Abstract
Breast reconstruction after mastectomy plays an active role in improving the quality-of-life (QoL) and alleviating the psychological trauma of breast cancer patients, and has become an indispensable part of the comprehensive treatment in breast cancer. However, compared with mastectomy alone, breast reconstruction also increase operative complications. The surgical, oncological outcomes, and cosmetic effect of breast reconstruction remains to be evaluated. Data for patients with breast cancer who underwent breast reconstruction after mastectomy from February 2009 to November 2015 in our hospital were retrospectively analyzed, with a median follow-up time of 44 months. The operating time, blood loss, drainage fluid, postoperative complications, postoperative cosmesis, oncological outcomes, and QoL were evaluated and compared between different reconstruction types. A total of 151 women were included. The flap-based group had higher complication rates of marginal necrosis of incision, while the incidence of capsular contracture was higher in immediate implant group. There was no difference in blood loss, drainage fluid, and other postoperative complications. Several independent factors were associated with increased postoperative complications included diabetic, obese, and reconstruction with flap. There was no significant difference in the disease-free survival rate and overall survival rate between different surgical groups. In terms of cosmetic effect, patients in the tissue expander group were more likely to get a satisfactory postoperative breast appearance. QoL outcomes shown that the tissue expander group has better body image and sexual enjoyment, while there was no significant difference for other QoL domains. In conclusion, different methods of breast reconstruction are safe and feasible for patients with breast cancer, tissue expander implantation following delayed implant breast reconstruction is a more effective treatment on cosmetic and QoL outcomes.
Keywords: breast reconstruction, mastectomy, postoperative outcomes
1. Introduction
Breast cancer is a common disease affecting millions of women, the incidence rate showed an upward trend, and the incidence becomes much younger recently in China. The cornerstone of breast cancer treatment is surgery. Surgical treatment for women with invasive breast cancer includes either breast-conserving surgery or mastectomy.[1] More patients with breast cancer are being diagnosed at early stages and the rate of breast-conserving surgery is increasing. However, a large number of patients still need total mastectomy. The absence of a breast has a great effect on the body and mind of the patients, especially for young patients. In recent years, reconstruction following mastectomy has becoming an integral part of breast cancer management, offers women an opportunity to mollify some of the emotional and aesthetic effects of this devastating disease.[2]
The type of breast reconstruction includes autologous tissue (flap) reconstruction and implant reconstruction, or a combination of both.[3] Breast reconstruction can be performed immediately or delayed. The timing and operate method was determined by patient preference, physical characteristics, and risk factors. The cosmetic outcome of breast reconstruction is superior to mastectomy. Literature has proven good psychosocial outcome and quality of life (QoL) in patients who underwent breast reconstruction.[4,5] However, despite the evidence and recommendations, almost two-thirds of the mastectomies are still performed without breast reconstruction.[6] An important reason was that patients refused additional surgery, which may have an inherent complication risk and longer recovery periods.[7]
Autologous tissue provides the most natural and lasting outcomes, autologous reconstruction sought to provide a more aesthetic and natural alternative, and avoiding the drawbacks of early breast implants such as capsular contracture, increased risk of infection and rupture and their incompatibility with radiotherapy.[8,9] While autologous reconstruction is the surgical operation for breast reconstruction, complications can occur such as necrosis of skin flap, flap shrinkage, and even calcifications. Implant-based breast reconstruction continues to be the more popular option, with advantage of no donor-site morbidity, shorter procedures.[10] This procedure is particularly suitable for patients with a lack of autologous donor tissue. While convenient, implant-based reconstructive procedures do have their disadvantages. Postoperative complications, such as mastectomy-skin necrosis and reconstructive failure are higher.[11]
The application of postmastectomy breast reconstruction remains controversial, how to choose the right individualized surgical procedures is still an important topic, which needs to discuss. The aim of this report is to analyze surgical outcomes, oncological safety, complications, and satisfaction of different methods of breast reconstruction after mastectomy in breast cancer patients in our hospital.
2. Methods
2.1. Patients
A retrospective analysis of 151 breast cancer patients who underwent breast reconstruction postmastectomy between February 2009 and November 2015 in our unit. The inclusion criteria for the present study were as follows: patients had pathology confirmed as breast cancer; patients who had undergone immediate or delayed unilateral reconstructions following mastectomy; female patients; and patients with Eastern Cooperative Oncology Group performance status of 0 or 1. The exclusion criteria for the present study were as follows: patients without available pathological data; patients who had not received standard adjuvant treatment; patients underwent bilateral reconstructions; patients with synchronous bilateral invasive breast cancer or metachronous contralateral breast cancer; and patients without follow-up records. To reduce the heterogeneity of the patient, bilateral reconstruction cases were exclude, for these cases may had synchronous bilateral invasive breast cancer. Patients were either contacted by telephone or interviewed in person at our outpatient clinic. Electronic data were collected from surgical operating notes, clinical letters, and breast care nurses records, preoperative data included patient demographics, smoking history and co-morbidities (obesity, diabetes) and tumor characteristics (largest preoperative size at imaging, location, pathological details) and any neoadjuvant treatment were recorded.
All the patients provided informed consent, which was approved by the Ethics Committee of The Affiliated Tumor Hospital of Guangxi Medical University, China. All clinical procedures were conducted in accordance with Good Clinical Practice Guidelines and any related municipal or federal regulations.
2.2. Surgical outcomes
Surgical outcome measures included the operating time, blood loss, drainage fluid, and postoperative complications (infection, marginal necrosis of incision, dehiscence of incisions, upper limb lymphedema, bleeding, nipple necrosis, seroma, capsular contracture). Risk factors for complications after breast reconstruction were analyzed.
2.3. Oncological outcomes
The follow-up period was calculated from the date of surgery to the date of either death or last follow-up. The disease-free survival (DFS), overall survival (OS), and locoregional recurrence-free survival (LRFS) rates were calculated. The primary endpoint was DFS.
2.4. Cosmetic outcomes
The cosmetic outcome of breast reconstruction was evaluated by the surgeon and patients together as follows: Excellent, the reconstructed breast and the contralateral symmetry were of the same size, the patients were very satisfied; Good, the reconstructed breast was equal in size but slightly higher or lower than the contralateral side, there were no significant differences in clothes and patients were satisfied; Mediocre, the reconstructed breast was significantly asymmetrical with the contralateral side, and the patients were dissatisfied; Poor, the reconstructed breast was markedly deformed, the patients were extremely dissatisfied. This assessment method had been used in other literature.[12]
2.5. Assessment of QoL
One years after therapy, the patients were invited to finish a questionnaire, consisting of the questionnaires of the EORTC QLQ-C30 (the European Organization on the Research and Treatment of Cancer Quality of Life Questionnaire Version 3.0)[13] and QLQ-BR23 (the EORTC Breast Cancer Module).[14] All the scales were converted linearly to a scale of 0 to 100 according to the standard scoring procedures of EORTC. Higher scores stand for better health status and functioning for the scales that evaluate the global health and functioning, higher scores conformed to more complaints and/or symptoms to evaluate the symptoms. The outcomes of mean QoL were compared between different regimens of treatment and were compared with the reference values of EORTC.
2.6. Statistical analysis
All statistical analyses were performed on SPSS 19.0 (SPSS Inc, Chicago, IL). In order to determine risk factors associated with increased postoperative complications, multivariate step-wise logistic regression was used. Categorical variables were analyzed by chi-square test and continuous variables with Student t test where appropriate, the mean data of multiple groups was detected by analysis of variance. Survival analysis was performed using Kaplan–Meier analysis and log-rank tests. A P < .05 was considered statistically significant.
3. Results
3.1. Patient characteristics
During the period reviewed, 151 patients underwent breast reconstruction following mastectomy. The median age at primary surgery was 41 years (range: 23–58). The median follow-up from index surgery was 44 months (range: 12–80). Of the 151 patients, 59 patients (39.1%) underwent autologous tissue reconstruction, 54 patients (35.7%) underwent immediate implant reconstruction and the remaining 38 (25.2%) underwent tissue expander implant following delayed implant breast reconstruction. No significant differences in age, body mass index (BMI), diabetes, smoking history, hypertension, TNM stage, pathological types, hormone receptor and human epidermal receptor-2 (Her2) status, blood loss, and postoperative drainage were found between the 3 groups. The operative time in the flap group was longer than in the others (P = .000), and the drainage was also more than other groups (P = .001). Of the 151 patients, 32 received neoadjuvant chemotherapy, 57 underwent radiotherapy, 108 adjuvant chemotherapy, and 119 endocrine therapy. Patient and tumor characteristics were summarized in Table 1.
Table 1.
Patient and tumor characteristics and operation details according to reconstruction type.

3.2. Complications and risk factors
Total complication rate was 26.5%, there was no operative mortality. The patients were divided into 3 groups based on the type of reconstruction. There were significantly more complications after flap-based reconstruction than any other type of reconstruction (P = .028). There was increased marginal necrosis of incision (25.4%) after flap-based reconstruction (P = .000). There was increased capsular contracture (16.7%) after immediate implant reconstruction (P = .005). We found no significant differences in the rate of infection, dehiscence of incisions, upper limb lymphedema, bleeding, nipple necrosis, and seroma in different groups (Table 2). We evaluated whether these complications result in delay to adjuvant treatment, results shown that no significant differences in the time from surgery to subsequent treatment between patients with and without complications. Several independent factors were associated with increased postoperative complications, such as obese (odds ratio [OR] 1.76, confidence interval [CI] 1.28–2.69, P = .025), diabetic (OR 1.28, CI 1.06–1.55, P = .043). Flap-based reconstruction was also a risk factor for postoperative complications (OR 1.58, CI 1.32–2.75, P = .032). The results are shown in Table 3.
Table 2.
Comparison of postoperative complication between different breast reconstruction groups.

Table 3.
Multivariate logistic regression for risk factors associated with postoperative complications.

3.3. Oncologic outcomes
In the flap-based reconstruction group, 4 patients had locoregional recurrence, 3 patients had distant metastasis. In the immediate implant reconstruction group, 2 patients had locoregional recurrence, 2 patients had distant metastasis (Table 4). In the tissue expander group, 5 patients had locoregional recurrence, 2 patients had distant metastasis. There was no significant difference in DFS (log-rank P = .358) (Fig. 1) and OS (log-rank P = .738) (Fig. 2).
Table 4.
Oncologic outcomes in different breast reconstruction groups.

Figure 1.
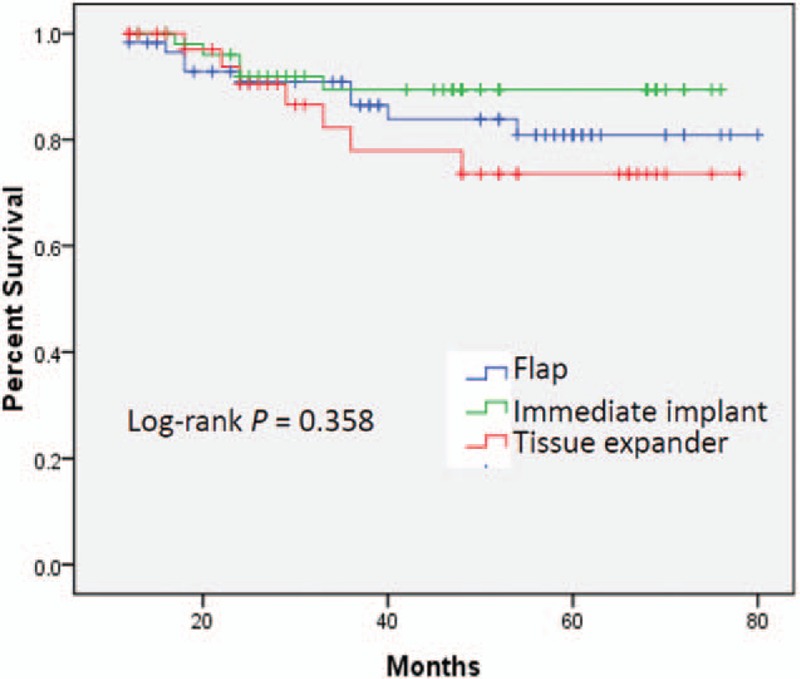
Comparison of disease-free survival (DFS) between different breast reconstruction groups.
Figure 2.
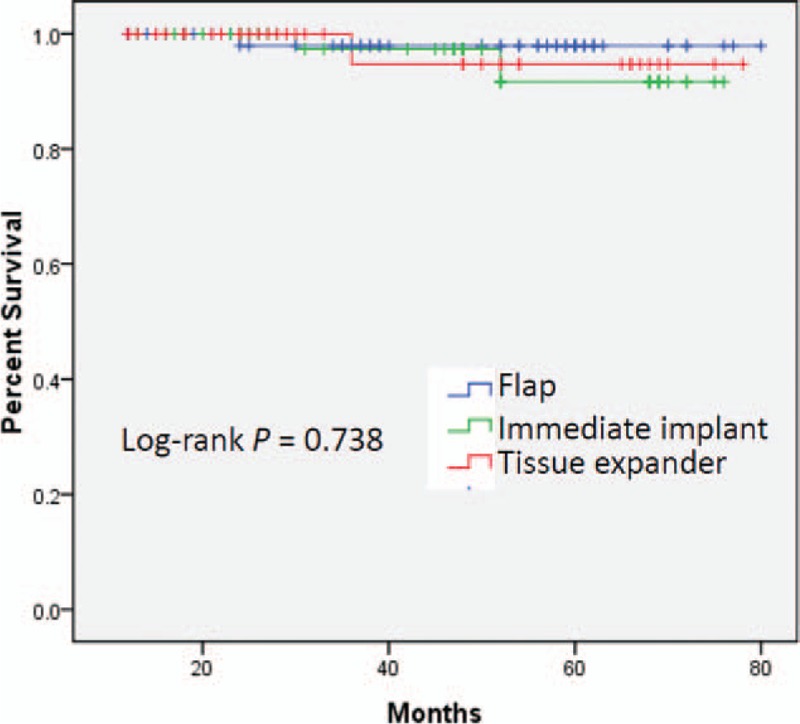
Comparison of overall survival (OS) between different breast reconstruction groups.
3.4. Cosmetic result
Comparing cosmetic outcomes between the 3 groups (Table 5), we found a better outcome (excellent or good) in the tissue expander group compared with the others (tissue expander vs flap vs immediate implant = 76.3% vs 62.7% vs 46.3%).
Table 5.
Comparison of cosmetic effect between different breast reconstruction groups.

3.5. QoL outcomes
For the questionnaires of EORTC QLQ-C30, patients in the of tissue expander group had better cognitive function and role function, patients who received reconstruction based on flap had much better global QoL and emotional function, and patients who received immediate implant reconstruction had better scores on social and physical functions. However, as shown in Table 6, the differences were quite subtle and not statistically significant.
Table 6.
QoL of patients according to the QLQ-C30 questionnaire.

Based on the questionnaires of EORTC QLQ BR23, the immediate implant group of patients reported significantly worse breast symptoms, and those in the tissue expander group had much better sexual enjoyment and body image, which were statistically difference (P < .05). There was no significant difference for other QoL domains, as shown in Table 7.
Table 7.
QoL of patients according to the QLQ-BR23 questionnaire.

4. Discussion
With the innovation of breast surgery, patients have more choices for the surgical approach than ever before. The number of patients who underwent breast reconstruction following mastectomy has increased in recent years, this is likely due to in part to advances in breast reconstruction, particularly tissue expander surgery. However, concerns remain regarding oncologic outcomes, surgical complications, and the National Comprehensive Cancer Network recommends breast reconstruction following mastectomy only for selected patients treated by experienced multidisciplinary teams.[15]
Since breast reconstruction is more complex than conventional breast cancer surgery, patients may be concerned that the resulting surgical complications may increase. As seen in our study, the total complication rate was only 26.5%, which is comparable to previous series of oncoplastic breast surgery.[7,16] The incidence of marginal necrosis of incision was increased in flap-based reconstruction group, compare with immediate implant or tissue expander reconstruction. In addition, the incidence of capsular contracture was increased in immediate implant reconstruction group, compare with other groups. Other complications had no significant difference. Although these are minor complications from surgical perspective, their duration may affect patients’ QoL and subsequent treatment. The operation time and drainage were statistically different, and were increased in flap-based reconstruction group, we hold the opinion that which is because of the operation itself, because all the operations were done in the same department, and the technical skills of the surgical teams were at the same level. We evaluated whether these complications result in delay to adjuvant treatment, results shown that no significant differences in the time from surgery to subsequent treatment between patients with and without complications. The main reason maybe the complications were mild and less influential. It is suggested that breast reconstruction is a safe and reliable operation from surgical perspective. Several independent factors were associated with increased operative complications such as obese and diabetic patients with these risk factors do not recommend complex breast reconstruction surgery.
Oncological safety is an important factor for patients to consider whether to undergo breast reconstruction. The local recurrence rate and distant recurrence rate was 7.3% and 4.6%, respectively, in our series, at a median follow-up of 44 months. The recurrence rate is within the range reported in many series of mastectomy treatment for breast cancer patients.[17,18] There were no significant differences in OS, DFS, and LRFS between different groups. In preoperative conversation, some of patients choose to forgo autogenous flap reconstruction for fear that it will make detection of recurrent breast cancer difficult. Some patients worry that implants or tissue expander may cause breast cancer. There have been a few matched case–control studies have reported no difference in oncologic outcomes between different types of breast reconstruction, oncologic outcomes was mainly related to the biological characteristics and stages of tumor.[19,20] In the present study, multivariate analysis show that the independent factors of prognosis were tumor stage, estrogen receptor/progestrone receptor status, and Her2 status. Our results coincide with those of other matched case–control studies,[5,21] suggesting that breast reconstruction is an oncologically safe procedure, whether it is autogenous tissue reconstruction, implant reconstruction, immediate breast reconstruction or delayed reconstruction.
The goal of breast reconstruction was to improve patients’ QoL after mastectomy, and patients’ satisfaction with breast symmetry is most important.[22,23] Achieving symmetry during breast reconstruction is also the most important goal for breast surgeons. The shape and volume of breasts differing in every person, the implants or tissue flap cannot meet the unique circumstances and needs of each patient. While bilateral breast symmetry is important, surgeons mainly choose the appropriate surgical method based on contralateral side. For a general size of the breast, we believe that autologous tissue transplantation is a more ideal method for breast reconstruction in term of tissue volume, size and softness, while implant styles are limited in matching the exact shape of the contralateral side. Previous studies have shown that volume is a more critical factor to patient satisfaction,[24] implants can provide a similar volume, which may confer a stable feeling of symmetry and great satisfaction on the patient when wearing a brassier. However, in our study, the patient satisfaction scores were generally higher in the tissue expander group, it can establish more appropriate breast volume and have low incidence of capsular contracture. Compare with immediate implant reconstruction, a better cosmetic outcome was found in the autologous flap reconstruction group, more natural shape and softness make it more advantageous; meanwhile, there is no capsular contracture in the long term. It is undeniable that reconstruction is probably from an outcome perspective most important for consideration on improvement on self-esteem and QoL, our results shown that the global QoL of the patients in different groups was generally high. This suggests that different ways of breast reconstruction do not have influence on global QoL. However, patients in the tissue expander group reported significantly better body image and sexual enjoyment, probably because this group has a better cosmetic outcome therefore improves self-esteem.
Our study has a few limitations. It was a retrospective study; therefore, selection bias may be an issue. Although all tested factors were matched successfully, the sample size was smaller. The patients’ pathological types were different, which may have an impact on the prognostic results, but the difference was small and not statistically. In addition, the follow-up duration was also relatively short for comparing long-term outcomes.
In conclusion, breast reconstruction following mastectomy could be a feasible surgical treatment option for breast cancer, tissue expander implantation following delayed implant breast reconstruction is a more effective treatment in terms of cosmetic and QoL outcomes, but the appropriate surgical procedures should be chosen according to the patient's actual situation. In future studies, a larger study population with a long-term follow-up is needed to more accurately determine oncologic outcomes.
Acknowledgment
The authors thank the patients enrolled in this study.
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, ER = estrogen receptor, Her2 = human epidermal receptor-2, OR = odds ratio, OS = overall survival, PFS = progression-free survival, PR = progestrone receptor.
QQ and QT contributed equally to this work.
This study was supported by National Natural Science Foundation of China (No.81360396), and Science and Technology Research Fund of Guangxi Zhuang Autonomous Region Science and Technology Department (No. 1355005–3-12).
The authors report no conflicts of interest.
References
- [1].Xing L, He Q, Wang YY, et al. Advances in the surgical treatment of breast cancer. Chin Clin Oncol 2016;5:34. [DOI] [PubMed] [Google Scholar]
- [2].Yueh JH, Slavin SA, Adesiyun T, et al. Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Reconstr Surg 2010;125:1585–95. [DOI] [PubMed] [Google Scholar]
- [3].Noone RB. Thirty-five years of breast reconstruction: eleven lessons to share. Plast Reconstr Surg 2009;124:1820–7. [DOI] [PubMed] [Google Scholar]
- [4].Heneghan HM, Prichard RS, Lyons R, et al. Quality of life after immediate breast reconstruction and skin-sparing mastectomy—a comparison with patients undergoing breast conserving surgery. Eur J Surg Oncol 2011;37:937–43. [DOI] [PubMed] [Google Scholar]
- [5].Robertson S, Wengstrom Y, Eriksen C, et al. Breast surgeons performing immediate breast reconstruction with implants—assessment of resource-use and patient-reported outcome measures. Breast 2012;21:590–6. [DOI] [PubMed] [Google Scholar]
- [6].Morrow M, Li Y, Alderman AK, et al. Access to breast reconstruction after mastectomy and patient perspectives on reconstruction decision making. JAMA Surg 2014;149:1015–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ilonzo N, Tsang A, Tsantes S, et al. Breast reconstruction after mastectomy: a ten-year analysis of trends and immediate postoperative outcomes. Breast 2017;32:7–12. [DOI] [PubMed] [Google Scholar]
- [8].Groen JW, Negenborn VL, Twisk D, et al. Autologous fat grafting in onco-plastic breast reconstruction: A systematic review on oncological and radiological safety, complications, volume retention and patient/surgeon satisfaction. J Plast Reconstr Aesthet Surg 2016;69:742–64. [DOI] [PubMed] [Google Scholar]
- [9].Kakagia D, Pallua N. Autologous fat grafting: in search of the optimal technique. Surg Innov 2014;21:327–36. [DOI] [PubMed] [Google Scholar]
- [10].Cemal Y, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. breast reconstruction: part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg 2013;131:320e–6e. [DOI] [PubMed] [Google Scholar]
- [11].Kalus R, Dixon Swartz J, Metzger SC. Optimizing safety, predictability, and aesthetics in direct to implant immediate breast reconstruction: evolution of surgical technique. Ann Plast Surg 2016;76(suppl 4):S320–7. [DOI] [PubMed] [Google Scholar]
- [12].Du J, Liang Q, Qi X, et al. Endoscopic nipple sparing mastectomy with immediate implant-based reconstruction versus breast conserving surgery: a long-term study. Sci Rep 2017;7:45636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365–76. [DOI] [PubMed] [Google Scholar]
- [14].Sprangers MA, Groenvold M, Arraras JI, et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol 1996;14:2756–68. [DOI] [PubMed] [Google Scholar]
- [15].Gradishar WJ, Anderson BO, Balassanian R, et al. Breast Cancer Version 2.2015. J Natl Compr Canc Netw 2015;13:448–75. [DOI] [PubMed] [Google Scholar]
- [16].Ho W, Stallard S, Doughty J, et al. Oncological outcomes and complications after volume replacement oncoplastic breast conservations—The Glasgow Experience. Breast Cancer (Auckl) 2016;10:223–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].De La Cruz L, Moody AM, Tappy EE, et al. Overall survival, disease-free survival, local recurrence, and nipple-areolar recurrence in the setting of nipple-sparing mastectomy: a meta-analysis and systematic review. Ann Surg Oncol 2015;22:3241–9. [DOI] [PubMed] [Google Scholar]
- [18].Petit JY, Gentilini O, Rotmensz N, et al. Oncological results of immediate breast reconstruction: long term follow-up of a large series at a single institution. Breast Cancer Res Treat 2008;112:545–9. [DOI] [PubMed] [Google Scholar]
- [19].Wu W, Cheng S, Deng H, et al. Impact of breast cancer subtype defined by immunohistochemistry hormone receptor and HER2 status on the incidence of immediate postmastectomy reconstruction. Medicine (Baltimore) 2016;95:e2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Park SH, Han W, Yoo TK, et al. Oncologic safety of immediate breast reconstruction for invasive breast cancer patients: a matched case control study. J Breast Cancer 2016;19:68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ryu JM, Paik HJ, Park S, et al. Oncologic outcomes after immediate breast reconstruction following total mastectomy in patients with breast cancer: a matched case-control study. J Breast Cancer 2017;20:74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bellino S, Fenocchio M, Zizza M, et al. Quality of life of patients who undergo breast reconstruction after mastectomy: effects of personality characteristics. Plast Reconstr Surg 2011;127:10–7. [DOI] [PubMed] [Google Scholar]
- [23].Serletti JM, Fosnot J, Nelson JA, et al. Breast reconstruction after breast cancer. Plast Reconstr Surg 2011;127:124e–35e. [DOI] [PubMed] [Google Scholar]
- [24].Baek WY, Byun IH, Kim YS, et al. Patient satisfaction with implant based breast reconstruction associated with implant volume and mastectomy specimen weight ratio. J Breast Cancer 2017;20:98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]


