9) | 12.1 | 10.1-15.0 | 417.0 (30.9) | 415.0 | 351.0-542.0 | 716.6 (52.8) | 706.0 | 608.0-857.0 |
| 6 | 12.8 (0.9) | 12.8 | 10.5-15.5 | 505.3 (42.5) | 508.0 | 392.0-571.0 | 840.9 (69.8) | 836.5 | 562.0-962.0 |
| 7 | 13.2 (0.9) | 13.2 | 11.1-16.0 | 570.4 (21.7) | 571.0 | 513.0-609.0 | 938.5 (44.0) | 947.0 | 786.0-1,000.0 |
| 8 | 13.7 (1.0) | 13.8 | 11.6-16.4 | 602.6 (12.5) | 609.0 | 540.0-609.0 | 988.9 (21.5) | 1,000.0 | 909.0-1,000.0 |
| SSMS stage | |||||||||
| 1 | 11.0 (0.9) | 10.5 | 10.2-12.6 | 300.9 (61.9) | 341.0 | 221.0-363.0 | 466.5 (74.2) | 465.5 | 380.0-573.0 |
| 2 | 11.7 (0.8) | 11.6 | 10.2-13.8 | 376.4 (36.2) | 374.0 | 293.0-450.0 | 625.8 (83.6) | 641.0 | 332.0-761.0 |
| 3 | 12.3 (1.0) | 12.3 | 10.1-15.5 | 413.3 (23.2) | 415.0 | 351.0-514.0 | 715.3 (52.6) | 705.5 | 613.0-905.0 |
| 4 | 12.6 (1.0) | 12.6 | 10.9-16.0 | 472.5 (42.2) | 466.0 | 401.0-562.0 | 790.7 (67.3) | 791.0 | 668.0-953.0 |
| 5 | 13.0 (0.8) | 12.9 | 11.0-15.0 | 524.5 (29.0) | 527.0 | 466.0-568.0 | 865.0 (76.1) | 876.5 | 556.0-954.0 |
| 6 | 13.2 (1.0) | 13.3 | 10.5-15.9 | 568.6 (31.6) | 567.0 | 453.0-609.0 | 934.0 (60.0) | 948.0 | 731.0-1,000.0 |
| 7 | 13.5 (0.9) | 13.5 | 11.6-14.9 | 600.7 (19.1) | 609.0 | 502.0-609.0 | 987.8 (31.5) | 1,000.0 | 784.0-1,000.0 |
Comparison of TOCI and SSMS Staging of Key Growth Parameters
Timing of Peak Height Velocity
One hundred and seven patients with clearly identifiable growth peaks were used for this analysis. The mean peak height velocity was 7.43 ± 1.45 cm/yr (range, 5 to 11.95 cm/yr) and occurred at mean age of 11.93 ± 0.86 years (range, 9.73 to 13.99 years).
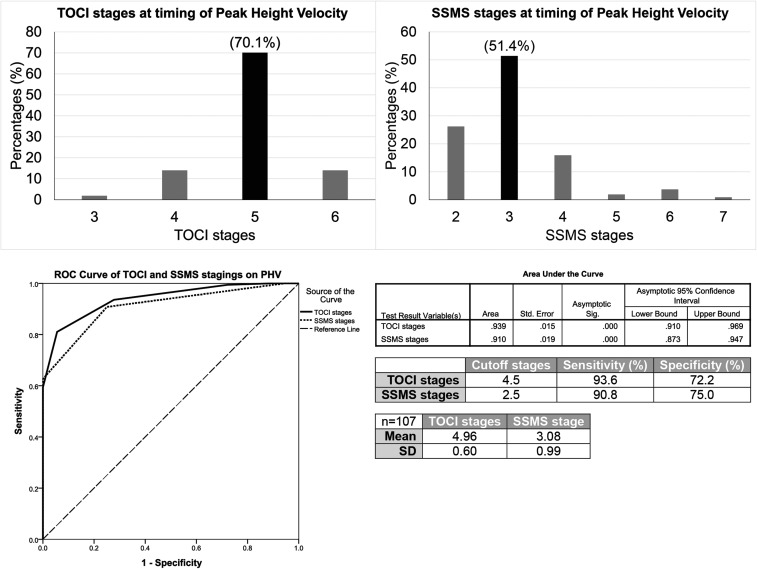
Both the TOCI and the SSMS stages were strongly associated with the peak height velocity as confirmed by strong Cramer V correlations (0.526 and 0.466, respectively), with statistical significance (p < 0.01).
As shown in Figure 4, 70.1% and 51.4% of the subjects attained their peak height velocity at TOCI stage 5 ± 0.60 and SSMS stage 3 ± 0.99, respectively, both with a median DSA score of 415.
Fig. 4.
Comparison of descriptive statistics, percentage distributions, and results of receiver operating characteristic (ROC) curve analysis of the TOCI and SSMS to determine the timing of peak height velocity (PHV).
The analysis of the area under the receiver operating characteristic curve indicated that the cutoff stages that predicted the timing of peak height velocity with the best sensitivity and specificity were TOCI stage 4.5, with a sensitivity of 93.6% and a specificity of 72.2%, and SSMS stage 2.5, with a sensitivity of 90.8% and a specificity of 75.0%.
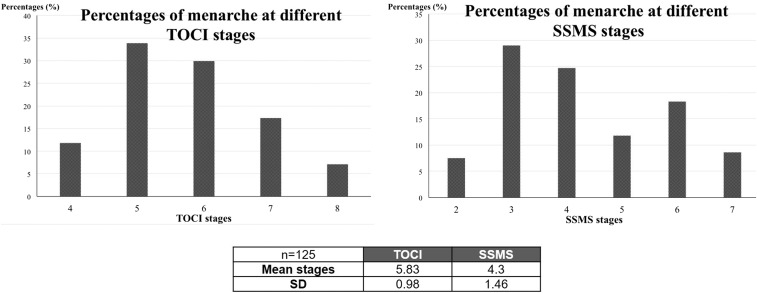
Timing of Menarche
The mean age at menarche was 12.57 ± 1.12 years (range, 9.4 to 14.3 years), and menarche was found to occur over several stages in both the TOCI and the SSMS (Fig. 5).
Fig. 5.
Percentage distribution of menarche occurring at different TOCI and SSMS stages.
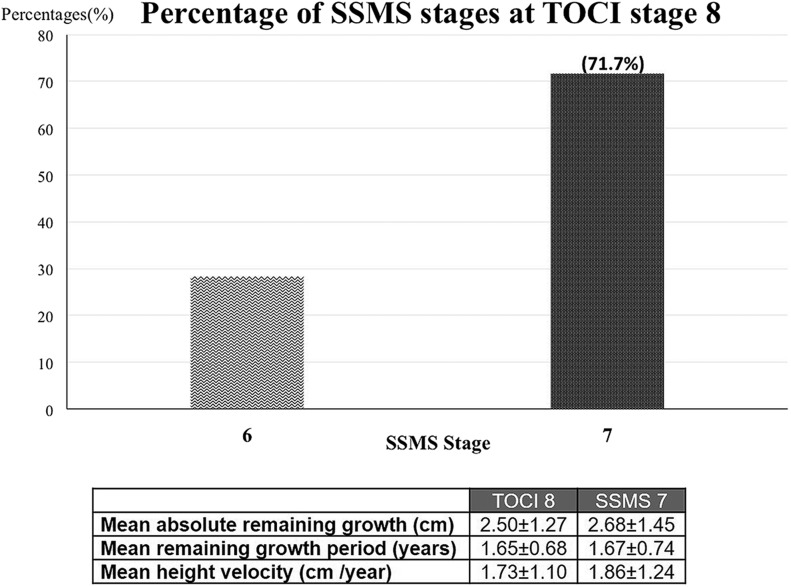
Growth-Remaining Profile
We found that 71.7% of the subjects at TOCI stage 8 were at SSMS stage 7. The median DSA score at both stages was 609. Overall, the mean amount of final growth remaining at these 2 stages was <2 cm/yr over <1.7 years. The growth-remaining profiles are summarized in Figure 6.
Fig. 6.
The percentage of patients at SSMS stage 7 who were at TOCI stage 8 and the growth-remaining profiles at SSMS stage 7 and TOCI stage 8.
Reliability Test
All 6 clinical professionals showed excellent interrater and intrarater agreement for the TOCI classification (Table II).
TABLE II.
Interrater and Intrarater Reliability Test Results for Orthopaedic Surgeons and Non-Medical Assistants*
| Junior Orthopaedic Surgeons | Non-Medical Assistants | |
| Interrater | ||
| First phase | 0.976 (0.961-0.986) | 0.985 (0.975-0.992) |
| Second phase, 4 wk later | 0.990 (0.984-0.994) | 0.988 (0.980-0.994) |
| Intrarater, first phase versus second phase | 0.995 (0.992-0.997) | 0.989 (0.981-0.994) |
The values are given as the reliability with the 95% confidence interval in parentheses.
Discussion
An ideal bone maturity assessment model should be both simple and reliable for clinical usage, with good correlation to a standard scoring system. The excellent reliability of the TOCI demonstrated that it is easy to learn, with a relatively short learning curve even among novice users. More importantly, it also has excellent correlation with DSA and RUS scores.
Sanders et al. proposed an important simplified skeletal maturity scoring system4 (SSMS) with 8 stages based on the ossification patterns of all digital epiphyses of the hand and using the same descriptors as utilized in the TW3 system. They reported that the SSMS had excellent correlation with the curve acceleration phase (r = 0.9) in 22 female subjects and excellent reliability among senior orthopaedic surgeons4. However, a subsequent validation study of 275 patients demonstrated a steep learning curve for less experienced users16. Other recently reported simplified models using the olecranon apophysis17 or the distal part of the radius and the ulnar epiphysis3 (DRU classification) were either not evaluated in strictly conducted longitudinal studies or not fully validated through comparison with the standard DSA and RUS scoring systems. The modified Risser grading system had low specificity and interobserver reliability18.
As is the case for the existing systems3,4,9,17, any proposed simplified system must be able to accurately predict the timing of peak height velocity and menarche as well as the growth-remaining period to inform the clinical decision regarding bracing and prognostic counseling about curve progression.
The mean age at peak height velocity (11.93 ± 0.86 years) in our study was comparable with that in most previous studies3,6,14,17,19. The growth velocity magnitude was similar to that in Asian studies3,19 and less than that in European17 and U.S. studies6,14. The age at peak height velocity in our study of subjects with idiopathic scoliosis was delayed (by a mean of 1.47 years) compared with that of normal subjects20,21, signifying a longer period of peripubertal growth, which may have an effect on curve progression. Radiographically, the preponderance of capping of the epiphyses of the distal and middle phalanges (of the ulnar 4 digits) and of the proximal phalanges and metacarpal bones (of all 5 digits) at SSMS stage 3 was found to best represent the timing of peak height velocity4,5. This stage corresponds well to stage 5 in our TOCI classification. The median DSA score at TOCI stage 5 was 415 (Table I), which coincides exactly with the reported critical DSA range of 400 to 425 (SSMS stage 3) that best matched with the timing of the peak height velocity and onset of the curve acceleration phase6. Our results showed that TOCI stage 5 had good accuracy for predicting peak height velocity compared with SSMS stage 3, as demonstrated by a better Cramer V association (0.526 versus 0.466), a narrower standard deviation (0.60 compared with 0.99), and similar sensitivity and specificity on receiver operating characteristic curve analysis (Fig. 4). More importantly, it is simpler to use TOCI stage 5 for this purpose as one only needs to pay attention to advanced capping over the ulnar corner of the proximal phalangeal epiphysis in the thumb.
The mean age at menarche onset in our study was 12.6 years, which was 8 months later than the mean age at peak height velocity (11.9 years), and menarche consistently occurred between the median ages at TOCI stages 5 and 6, representing the early descending phase of the growth curve. The wide range of menarche age in this series (9.4 to 14.3 years) indicated its limitation in accurately predicting remaining growth. This finding echoed the observations by Charles et al.17 and Little et al.14 and was similar to that in a study of 2,196 Chinese girls with adolescent idiopathic scoliosis22. As the onset of menarche is affected by multiple factors of growth, and because of the age spread and considerable overlapping with the timing of peak height velocity, menarche could not be matched with a single representative stage in either the SSMS or TOCI system (Fig. 5). In our series, 33.9% of the subjects had the onset of menarche at the TOCI stage at which peak height velocity occurred (TOCI stage 5), 54.3% had it after that stage (menarche began at stage 6, 7, or 8), and 11.8% had it before that stage (menarche began at stage 4). This pattern is similar to that reported in longitudinal studies by Little et al.14, Tanner8, and Buckler15.
The growth-remaining prediction refers to the more advanced TOCI stages (6, 7, and 8), matched with the descending phase of pubertal growth (Fig. 3). TOCI stage 8 (completed fusion of the proximal phalangeal epiphysis of the thumb) is equivalent to SSMS stage 7 (completed fusion of all digital epiphyses) as evidenced by 71.7% concordance between these 2 systems and their comparable final growth-remaining profiles (Fig. 6). Radiographically, both the TOCI and the SSMS still rely on distal radial epiphyseal fusion status to determine the end of growth, although it is controversial whether clinically relevant growth is still possible at the late radiographic stages of fusion of the distal radial physis16. The SSMS may provide more clarity about growth remaining at this stage since it shows the distal radial physis.
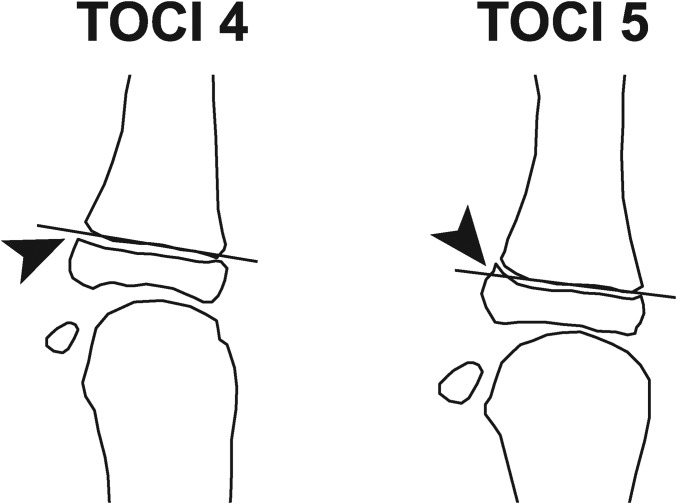
The concept of using only the thumb distal phalanx, proximal phalanx, and adductor sesamoid to predict skeletal maturity is novel but derived from precedent. The distal and proximal phalangeal epiphyses of the thumb have been used in traditional methods for determining orthopaedic bone age (e.g., the Greulich and Pyle atlas23 and the TW3 method8). The adductor sesamoid is known to be always present in adolescents24, is easily detectable, and has been extensively used to estimate skeletal maturity in orthodontic surgery (by determining the onset of puberty, it is possible to predict facial growth and the timing for mandibular reconstruction10-12). In addition, the pronated position of the thumb proximal phalanx relative to the orientation of the 4 ulnar digits provides easier visualization of the capping of the epiphysis at a very early stage. The relatively large black “cartilage gap” allows further separation into early and advanced capping stages through the use of a reference line (Fig. 7). The thumb adductor sesamoid allows extra precision in predicting the onset of puberty9-12. The composite index score of the 2 thumb epiphyses and the adductor sesamoid corresponds well to different stages of pubertal growth curve as summarized in the integrated growth chart in Figure 3. Most importantly, because the thumb epiphyses and the adductor sesamoid are located so close to each other, they can be easily imaged with a magnified view through the use of a very low-radiation mini-mobile x-ray machine in the clinic.
Fig. 7.
Illustration of “early capping” of the proximal phalangeal epiphysis at TOCI stage 4 compared with “advanced capping” at TOCI stage 5. A reference line is drawn along the most distal osseous subchondral border of the proximal phalangeal metaphysis. “Early capping” is defined when the “capping” at the ulnar corner is below this reference line (left arrowhead), and “advanced capping” is defined when it touches or extends distal to this reference line (right arrowhead).
To our knowledge, this is the first study to investigate the use of the thumb epiphyses to predict skeletal maturity in subjects with idiopathic scoliosis and to validate the method with a large number of longitudinal hand radiographs made before menarche and at an average of 6-month intervals in the peripubertal period. We believe that the newly proposed thumb ossification composite index (TOCI) was shown to be simple to use and to have excellent reliability and accuracy in the prediction of skeletal maturity comparable with the Sanders SSMS. It has the potential for application in a busy clinic setting. Further validation in larger multicenter studies involving different ethnic groups, males, longitudinal correlation with normal adolescents at different time points, and curve progression profiles are ongoing.
Acknowledgments
Note: The authors thank Mr. Patrick Tsang for retrieval of information from the scoliosis database, Ms. Vivian Hung for technical support in the reliability testing material, Prof. Ben Yip for advice regarding the methodology design of the reliability tests, Dr. Ronald Wong for dubbing the TOCI short training video, and Ms. Huang Xueying for production and aftereffect of the TOCI short training video.
Footnotes
Investigation performed at Prince of Wales Hospital, Shatin, Hong Kong
Disclosure: There was no outside funding source for this study. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/E323).
References
- 1.Nachemson AL, Lonstein JE, Weinstein SL, editors. Report of the Prevalence and Natural History Committee of the Scoliosis Research Society; Denver; 1982. [Google Scholar]
- 2.Song KM, Little DG. Peak height velocity as a maturity indicator for males with idiopathic scoliosis. J Pediatr Orthop. 2000. May-Jun;20(3):286-8. [PubMed] [Google Scholar]
- 3.Luk KDK, Saw LB, Grozman S, Cheung KMC, Samartzis D. Assessment of skeletal maturity in scoliosis patients to determine clinical management: a new classification scheme using distal radius and ulna radiographs. Spine J. 2014. February 1;14(2):315-25. Epub 2013 Nov 12. [DOI] [PubMed] [Google Scholar]
- 4.Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF, 3rd, Arnold KD, McConnell SJ, Bauman JA, Finegold DN. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008. March;90(3):540-53. [DOI] [PubMed] [Google Scholar]
- 5.Sanders JO, Browne RH, Cooney TE, Finegold DN, McConnell SJ, Margraf SA. Correlates of the peak height velocity in girls with idiopathic scoliosis. Spine (Phila Pa 1976). 2006. September 15;31(20):2289-95. [DOI] [PubMed] [Google Scholar]
- 6.Sanders JO, Browne RH, McConnell SJ, Margraf SA, Cooney TE, Finegold DN. Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg Am. 2007. January;89(1):64-73. [DOI] [PubMed] [Google Scholar]
- 7.Sanders JO. Maturity indicators in spinal deformity. J Bone Joint Surg Am. 2007. February;89(Suppl 1):14-20. [DOI] [PubMed] [Google Scholar]
- 8.Tanner JM. Assessment of skeletal maturity and prediction of adult height (TW3 method). New York: WB Saunders; 2001. [Google Scholar]
- 9.Fishman LS. Radiographic evaluation of skeletal maturation. A clinically oriented method based on hand-wrist films. Angle Orthod. 1982. April;52(2):88-112. [DOI] [PubMed] [Google Scholar]
- 10.Sidlauskas A, Zilinskaite L, Svalkauskiene V. Mandibular pubertal growth spurt prediction. Part one: method based on the hand-wrist radiographs. Stomatologija. 2005;7(1):16-20. [PubMed] [Google Scholar]
- 11.Pileski RC, Woodside DG, James GA. Relationship of the ulnar sesamoid bone and maximum mandibular growth velocity. Angle Orthod. 1973. April;43(2):162-70. [DOI] [PubMed] [Google Scholar]
- 12.Chapman SM. Ossification of the adductor sesamoid and the adolescent growth spurt. Angle Orthod. 1972. July;42(3):236-44. [DOI] [PubMed] [Google Scholar]
- 13.Hung A, Shi B, Chau W, Yip B, Yu F, Hung V, Lam T, Ng B, Cheng J. Can ossification pattern of the thumb epiphyses reliably simplify the classical Tanner-Whitehouse hand skeletal maturity assessment? A study of 645 hand radiographs from 125 premature AIS girls followed longitudinally till skeletal maturity. Read at the 51st Annual Meeting of the Scoliosis Research Society; 2016 Sep 21-4; Prague, Czech Republic.
- 14.Little DG, Song KM, Katz D, Herring JA. Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls. J Bone Joint Surg Am. 2000. May;82(5):685-93. [DOI] [PubMed] [Google Scholar]
- 15.Buckler JMH. A longitudinal study of adolescent growth. London: Springer; 1990. [Google Scholar]
- 16.Verma K, Sitoula P, Gabos P, Loveland K, Sanders J, Verma S, Shah SA. Simplified skeletal maturity scoring system: learning curve and methods to improve reliability. Spine (Phila Pa 1976). 2014. December 15;39(26):E1592-8. [DOI] [PubMed] [Google Scholar]
- 17.Charles YP, Diméglio A, Canavese F, Daures JP. Skeletal age assessment from the olecranon for idiopathic scoliosis at Risser grade 0. J Bone Joint Surg Am. 2007. December;89(12):2737-44. [DOI] [PubMed] [Google Scholar]
- 18.Nault ML, Parent S, Phan P, Roy-Beaudry M, Labelle H, Rivard M. A modified Risser grading system predicts the curve acceleration phase of female adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010. May;92(5):1073-81. [DOI] [PubMed] [Google Scholar]
- 19.Chazono M, Tanaka T, Marumo K, Kono K, Suzuki N. Significance of peak height velocity as a predictive factor for curve progression in patients with idiopathic scoliosis. Scoliosis. 2015. February 11;10(Suppl 2):S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chae HW, Suh I, Kwon AR, Kim YJ, Kim YH, Kang DR, Kim HY, Oh SM, Kim HC, Kim DH, Kim HS. Longitudinal standards for height and height velocity in Korean children and adolescents: the Kangwha study. [corrected]. J Korean Med Sci. 2013. October;28(10):1512-7. Epub 2013 Sep 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee TS, Chao T, Tang RB, Hsieh CC, Chen SJ, Ho LT. A longitudinal study of growth patterns in school children in Taipei area I: growth curve and height velocity curve. J Chin Med Assoc. 2004. February;67(2):67-72. [PubMed] [Google Scholar]
- 22.Mao SH, Jiang J, Sun X, Zhao Q, Qian BP, Liu Z, Shu H, Qiu Y. Timing of menarche in Chinese girls with and without adolescent idiopathic scoliosis: current results and review of the literature. Eur Spine J. 2011. February;20(2):260-5. Epub 2010 Dec 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. Stanford: Stanford University Press; 1950. [Google Scholar]
- 24.Yammine K. The prevalence of the sesamoid bones of the hand: a systematic review and meta-analysis. Clin Anat. 2014. November;27(8):1291-303. Epub 2014 Feb 25. [DOI] [PubMed] [Google Scholar]