Abstract
Inner retina in Alzheimer's Disease (AD) may experience neuroinflammation resulting in atrophy. The objective of our study was to determine whether retinal GCIPL (ganglion cell-inner plexiform layer) or nerve fiber layer (NFL) thickness may serve as noninvasive biomarkers to diagnose AD. This cross-sectional case-control study enrolled 15 mild cognitive impairment (MCI) patients, 15 mild-moderate AD patients, and 18 cognitively normal adults. NFL and GCIPL thicknesses on optical coherence tomography (OCT) were measured using Duke Optical Coherence Tomography Retinal Analysis Program (DOCTRAP) and Spectralis software. We demonstrated that regional thicknesses of NFL or GCIPL on macular or nerve OCTs did not differ between groups. However, a multi-variate regression analysis identified macular areas with a significant thickening or thinning in NFL and GCIPL in MCI and AD patients. Our primary findings controvert previous reports of thinner NFL in moderate-to-severe AD. The areas of thickening of GCIPL and NFL in the macula adjacent to areas of thinning, as revealed by a more complex statistical model, suggest that NFL and GCIPL may undergo dynamic changes during AD progression.
Introduction
Alzheimer’s disease (AD) is the only one of America’s top 10 leading causes of death that has no proven preventive or curative interventions. Early and cost effective diagnosis is crucial to the next stage of treatment and drug development. Current diagnostic modalities for AD are limited by cost (magnetic resonance imaging [MRI] or positron emission tomography [PET]), invasiveness (cerebrospinal fluid [CSF] biomarkers), or suboptimal specificity and sensitivity (genetic markers, serum amyloid) [1]. Neuropsychological evaluation is the “gold standard” for pre-mortem diagnosis of AD [2], but the testing is time-intensive, and may require multiple evaluations or access to specialists. By contrast, optical imaging is an inexpensive, fast, and noninvasive way to view the retina of live patients that may detect neural biomarkers during early stages of AD. Compared to brain imaging modalities, the higher resolution photography achievable with retinal imaging could greatly facilitate early dementia detection [3].
Optical Coherence Tomography (OCT) imaging reveals individual neuronal layers of the retina, including ganglion cell complex layer (GCIPL) and the retinal nerve fiber layer (NFL). Deviation from the age-matched normal range of the thickness for these layers directly correlates with the ganglion cells’ health and is a known biomarker in neurodegenerative diseases such as glaucoma [4], multiple sclerosis [5, 6], or amyotrophic lateral sclerosis [7].
It has long been recognized that patients with early AD experience abnormalities in visual acuity [8, 9], contrast sensitivity [10], color perception [11], visual field [12, 13], and motion perception [14, 15]. Many of the retinal findings associated with AD have been detected early in the disease course and mirror neurodegenerative changes in the brain [16–22]. Javaid and collaborators recently reviewed a dozen of potential visual or ocular markers of Alzheimer’s disease [23]. One of the most promising biomarkers is NFL thickness on OCT. A number of clinical studies have demonstrated quadrant-specific retinal NFL abnormalities in patients with mild cognitive impairment (MCI) or prodromal AD [16–22, 24, 25]. However, the region of the NFL affected varies substantially between these studies. Some have found thinning of NFL in all quadrants surrounding the nerve except nasal[26], others in all quadrants except superior [25], and others only in the temporal [27] or superior quadrant [28]. In contrast, three other studies did not find significant differences in NFL thickness between MCI and cognitively normal controls after carefully excluding potential confounders [29, 30], and in fact a recent study uncovered an inverse relationship between OCT thickness and cognitive scores [30].
The goal of the current study was to resolve this controversy through (1) a carefully designed cross-sectional, case-control study of age-matched, cognitively characterized normal controls, MCI and early-moderate AD patients; and (2) application of two separate tools for OCT layer segmentation. Semi-automatic segmentation methods were employed to precisely quantify NFL and GCIPL thicknesses on OCTs of both the macula and the optic nerve. To our knowledge, our study is the first to have three age-matched cognitive groups with neurocognitive group assignment made by clinical evaluation and consensus diagnosis, as well as careful exclusion of eyes with neovascular age-related macular degeneration (AMD), glaucoma and image artifacts (epiretinal membranes with traction etc.).
Materials and methods
Study subjects
The cross-sectional case-control clinical study NCT01937221 at a single academic center enrolled 15 patients with MCI, 15 patients with mild-to-moderate AD, and 18 control subjects who were cognitively normal and age-matched to the patient groups. Written informed consent was obtained from all study participants. 53 subjects were approached from November 14, 2013 and July 8th, 2015 and 5 patients screen failed due to the presence of ocular exclusion criteria detailed below. Patients were recruited from the ADRC’s Memory Disorders clinic and included in the mild-to-moderate AD group if they had a diagnosis of probable AD in accordance with the National Institute for Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) criteria[31] and were deemed to have symptoms characteristic of the mild to moderate stage of the disease. All clinical, imaging, and laboratory data were reviewed by one neurologist (JRB) and one clinical neuropsychologist (GGP) from the Duke Alzheimer’s Disease Research Center (ADRC) to arrive at a consensus decision regarding assignment to cognitive diagnostic group. Patients assigned to the MCI group were deemed to be symptomatic and have predementia, in accordance with published core clinical criteria for MCI [32]. In addition to available diagnoses of cognitive impairment, the clinicians evaluated clinical history for presence of cognitive and functional impairment, and for evidence of change in cognitive or functional impairment over time. Record review included the results of MRI, PET, and laboratory studies collected in the last year, as available. The clinicians viewed these as supportive information rather than as biomarkers. Normal age-matched controls were recruited from the ADRC registries, which monitor cognitive trajectories of individuals in the community. Individuals with normal performance on ADRC registry batteries (MoCA[33], Trail Making B[34], and Delayed Recall from the CERAD Word-listing learning test[35]) were contacted and neurocognitive assessment (Montreal cognitive assessment, MoCA) was repeated at the time of enrollment. Control subjects did not have a history of alcohol abuse, and were not affected by metabolic diseases, psychiatric or neurological disorders that can lead to cognitive decline.
Study inclusion criteria were the following: 1) Clinical review by ADRC clinicians who assigned patients to one of the participant groups, 2) Age ≥ 50 years and matched (+/- 5 years in all but two cases) to a participant in each of the other diagnostic groups, and 3) Fluency in English. Exclusion Criteria were: 1) Known or suspected diagnosis of non-AD, associated dementia, 2) Alcohol or drug addiction in past year or current systemic illness that could influence the patient’s safety and compliance with the protocol, and 3) Major ophthalmologic comorbidities: Ruptured globe, retinal vascular occlusive disease, retinal artery occlusion, anterior ischemic optic neuropathy, media opacification due to corneal abnormalities or cataract that prevent ocular and OCT examination, glaucoma, AMD, and macular edema.
Informed consent was obtained from all the patients or from their legal representatives when appropriate. The research followed the tenets of the Declaration of Helsinki and the protocol was approved by the Institutional Review Board at Duke University Medical Center.
Ophthalmologic examination
Study participants underwent a complete ophthalmologic examination including assessment of best-corrected visual acuity (BCVA), refraction, ocular motility, pupillary reflexes, intraocular pressure, and a dilated slit lamp ophthalmic exam and binocular indirect ophthalmoscopy. All participants had a corrected visual acuity of 20/40 Snellen or better and IOPs less than 21 mm Hg. The exam was performed by ophthalmologists masked to cognitive status and diagnosis (EML and SWC). Following pupil dilation with 1% tropicamide and 2.5% phenylephrine, ultra-high-resolution SD-OCT (Spectralis OCT, Heidelberg Engineering, Heidelberg, Germany) of both macula and the optic nerve (OCT NFL) and stereo photos of the optic nerve were obtained. All eyes that satisfied the inclusion criteria were included in the analysis.
NFL/GCIPL thickness measurement
The captured OCT images were enhanced using Spectralis Automatic Real-time Tracking (ART), which resulted in averaging between 7 to 41 B-scans. The macula scan protocol was set to capture 49 line scans for the 20 by 20 degrees scans and 61 line scans for the 30 by 25 degrees scans. For each macular and optic nerve volumetric scan, location-specific NFL and GCIPL thicknesses were measured semi-automatically as previously described using the Duke Optical Coherence Tomography Retinal Analysis Program (DOCTRAP) software that has been validated in numerous large scale clinical trials [36–41]. The software defined 6 retinal sublayers including NFL and GCIPL. GCIPL was defined as the sum of the ganglion cell layer and inner plexiform layer. Automated grading performed by the DOCTRAP software was followed by a two-grader quality control procedure to further examine segmentation boundaries and perform any manual corrections in masked fashion, as previously described [42]. Sub-layer thicknesses were automatically measured in each scan and average macular sub-layer thicknesses were calculated for each volumetric scan.
NFL and GCIPL layers were segmented and thicknesses were measured in all clock hours surrounding the optic nerve (peripapillary) and in all macular regions as defined by the Early Treatment Diabetic Retinopathy Study (ETDRS) [43] (S1 Fig). The OCT grader was masked to participant group assignment. The NFL thicknesses in areas surrounding the optic nerve were also generated and analyzed using the Heidelberg automated software. Masked graders checked for segmentation errors made by the Heidelberg automated software and corrected for any errors identified.
The nine-point advised protocol for OCT study terminology and elements (APOSTEL)[44] is presented in S1 Table.
Descriptive statistics
Descriptive statistics were computed for the three study groups for all variables. Demographics were compared using analysis of variance for continuous variables and Fisher’s exact test for categorical variables. Snellen visual acuities were converted to LogMAR units for analysis. Descriptive statistics for measures of thickness were computed by region using both eyes for a given layer (NFL and GCIPL) and OCT image type (macula and nerve). p value <0.05 defined statistical significance. Means were compared among and between groups using generalized estimating equations (GEE) to account for multiple eyes per subject. Statistical analyses were performed in SAS 9.3 (SAS Institute Inc., Cary, NC, USA). A sample size of 15 per group (3 groups, with uniform dispersion) provides sufficient power to detect large signals (Beta = 0.83 for effect size = 0.5), as would be ideal to develop a diagnostic test with high clinical value.
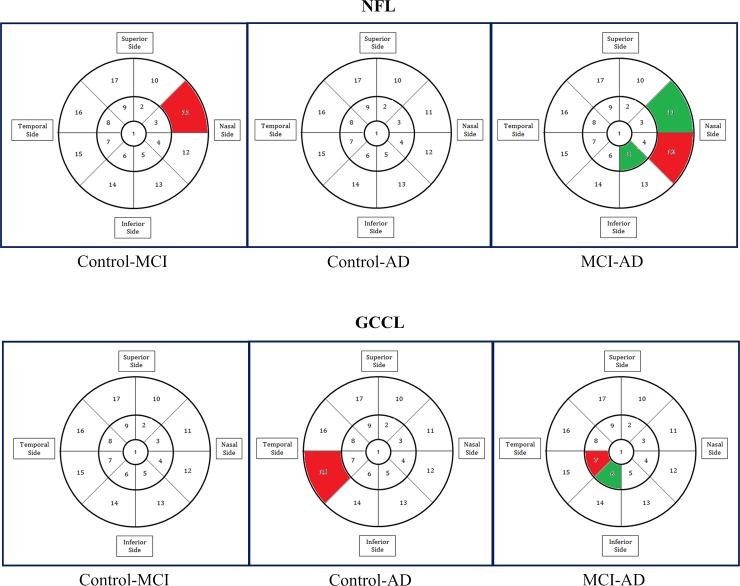
Multivariate regression analysis of NFL/GCIPL thickness
We used multivariate regression analysis to study the association between the input data (NFL and GCIPL layer thicknesses) to the output data (disease categories of the participants: control, MCI or AD). For this analysis, there were 17 ETDRS regional thickness values for both NFL and GCIPL. We accounted for the presence of two eyes for each participant by using Quasi-Least Squares (QLS) technique [45]. The sign of the coefficient of regression for the input variable represents the direction of association. The associations and directions are pictorially depicted in Fig 1, in which associated regions (p<0.05) are colored in green or red according to its direction: increase (green) or decrease (red) in thickness. A Bonferroni correction was then applied to account for multiple comparisons across the 17 areas (p<0.0029), and the regions that remained statistically different were shown in Fig 2.
Fig 1. Results of a multi-variate regression analysis with quasi-least squares, without correction for multiple comparisons.
This analysis identified areas in the macula that were statistically significantly thinner (red) or thicker (green) in NFL and GCIPL in MCI and AD patients as compared to controls, or in AD compared to MCI.
Fig 2. Results of the multi-variate regression analysis with quasi-least squares, adjusted for multiple comparisons.
Results
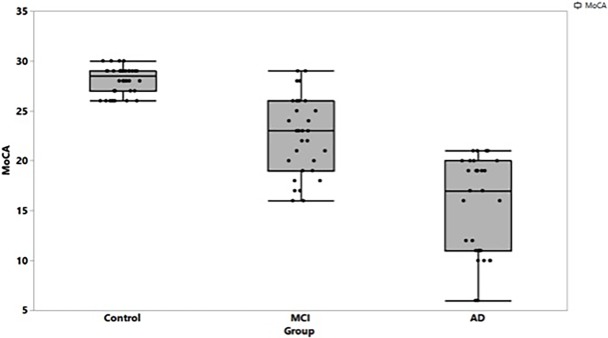
The three study groups (cognitively normal control group, MCI and mild to-moderate AD groups) were well balanced in terms of age (p = 0.79), gender, race (Table 1), visual acuity, and intraocular pressure (S2 Table). The MCI and AD groups exhibited statistically significantly lower neurocognitive scores than the control subjects (p<0.001) (Table 1). The distribution of the MoCA scores is depicted in Fig 3. Overlap was noted in the range of the MoCA scores between the AD and MCI group and between the MCI and control group, but not between the AD and the control group.
Table 1. Demographic characteristics of the cohort.
| Variable | Statistic | Alzheimer | Control | MCI | Overall P-Value |
Alzheimer vs Control P-Value* |
MCI vs Control P-Value* |
Alzheimer vs Control P-Value* |
|---|---|---|---|---|---|---|---|---|
| Age | N | 15 | 18 | 15 | ||||
| Mean (SD, range) | 74.20 (8.98, 55–86) | 75.17 (5.92, 66–83) | 73.07 (9.06, 58–86) | |||||
| Min, Median, Max | 55.0, 77.0, 86.0 | 66.0, 74.5, 83.0 | 58.0, 75.0, 86.0 | 0.789* | - | - | - | |
| Male Gender | N (%) | 8 (53) | 10 (56) | 7 (47) | 0.872** | - | - | - |
| Ethnicity, % Caucasian | N (%) | 14 (93.3) | 14 (93.3) | 15 (100) | 0.521** | - | - | - |
| MoCA | N | 15 | 18 | 15 | ||||
| Mean (SD) | 15.47 (4.96) | 28.06 (1.39) | 22.47 (3.96) | |||||
| Min, Median, Max | 6.0, 17.0, 21.0 | 26.0, 28.5, 30.0 | 16.0, 23.0, 29.0 | <0.001* | <0.001 | <0.001 | 0.001 |
*P-value based on Kruskal-Wallis test of difference among medians or Wilcoxon rank sum test of difference between medians.
**P-value based on chi-square test of difference among proportions.
Comparisons between groups not reported, as omnibus test failed to detect a significant difference across groups (p>0.5).
Fig 3. Distribution of MoCA scores among the three study groups.
First, NFL and GCIPL thicknesses measured using semi-automatic segmentation employing DOCTRAP software were compared separately for the various regions on the volumetric OCT macular scans as defined by the ETDRS study [43] and for all of the 12 clock hours surrounding the optic nerve on the volumetric OCT nerve scans. No statistically significant differences were observed between groups in thickness of NFL or GCIPL on OCTs of the macula or the optic nerve. The lack of difference between groups persisted when we compared measures that represented thicknesses of macula or optic nerve globally (Table 2), thicknesses of specific ETDRS areas in the macula or clock hours surrounding the optic nerve, or combination measures representing the thickness of larger geographic regions of the macula (inner and outer, superior, inferior, nasal and temporal) after adjusting for multiple comparisons (S3–S6 Tables).
Table 2. Global GCIPL and NFL thicknesses obtained using the DOCTRAP software in OCT volume scans of the macula and nerve.
| Region | Statistic | Alzheimer | Control | MCI | Overall P-Value* |
Alzheimer vs Control P-Value* |
MCI vs Control P-Value* |
Alzheimer vs MCI P-Value* |
|---|---|---|---|---|---|---|---|---|
| Global Macula GCCL | N | 29 | 33 | 23 | ||||
| Mean (SD) | 64.14 (8.19) | 64.08 (3.60) | 63.71 (7.12) | 0.993 | 0.979 | 0.919 | 0.921 | |
| Min, Median, Max | 42.1, 65.5, 76.9 | 56.3, 65.2, 68.7 | 45.8, 65.2, 75.3 | |||||
| Global Macula NFL | N | 29 | 33 | 23 | ||||
| Mean (SD) | 39.29 (4.49) | 37.71 (3.99) | 36.68 (4.22) | 0.220 | 0.328 | 0.364 | 0.080 | |
| Min, Median, Max | 30.8, 39.4, 50.8 | 31.3, 36.8, 50.1 | 27.6, 37.8, 43.3 | |||||
| Global Nerve GCCL | N | 30 | 36 | 30 | ||||
| Mean (SD) | 42.17 (7.68) | 40.20 (3.31) | 41.28 (4.22) | 0.476 | 0.326 | 0.359 | 0.671 | |
| Min, Median, Max | 33.6, 41.0, 68.7 | 33.5, 40.2, 46.3 | 33.6, 40.9, 52.5 | |||||
| Global Nerve NFL | N | 30 | 36 | 30 | ||||
| Mean (SD) | 100.7 (16.13) | 97.15 (8.94) | 95.69 (10.92) | 0.561 | 0.409 | 0.655 | 0.283 | |
| Min, Median, Max | 45.0, 101.9, 129.1 | 82.7, 96.8, 115.7 | 69.6, 93.1, 123.0 |
*P-values based on test of difference among and between groups using generalized estimating equations (GEE) to account for multiple eyes per subject.
Similarly, no statistically significant differences were observed between groups in thickness of NFL layer surrounding the optic nerve obtained via automated segmentation with the Heidelberg software (Table 3).
Table 3. NFL thicknesses obtained using the automated Heidelberg software in various regions surrounding the optic nerve.
| Variable | Statistic | Alzheimer | Control | MCI | P-Value |
|---|---|---|---|---|---|
| Nasal Superior | N | 15 | 18 | 15 | |
| Mean (SD) | 92.53 (23.51) | 85.44 (15.05) | 91.33 (19.79) | ||
| Min, Median, Max | 26.0, 90.0, 126.0 | 60.0, 86.5, 115.0 | 67.0, 97.0, 136.0 | 0.347 | |
| Nasal | N | 15 | 18 | 15 | |
| Mean (SD) | 78.27 (22.86) | 66.56 (14.57) | 68.00 (13.02) | ||
| Min, Median, Max | 46.0, 75.0, 133.0 | 35.0, 68.0, 91.0 | 37.0, 68.0, 95.0 | 0.272 | |
| Nasal Inferior | N | 15 | 18 | 15 | |
| Mean (SD) | 113.7 (33.67) | 104.8 (26.95) | 98.53 (25.10) | ||
| Min, Median, Max | 70.0, 107.0, 187.0 | 52.0, 105.5, 156.0 | 54.0, 97.0, 151.0 | 0.423 | |
| Temporal Superior | N | 15 | 18 | 15 | |
| Mean (SD) | 129.8 (24.17) | 123.9 (16.51) | 128.9 (16.23) | ||
| Min, Median, Max | 78.0, 134.0, 167.0 | 100.0, 122.5, 171.0 | 94.0, 131.0, 150.0 | 0.220 | |
| Temporal | N | 15 | 18 | 15 | |
| Mean (SD) | 72.33 (14.72) | 70.50 (14.01) | 68.27 (14.11) | ||
| Min, Median, Max | 51.0, 76.0, 93.0 | 49.0, 69.0, 100.0 | 49.0, 68.0, 97.0 | 0.634 | |
| Temporal Inferior | N | 15 | 18 | 15 | |
| Mean (SD) | 137.3 (23.20) | 131.4 (20.95) | 135.5 (15.00) | ||
| Min, Median, Max | 102.0, 144.0, 177.0 | 97.0, 128.5, 168.0 | 108.0, 138.0, 157.0 | 0.648 |
*P-value based on Kruskal-Wallis test of difference among medians.
The results of an analysis using a multi-variate regression model with quasi-least squares are shown in Figs 1 and 2. The results without correction (Fig 1) should be interpreted with caution. However, even after correcting for multiple comparisons across the 17 areas analyzed, we identified areas in the macula that were statistically significantly thinner (red) or thicker (green) in NFL and GCIPL layers in MCI and AD patients as compared to cognitively normal controls. It was observed that, when comparing data from MCI or AD to data from controls, areas that were found to be significantly thinner in AD or MCI were often abutting areas found to be significantly thicker in AD or MCI.
Discussion
Our case-controlled clinical study addressed a major controversy in the field of ocular biomarkers for early diagnosis of AD. We reported two parallel analyses employing different segmentation methods and standard statistical analyses, which both found no statistically significant difference in the thickness of inner retinal layers, NFL and GCIPL, in the macular and optic nerve volumes between cognitively healthy participants and MCI and early-moderate AD patients. This lack of difference was observed after careful exclusion of glaucoma, neovascular AMD and other significant retinal diseases, as well as areas with image artifacts or distortion secondary to retinal processes such as tractional epiretinal membranes. The first segmentation method employed was the DOCTRAP software, which has been used in many prior and ongoing clinical trials to accurately quantify the NFL and GCIPL thicknesses on OCT volumes of macula and optic nerve [42]. The second segmentation software used was that available on the Heidelberg SD-OCT units that quantifies NFL thicknesses in various areas surrounding the optic nerve, as previously done in a number of studies [16–25]. Our negative findings controverted previous reports of thinner NFL in moderate to severe AD patients compared to controls [16–25, 46].
We believe that our different result may be attributed to a number of factors: dynamic changes in the inner retinal layers with progression of MCI and AD[30], variable quality of case identification used in enrolling MCI and AD patients in other studies, or rigor of adjustment for confounders such as glaucoma and retinal artifacts (i.e. epiretinal membranes) that may influence retinal thickness. The current clinical study was robustly designed to address many of the limitations of previous studies, by using a case-control design, creating diagnostic groups balanced in age, race, and gender, and excluding confounding ocular conditions and systemic causes of cognitive decline. Consensus decisions regarding the assignment of the subjects to cognitive diagnostic groups were made by one neurologist one clinical neuropsychologist, both very experienced in diagnosis and management of AD [47]. Because controls were recruited from ADRC registries, they had undergone similar cognitive evaluations as the MCI or AD study participants.
Although our primary finding was the lack of association between NFL and GCIPL thicknesses and MCI or early AD, an interesting and important observation emerged from a more complex statistical analysis performed. Using a multi-variate regression model with quasi-least squares, we demonstrated the existence of specific areas of thickening alternating with areas of thinning in the macula of AD and MCI patients. This finding supports the idea that NFL and GCIPL thickness may be undergoing dynamic changes during the course of AD progression. Indeed, using the Spectralis OCT software, Ferrari and colleagues demonstrated a significant global NFL thinning in moderate AD but not mild AD patients as compared to controls [48], suggesting that thinning of the NFL may not occur until the severe stages of AD. Also in support of this hypothesis, Knoll and colleagues recently reported an inverse relationship between NFL thickness and scores on two neurocognitive tests, a delayed story recall and word list learning test [30]. The retinal thickening in early cognitive impairment was attributed to gliosis (and transient thickening) preceding neuronal loss and atrophy of the axonal projections in the NFL [30]. This concept has been reinforced by histopathology work suggesting that gliosis precedes human AD pathology in the brain [49, 50]. Although current OCT technology cannot differentiate between gliosis and axonal projections in the NFL, new retinal imaging modalities such as adaptive optics scanning laser ophthalmoscope is expected to enable visualization of the various tissue compartments of the retina with high degree of confidence [51]. A longitudinal study is necessary to ascertain whether the dynamic changes in the inner retina are reproducible, and whether specific areas of NFL/GCIPL thickening precede atrophic areas in MCI/AD subjects.
Questions remain about why various stages of AD might be associated with dynamic changes in the retina. Considering that the retina is a developmental outgrowth of the brain, one possibility is that the retina is vulnerable to the same neuroinflammatory injury that causes neurodegenerative disease in the brain. A second hypothesis is that neuronal dysfunction in the brain of a person with AD may lead to nerve loss in the retina via Wallerian-like degeneration. For example, the nucleus basalis of Meynert (NBM) is implicated in early AD and plays an important role in vision, sending projections to primary visual cortex [52–54]. Very early in the course of AD, the NBM undergoes degeneration and decreased acetylcholine production, which could result in decreased activation in visual cortex. In support of this hypothesis, multiple histopathological reports demonstrated retinal ganglion cell loss and optic nerve degeneration in AD patients [55–57] that would have experienced NBM degeneration very early in the disease process.
Our study has several limitations that may affect interpretation of results. One limitation is the small sample size, which limits power to detect small differences between groups. One larger study that reported significantly thinner retinal NFL in AD observed a small standard difference of 0.2 between AD and MCI [46]. If the population difference is similar to that observed difference, a sample size of over 800 is required to achieve 80% power to detect the difference (with 0.05 alpha error). However, we did not observe even a trend in the hypothesized direction using standard statistical analysis, noting that thicker mean NFL was observed in the AD group. Second, we excluded a small number of areas of the retina with prominent epiretinal membranes, which can result in traction and artifactually higher NFL and GCIPL thickness, and the exclusions effectively decreased the number of areas analyzed on the OCT volumetric scans of the macula and nerve. A third limitation may be the careful exclusion of glaucoma in our study and prior others, since open angle and normal tension glaucoma may be closely linked to AD. In a retrospective, propensity-score-matched analysis, Lin and colleagues reported that primary open glaucoma is a significant predictor of AD [58]. Therefore, our exclusion of glaucoma (which was intended to avoid confounding) may have caused us to miss a clinically significant relationship between AD and retinal thinning that is mediated by, rather than confounded by, glaucoma. A case control study of AD patients with and without glaucoma in which NFL and GCIPL OCT layer thicknesses can be compared would be an informative direction of future inquiry. A fourth limitation is that controls were drawn from a community registry, while cases were recruited from a sample of Memory Disorders clinic patients. Nonetheless, the diagnostic approaches were valid for the respective groups, and our confidence in group assignment was bolstered by the cognitive scores obtained at enrollment. Lastly, some of the AD subjects enrolled in our study may have had concomitant cerebral small-vessel disease (SVD), as AD has been reported to present frequently with SVD [59]. SVD is characterized by lacunar infarcts or diffuse white matter lesions on CT and MRI. Our study excluded patients with known or suspected clinical diagnosis of non-AD associated dementia including stroke and vascular dementia. However, although record review of the subjects enrolled included neuroimaging if previously performed, CT and MRI studies were not always available to exclude a diagnosis of SVD. A recent study of over 4000 Korean subjects showed that NFL defects were significantly associated with white matter lesions, although not with lacunar infarctions [60]. Therefore, it is possible that some of the AD subjects enrolled had concomitant SVD, which may have accounted for the macular areas with thinning in NFL on our multi-variate regression analysis. A future larger study should recruit a larger patient group well characterized by neuroimaging that would allow the diagnosis of SVD as well as identification and validation of useful clinical diagnostic endpoints.
Although the focus of this manuscript is analysis of inner retinal layers on SD-OCT, an important future direction is investigation of other potential retinal biomarkers of early AD. It has been long noted that AMD shares several clinical and pathological features with Alzheimer’s disease [61], which include peripheral retinal abnormalities such as drusen and pigment changes seen on color fundus photographs of AD patients [62, 63]. A recent clinical study has shown significant difference in presence of hard drusen in peripheral retina (manually graded on color and autofluorescence fundus images) of 56 AD patients (25.4%) vs. 46 controls (4.2%) [64]. Amyloid-ß plaques were detected in post-mortem retinas of 8 AD patients and five “probable” AD patients, but not in the five age-matched controls [65]. If future work is able to identify a set of retinal biomarkers, or an algorithm based on a combination of biomarkers, that reliably predicts cognitive decline, the impact on clinical care could be immediate. Even before effective therapy is developed, patients with MCI and their families would benefit from reliable prognostic information in terms of their ability to plan for the future (financial decisions, advanced directives, care/residence decisions, etc.). Reliable prognostication and better planning at the individual level could have significant societal benefit, considering the high societal cost of dementia care world-wide [66]. In the longer-term, better diagnostic tools for early AD would likely hasten the development of effective treatments for this devastating disease.
Supporting information
Examples of segmentation of OCT B-scans of the macula (A) and nerve (B) using DOCTRAP software. NFL is the layer between the red and yellow segmentation lines and GCIPL between the yellow and green lines.
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We would like to thank Maria Cecilia Santiago-Turla and Alice Ventura for assistance with subject enrollment and Julia Bellatoni for data entry.
Funding sources: Alzheimer’s Association New Investigator Research Grant (NIRG-13-282202), Duke Institute for Brain Sciences Incubator Award, Duke/Duke-NUS pilot award.
Abbreviations
- ADRC
Alzheimer’s Disease Research Center
- AMD
age-related macular degeneration
- BCVA
best corrected visual acuity
- CSF
cerebrospinal fluid
- DOCTRAP
Duke Optical Coherence Tomography Retinal Analysis Program
- ETDRS
Early Treatment Diabetic Retinopathy Study
- GCIPL
ganglion cell complex layer
- GEE
generalized estimating equations
- LogMAR
Logarithm
of the Minimum Angle of Resolution
- MCI
mild cognitive impairment
- MoCA
Montreal cognitive assessment
- MRI
magnetic resonance imaging
- NINCDS-ADRDA
National Institute for Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association
- NFL
nerve fiber layer
- PET
positron emission tomography
- QLS
Quasi-Least Squares
- SD-OCT
Spectral domain optical coherence tomography
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was funded by an Alzheimer’s Association New Investigator Research Grant (NIRG-13-282202, HEW), https://www.alz.org/; Duke Institute for Brain Sciences Incubator Award (EML), https://dibs.duke.edu/; and Duke/Duke-NUS pilot award (HEW), https://medicine.duke.edu/medicinenews/funding-opp-duke-nus-research-collaborations-pilot-projects. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Grossman I, Lutz MW, Crenshaw DG, Saunders AM, Burns DK, Roses AD. Alzheimer's disease: diagnostics, prognostics and the road to prevention. EPMA J. 2010;1(2):293–303. Epub 2010/12/03. doi: 10.1007/s13167-010-0024-3 ; PubMed Central PMCID: PMC2987528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thal LJ, Kantarci K, Reiman EM, Klunk WE, Weiner MW, Zetterberg H, et al. The role of biomarkers in clinical trials for Alzheimer disease. Alzheimer disease and associated disorders. 2006;20(1):6–15. Epub 2006/02/24. doi: 10.1097/01.wad.0000191420.61260.a8 ; PubMed Central PMCID: PMC1820855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parnell M, Guo L, Abdi M, Cordeiro MF. Ocular manifestations of Alzheimer's disease in animal models. International journal of Alzheimer's disease. 2012;2012:786494 Epub 2012/06/06. doi: 10.1155/2012/786494 ; PubMed Central PMCID: PMC3362039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowd C, Tafreshi A, Zangwill LM, Medeiros FA, Sample PA, Weinreb RN. Pattern electroretinogram association with spectral domain-OCT structural measurements in glaucoma. Eye. 2011;25(2):224–32. doi: 10.1038/eye.2010.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martinez-Lapiscina EH, Arnow S, Wilson JA, Saidha S, Preiningerova JL, Oberwahrenbrock T, et al. Retinal thickness measured with optical coherence tomography and risk of disability worsening in multiple sclerosis: a cohort study. The Lancet Neurology. 2016;15(6):574–84. Epub 2016/03/25. doi: 10.1016/S1474-4422(16)00068-5 . [DOI] [PubMed] [Google Scholar]
- 6.Petzold A, Balcer LJ, Calabresi PA, Costello F, Frohman TC, Frohman EM, et al. Retinal layer segmentation in multiple sclerosis: a systematic review and meta-analysis. The Lancet Neurology. 2017;16(10):797–812. Epub 2017/09/19. doi: 10.1016/S1474-4422(17)30278-8 . [DOI] [PubMed] [Google Scholar]
- 7.Simonett JM, Huang R, Siddique N, Farsiu S, Siddique T, Volpe NJ, et al. Macular sub-layer thinning and association with pulmonary function tests in Amyotrophic Lateral Sclerosis. Scientific Reports. 2016;6:29187 doi: 10.1038/srep29187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cogan DG. Visual disturbances with focal progressive dementing disease. Am J Ophthalmol. 1985;100(1):68–72. Epub 1985/07/15. . [DOI] [PubMed] [Google Scholar]
- 9.Uhlmann RF, Larson EB, Koepsell TD, Rees TS, Duckert LG. Visual impairment and cognitive dysfunction in Alzheimer's disease. J Gen Intern Med. 1991;6(2):126–32. . [DOI] [PubMed] [Google Scholar]
- 10.Cronin-Golomb A, Corkin S, Rizzo JF, Cohen J, Growdon JH, Banks KS. Visual dysfunction in Alzheimer's disease: relation to normal aging. Ann Neurol. 1991;29(1):41–52. Epub 1991/01/01. doi: 10.1002/ana.410290110 . [DOI] [PubMed] [Google Scholar]
- 11.Pache M, Smeets CH, Gasio PF, Savaskan E, Flammer J, Wirz-Justice A, et al. Colour vision deficiencies in Alzheimer's disease. Age Ageing. 2003;32(4):422–6. Epub 2003/07/10. . [DOI] [PubMed] [Google Scholar]
- 12.Trick GL, Trick LR, Morris P, Wolf M. Visual field loss in senile dementia of the Alzheimer's type. Neurology. 1995;45(1):68–74. Epub 1995/01/01. . [DOI] [PubMed] [Google Scholar]
- 13.Whittaker KW, Burdon MA, Shah P. Visual field loss and Alzheimer's disease. Eye (Lond). 2002;16(2):206–8. Epub 2002/05/04. doi: 10.1038/sj/EYE/6700037 . [DOI] [PubMed] [Google Scholar]
- 14.Gilmore GC, Wenk HE, Naylor LA, Koss E. Motion perception and Alzheimer's disease. J Gerontol. 1994;49(2):P52–7. Epub 1994/03/01. . [DOI] [PubMed] [Google Scholar]
- 15.Mielke R, Kessler J, Fink G, Herholz K, Heiss WD. Dysfunction of visual cortex contributes to disturbed processing of visual information in Alzheimer's disease. The International journal of neuroscience. 1995;82(1–2):1–9. Epub 1995/05/01. . [DOI] [PubMed] [Google Scholar]
- 16.Cordeiro MF, Guo L, Coxon KM, Duggan J, Nizari S, Normando EM, et al. Imaging multiple phases of neurodegeneration: a novel approach to assessing cell death in vivo. Cell death & disease. 2010;1:e3 Epub 2010/01/01. doi: 10.1038/cddis.2009.3 ; PubMed Central PMCID: PMC3032512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paquet C, Boissonnot M, Roger F, Dighiero P, Gil R, Hugon J. Abnormal retinal thickness in patients with mild cognitive impairment and Alzheimer's disease. Neurosci Lett. 2007;420(2):97–9. Epub 2007/06/05. doi: 10.1016/j.neulet.2007.02.090 . [DOI] [PubMed] [Google Scholar]
- 18.Berisha F, Feke GT, Trempe CL, McMeel JW, Schepens CL. Retinal abnormalities in early Alzheimer's disease. Investigative ophthalmology & visual science. 2007;48(5):2285–9. Epub 2007/04/27. doi: 10.1167/iovs.06-1029 . [DOI] [PubMed] [Google Scholar]
- 19.Koronyo-Hamaoui M, Koronyo Y, Ljubimov AV, Miller CA, Ko MK, Black KL, et al. Identification of amyloid plaques in retinas from Alzheimer's patients and noninvasive in vivo optical imaging of retinal plaques in a mouse model. Neuroimage. 2011;54 Suppl 1:S204–17. Epub 2010/06/17. doi: 10.1016/j.neuroimage.2010.06.020 ; PubMed Central PMCID: PMC2991559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frost S, Martins RN, Kanagasingam Y. Ocular biomarkers for early detection of Alzheimer's disease. J ournal of Alzheimer's disease: JAD. 2010;22(1):1–16. Epub 2010/09/18. doi: E1017312Q5702570 [pii] doi: 10.3233/JAD-2010-100819 . [DOI] [PubMed] [Google Scholar]
- 21.Kesler A, Vakhapova V, Korczyn AD, Naftaliev E, Neudorfer M. Retinal thickness in patients with mild cognitive impairment and Alzheimer's disease. Clin Neurol Neurosurg. 2011;113(7):523–6. Epub 2011/04/02. doi: 10.1016/j.clineuro.2011.02.014 . [DOI] [PubMed] [Google Scholar]
- 22.Lu Y, Li Z, Zhang X, Ming B, Jia J, Wang R, et al. Retinal nerve fiber layer structure abnormalities in early Alzheimer's disease: evidence in optical coherence tomography. Neurosci Lett. 2010;480(1):69–72. Epub 2010/07/09. doi: 10.1016/j.neulet.2010.06.006 . [DOI] [PubMed] [Google Scholar]
- 23.Javaid FZ, Brenton J, Guo L, Cordeiro MF. Visual and Ocular Manifestations of Alzheimer's Disease and Their Use as Biomarkers for Diagnosis and Progression. Frontiers in neurology. 2016;7:55 Epub 2016/05/06. doi: 10.3389/fneur.2016.00055 ; PubMed Central PMCID: PMCPmc4836138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.He XF, Liu YT, Peng C, Zhang F, Zhuang S, Zhang JS. Optical coherence tomography assessed retinal nerve fiber layer thickness in patients with Alzheimer's disease: a meta-analysis. International journal of ophthalmology. 2012;5(3):401–5. Epub 2012/07/10. doi: 10.3980/j.issn.2222-3959.2012.03.30 ; PubMed Central PMCID: PMCPmc3388417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coppola G, Di Renzo A, Ziccardi L, Martelli F, Fadda A, Manni G, et al. Optical Coherence Tomography in Alzheimer's Disease: A Meta-Analysis. PloS one. 2015;10(8):e0134750 Epub 2015/08/08. doi: 10.1371/journal.pone.0134750 ; PubMed Central PMCID: PMCPmc4529274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ascaso FJ, Cruz N, Modrego PJ, Lopez-Anton R, Santabarbara J, Pascual LF, et al. Retinal alterations in mild cognitive impairment and Alzheimer's disease: an optical coherence tomography study. Journal of neurology. 2014;261(8):1522–30. Epub 2014/05/23. doi: 10.1007/s00415-014-7374-z . [DOI] [PubMed] [Google Scholar]
- 27.Gao L, Liu Y, Li X, Bai Q, Liu P. Abnormal retinal nerve fiber layer thickness and macula lutea in patients with mild cognitive impairment and Alzheimer's disease. Archives of gerontology and geriatrics. 2015;60(1):162–7. Epub 2014/12/03. doi: 10.1016/j.archger.2014.10.011 . [DOI] [PubMed] [Google Scholar]
- 28.Liu D, Zhang L, Li Z, Zhang X, Wu Y, Yang H, et al. Thinner changes of the retinal nerve fiber layer in patients with mild cognitive impairment and Alzheimer's disease. BMC neurology. 2015;15:14 Epub 2015/04/18. doi: 10.1186/s12883-015-0268-6 ; PubMed Central PMCID: PMCPmc4342899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shen Y, Liu L, Cheng Y, Feng W, Shi Z, Zhu Y, et al. Retinal nerve fiber layer thickness is associated with episodic memory deficit in mild cognitive impairment patients. Current Alzheimer research. 2014;11(3):259–66. Epub 2014/02/04. . [DOI] [PubMed] [Google Scholar]
- 30.Knoll B, Simonett J, Volpe NJ, Farsiu S, Ward M, Rademaker A, et al. Retinal nerve fiber layer thickness in amnestic mild cognitive impairment: Case-control study and meta-analysis. Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring. 2016;4:85–93. http://dx.doi.org/10.1016/j.dadm.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34(7):939–44. Epub 1984/07/01. . [DOI] [PubMed] [Google Scholar]
- 32.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7(3):270–9. Epub 2011/04/26. doi: 10.1016/j.jalz.2011.03.008 ; PubMed Central PMCID: PMCPMC3312027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society. 2005;53(4):695–9. Epub 2005/04/09. doi: 10.1111/j.1532-5415.2005.53221.x . [DOI] [PubMed] [Google Scholar]
- 34.Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Archives of clinical neuropsychology: the official journal of the National Academy of Neuropsychologists. 2004;19(2):203–14. Epub 2004/03/11. doi: 10.1016/s0887-6177(03)00039-8 . [DOI] [PubMed] [Google Scholar]
- 35.Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology. 1989;39(9):1159–65. Epub 1989/09/01. . [DOI] [PubMed] [Google Scholar]
- 36.Jain N, Farsiu S, Khanifar AA, Bearelly S, Smith RT, Izatt JA, et al. Quantitative Comparison of Drusen Segmented on SD-OCT versus Drusen Delineated on Color Fundus Photographs. Investigative Ophthalmology & Visual Science. 2010;51(10):4875–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maldonado RS, O'Connell RV, Sarin N, Freedman SF, Wallace DK, Cotten CM, et al. Dynamics of Human Foveal Development after Premature Birth. Ophthalmology. 2011;118(12):2315–25. doi: 10.1016/j.ophtha.2011.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chiu SJ, Izatt JA, O'Connell RV, Winter KP, Toth CA, Farsiu S. Validated Automatic Segmentation of AMD Pathology Including Drusen and Geographic Atrophy in SD-OCT Images. Investigative Ophthalmology & Visual Science. 2012;53(1):53–61. [DOI] [PubMed] [Google Scholar]
- 39.Li S, Fang L, Yin H. An efficient dictionary learning algorithm and its application to 3-D medical image denoising. IEEE Trans Biomed Eng. 2012;59(2):417–27 doi: 10.1109/TBME.2011.2173935 [DOI] [PubMed] [Google Scholar]
- 40.http://clinicaltrials.gov/ct2/show/NCT00734487. Age-Related Eye Disease Study 2 Ancillary Spectral Domain Optical Coherence Tomography Study (A2ASDOCT) 2008–2013. [DOI] [PubMed]
- 41.http://clinicaltrials.gov/ct2/show/NCT00950638. A Study of ARC1905 (Anti-C5 Aptamer) in Subjects With Dry Age-related Macular Degeneration2009-2011.
- 42.Chiu SJ, Toth CA, Bowes Rickman C, Izatt JA, Farsiu S. Automatic segmentation of closed-contour features in ophthalmic images using graph theory and dynamic programming. Biomedical optics express. 2012;3(5):1127–40. Epub 2012/05/09. doi: 10.1364/BOE.3.001127 ; PubMed Central PMCID: PMCPmc3342188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98(5 Suppl):786–806. Epub 1991/05/01. . [PubMed] [Google Scholar]
- 44.Cruz-Herranz A, Balk LJ, Oberwahrenbrock T, Saidha S, Martinez-Lapiscina EH, Lagreze WA, et al. The APOSTEL recommendations for reporting quantitative optical coherence tomography studies. Neurology. 2016;86(24):2303–9. Epub 2016/05/27. doi: 10.1212/WNL.0000000000002774 ; PubMed Central PMCID: PMCPMC4909557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shults J. Quasi-least squares fitting. Wiley Interdisciplinary Reviews: Computational Statistics. 2015;7(3):194–204. doi: 10.1002/wics.1349 [Google Scholar]
- 46.Cheung CY, Ong YT, Hilal S, Ikram MK, Low S, Ong YL, et al. Retinal ganglion cell analysis using high-definition optical coherence tomography in patients with mild cognitive impairment and Alzheimer's disease. Journal of Alzheimer's disease: JAD. 2015;45(1):45–56. Epub 2014/11/28. doi: 10.3233/JAD-141659 . [DOI] [PubMed] [Google Scholar]
- 47.Plassman BL, Langa KM, McCammon RJ, Fisher GG, Potter GG, Burke JR, et al. Incidence of dementia and cognitive impairment, not dementia in the United States. Ann Neurol. 2011;70(3):418–26. Epub 2011/03/23. doi: 10.1002/ana.22362 ; PubMed Central PMCID: PMCPMC3139807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ferrari L, Huang SC, Magnani G, Ambrosi A, Comi G, Leocani L. Optical Coherence Tomography Reveals Retinal Neuroaxonal Thinning in Frontotemporal Dementia as in Alzheimer's Disease. Journal of Alzheimer's disease: JAD. 2017;56(3):1101–7. Epub 2017/01/21. doi: 10.3233/JAD-160886 . [DOI] [PubMed] [Google Scholar]
- 49.Mandybur TI. Cerebral amyloid angiopathy and astrocytic gliosis in Alzheimer's disease. Acta neuropathologica. 1989;78(3):329–31. Epub 1989/01/01. . [DOI] [PubMed] [Google Scholar]
- 50.Bates KA, Fonte J, Robertson TA, Martins RN, Harvey AR. Chronic gliosis triggers Alzheimer's disease-like processing of amyloid precursor protein. Neuroscience. 2002;113(4):785–96. Epub 2002/08/17. . [DOI] [PubMed] [Google Scholar]
- 51.Chen MF, Chui TYP, Alhadeff P, Rosen RB, Ritch R, Dubra A, et al. Adaptive Optics Imaging of Healthy and Abnormal Regions of Retinal Nerve Fiber Bundles of Patients With GlaucomaAdaptive Optics Imaging of Glaucomatous Damage. Investigative Ophthalmology & Visual Science. 2015;56(1):674–81. doi: 10.1167/iovs.14-15936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kilimann I, Grothe M, Heinsen H, Alho EJ, Grinberg L, Amaro E Jr., et al. Subregional basal forebrain atrophy in Alzheimer's disease: a multicenter study. J Alzheimers Dis. 2014;40(3):687–700. Epub 2014/02/08. doi: 10.3233/JAD-132345 ; PubMed Central PMCID: PMCPMC4120953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu AK, Chang RC, Pearce RK, Gentleman SM. Nucleus basalis of Meynert revisited: anatomy, history and differential involvement in Alzheimer's and Parkinson's disease. Acta neuropathologica. 2015;129(4):527–40. Epub 2015/01/31. doi: 10.1007/s00401-015-1392-5 ; PubMed Central PMCID: PMCPMC4366544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu AJ, Dayan P. Uncertainty, neuromodulation, and attention. Neuron. 2005;46(4):681–92. Epub 2005/06/10. doi: 10.1016/j.neuron.2005.04.026 . [DOI] [PubMed] [Google Scholar]
- 55.Hinton DR, Sadun AA, Blanks JC, Miller CA. Optic-nerve degeneration in Alzheimer's disease. The New England journal of medicine. 1986;315(8):485–7. Epub 1986/08/21. doi: 10.1056/NEJM198608213150804 . [DOI] [PubMed] [Google Scholar]
- 56.Sadun AA, Bassi CJ. Optic nerve damage in Alzheimer's disease. Ophthalmology. 1990;97(1):9–17. Epub 1990/01/01. . [DOI] [PubMed] [Google Scholar]
- 57.Tsai CS, Ritch R, Schwartz B, Lee SS, Miller NR, Chi T, et al. Optic nerve head and nerve fiber layer in Alzheimer's disease. Archives of ophthalmology (Chicago, Ill: 1960). 1991;109(2):199–204. Epub 1991/02/01. . [DOI] [PubMed] [Google Scholar]
- 58.Lin IC, Wang YH, Wang TJ, Wang IJ, Shen YD, Chi NF, et al. Glaucoma, Alzheimer's disease, and Parkinson's disease: an 8-year population-based follow-up study. PloS one. 2014;9(9):e108938 Epub 2014/10/03. doi: 10.1371/journal.pone.0108938 ; PubMed Central PMCID: PMCPmc4183534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Esiri MM, Joachim C, Sloan C, Christie S, Agacinski G, Bridges LR, et al. Cerebral subcortical small vessel disease in subjects with pathologically confirmed Alzheimer disease: a clinicopathologic study in the Oxford Project to Investigate Memory and Ageing (OPTIMA). Alzheimer disease and associated disorders. 2014;28(1):30–5. Epub 2013/07/12. doi: 10.1097/WAD.0b013e31829b72f1 . [DOI] [PubMed] [Google Scholar]
- 60.Kim M, Park KH, Kwon JW, Jeoung JW, Kim TW, Kim DM. Retinal nerve fiber layer defect and cerebral small vessel disease. Investigative ophthalmology & visual science. 2011;52(9):6882–6. Epub 2011/07/28. doi: 10.1167/iovs.11-7276 . [DOI] [PubMed] [Google Scholar]
- 61.Kaarniranta K, Salminen A, Haapasalo A, Soininen H, Hiltunen M. Age-Related Macular Degeneration (AMD): Alzheimer's Disease in the Eye? Journal of Alzheimer's Disease. 2011;24(4):615–31. doi: 10.3233/JAD-2011-101908 [DOI] [PubMed] [Google Scholar]
- 62.Hagerman K, Taussig M, Coalter J, Jay W. Low Vision Rehabilitation in Patients with Visual and Cognitive Impairment. Visual Impairment Research. 2007;9(1):19–22. [Google Scholar]
- 63.Stelmack J. Emergence of a rehabilitation medicine model for low vision service delivery, policy, and funding. Optometry. 2005;76(5):318–26. Epub 2005/05/12. . [DOI] [PubMed] [Google Scholar]
- 64.Ritchie CW, Peto T, Barzegar-Befroei N, Csutak A, Ndhlovu P, Wilson D, et al. Peripheral Retinal Drusen as a Potential Surrogate Marker for Alzheimer's Dementia: A Pilot Study Using Ultra-Wide Angle Imaging. Invest Ophthalmol Vis Sci. 2011;52(6):6683-. [Google Scholar]
- 65.Koronyo-Hamaoui M, Koronyo Y, Ljubimov AV, Miller CA, Ko MK, Black KL, et al. Identification of amyloid plaques in retinas from Alzheimer's patients and noninvasive in vivo optical imaging of retinal plaques in a mouse model. NeuroImage. 2011;54, Supplement 1(0):S204–S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wimo A, Jonsson L, Bond J, Prince M, Winblad B. The worldwide economic impact of dementia 2010. Alzheimers Dement. 2013;9(1):1–11.e3. Epub 2013/01/12. doi: 10.1016/j.jalz.2012.11.006 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Examples of segmentation of OCT B-scans of the macula (A) and nerve (B) using DOCTRAP software. NFL is the layer between the red and yellow segmentation lines and GCIPL between the yellow and green lines.
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.