Abstract
Health care extension is an approach to providing external support to primary care practices with the aim of diffusing innovation. EvidenceNOW was launched to rapidly disseminate and implement evidence-based guidelines for cardiovascular preventive care in the primary care setting. Seven regional grantee cooperatives provided the foundational elements of health care extension—technological and quality improvement support, practice capacity building, and linking with community resources—to more than two hundred primary care practices in each region. This article describes how the cooperatives varied in their approaches to extension and provides early empirical evidence that health care extension is a feasible and potentially useful approach for providing quality improvement support to primary care practices. With investment, health care extension may be an effective platform for federal and state quality improvement efforts to create economies of scale and provide practices with more robust and coordinated support services.
It is well established that robust primary care is essential to a high-value health care system.1–3 However, the US primary care system faces considerable challenges.4,5 Strategies are needed to assist practices in adapting to a rapidly changing health care landscape.6,7 While there is no single solution to address these primary care needs, a program implemented in agriculture in the early 1900s that brought research and education directly to rural communities has been suggested as a model that could bring similar assistance to primary care.8,9
The Cooperative Extension Service, established in 1914 under the Smith-Lever Act, was a cooperative undertaking of county, state, and federal partners.10 The federal government funded each state’s land-grant university to develop the workforce and infrastructure to spread agricultural expertise, create bidirectional communication between farmers and academic sites of knowledge production, and facilitate the diffusion of agricultural innovations. A key aspect of extension was the placement of extension agents in close proximity to communities to ensure consistent understanding of needs and delivery of services.11 This effort introduced new technology and resources to farmers and contributed significantly to making food affordable and accessible.12,13
Federal and state leaders have championed the use of the extension model to support and improve primary care.1,8,9,13,14 Evidence shows that primary care practices benefit from external support to develop quality improvement infrastructure and expertise,6 but strengthening the primary care infrastructure requires reaching many practices —small and large, rural and urban— across the nation to rapidly diffuse innovation and facilitate quality improvement. A cooperative extension for health care called the Primary Care Extension Program was included in the Affordable Care Act (ACA), although no funds were appropriated for it.
In spite of the lack of funds, this effort advanced the idea of health care extension and took advantage of already established Quality Improvement Organizations15 (created by the Centers for Medicare and Medicaid Services [CMS] to aid Medicare beneficiaries by providing better care and better health at lower cost) and Regional Extension Centers16 (which provide external support to eligible primary care providers in their adoption and meaningful use of certified electronic health record [EHR] technology). To complement these efforts, CMS created the Transforming Clinical Practice Initiative17 (which established peer-based learning networks to help primary care practices with large-scale transformation) and the Accountable Health Communities Model18 (which addresses health-related social needs through partnerships between practices and community resources).
To further the mission of the Primary Care Extension Program, the Agency for Healthcare Research and Quality (AHRQ) funded Infrastructure for Maintaining Primary Care Transformation (IMPaCT)19 grants in 2011, to develop and test state-level initiatives to advance Primary Care Extension. IMPaCT laid an important foundation for health care extension with the development of the Health Extension Toolkit, which outlined a model of health care extension as “a community-based, state-wide, but university-linked network of agents that can assist primary care practices with the best evidence-based practices to support the provision of quality care and practice transformation.”20
AHRQ has continued its efforts to advance the Primary Care Extension Program through the EvidenceNOW initiative, which was launched in 2015 and funded through 2018. The goal of EvidenceNOW is to improve the delivery of heart health care in approximately 1,500 primary care practices across the US by targeting four areas for quality improvement known as the ABCS: aspirin use,21 blood pressure control,22 cholesterol management,23 and smoking cessation support24 (see online appendix Exhibit A1).25 There are seven EvidenceNOW Cooperatives (ENCs) around the country, coordinated by universities working jointly with community partners and practices. Each cooperative employs a dozen or more extension agents (for example, practice facilitators) who connect practices with existing resources or work directly with practices to support quality improvement in heart health care.
This article presents a first look at early empirical findings from the AHRQ-funded evaluation of the ENCs, conducted by an evaluation team including many of the authors of this article.26 We identify common functions performed by the cooperatives and the challenges of extension implementation. We also identify critical features of emerging health care extensions and the role they may play in diffusing other practice innovations and sustaining primary care in the US.
Study Data And Methods
In this implementation phase of the Evidence-NOW evaluation (known as Evaluating System Change to Advance Learning and Take Evidence to Scale, or ESCALATES), we characterized the structure and function of the seven ENCs using qualitative and quantitative data for cross-case comparison. Qualitative data collected in real time, throughout 2015 to 2017, included documents (for example, grant applications and training materials); online diaries,27 an interactive platform for communicating in real time with key stakeholders from each cooperative to understand their experiences and work; observation notes made during annual site visits to the cooperatives; and semistructured interview data with key cooperative stakeholders.
We created matrices28 for side-by-side comparison of the data and then used an immersion/crystallization process, in which the evaluation team looked closely at the data (immersion) and then took a step back to identify patterns across ENCs (crystallization).29 We prepared data summaries before the start of the ENC interventions to provide baseline information and updated these summaries over time. Through this process, we identified the challenges ENCs faced and the different approaches and functions each ENC used to address these challenges and engage practices in a rapid improvement process. Importantly, we examined the infrastructure each ENC built to reach practices and diffuse the ABCS evidence, along with factors that influenced the approaches taken across ENC regions. We also examined each ENC’s past experience with extension work, as three states that participated in IMPaCT are also participating in Evidence-NOW, and all ENCs have at least one Regional Extension Center as a partner.
Two surveys were used to collect quantitative data characterizing EvidenceNOW practices before the start of the intervention. A survey completed by practice leaders focused on collecting infrastructure data about each practice (for example, practice size, ownership, patient panel characteristics), EHR capabilities, and use of quality improvement strategies as measured by the Change Process Capability Questionnaire.30 A survey completed by practice clinicians and staff members measured self-reported burnout and assessed the practices’ internal culture—or features that indicated each practice’s ability to make and sustain change—using the fourteen-item adaptive reserve measure.31 CMS clinical quality measures were used to assess the ABCS patient outcomes; these were collected by the ENCs and shared with evaluators. Descriptive statistics from surveys and ABCS outcomes at baseline provided a picture of the types of practices engaged by ENCs.
This study was approved by the Institutional Review Board at Oregon Health & Science University and was registered as an observational study online with clinicaltrials.gov (Identifier No. NCT02560428).
LIMITATIONS
This study had two important limitations. First, it was not possible to assess the effectiveness of the ENCs, as relevant data were not yet available. Nevertheless, the work of developing extension services to reach more than two hundred primary care practices in each region is complete, and identifying common challenges and functions of the ENCs is timely.
Second, more work is needed to identify what services practices chose to take part in, which were most beneficial, and what degree of external support is still needed. Practices’ experiences may vary based on ownership, types of patients, and practice location, for instance. While some of these variations are manifested in the ENC-level findings we report here, practice-level analyses and outcomes data are needed to identify health care extension best practices and clarify the overall impact of EvidenceNOW.
Study Results
Collectively, the ENCs enrolled 1,710 practices, with approximately 5,000 clinicians and over eight million patients across twelve states (exhibit 1). Each ENC is coordinated through a hub, typically an academic health center or the ENC principal investigator’s home institution.
Exhibit 1. Practices in EvidenceNOW.
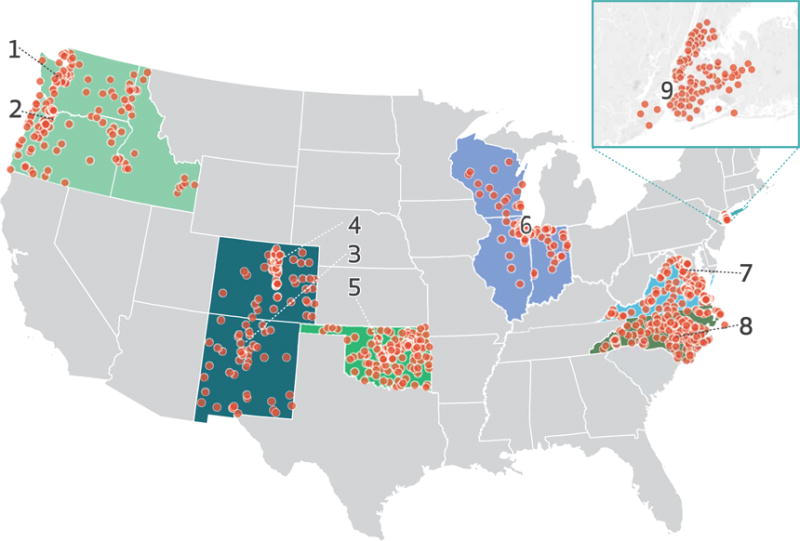
SOURCE Authors’ analysis of data from the EvidenceNOW evaluation. NOTES Each circle represents a ZIP code where one or more practices participate in an EvidenceNOW Cooperative, which coordinates its work through a hub. States grouped by color represent a single EvidenceNOW Cooperative. The hubs are as follows: (1) Kaiser Permanente Washington Health Research Institute, in Seattle; (2) Oregon Health & Science University, in Portland; (3) the University of New Mexico, in Albuquerque; (4) the University of Colorado, in Denver; (5) the University of Oklahoma, in Tulsa; (6) Northwestern University, in Chicago; (7) George Mason University, in Fairfax, VA; (8) the University of North Carolina at Chapel Hill; and (9) New York University, in New York City. The inset shows the New York City ZIP codes.
ENCs are supporting both independent small practices and practices owned by health systems. Almost 90 percent of the practices are small or medium size (1–10 clinicians), about 40 percent are clinician owned, over 60 percent are located in urban areas, and 33 percent are located in medically underserved areas (exhibit 2). The average clinical quality of the practices on the ABCS measures was less than optimal at baseline, with wide variation in quality scores. Few practices were using quality improvement strategies, and many practices lacked the capacity to use their EHR for data-informed quality improvement at baseline.
Exhibit 2.
Characteristics of the primary care practices in EvidenceNOW
| Practice (N
= 1,489) |
|||
|---|---|---|---|
| Number | Percent | Range across the cooperatives (%) | |
| Practice location | |||
| Urban | 945 | 63.5 | (34.9–100.0) |
| Suburban | 107 | 7.2 | (0.0–14.8) |
| Large town | 201 | 13.5 | (0.0–29.5) |
| Rural area | 235 | 15.8 | (0.0–27.9) |
|
| |||
| Number of clinicians | |||
| 1 | 354 | 23.8 | (6.3–52.4) |
| 2–5 | 695 | 46.7 | (16.2–59.1) |
| 6–10 | 205 | 13.8 | (6.8–17.2) |
| 11 or more | 160 | 10.7 | (1.9–23.4) |
|
| |||
| Practice ownership | |||
| Clinician | 601 | 40.4 | (27.8–72.8) |
| Hospital or health system | 342 | 23.0 | (1.6–53.9) |
| FQHC, RHC, IHS, or federal | 321 | 21.6 | (8.4–42.7) |
| Academic | 19 | 1.3 | (0.0–5.8) |
| Other or none | 147 | 9.9 | (1.0–38.8) |
|
| |||
| Medically underserved area | 493 | 33.1 | (15.7–45.0) |
SOURCE Authors’ analysis of data from the EvidenceNOW evaluation. NOTES 1,489 is the number of practice surveys included in this analysis. Percentages might not sum to 100 because of missing data. FQHC is federally qualified health center. RHC is rural health clinic. IHS is Indian Health Service. “Federal” refers to practices owned by agencies of the federal government, including the Departments of Defense and Veterans Affairs.
To achieve the EvidenceNOW goal of rapid dissemination and implementation of evidence-based practices to support cardiovascular risk reduction, ENCs needed to connect to, or establish, a network of resources for primary care practices. In the context of this initiative, partnerships and infrastructure were needed to perform four fundamental functions: technology support, quality improvement support, capacity building, and linking with the community) (see appendix exhibit A2).25 The external support that the ENCs provided practices varied according to the availability of existing resources and relationships, and regardless of a cooperative’s stage of development, all ENCs experienced challenges implementing interventions.
FOUR FUNCTIONS OF HEALTH CARE EXTENSION
Depite the diversity of ENCs, we found that all of them performed four fundamental functions to support primary care practices in improving cardiac risk prevention. The ENCs helped practices identify performance gaps by comparing their clinical quality performance data to state and national benchmarks, which allowed the practices to target areas for improvement and monitor the effects on patient outcomes (elements related to technology support); learn about current evidence from experts and how to implement practice and care delivery changes to align with evidence and improve care quality (quality improvement support); develop motivation, capacity, and resilience among practice members to respond to environmental changes and external reporting requirements (capacity building); and foster a broader and more connected network of community partnerships to better serve their patients (linking with the community).
ENCs needed technology support elements to help practices measure the quality of the cardiovascular preventive care being delivered, so that each practice could identify gaps and take steps to address them. This required providing practices with health information technology (IT) experts to aid practices in effectively using their EHR for quality improvement. To provide quality improvement elements, practice facilitators worked directly with practices to help build quality improvement capability by addressing work-flows and clinical care delivery. Practice facilitators taught practices how to improve processes of care and address their “pain points”—that is, the problems the practice identified; use rapid-cycle improvement strategies (based on the plan-do-study-act method, for example); and then monitor progress. Practice facilitators also provided capacity-building elements by teaching practices how to use measurement to improve workflows, clinical practice, and patient care. Online learning modules and web-based platforms provided access to resources as needed. ENCs also connected practices to peers through learning collaboratives, which fostered the sharing of ideas, bolstered motivation, and reduced feelings of isolation.
Finally, ENCs sought to connect practices to community resources (linking them with the community) that could help serve their patients. Some regions had already implemented the use of specific regional extension agents: In Colorado they are called Regional Health Connectors, while in New Mexico they are agents of Health Extension Rural Offices. In Oklahoma, practice facilitators collaborated with County Health Improvement Organizations that bring community members together to address local health issues.13 These agents reside where they work and act as local points of contact for practices. The degree to which ENCs linked practices with community resources varied widely, and these elements were often seen as formative and experimental.
Three years into the process, ENCs have put foundational elements of health care extension in place to facilitate the goals of this initiative regardless of their stage of development at the outset.
STAGES OF DEVELOPMENT
To create regional health care extensions, the convening organization—often the principal investigator’s home institution—needed to connect to or establish a network of resources to meet the Evidence-NOW initiative’s goals. Conveners built on an existing regional health care extension foundation or developed this infrastructure with partners in the context of EvidenceNOW.
ENCs came to EvidenceNOW at different stages of health care extension development and with different levels of experience working with practices and partner organizations in their regions. Previous extension experience, the existing regional resources, and the ENCs’ existing relationships with practice support partners shaped the structure of the ENCs. They engaged new and established partners based on those partners’ expertise and available workforce to provide practice facilitation and IT support, location relative to practices, and connection to practices through previous work. In some regions, multiple states were engaged. Key partners included academic health centers and research institutions; Regional Extension Centers and Quality Improvement Organizations; Area Health Education Centers; departments of health at the city, county, and state levels; and health IT organizations (exhibit 3).
Exhibit 3.
Characteristics of EvidenceNOW cooperatives
| Healthy Hearts in the Heartland | Heart Health Now! | Healthy Hearts Northwest | Healthy Hearts NYC | Healthy Hearts for Oklahoma | EvidenceNOW Southwest | Heart of Virginia Healthcare | |
|---|---|---|---|---|---|---|---|
| Region | Illinois, Indiana, Wisconsin | North Carolina | Idaho, Oregon, Washington | New York City | Oklahoma | Colorado, New Mexico | Virginia |
|
| |||||||
| Median distance to practices in miles (range) | 25 (0–331) | 115 (2–290) | 107 (1–819) | 10 (0–24) | 108 (0–351) | 47 (5–381) | 95 (1–374) |
|
| |||||||
| Academic institution(s) involved | Northwestern University, Northern Illinois University, and Purdue University | University of North Carolina at Chapel Hill | Kaiser Permanente Washington Health Research Institute, University of Washington, and Oregon Health & Science University | New York University | University of Oklahoma | University of Colorado and University of New Mexico | Virginia Commonwealth University, George Mason University, Eastern Virginia Medical School, Virginia Tech, and University of Virginia |
|
| |||||||
| Practice facilitators | 17 | 15 | 16 | 17 | 24 | 32 | 21 |
|
| |||||||
| Practices | 227 | 245 | 209 | 315 | 254 | 211 | 249 |
|
| |||||||
| Unique EHRs extension practices used | 22 | 18 | 30 | 4 | 32 | 24 | 10 |
SOURCE Authors’ analysis of EvidenceNOW evaluation data. NOTES Distances were calculated using the ZIP codes of the individual practices and their respective cooperative hubs, then summarized at the cooperative level. Computation was done using the ggmap package in R, version 3.3.3.
We found that the criteria for reaching a mature stage of development in a health care extension are time, experience, and consistent state support. North Carolina and Virginia represent contrasting stages of development and illustrate the challenges and nuances of working with established versus new partners in the context of EvidenceNOW.
▸ NORTH CAROLINA
North Carolina has a deep history of state support for the three primary partners in its ENC, called Heart Health NOW!: the University of North Carolina at Chapel Hill, the North Carolina Area Health Education Centers Program, and Community Care of North Carolina. These partners have collaborated on multiple grants and statewide projects (such as IMPaCT). As we learned from our qualitative data, one Heart Health NOW! leader credited the state with enabling the development of “long-term, ongoing [productive] relationships” among the three, which was necessary for establishing health care extension and facilitating the organizations’ “trust in a process of how we work together.” The University of North Carolina was a natural ENC convener, having extensive experience and expertise in research and evaluation, health policy, and clinical practice. Community Care of North Carolina, which managed the state’s health information exchange, was tasked with developing new data infrastructure for practices in the ENC. The North Carolina Area Health Education Center, one of the oldest and most established of such programs in the country, has a responsibility to provide continuing education in the state. This requires an extensive network of coaches who have long-term relationships with practices and live in the communities where they work. A long-standing, statewide support system for primary care practices and enduring relationships with key partners thus enabled the North Carolina ENC to provide the elements needed in a health care extension.
▸ VIRGINIA
In contrast, Virginia had little previous experience with formalized health care extension before EvidenceNOW, when the state established its ENC—called Heart of Virginia Healthcare. The convener was the Virginia Center for Health Innovation, a nonprofit convener and public-private partnership focused on improving health care in the state. Leaders at the center saw the ENC initiative as an opportunity to transform primary care in Virginia, with the goals of improving the use of the ABCS and returning joy to practice. This ENC included health policy and economics experts, multiple academic medical centers, and state health systems. The center brought in Health Quality Innovators (Virginia’s Regional Extension Center–Quality Improvement Organization), which had experience supporting practices through EHR implementation, to support practices in quality improvement. Virginia put together a multifaceted team in a short time, but building the infrastructure that Heart of Virginia Healthcare needed was “ten times harder” than anticipated, according to one of the cooperative’s leaders. Theirs was a first attempt at building the relationships across the state needed to provide extension functions. Unlike the ENC in North Carolina, the one in Virginia did not have an informatics center in place to develop data infrastructure for its practices. Nor did the Virginia ENC have prior reach into all communities across the state. However, it capitalized on a strong network of academic faculty members to support the work of Health Quality Innovators’ experienced practice facilitators, who were centralized rather than dispersed statewide. While Virginia did not come to EvidenceNOW with a turnkey network in place for large-scale initiatives, the state’s ENC was ready to learn, adapt, and adopt strategies to overcome implementation challenges. In this way, Heart of Virginia Healthcare embodies the spirit of the cooperative extension model and offers a case study for what it may take to implement new health care extensions.
IMPLEMENTATION CHALLENGES
Regardless of their stage of development at the outset, ENCs faced challenges related to the large-scale recruitment of practices.32 Small practices face time and resource constraints, and overcoming the challenge of engaging these practices in quality improvement required ENCs to clearly establish the value of the services and support they offered. This challenge was also affected by the ENC’s stage of development, partner relationships with practices, and practice ownership in particular. Independent practices and those owned by health systems had different needs and required different amounts and types of support. For instance, independent practices did not typically have access to data experts to assist them with generating reports for quality improvement activities, while health system–owned practices usually had these resources available, albeit in a central location. In addition, health systems sometimes wanted to employ their own practice facilitators, while independent practices viewed assistance from an external practice facilitator as valuable. Practice ownership is an aspect of any diffusion of innovation model that will need consideration moving forward,33 as practice ownership has the potential to affect two of the most significant and pervasive implementation challenges: adopting and using health IT and providing support for conducting ongoing practice-level quality improvement.
Practices across the ENCs varied in their capacity to develop usable data reports from their EHRs, which affected both the starting point for and the pace of quality improvement work. Regional Extension Center partners may have worked with practices on implementing EHRs, but extracting and using data for quality improvement was not typically part of these efforts. Conducting data-informed quality improvement requires producing reliable reports and EHRs are often unable to readily support practice quality improvement. This was a challenge for both new and established ENCs, which dealt with this challenge in various ways, based on preexisting data resources and partners that could support data extraction for quality improvement. For example, in North Carolina, the Informatics Center of Community Care of North Carolina intended to extract ABCS-related quality data and populate a dashboard for ENC practices, while Virginia ENC practice facilitators worked exclusively with the practices’ own EHRs because they lacked a strong health IT partner, so data feedback or benchmarking was not a consistent element of the improvement process. For regions without previously established data warehouses or hubs, ENCs’ facilitators or health IT experts had to help practices extract data from 4–32 different EHR systems (exhibit 3).
Once data were available, the next step required support from a practice facilitator, who helped each practice use these data for quality improvement. The challenges involved in hiring, training, and supporting practice facilitators varied depending on the ENCs’ stage of development and the readily available workforce. More established ENCs had deeper relationships with networks or organizations that employed experienced practice facilitators placed across regions. Other ENCs needed to build or supplement existing infrastructures to make practice facilitation accessible to regional practices. Being able to reach more than two hundred practices across a region required either multiple partners across a territory or one partner that already had the required reach. For example, Colorado partnered with fifteen organizations to provide practice facilitators. North Carolina partnered with one organization—the state’s Area Health Education Centers Program—because its practice facilitators were spread statewide. The location of members of the practice facilitation workforce had important implications. Practice facilitators who covered large areas made fewer in-person visits to practices, instead conducting phone or virtual encounters when limited by time or weather. In addition, these faciliators tended not to be from the community they served, and ensuring the quality of practice facilitation was more challenging when multiple organizations were involved in delivering these services.
Discussion
Building an infrastructure and a web of relationships to reach practices and communities is a goal of health care extension, as these connections are critical to ensuring the health of communities and the diffusion of innovation.34 AHRQ is not alone in championing this model: Over the past decade multiple federal agencies have supported primary care improvement programs that include elements of health care extension. To accomplish the mission of the Primary Care Extension Program as set forth in the ACA, emerging health care extensions need to engage a range of regional partners to build relationships to increase practice capacity for quality improvement, innovation, and the efficient use of resources. These targets may be met by providing practices with technical assistance, education, and coaching to enhance quality and sustain the primary care workforce.8,9 In EvidenceNOW, the clinical target is ABCS, but the external support provided by health care extension can be adapted to other clinical targets, new technology, and changing payment models in primary care.
Health care extension is based on a model that is intentionally bidirectional, bipartisan, and grassroots in spirit. Extension agents are conduits for information being diffused to practices and, perhaps more importantly, are positioned to push local knowledge and problems to academic leaders, researchers, and policy makers. ENCs were empowered to help practices and their communities help themselves through the acquisition of innovative quality improvement tools and capacity for change support to move patients toward better health. After a decade of deliberate health care extension effort in a small number of states, particularly New Mexico’s, Oklahoma’s, and North Carolina’s experiences with IMPaCT,8,9,13,35 EvidenceNOW expanded and further developed the health care extension model, confirming the model’s feasibility in regions at different developmental stages and contexts. EvidenceNOW demonstrates that health care extension is able to address the functions identified above in both urban and rural communities in twelve states with very different demographic characteristics, economic situations, politics, and histories. This nationally relevant experimental initiative shows that healthcare extension has the potential to be taken to scale.
While the model is compelling, there are also reasons to proceed with caution, as the application in agriculture offers not only encouragement but also important lessons. Cooperative extension did not remedy all challenges to rural communities. However, it provides a model that has sustained and can adapt to local needs and new knowledge. Functional health care extension may be best focused on bridging the urban-rural divide, shrinking the distance between academic health centers and communities, and sustaining primary care practices large and small where they are needed most—in rural and medically underserved areas.
Policy Implications
Federal initiatives to support the widespread dissemination of evidence to improve primary care quality and promote the diffusion of innovation constitute an expensive investment. Because programs such as Regional Extension Centers, the Transforming Clinical Practice Initiative, and Accountable Health Communities Model grants fund external support similar to that provided by EvidenceNOW, there is an opportunity to align expertise and create economies of scale across such efforts. Robust health care extension can provide a platform for other federal and state efforts to provide the ongoing support needed to promote innovation, practice change, and attainment of the Triple and Quadruple Aims.36
Conclusion
EvidenceNOW has created the opportunity to observe and document seven large-scale efforts to fulfill the common functions of health care extension in diverse contexts. The health care extension model offers an adaptive system that has the potential to respond to local or regional environments where it is deployed. We provide early empirical data establishing the feasibility of health care extension networks. What remains unknown is whether (and to what degree) the external support provided through health care extension has affected clinical practice—and if it has, how to sustain those gains. Findings on the former are forthcoming, but a sustainment plan continues to be a challenge. Sustaining health care extension is currently determined by local capacity to secure resources through grant funds from local and federal initiatives. EvidenceNOW represents large investments in infrastructure and capacity that merit full evaluation and cooperative thinking about whether and how to preserve the capacity.
Acknowledgments
Early findings that informed this article were presented at the 9th Annual Conference on the Science of Dissemination and Implementation, in Washington, D.C., on December 14, 2016. This research was supported by the Agency for Healthcare Research and Quality (Grant No. R01HS023940-01). Sarah Ono and Samuel Edwards are employed by the Department of Veterans Affairs. The views expressed herein are those of the authors and do not represent the views of the Department of Veterans Affairs or of the authors’ other affiliated institutions. The authors thank Laura Damschroder, Robert Phillips, Claire Diener, Rikki Ward, Jennifer Hall, David Cameron, Amanda Delzer Hill, and Leah Gordon for their contributions to this work and the EvidenceNOW Cooperatives for sharing their experience with ESCALATES. The authors also thank the reviewers and editors for their thoughtful feedback.
Contributor Information
Sarah S. Ono, An assistant professor in the Department of Family Medicine at Oregon Health & Science University and an investigator in the Center to Improve Veteran Involvement in Care, Veterans Affairs (VA) Portland Health Care System, both in Portland
Benjamin F. Crabtree, Professor in the Department of Family Medicine and Community Health, Research Division, Rutgers Robert Wood Johnson Medical School, in New Brunswick, New Jersey
Jennifer R. Hemler, Research associate in the Department of Family Medicine and Community Health, Research Division, Rutgers Robert Wood Johnson Medical School
Bijal A. Balasubramanian, Associate professor in the Department of Epidemiology, Human Genetics, and Environmental Sciences, UTHealth School of Public Health in Dallas, in Texas
Samuel T. Edwards, Assistant research professor in the Department of Family Medicine and an assistant professor of medicine at Oregon Health & Science University and a staff physician in the Section of General Internal Medicine, VA Portland Health Care System
Larry A. Green, Professor of family medicine and the Epperson-Zorn Chair for Innovation in Family Medicine at the University of Colorado Denver, in Aurora
Arthur Kaufman, Distinguished professor in the Department of Family and Community Medicine and vice chancellor for community health at the University of New Mexico, in Albuquerque.
Leif I. Solberg, Senior adviser and director for care improvement research at HealthPartners Institute, in Minneapolis, Minnesota
William L. Miller, Chair emeritus in the Department of Family Medicine, Lehigh Valley Health Network, in Allentown, Pennsylvania
Tanisha Tate Woodson, Senior research associate in the Department of Family Medicine, Oregon Health & Science University.
Shannon M. Sweeney, Research associate in the Department of Family Medicine and Community Health, Research Division, Rutgers Robert Wood Johnson Medical School
Deborah J. Cohen, Professor and vice chair of research in the Department of Family Medicine at Oregon Health & Science University
NOTES
- 1.Meyers DS, Clancy CM. Primary care: too important to fail. Ann Intern Med. 2009;150(4):272–3. doi: 10.7326/0003-4819-150-4-200902170-00009. [DOI] [PubMed] [Google Scholar]
- 2.Grundy P, Hagan KR, Hansen JC, Grumbach K. The multi-stakeholder movement for primary care renewal and reform. Health Aff (Millwood) 2010;29(5):791–8. doi: 10.1377/hlthaff.2010.0084. [DOI] [PubMed] [Google Scholar]
- 3.Margolius D, Bodenheimer T. Transforming primary care: from past practice to the practice of the future. Health Aff (Millwood) 2010;29(5):779–84. doi: 10.1377/hlthaff.2010.0045. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press; 2001. [PubMed] [Google Scholar]
- 5.Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood) 2010;29(5):799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 6.Irwin R, Stokes T, Marshall T. Practice-level quality improvement interventions in primary care: a review of systematic reviews. Prim Health Care Res Dev. 2015;16(6):556–77. doi: 10.1017/S1463423615000274. [DOI] [PubMed] [Google Scholar]
- 7.Wolfson D, Bernabeo E, Leas B, Sofaer S, Pawlson G, Pillittere D. Quality improvement in small office settings: an examination of successful practices. BMC Fam Pract. 2009;10:14. doi: 10.1186/1471-2296-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grumbach K, Mold JW. A health care cooperative extension service: transforming primary care and community health. JAMA. 2009;301(24):2589–91. doi: 10.1001/jama.2009.923. [DOI] [PubMed] [Google Scholar]
- 9.Phillips RL, Jr, Kaufman A, Mold JW, Grumbach K, Vetter-Smith M, Berry A, et al. The primary care extension program: a catalyst for change. Ann Fam Med. 2013;11(2):173–8. doi: 10.1370/afm.1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasmussen WD. Taking the university to the people: seventy-five years of cooperative extension. Ames (IA): Iowa State Press; 1989. [Google Scholar]
- 11.Kaufman A, Rhyne RL, Anastasoff J, Ronquillo F, Nixon M, Mishra S, et al. Health extension and clinical and translational science: an innovative strategy for community engagement. J Am Board Fam Med. 2017;30(1):94–9. doi: 10.3122/jabfm.2017.01.160119. [DOI] [PubMed] [Google Scholar]
- 12.Gawande A. Testing, testing. New Yorker [serial on the Internet] 2009 Dec 14; [cited 2017 Dec 15]. Available from: https://www.newyorker.com/magazine/2009/12/14/testing-testing-2.
- 13.Mold JW. A cooperative extension service for primary care in Oklahoma. J Okla State Med Assoc. 2011;104(11–12):414–8. [PubMed] [Google Scholar]
- 14.Kaufman A, Powell W, Alfero C, Pacheco M, Silverblatt H, Anastasoff J, et al. Health extension in new Mexico: an academic health center and the social determinants of disease. Ann Fam Med. 2010;8(1):73–81. doi: 10.1370/afm.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CMS.gov. Quality Improvement Organizations [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; [last modified 2017 Nov 13 cited 2017 Dec 14]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityImprovementOrgs/index.html?redirect=/qualityimprovementorgs/ [Google Scholar]
- 16.HealthIT.gov. Regional Extension Centers (RECs) [Internet] Washington (DC): Department of Health and Human Services; [last updated 2014 Sep 11 cited 2017 Dec 15 ] Available from: https://www.healthit.gov/providers-professionals/rec-history. [Google Scholar]
- 17.CMS.gov. Transforming Clinical Practice Initiative [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; [last updated 2017 Nov 27 cited 2017 Dec 14]. Available from: https://innovation.cms.gov/initiatives/Transforming-Clinical-Practices/ [Google Scholar]
- 18.CMS.gov. Accountable Health Communities Model [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; [last updated 2017 Sep 5 cited 2017 Dec 14]. Available from: https://innovation.cms.gov/initiatives/ahcm/ [Google Scholar]
- 19.Agency for Healthcare Research and Quality. IMPaCT (Infrastructure for Maintaining Primary Care Transformation) [Internet] Rockville (MD): AHRQ; [last reviewed 2012 Sep cited 2017 Dec 14]. Available from: http://www.ahrq.gov/research/findings/factsheets/primary/impactaw/index.html. [Google Scholar]
- 20.Health Extension Toolkit [home page on the Internet] Albuquerque (NM): The Toolkit; [cited 2017 Dec 14]. Available from: http://healthextensiontoolkit.org/ [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. Ischemic vascular disease (IVD): use of aspirin or another antiplatelet [Internet] Baltimore (MD): CMS; [last updated 2017 Oct 25 cited 2017 Dec 15]. Available from: https://ecqi.healthit.gov/ecqm/measures/cms164v5. [Google Scholar]
- 22.Centers for Medicare and Medicaid Services. Controlling high blood pressure [Internet] Baltimore (MD): CMS; [last updated 2017 Jul 12 cited 2017 Dec 15]. Available from: https://ecqi.healthit.gov/ecqm/measures/cms165v3. [Google Scholar]
- 23.Centers for Medicare and Medicaid Services. Statin therapy for the prevention and treatment of cardiovascular disease [Internet] Baltimore (MD): CMS; [last updated 017 Oct 25 cited 2017 Dec 15 ]. Available from: https://ecqi.healthit.gov/ep/ecqms-2018-performance-period/statin-therapy-prevention-and-treatment-cardiovascular-disease. [Google Scholar]
- 24.Centers for Medicare and Medicaid Services. Preventive care and screening: tobacco use: screening and cessation intervention [Internet] Baltimore (MD): CMS; [last updated 2017 Jul 12 cited 2017 Dec 15]. Available from: https://ecqi.healthit.gov/ecqm/measures/cms138v3. [Google Scholar]
- 25.To access the appendix, click the Details tab of the article online.
- 26.Cohen DJ, Balasubramanian BA, Gordon L, Marino M, Ono S, Solberg LI, et al. A national evaluation of a dissemination and implementation initiative to enhance primary care practice capacity and improve cardiovascular disease care: the ESCALATES study protocol. Implement Sci. 2016;11(1):86. doi: 10.1186/s13012-016-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen DJ, Leviton LC, Isaacson N, Tallia AF, Crabtree BF. Online diaries for qualitative evaluation: gaining real-time insights. Am J Eval. 2006;27(2):163–84. [Google Scholar]
- 28.Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. 2nd. Thousand Oaks (CA): Sage Publications; 1994. [Google Scholar]
- 29.Borkan J. Immersion/crystallization. In: Crabtree BF, Miller WL, editors. Doing qualitative research. 2nd. Thousand Oaks (CA): Sage Publications; 1999. pp. 179–94. [Google Scholar]
- 30.Solberg LI, Asche SE, Margolis KL, Whitebird RR. Measuring an organization’s ability to manage change: the Change Process Capability Questionnaire and its use for improving depression care. Am J Med Qual. 2008;23(3):193–200. doi: 10.1177/1062860608314942. [DOI] [PubMed] [Google Scholar]
- 31.Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med. 2009;7(3):254–60. doi: 10.1370/afm.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sweeney SM, Hall JD, Ono SS, Gordon L, Cameron D, Hemler J, et al. Recruiting practices for change initiatives is hard: findings from EvidenceNOW. Am J Med Qual. 2017 Sep 1; doi: 10.1177/1062860617728791. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brach C. “Will it work here?”: health systems need contextual evidence before adopting innovations. Health Affairs Blog [blog on the Internet] 2017 Jun 16; [cited 2017 Dec 15]. Available from: http://www.healthaffairs.org/do/10.1377/hblog20170616.060641/full/
- 34.Greenhalgh T, Robert G, Bate P, Macfarlane F, Kyriakidou O. Diffusion of innovations in health service organisations: a systematic literature review. Malden (MA): Blackwell Publishing Ltd; 2005. [Google Scholar]
- 35.Kaufman A, Boren J, Koukel S, Ronquillo F, Davies C, Nkouaga C. Agriculture and health sectors collaborate in addressing population health. Ann Fam Med. 2017;15(5):475–80. doi: 10.1370/afm.2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bodenheimer T, Sinsky C. From Triple to Quadruple Aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–6. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]


