Abstract
Background
The 11 September 2001 (9/11) attacks were unprecedented in magnitude and mental health impact. While a large body of research has emerged since the attacks, published reviews are few, and are limited by an emphasis on cross-sectional research, short time frame, and exclusion of treatment studies. Additionally, to date, there has been no systematic review of available longitudinal information as a unique data set. Consequently, knowledge regarding long-term trajectories of 9/11-related post-traumatic stress disorder (PTSD) among highly exposed populations, and whether available treatment approaches effectively address PTSD within the context of mass, man-made disaster, remains limited.
Methods
The present review aimed to address these gaps using a systematic review of peer-reviewed reports from October 2001 to May 2016. Eligible reports were of longitudinal studies of PTSD among highly exposed populations. We identified 20 reports of 9/11-related PTSD, including 13 longitudinal prevalence studies and seven treatment studies.
Results
Findings suggest a substantial burden of 9/11-related PTSD among those highly exposed to the attack, associated with a range of sociodemographic and back-ground factors, and characteristics of peri-event exposure. While most longitudinal studies show declining rates of prevalence of PTSD, studies of rescue/recovery workers have documented an increase over time. Treatment studies were few, and generally limited by methodological shortcomings, but support exposure-based therapies.
Conclusion
Future directions for research, treatment, and healthcare policy are discussed.
Keywords: September 11, 2001, 9/11; post-traumatic stress disorder (PTSD); trauma exposure severity; treatment of PTSD
Introduction
The events of 11 September 2001 (9/11) claimed the lives of close to 3000 people and injured 6000 more, including hundreds of firefighters and many law enforcement officers and military personnel, with the economic cost of damages measured in the 10s of billions of dollars by some estimates (Kunreuther et al. 2003). Although the acute effects of 9/11 attacks across emotional, social, and political spectrums were exceedingly deep and widespread (Comer & Kendall, 2007), the focus of this review is on the long-term trajectory of post-traumatic stress disorder (PTSD) and outcomes of PTSD treatments in ‘highly exposed’ populations (i.e. populations with direct trauma exposure), for whom the risk of PTSD was the highest (Galea et al. 2005; Neria et al. 2008, 2011). We focused on longitudinal studies, a set of findings yet to be systematically reviewed since the attacks of 9/11. Moreover, our review is the first to review treatment studies of 9/11-related PTSD across all highly exposed populations.
PTSD is a disabling, maladaptive reaction to traumatic stress with significant functional impairment and comorbidity (Kessler et al. 1995, 2005; Breslau et al. 1998). Hence, it is unsurprising that PTSD is the most commonly studied disorder following major disasters (Norris et al. 2002, 2008; Galea et al. 2005). The attacks of 9/11 were no exception; previous reviews (Pfefferbaum et al. 2004; Bills et al. 2008; Neria et al. 2008, 2011; Pfefferbaum et al. 2013; Wilson, 2015) and one meta-analysis (Liu et al. 2014) have tracked a relatively large volume of epidemiological literature on 9/11-related PTSD, and have drawn conclusions regarding rates of PTSD across multiple affected populations. Such data have critically informed debates regarding the need to develop coordinated efforts for intervention and prevention efforts (Breslau & McNally, 2008). A key limitation of these reviews, however, is that the range of PTSD rates was extremely broad across populations and time periods, and has consequently been difficult to interpret. Wilson (2015), for example, reviewed prevalence rates of PTSD among first responders following mass man-made violence events ranging from 1.3% to 22%, while Bills et al. (2008) reviewed rates of PTSD ranging from 8% to 22.5% among first responders following 9/11. Our own previous review examining prevalence rates of 9/11-related PTSD reflects this challenge as well, with reported rates ranging from 1.5% to 42% across various high-exposure populations (Neria et al. 2011). Although some have suggested 10% as an approximate prevalence rate for PTSD among first responders involved in 9/11 (Wilson, 2015), observed heterogeneity has prevented general agreement on PTSD rates over time, and there has been little consensus regarding other high-exposure populations.
A prime contributor to this wide variability in prevalence rates of PTSD is data from cross-sectional studies conducted at different time points and among different populations. For example, reported rates of PTSD in the year following 9/11 include 1.5% in a community sample (Galea et al. 2003), 29.6% in a sample of children and adolescents (Pfeffer et al. 2007), and 8% in a sample of New York City (NYC) transit workers (Tapp et al. 2005). In subsequent years, prevalence rates of PTSD were reported at 3.8% in a community sample (Adams & Boscarino, 2006), 15% in a sample of World Trade Center evacuees (DiGrande et al. 2011), and 12.4% in a sample of rescue and recovery workers (Perrin et al. 2007).
Cross-sectional studies are by definition limited by data collected at a single time point, and therefore cannot inform PTSD prevalence rate change and development over time. This is particularly problematic in the case of PTSD, as the trajectory of PTSD varies across populations (e.g. see Debchoudhury et al. 2011), and PTSD is known to sometimes develop after a considerable delay (Andrews et al. 2007). Furthermore, cross-sectional studies cannot establish temporal sequence and have limited potential for inference of predictors of PTSD among characteristics of the traumatic exposure and other potential co-factors (Galea & Maxwell, 2009). Combining findings from cross-sectional studies that span disparate time points and sample populations does not mitigate these problem and over-reliance on an assumed heterogeneity between samples leads to a danger of distorting actual trends (Susser et al. 2006; Garcia-Vera et al. 2016). Such challenges potentially prevent valid estimation of impact as well as development of appropriate interventions following a large-scale disaster. For example, in a meta-analysis of 9/11-related PTSD, Liu et al. (2014) concluded that prevalence rates of PTSD were lower for first responders based on a pooling of data from cross-sectional and longitudinal studies. However, this statement is not supported by increasing rates for this population over time, a trend reflected by longitudinal studies focusing on this population (Berninger et al. 2010a, b; Bowler et al. 2012). Other reviews of 9/11 have similarly failed to sufficiently distinguish between longitudinal and cross-sectional findings, despite recognition by some of the inherent advantages of longitudinal data (Pfefferbaum et al. 2004; Bills et al. 2008; Neria et al. 2008, 2011; Pfefferbaum et al. 2013; Wilson, 2015).
An additional limitation of extant reviews of 9/11 PTSD literature is that most eschew treatment studies, with the exception of a review conducted on treatment of first responders only (Haugen et al. 2012). Treatment studies naturally complement longitudinal epidemiological efforts by demonstrating how interventions may interact with illness trajectory, thus providing a more comprehensive picture. Moreover, with the recent increase in natural disaster and terror attacks worldwide, long-term longitudinal data, which include intervention, may serve as guidelines for handling similar traumatic experiences in the USA and abroad.
The current investigation aimed to address inherent limitations of previous reviews as new longitudinal data have emerged regarding course of 9/11-related PTSD and treatment among high-risk populations, including data collected through organized registries such as the World Trade Center Health Registry (WTC-HR) and the World Trade Center Health Program (WTC-HP). The goal of this review is to systematically survey 9/11 research in the 15 years since the attacks, focusing on evidence regarding course of PTSD, risk factors, and treatment of PTSD among 9/11 exposed populations, emphasizing findings unique to longitudinal investigations.
Methods
For the present review, we performed a search of peer-reviewed literature published from October 2001 to May 2016 and included published studies on longitudinal course of PTSD related to the events of 11 September, factors concerning risk and resilience, and treatment. We used two search engines: EBSCOhost Research Databases and Medline/PubMed. Articles were tagged for review if they included (a) the terms 9 11, 9/11, September 11, September 11th, or World Trade Center entered as search terms in the text body, title, or subject heading of an article, and (b) PTSD, in the same fields, using the terms PTSD, trauma, and posttraumatic stress. The initial search generated 3477 articles through EBSCOhost and 2017 through Medline/PubMed. We also cross-referenced previous reviews and meta-analyses concerning 9/11-related PTSD and/or treatment (Pfefferbaum et al. 2004; Bills et al. 2008; Neria et al. 2008, 2011; Haugen et al. 2012; Pfefferbaum et al. 2013; Liu et al. 2014; Wilson, 2015). Reports were excluded if they did not highlight highly exposed populations, defined as those living or working in close proximity to the 9/11 attacks, as well as first responders, rescue, recovery, and clean-up workers who attended the World Trade Center on 9/11 or directly afterward. We further excluded secondary analyses, review articles, editorials, commentaries, case reports, and studies that lacked full assessment of PTSD and/or prevalence rates or that focused primarily on physical illnesses associated with 9/11 rather than mental health, as well as those that contained cross-sectional data only. Our final list consists of 20 peer-reviewed articles, classified as longitudinal studies (n = 13) and treatment studies (n = 7). Survey methods included face-to-face interviews, in-person questionnaires, telephone interviews, online questionnaires, or mailed questionnaires depending on the study. Standardized PTSD instruments included the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (SCID; First et al. 1995), Clinician-Administered PTSD Scale (CAPS; Blake et al. 1995), and the PTSD Symptom Checklist (PCL; Blanchard et al. 1996). With one exception (Cukor et al. 2011), most of the epidemiological studies included in this review utilized measures that do not constitute clinician-administered assessments of PTSD. For this reason, the term ‘probable’ was used when referring to estimates of PTSD prevalence for most studies. A meta-analysis was not conducted due to the high degree of variability in methods present across studies reviewed.
In this review, we have reported time points of data collection post-9/11, sample size at each time point, PTSD assessment instruments, and estimated prevalence of probable PTSD in Table 1. Correlates of PTSD were reported in Table 2. Results of multivariate analyses were reported in favor of bivariate results if both were reported in the study of origin. Only correlates that showed a statistically significant relationship with PTSD (p < 0.05) were reported. Continuous variables (e.g. age, arrival time at scene of 9/11) were listed in abbreviated fashion for some studies in the interest of clarity. In such instances, only the effect size, odds ratio, or other reported statistic of greatest magnitude was reported.
Table 1.
Prevalence of PTSD/probable PTSD in highly exposed populations by Time Post-9/11
| Source | Sample population | Sampling method and type | PTSD instrument | Average time frame post-9/11 and population at each time point (n) | Estimated prevalence of PTSD/probable PTSD (%) |
|---|---|---|---|---|---|
| Adams & Boscarino (2006) | NYC residents | Random, CATI | NWS | 1 year (2323) | 4.7 |
| 2 years (1681) | 3.8 | ||||
| Berninger et al. (2010a) | Firefighters | Systematic, IPQ | PCL (DSM–IV criteria and non-weighted cut-off score nine out of 14 possible items) | 1 year (8679) | 9.8 |
| 2 years (1161) | 9.9 | ||||
| 3 years (2820) | 11.7 | ||||
| 4 years (4166) | 10.6 | ||||
| Berninger et al. (2010b) | Firefighters | Systematic, IPQ | PCL (DSM–IV criteria and non-weighted cut-off score of nine out of 14 possible items) | 0–6 months (5656) | 8.6 |
| 3–4 years (5656) | 11.1 | ||||
| Bowler et al. (2012) | Police responders | Convenience, CATI, FTFI | PCL (DSM-IV criteria) | 2–3 years (2940) | 7.8 |
| 5–6 years (2940) | 16.5 | ||||
| Brackbill et al. (2009) | RR, LMR, LMO, PB | Mixed, CATI | PCL (cut-off score 44) | 2–3 years (40 032) | 14.3 |
| R/R (20 294) | 12.1 | ||||
| LMR (5852) | 13.2 | ||||
| LMO (14 718) | 16.9 | ||||
| PB (2087) | 19.3 | ||||
| 5–6 years (40 032) | 19.1 | ||||
| R/R (20 294) | 19.5 | ||||
| LMR (5852) | 16.3 | ||||
| LMO (14 718) | 19.1 | ||||
| PB (2087) | 23.2 | ||||
| Cone et al. (2015) | Police responders | Convenience, FTFI | PCL (cut-off score 44) | 2–3 years (2204) | 13.6 |
| 5–8 years (2204) | 11.9 | ||||
| 10–11 years (2204) | 11.0 | ||||
| Cukor et al. (2011) | Utility workers | Convenience, FTFI, IPQ | CAPS and PCL (DSM-IV criteria) | 1–2 years (2960) | 9.5a |
| 3–4 years (2626) | 4.8 | ||||
| 6–7 years (1983) | 2.4 | ||||
| Debchoudhury et al. (2011) | Affiliated and lay volunteer disaster workers | Convenience, CATI, CAPI | PCL (cut-off score 44) | 3–4 years (4974) | 10.8 |
| Affiliated (3702) | 7.5 | ||||
| Lay (1272) | 20.2 | ||||
| 5–6 years (4974) | 15.9 | ||||
| Affiliated (3702) | 11.2 | ||||
| Lay (1272) | 29.6 | ||||
| Neria et al. (2010) | Primary care patients | Systematic, IPQ | PCL (cut-off score 44) | 1 year (455) | 9.6 |
| 4 years (455) | 4.1 | ||||
| Pfeffer et al. (2007) | BC, NBC | Convenience, FTFI – child and parent | K-SADS | 4 months to 2.6 years (79)b | 17 |
| BC (45) | 29.6 | ||||
| NBC (34) | 2.9 | ||||
| Timepoint 2 (79) | ~ 4 | ||||
| BC (45) | ~ 5 | ||||
| NBC (34) | <3 | ||||
| Pietrzak et al. (2014) | PR, NR | Convenience, IPQ | PCL (cut-off score 44) | 1–5 years (10 835) | 18.3 |
| PR (4035) | 8.5 | ||||
| NR (6800) | 24.1 | ||||
| 4–7 years (10 835) | 18.7 | ||||
| PR (4035) | 9.3 | ||||
| NR (6800) | 24.2 | ||||
| 6–9 years (10 835) | 17.8 | ||||
| PR (4035) | 9.8 | ||||
| NR (6800) | 22.5 | ||||
| Silver et al. (2005a) | US residents: DE, LME, NLE | Random, OQ | At 2 weeks, ASD assessed with SASRQ (DSM–IV criteria); at 1 year, PCL (DSM–IV criteria) | 2 weeks (1906) | 11.9 |
| DE (57) | 9.3 | ||||
| LME (1225) | 12.8 | ||||
| NLE (624) | 10.4 | ||||
| 1 year (1906) | 4.5 | ||||
| DE (57) | 11.2 | ||||
| LME (1225) | 4.7 | ||||
| NLE (624) | 3.4 | ||||
| Zvolensky et al. (2015) | Rescue and recovery workers: PR, NR | Convenience, IPQ | PCL | 1–9 years (18 896)c | 14.3 |
| PR (8466) | 11.7 | ||||
| NR (10 430) | 16.4 | ||||
| 3.5–11.5 years (18 896) | 15.3 | ||||
| PR (8466) | 13 | ||||
| NR (10 430) | 17.2 |
ASD, acute stress disorder; BC, bereaved children; CAPI, computer-assisted in-person personal interviewing; CAPS, Clinician-Administered PTSD Scale; CATI, computer-assisted telephone interview; DE, direct exposure; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; FTFI, face-to-face interview; IPQ, in-person questionnaire; K-SADS, Child Schedule for Affective Disorders and Schizophrenia; LME, live media exposure; LMO, lower Manhattan office workers; LMR, lower Manhattan residents; NBC, non-bereaved children; NLE, no live exposure; NR, non-traditional responders; NYC, New York City; OQ, online questionnaire; PB, passersby; PCL, PTSD Checklist; PR, police responders; PTSD, post-traumatic stress disorder; RR, rescue/recovery workers; SASRQ, Stanford Acute Stress Reaction Questionnaire
CAPS was administered only to a ‘high-risk’ subset of the total sample at the second (n = 2556) and third (n = 770) time points due to cost constraints. CAPS scores for the three time points were 14.9%, 8.4%, and 5.8%, respectively.
Initial time point varied. Participants were reassessed every 6 months.
Initial time point varied. Participants were reassessed after an average of 2.5 years.
Table 2.
Prevalence and correlates of probable PTSD in highly exposed populations by time post-9/11
| Source | Sample population | Significant correlates of PTSD/probable PTSD by time post-9/11 and type of analysisa
|
||||
|---|---|---|---|---|---|---|
| Correlate | Time 1 | Time 2 | Time 3 | Time 4 | ||
| Adams & Boscarino (2006) | NYC residents | Multivariate (adjusted OR) | 1 yr | 2 yrs | ||
| Younger age | 3.79 | N.S. | ||||
| Middle age | N.S. | 10.86 | ||||
| Female gender | 2.78 | N.S. | ||||
| Latino ethnicity | N.S. | 2.48 | ||||
| Greater 9/11 exposure | 2.71 | N.S. | ||||
| Non-9/11 trauma | 5.94 | 6.64 | ||||
| Multiple negative life events | 2.23 | 9.98 | ||||
| Low social support | 1.85 | N.S. | ||||
| Low self-esteem | 4.68 | 3.54 | ||||
| Berninger et al. (2010a) | Firefighters | Bivariate (unadjusted OR) | 1 yr | 2 yrs | 3 yrs | 4 yrs |
| Difficulty functioning at home | 17 | 20.6 | 26.7 | 22.6 | ||
| Difficulty functioning at work | 12.1 | 23.0 | 18.4 | 20.1 | ||
| Multivariate (adjusted OR) | ||||||
| Earliest arrival at WTC | 3.4 | 1.5 | 2.5 | 3.3 | ||
| Longer duration, WTC site | 1.6 | 1.6 | 2.1 | 1.7 | ||
| 9/11-related disability retirement | 1.5 | 2.6 | 1.8 | N.S. | ||
| Number of deaths in firehouse | 1.1 | 1.1 | N.S. | N.S. | ||
| Increase in alcohol use | 2.8 | 3.2 | 2.4 | 2.2 | ||
| Emotional support | 1.5 | NA | NA | NA | ||
| Decrease in exercise habits | 2.3 | NA | 2.3 | 2.6 | ||
| Use of counseling services | 2.9 | 4.0 | 4.3 | 3.5 | ||
| Religious affiliation | N.S. | N.S. | N.S. | 1.8 | ||
| Berninger et al. (2010b) | Firefighters | Multivariate (adjusted OR)b | ||||
| Middle age | 1.0 | |||||
| Older age | 0.6 | |||||
| Above high school education | 1.2 | |||||
| Not living with a partner | 1.06 | |||||
| Earliest arrival at WTC | 4.8 | |||||
| Longer duration, WTC site | 2.0 | |||||
| Higher rank | 1.1 | |||||
| Number deaths in firehouse | 2.3 | |||||
| 9/11 supervising responsibilities | 2.2 | |||||
| Previous disaster experience | 1.4 | |||||
| Bowler et al. (2012) | Police responders | Multivariate (β)b | ||||
| Female gender | 5.37 | |||||
| Older age | 0.07 | |||||
| Study response, phone | 8.33 | |||||
| Greater 9/11 exposure | 2.17 | |||||
| Current smoker | 1.91 | |||||
| Job lost post-9/11 | 4.45 | |||||
| Less social integration | −2.28 | |||||
| Interaction (variable × time) | ||||||
| Male gender | −0.91 | |||||
| Study response, mail or web | −1.33 | |||||
| Job lost post-9/11 | 1.76 | |||||
| Being disabled | 1.44 | |||||
| Brackbill et al. (2009) | Rescue/recovery workers, lower Manhattan residents and office workers, passersby | Multivariate (adjusted OR)c | 5–6 yrs | |||
| Pre-event depression | 1.8 | |||||
| Greater dust cloud exposure | 2.0 | |||||
| Greater WTC exposure | 2.2 | |||||
| Sustained injury 9/11 | 2.3 | |||||
| Loss/death of other 9/11 | 30.9 | |||||
| Post-event job loss | 4.6 | |||||
| Fewest social supports | 6.9 | |||||
| Cone et al. (2015) | Police responders | Multivariate (adjusted OR)d | 5–8 yrs | 10–11 yrs | ||
| Lower social support | 4.5 | 2.6 | ||||
| Unable to work due to health | 8.0 | 3.7 | ||||
| Life threatened post-9/11 | 1.9 | 3.3 | ||||
| Unmet mental health needs | 10.8 | 9.5 | ||||
| Recent life stressors | 3.2 | 3.2 | ||||
| Sustained injuries during 9/11 | 2.7 | N.S. | ||||
| Cukor et al. (2011) | Utility workers | Multinomial (adjusted OR) | 6–7 yrs | |||
| Trauma history | 2.27 | |||||
| Major depressive disorder | 2.80 | |||||
| Occupational exposure to 9/11 | 1.31 | |||||
| Neria et al. (2010) | Primary care patients | Multinomial (OR)b | 10.18 | |||
| Depression pre-9/11 | ||||||
| Depression post-9/11 | ||||||
| Pfeffer et al. (2007) | Bereaved and non-bereaved children | Bereavemente | ||||
| Hypothalamic-pituitaryadrenal axis dysregulation | ||||||
| Cortisol suppression | ||||||
| Pietrzak et al. (2014) | Police and non-traditional responders | Multinomial (adjusted OR)b,f | ||||
| Police responders | ||||||
| Previous psychiatric disorder | ||||||
| Greater stressors pre-9/11 | ||||||
| Greater 9/11 exposure | ||||||
| 9/11-related medical conditions | ||||||
| Non-traditional responders | ||||||
| Hispanic ethnicity | ||||||
| Previous psychiatric disorder | ||||||
| More stressors pre-9/11 | ||||||
| Greater 9/11 exposure | ||||||
| 9/11-related medical conditions | ||||||
| Silver et al. (2005a) | US residents with direct and indirect exposure | Bivariate (adjusted OR)b | 2 weeks | 1 yr | ||
| Proximity to WTC | 0.42 | N.S. | ||||
| Pre-9/11 mental health problems | 1.72 | 1.82 | ||||
| Female gender | 1.56 | N.S. | ||||
| Age | 0.98 | N.S. | ||||
| Acute stress at time point 1 | NA | 2.44 | ||||
| Lower education | N.S. | 0.33 | ||||
| Lower income | N.S. | 0.89 | ||||
| Zvolensky et al. (2015) | Police and non-traditional responders | Bivariate (r) | 1–9 yrs | 3.5–11.5 yrs | ||
| Age | −0.02 | 0.16 | ||||
| Gender | 0.16 | 0.26 | ||||
| Hispanic ethnicity | 0.22 | −0.14 | ||||
| African–American ethnicity | −0.11 | 0.04 | ||||
| Exposure to dust cloud | 0.09 | 0.14 | ||||
| Know someone injured | 0.20 | 0.07 | ||||
| Traumatic loss | 0.13 | 0.79 | ||||
| Depression | 0.78 | 0.72 | ||||
| Disability | 0.70 | 0.41 | ||||
| Life stress post-9/11 | NA | 0.29 | ||||
NA, not applicable/available; N.S., non-significant; NYC, New York City; OR, odds ratio; PTSD, post-traumatic stress disorder; WTC, World Trade Center; yrs, years. Note. Debchoudhury et al. (2011) was excluded due to absence of correlates of PTSD/probable PTSD.
In instances of multiple reported ORs, only the OR of greatest magnitude was reported. Multivariate correlates were reported in favor of bivariate correlates.
Correlates not differentiated by time frame post-9/11.
Correlates presented here represent a composite of four subgroups, including rescue/recovery workers, lower Manhattan residents, lower Manhattan office workers, and passersby. See article for detailed breakdown of correlates by subgroup.
All reported ORs were calculated using new instances of probable PTSD at each time point. Groups were compared with a ‘resilient’ group. An additional group, ‘chronic PTSD’, is not reported here.
This study derived correlates by comparing relative rates of probable PTSD across groups.
ORs for correlates were further delineated by subgroup depending on onset and course of PTSD. See article for specific details.
Results
Prevalence and course of PTSD
Traditional and non-traditional first responders
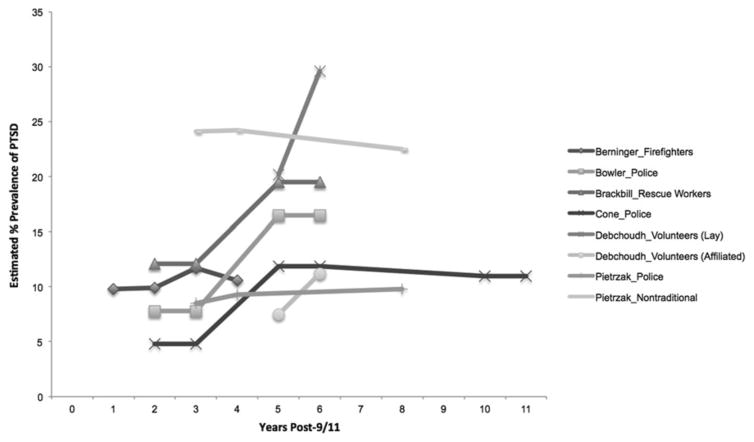
Eight of the 13 epidemiological reports reviewed concerned first responders and rescue and recovery workers, representing the greatest concentration of longitudinal studies of high-exposure populations affected by 9/11 (see Fig. 1). Prevalence rates for probable PTSD varied among these eight studies depending on when data were collected, as well as by responder type (see Table 1). Studies of traditional first responders (e.g. police, firefighters) within the first 4 years found little change in rates of probable PTSD, remaining steady at between approximately 8% and 12% (Brackbill et al. 2009; Berninger et al. 2010a, b). For most longitudinal studies that included later time periods, notable increases were present at 5–6 years post-9/11 relative to earlier time points, with estimated prevalence of probable PTSD at this later time point increasing from 4.8% to 7.8% to the higher rate of 7.4–16.5% (Brackbill et al. 2009; Bowler et al. 2012; Cone et al. 2015). An exception was Pietrzak et al. (2014), who found an increase of <1% from approximately years 3 to 6 post-9/11 among police responders (8.5% and 9.3%, respectively). We found only two studies that tracked longitudinal data across time points later than 6 years. Both found rates of PTSD of approximately 10% at year 6 post-9/11 and little change between year 6 and years 8–10 among police responders (Pietrzak et al. 2014; Cone et al. 2015).
Fig. 1.
Prevalence of estimated PTSD of first responders/rescue recovery workers by study. Multiple articles using the same data set are listed only once. Zvolensky et al. (2015) was excluded due to lack of information regarding specific time points. Studies that used a range of time points (e.g. data collected at 2–3 years post-9/11) include notation at the both upper and lower ranges.
Three longitudinal studies directly compared probable PTSD prevalence in traditional (e.g. policemen and firefighters) v. non-traditional (e.g. volunteer) responders. They found markedly higher prevalence of probable PTSD among non-traditional responders. The studies, however, differed somewhat with regard to course of PTSD. Zvolensky et al. (2015), who used variable beginning and follow-up time points, found an average increase in probable PTSD prevalence from 11.7% to 13.0% for traditional responders as compared with an increase from 16.4% to 17.2% among non-traditional responders as measured after an interval of approximately 2.5 years following visit 1. Debchoudhury et al. (2011) examined changes from years 3 to 4 post-9/11 to years 5–6 post-9/11, finding increase in probable prevalence from 20.2% to 29.6% among lay volunteers, and from 7.5% to 11.2% among affiliated volunteers (i.e. those affiliated with the Red Cross or other similar relief organization). Pietrzak et al. (2014) found that prevalence of probable PTSD decreased among non-traditional responders across years 3 and 8 post-9/11 from 24.1% to 22.5%, but increased from 8.5% to 9.8% among traditional responders over the same time interval.
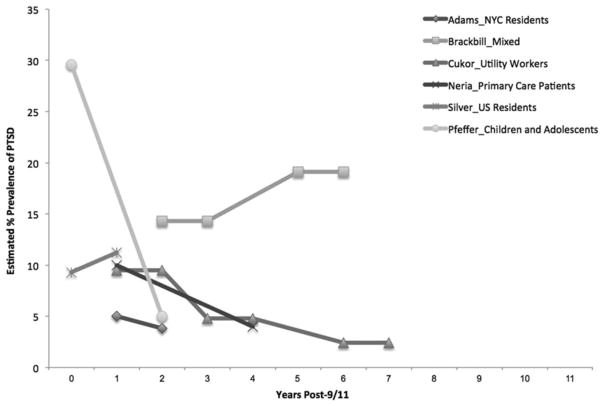
Other populations
Five longitudinal epidemiological studies concerned other populations directly exposed to the attacks. These studies found decreasing prevalence of probable PTSD over time (see Fig. 2). Adams & Boscarino (2006) found a decrease from 5% to 3.8% from 1 to 2 years post-9/11 in a sample of NYC residents. Cukor et al. (2011), who examined rates of PTSD in utility workers who assisted in cleanup, but not rescue and recovery, found decreasing rates of PTSD from years 1 to 2 through years 6–7 post-9/11. Specific results of this study varied by the rating instrument for PTSD, but indicated a steady decline over time. A study of primary care patients reported reductions in rates of probable PTSD from approximately 10% to 4% from years 1 to 4 post-9/11 (Neria et al. 2010). Pfeffer et al. (2007), who conducted the only longitudinal study with children directly exposed to the events of 9/11, found that the prevalence of probable PTSD declined from 30% at 4 months post-9/11 to about 5% at 2 years. Silver et al. (2005a) found increasing rates of trauma symptoms in those directly exposed in NYC and Washington, DC. They found a 9.3% prevalence of probable acute stress disorder among those highly exposed 2 weeks following 9/11, and an 11.2% prevalence of probable PTSD after 1 year. An additional study, which included both first responders and other NYC residents, found increasing rates of probable PTSD from 14.3% at 2–3 post-9/11 to 19.1% 5–6 years post-9/11 and showed increasing rates for all responder and non-responder populations over time (Brackbill et al. 2009). With the exception of studies focusing on rescue and recovery workers, no longitudinal study reported data following year 4 post-9/11 (see Table 1).
Fig. 2.
Prevalence of estimated PTSD for non-first responders/rescue recovery workers by study. Silver et al. (2005a) estimated acute stress disorder, rather than PTSD, for the first time point. Studies that used a range of time points (e.g. data collected at 2–3 years post-9/11) include notation at the both upper and lower ranges.
PTSD correlates
As can be seen in Table 2, the primary risk factor for PTSD across most studies was trauma exposure, with greater severity and amount of trauma exposure associated with higher likelihood of PTSD (Adams & Boscarino, 2006; Brackbill et al. 2009; Berninger et al. 2010a; Bowler et al. 2012; Pietrzak et al. 2014; Zvolensky et al. 2015). Other notable risk factors included bereavement/traumatic loss (Pfeffer et al. 2007; Brackbill et al. 2009; Berninger et al. 2010a), female gender (Silver et al. 2005a; Adams & Boscarino, 2006; Bowler et al. 2012; Zvolensky et al. 2015), and Hispanic or Latino ethnicity (Adams & Boscarino, 2006; Bowler et al. 2012; Pietrzak et al. 2014; Zvolensky et al. 2015). Previous trauma exposure or other history of psychopathology, low social support, and recent life stressors or ongoing stress post-9/11 was found to contribute to chronicity of PTSD (Silver et al. 2005a; Adams & Boscarino, 2006; Pfeffer et al. 2007; Neria et al. 2010; Cukor et al. 2011; Bowler et al. 2012; Pietrzak et al. 2014; Cone et al. 2015; Zvolensky et al. 2015). Notably, a repeat finding among longitudinal studies of first responders and rescue and recovery workers, whether traditional or non-traditional, was physical impairment and/or job loss related to 9/11 as a correlate of PTSD (Brackbill et al. 2009; Berninger et al. 2010a, b; Bowler et al. 2012; Pietrzak et al. 2014; Cone et al. 2015; Zvolensky et al. 2015).
Treatment studies
We identified seven studies examining efficacy and/or effectiveness of various treatment approaches to PTSD related to 9/11 (see Table 3). Two treatment studies were conducted with children and adolescents under the auspices of the Child and Adolescent Treatment Services (CATS) Consortium, aiming to deliver evidence-based, trauma-focused treatment to New York youth and study the implementation processes of these services (CATS Consortium, 2007). In one study involving 306 children, brief cognitive–behavioral therapy (CBT) or trauma-specific CBT was provided based on level of symptom severity, with significant clinical improvement in both groups (CATS Consortium, 2010). In a similar study, both trauma-specific CBT and Tell-Me-A-Story Narrative Trauma Therapy (TEMAS-NTT) were shown to be effective in a sample of 131 children, with TEMAS-NTT possibly showing some advantages for younger children and Hispanic children (Costantino et al. 2014). Although conclusions suggested the utility of treatment approaches established within existing school environs (CATS Consortium, 2007), findings regarding efficacy are limited mostly by lack of control group and randomization.
Table 3.
Treatment of PTSD in highly exposed 9/11 populations
| Source and study design | Sample | Time frame of data collection post-9/11 | PTSD instrument | Treatment conditions | Outcomes | Average reduction in scoresa |
|---|---|---|---|---|---|---|
| CATS Consortium (2010) (quasi-experimental) | NYC youths aged 5–21 (n = 306) | 1–4 years | PTSD-RI (trauma-specific CBT >25, brief CBT skills <25) | Trauma-specific CBT, brief CBT skills training (assignment depending on symptom severity) | Both groups showed improvement | Trauma-specific CBT: 14.88 CBT skills training: 7.93 |
| Costantino et al. (2014) (quasi-experimental) | Hispanic/Latino NYC public schoolchildren (n = 131) | 2–4 years | PTSD-RI (cut-off score 25) | TF-CBT v. TEMAS-NTT | TF-CBT and TEMAS-NTT effective in reducing PTSD, depression, and anxiety. TEMAS-NTT possibly better for younger children | TF-CBT: 15.82 TEMAS-NTT: 19.89 |
| Difede et al. (2006) (experimental) | NYC residents (n = 17) | Not reported | CAPS | Virtual reality v. waitlist control | VR is effective, may be especially effective for those who did not succeed with imaginal exposure | VR = 1.53 (reported effect size) Waitlist = N.S. |
| Difede et al. (2007) (experimental) | Disaster relief workers (n = 31) | 7 months to 3 years | CAPS (cut-off score 30), PCL | Exposure-based CBT v. TAU | CBT effective in reducing symptoms; drop-out rate relatively high | CBT = 24.86 (CAPS), 14.28 (PCL) TAU = 2.43 (CAPS), 5.38 (PCL) |
| Levitt et al. (2007) (quasi-experimental) | NYC residents with direct or indirect exposure (n = 59) | 1 year | MPSS-SR | CBT (STAIR/MPE) | Significant reduction of PTSD and depression, improved functioning | 36 |
| Schneier et al. (2012) (experimental) | NYC residents (n = 37) | 3–8 years | CAPS (cut-off score 50), PCL | PE + SSRI v. PE + placebo | Combined treatment more efficacious | PE + SSRI: 42.2 PE + placebo: 37.5 |
| Silver et al. (2005b) (quasi-experimental) | NYC residents with direct or indirect exposure (n = 65) | 2–48 weeks | IES-R (cut-off score 45) | EMDR (early: 2–10 weeks post-9/11; late: 30–48 weeks post-9/11) | Significant reduction in anxiety, depression, and PTSD symptoms | 22.8 |
CAPS, Clinician-Administered PTSD Scale; CBT, cognitive–behavioral therapy; EMDR, eye movement desensitization and reprocessing therapy; IES-R, Impact of Event Scale; MPSS-SR, Modified PTSD Symptom Scale Self-Report; N.S., non-significant; NYC, New York City; PCL, PTSD Checklist; PE, prolonged exposure; PTSD, post-traumatic stress disorder; PTSD-RI, PTSD Reaction Index; STAIR/MPE, Skills Training in Affective and Interpersonal Regulation/Modified Prolonged Exposure; TAU, treatment as usual; TEMAS-NTT, Tell-Me-A-Story Narrative Trauma Therapy; TF-CBT, trauma-focused CBT; VR, virtual reality.
All reported scores represented a significant difference (p < 0.05) unless otherwise specified.
Among studies of highly exposed adults, only three were randomized controlled trials, and all three had relatively small samples. In the sole treatment study focusing on rescue and recovery workers, Difede et al. (2007) found that symptoms significantly improved for patients who received exposure-based treatment as compared with treatment-as-usual (n = 31). The authors noted a relatively high drop-out rate (40%) compared with other studies using exposure therapies. Schneier et al. (2012) studied 37 patients with 9/11-related PTSD, finding that prolonged exposure (PE) therapy combined with the selective serotonin reuptake inhibitor (SSRI) paroxetine was more efficacious than PE plus placebo. Finally, in a pilot study of 17 participants investigating the efficacy of virtual reality (VR) exposure therapy v. wait-list control, Difede et al. (2006) found evidence that VR may be an effective tool for exposure, particularly for patients who previously experienced difficulty with imaginal procedures. Two other treatment studies did not use a control group. In an open trial of eye movement desensitization and reprocessing therapy, improvement was noted in a sample of 65 patients (Silver et al. 2005b). In a second open trial, a flexibly applied modified manualized CBT approach resulted in improvement in a study involving 59 patients (Levitt et al. 2007).
Discussion
The goal of this review was to clarify the longitudinal prevalence, course, and correlates of PTSD in high-exposure populations during the 15 years since 9/11. Although previous reviews of PTSD related to man-made disasters have noted the importance of longitudinal data and its scarcity (Pfefferbaum et al. 2004; Bills et al. 2008; Neria et al. 2008, 2011; Wilson, 2015; Garcia-Vera et al. 2016), this is the first systematic review of longitudinal studies of 9/11-related PTSD and probable PTSD. We also reviewed treatment studies, which serve to elucidate the course of PTSD in the context of clinical care and the efficacy and effectiveness of interventions for 9/11-related PTSD. We have purposefully focused on longitudinal studies, to the exclusion of cross-sectional examinations, so as not to be encumbered by concerns generated by combining disparate data, and confusing causal inference, that limit previous reviews (Susser et al. 2006; Galea & Maxwell, 2009; Garcia-Vera et al. 2016).
A number of conclusions may be drawn from our review. Overall prevalence of PTSD following 9/11 appears to be relatively high in the period directly following the attacks, particularly for those with the greatest levels of traumatic exposure. These rates appear to decline over time for the majority. The exception is first responders and rescue/recovery workers, who appear to have had lower PTSD prevalence than other populations in the first 3 years following 9/11, but show substantial increase in prevalence after that point. Conclusions regarding longer term prevalence are limited, as only two studies considered time points for this population later than 6 years, but available studies suggest that rates of PTSD may peak at 5 or 6 years post-9/11. A similar trend was found for non-traditional responders, except that prevalence of PTSD among non-traditional responders is markedly higher than for traditional responders. Initially, lower but increasing rates of PTSD among traditional responders may result from resistance to help-seeking behavior and under-reporting, and possibly due to the nature of training and preparedness. These possibilities have been discussed in prior literature addressing trauma in first responders, with no clear satisfactory conclusion reached (Pietrzak et al. 2014). More nuanced longitudinal data are needed to better explore the extent and nature of exposure and its relationship to PTSD prevalence, as well as stigma and other factors that may affect epidemiological inquiry. The higher prevalence of PTSD among non-traditional responders might be explained by greater vulnerability due to lower levels of training and support, but more research is likewise needed to better understand this phenomenon.
Risk factors reviewed here are consistent with earlier reviews (Neria et al. 2008) that identified exposure intensity as a primary risk factor. An important finding drawn from the longitudinal studies concerning first responders was that 9/11-related injury and job loss are important factors in chronicity of PTSD. This finding is consistent with results of a cross-sectional study conducted 10 years post-9/11, which found health-related unemployment to be the greatest predictor of chronic PTSD (Caramanica et al. 2014). Risk factors for chronic PTSD are not well understood, but some evidence suggests that constant, negative reminders of the trauma, such as physical pain, may be a comorbid expression of the disorder and/or help maintain it (Brennstuhl et al. 2015).
Our findings regarding prevalence and declining course of probable PTSD are consistent with data collected across multiple disaster types (Neria et al. 2008) and specifically in regard to terrorist attacks (Garcia-Vera et al. 2016). However, prior findings regarding first responders and rescue and recovery workers in the context of natural and man-made disasters are mixed, with significant disparities in reported PTSD prevalence and course across studies. Presented theories across contexts alternatively suggest enhanced resilience among first responders due to greater preparedness and professional training, higher risk for PTSD due to increased exposure, or both (Neria et al. 2008; McCaslin et al. 2009). Nonetheless, there appears to be agreement on a prevalence rate of approximately 10% for PTSD among rescue and recovery workers, and suggestion that rates of PTSD typically decline (Neria et al. 2008; Berger et al. 2012). This estimate is consistent with a recent cross-sectional findings among first responders conducted an average of 12 years after 9/11 (Bromet et al. 2016), although others, which combine first responders with other populations, indicate higher rates (Caramanica et al. 2014). While it remains beyond the scope of the current effort to fully disentangle the factors that affect observed rates of PTSD across studies of first responders and rescue and recovery workers across disasters, lack of clarity is likely exacerbated by a tendency to pool results of cross-sectional and longitudinal studies, as well as those involving disparate populations (e.g. traditional v. non-traditional responders).
The overall lack of longitudinal studies 15 years post-9/11 is disappointing. We identified 45 epidemio-logical articles concerning PTSD in those highly exposed to 9/11 in the process of conducting the literature review for the present study. Of these, only 13, less than one-third, have been identified as longitudinal in design. Furthermore, a drawback of the available longitudinal data is that the bulk of these studies were collected on only one highly exposed subpopulation. First responders and rescue and recovery workers are certainly an important group that deserves resources and attention, but one that has come to be disproportionately represented in the 9/11 literature to the exclusion of other groups. Children and adolescents, for example, were the subject of only one longitudinal study, limited by small sample size and limited to 2 years post-9/11, despite possible unique vulnerabilities in this population, as well as additional areas of concern including impact on developmental trajectory and risk for later psychopathology. Similarly, we found only three studies that considered NYC residents (Silver et al. 2005a; Adams & Boscarino, 2006; Brackbill et al. 2009) and no studies that focused exclusively on highly exposed NYC residents. Available longitudinal studies are also limited by length of follow-up, as only a very few to date extend beyond 6 years. In addition, though a small number of articles make reference to resilient groups or possible factors that may affect resilience (Berninger et al. 2010b; Bowler et al. 2012; Pietrzak et al. 2014), such as social support, to our knowledge little data are available considering factors affecting resilience. While risk factors remain an important area of focus, resiliency data represents an important counterpoint to such data.
As noted, we found very few treatment studies, and of these, most used small samples, many utilized a quasi-experimental design rather than a randomized controlled trial, and none conducted follow-up analyses. It remains particularly surprising that no treatment study was developed to treat PTSD in first responders specifically, especially considering the efforts made to create registries and develop resources for first responders, which limits knowledge regarding effective interventions in first responders following mass-scale terrorist events. Others have also commented on this unfortunate dearth (Foa et al. 2005; Bills et al. 2008; Haugen et al. 2012). The small number of treatment studies found parallels the lack of adequate quantity of longitudinal investigations.
Despite these limitations, available treatment studies broadly demonstrate the effectiveness of mental health treatment for traumatized individuals within the context of a national disaster. Exposure-based approaches to PTSD were further validated (Silver et al. 2005b; Difede et al. 2007; Levitt et al. 2007), including approaches utilizing VR technology (Difede et al. 2006) and deliveries in conjunction with SSRI medication (Schneier et al. 2012). The few available studies on psychotherapy with children and adolescents support school- and community-based initiatives (CATS Consortium, 2010; Costantino et al. 2014). These findings are consistent with previous efforts suggesting the utility of exposure-based approaches for the treatment of PTSD following disasters (Lopes et al. 2014). Unfortunately, as with the 9/11 literature, data are limited given the very small number of treatment studies of those exposed to disasters, whether natural or man-made, including with first responders or rescue/recovery workers, that utilize randomized controlled trials (RCT; Haugen et al. 2012; Lopes et al. 2014). The lack of RCTs in the area of disaster literature is a recognized problem, as without such efforts it remains unknown whether the efficacy of exposure therapy established in other contexts truly translates to those exposed to disaster-related trauma. The logistical difficulties of organizing an RCT in the aftermath of disasters is undoubtedly considerable, as has been noted elsewhere (Difede & Cukor, 2009). Nonetheless, that the prevalence of probable PTSD has continued so many years after 9/11 suggests that such efforts are worthwhile, even if they are not implemented in the immediate aftermath of a disaster.
In summary, despite the relatively small amount of available longitudinal research, these data may shed unique light on course of PTSD following 9/11 in populations highly exposed to 9/11, particularly traditional and non-traditional responders. Our review highlights the importance of longitudinal studies when disaster strikes, as such design is less vulnerable to the variability concerns common to cross-sectional investigations that span disparate time points and populations. Our review further underscores the importance of greater investment in not just using large registries for data tracking following large-scale disasters, but also connecting victim to treatment and measuring the outcome of interventions. The overwhelming focus on cross-sectional investigations, to the exclusion of longitudinal and treatment studies, suggests that such are perhaps easier or more affordable for investigators to complete; this likelihood implies the need for greater, more comprehensive, and more organized funding and direction of research efforts in the event of grand-scale disasters such as 9/11.
Although we cannot make a definitive statement absent direct statistical comparison, we believe the data presented here are less highly variable than the typical range ubiquitous among cross-sectional data from trauma-related studies of 9/11 and other disasters. Nonetheless, a limitation of this review is that methodology was not consistent across the individual studies, with regard to sampling methods, sample size, measurement of PTSD, adjustment for loss to follow-up in the longitudinal studies, and use of controls. This likely contributed to variability and suggests caution in interpretation of composite estimates. The extent of overlap between populations across epidemiological and treatment studies is also unknown. The use of self-report data and other limited assessment techniques by the majority of studies limits conclusions that may be drawn regarding actual rates of PTSD. In particular, some apparent symptoms of PTSD may overlap with respiratory or other medical conditions for some respondents. Sex differences in rates of PTSD were not discussed here for reason of inconsistent reporting in previous studies, and variability of the significance of sex as a correlate of PTSD was also a factor; however, sex differences in rates of PTSD is a known phenomenon that would likely benefit from further consideration in the context of exposure to man-made disasters. Another limitation is that most studies used retrospective assessment of exposure and risk factors. This makes the information on exposure and related factors susceptible to recall bias. An additional limitation is that generalizability from high-exposure populations to other populations is limited. Future research should put greater emphasis on longitudinal studies, include treatment outcomes, and collect data on biomarkers, rather than focus solely on epidemiological data. Although prevalence, course, and risk factors are all of interest in PTSD research, enhanced knowledge of the role of biological factors and of effective components of PTSD treatment may serve to exponentially benefit those exposed to large-scale traumatic events.
Acknowledgments
Dr Suarez-Jimenez’s work was supported by a NIMH T32 MH015144 grant. Dr Neria’s work was supported by the New York State Psychiatric Institute, and NIMH RO1 MHO72833 grant.
References
- Adams RE, Boscarino JA. Predictors of PTSD and delayed PTSD after disaster: the impact of exposure and psychosocial resources. The Journal of Nervous and Mental Disease. 2006;194:485–493. doi: 10.1097/01.nmd.0000228503.95503.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews B, Brewin CR, Philpott R, Stewart L. Delayed-onset posttraumatic stress disorder: a systematic review of the evidence. American Journal of Psychiatry. 2007;164:1319–1326. doi: 10.1176/appi.ajp.2007.06091491. [DOI] [PubMed] [Google Scholar]
- Berger W, Coutinho ESF, Figueira I, Marques-Portella C, Luz MP, Neylan TC, Marmar CR, Mendlowicz MV. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social Psychiatry and Psychiatric Epidemiology. 2012;47:1001–1011. doi: 10.1007/s00127-011-0408-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berninger A, Webber MP, Cohen HW, Gustave J, Lee R, Niles JK, Chiu S, Zeig-Owens R, Soo J, Kelly K, Prezant DJ, et al. Trends of elevated PTSD risk in firefighters exposed to the World Trade Center disaster: 2001–2005. Public Health Reports. 2010a;125:556–566. doi: 10.1177/003335491012500411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berninger A, Webber MP, Niles JK, Gustave J, Lee R, Cohen HW, Kelly K, Corrigan M, Prezant DJ. Longitudinal study of probable post-traumatic stress disorder in firefighters exposed to the World Trade Center disaster. American Journal of Industrial Medicine. 2010b;53:1177–1185. doi: 10.1002/ajim.20894. ( http://www.ncbi.nlm.nih.gov/pubmed/20862700) [DOI] [PubMed] [Google Scholar]
- Bills CB, Levy NAS, Sharma V, Charney DS, Herbert R, Moline J, Katz CL. Mental health of workers and volunteers responding to events of 9/11: review of the literature. The Mount Sinai Journal of Medicine. 2008;75 doi: 10.1002/msj.20026. 173–115–127. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. ( http://www.ncbi.nlm.nih.gov/pubmed/7712061) [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bowler RM, Harris M, Li J, Gocheva V, Stellman SD, Wilson K, Alper H, Schwarzer R, Cone JE. Longitudinal mental health impact among police responders to the 9/11 terrorist attack. American Journal of Industrial Medicine. 2012;55:297–312. doi: 10.1002/ajim.22000. [DOI] [PubMed] [Google Scholar]
- Brackbill RM, Hadler JL, DiGrande L, Ekenga CC, Farfel MR, Friedman S, Perlman SE, Stellman SD, Walker DJ, Wu D, Yu S, Thorpe LE. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA. 2009;302:502–516. doi: 10.1001/jama.2009.1121. [DOI] [PubMed] [Google Scholar]
- Brennstuhl MJ, Tarquinio C, Montel S. Chronic pain and PTSD: evolving views on their comorbidity. Perspectives in Psychiatric Care. 2015;51:295–304. doi: 10.1111/ppc.12093. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community : the 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, McNally RJ. The epidemiology of 9–11: technical advances and conceptual conundrums. In: Neria Y, Gross R, Marshall RD, editors. 9/11: Mental Health in the Wake of Terrorist Attacks. Cambridge University Press; Cambridge, UK: 2008. pp. 521–528. [Google Scholar]
- Bromet EJ, Hobbs MJ, Clouston SAP, Gonzalez A, Kotov R, Luft BJ. DSM-IV post-traumatic stress disorder among World Trade Center responders 11–13 years after the disaster of 11 September 2001 (9/11) Psychological Medicine. 2016;46:771–783. doi: 10.1017/S0033291715002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caramanica K, Brackbill RM, Liao T, Stellman SD. Comorbidity of 9/11-related PTSD and depression in the World Trade Center health registry 10–11 years postdisaster. Journal of Traumatic Stress. 2014;27:680–688. doi: 10.1002/jts.21972. [DOI] [PubMed] [Google Scholar]
- CATS Consortium. Implementing CBT for traumatized children and adolescents after September 11: lessons learned from the Child and Adolescent Trauma Treatments and Services (CATS) Project. Journal of Clinical Child and Adolescent Psychology : the Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2007;36:581–592. doi: 10.1080/15374410701662725. ( http://www.ncbi.nlm.nih.gov/pubmed/18088216) [DOI] [PubMed] [Google Scholar]
- CATS Consortium. Implementation of CBT for youth affected by the World Trade Center disaster: matching need to treatment intensity and reducing trauma symptoms. [Accessed 6 January 2016];Journal of Traumatic Stress. 2010 23:699–707. doi: 10.1002/jts.20594. ( http://www.mendeley.com/catalog/implementation-cbt-youth-affected-world-trade-center-disaster-matching-need-treatment-intensity-redu/) [DOI] [PubMed] [Google Scholar]
- Comer JS, Kendall PC. Terrorism: the psychological impact on youth. Clinical Psychology: Science and Practice. 2007;14:179–212. [Google Scholar]
- Cone JE, Li J, Kornblith E, Gocheva V, Stellman SD, Shaikh A, Schwarzer R, Bowler RM, Mph Ã. Chronic probable PTSD in police responders in the World Trade Center Health Registry ten to eleven years after 9/11. American Journal of Industrial Medicine. 2015;58:483–493. doi: 10.1002/ajim.22446. [DOI] [PubMed] [Google Scholar]
- Costantino G, Primavera LH, Malgady RG, Costantino E. Culturally oriented trauma treatments for Latino children post 9/11. Journal of Child and Adolescent Trauma. 2014;7:247–255. [Google Scholar]
- Cukor J, Wyka K, Mello B, Olden M, Jayasinghe N, Roberts J. The longitudinal course of PTSD among disaster worker deployed to the World Trade Center following the attacks of September 11th. Journal of Traumatic Stress. 2011;24:506–514. doi: 10.1002/jts.20672. [DOI] [PubMed] [Google Scholar]
- Debchoudhury I, Welch AE, Fairclough MA, Cone JE, Brackbill RM, Stellman SD, Farfel MR. Comparison of health outcomes among affiliated and lay disaster volunteers enrolled in the World Trade Center Health Registry. Preventive Medicine. 2011;53:359–363. doi: 10.1016/j.ypmed.2011.08.034. ( http://dx.doi.org/10.1016/j.ypmed.2011.08.034) [DOI] [PubMed] [Google Scholar]
- Difede J, Cukor J. Evidence-based long-term treatment of mental health consequences of disasters among adults. In: Neria Y, Galea S, Norris FH, editors. Mental Health and Disasters. Cambridge University Press; Cambridge: 2009. [Accessed 23 March 2017]. pp. 336–349. ( http://ebooks.cambridge.org/ref/id/CBO9780511730030A033) [Google Scholar]
- Difede J, Cukor J, Patt I, Giosan C, Hoffman H. The application of virtual reality to the treatment of PTSD following the WTC attack. Annals of the New York Academy of Sciences. 2006;1071:500–501. doi: 10.1196/annals.1364.052. ( http://doi.wiley.com/10.1196/annals.1364.052) [DOI] [PubMed] [Google Scholar]
- Difede J, Malta LS, Best S, Henn-Haase C, Metzler T, Bryant R, Marmar C. A randomized controlled clinical treatment trial for World Trade Center attack-related PTSD in disaster workers. The Journal of Nervous and Mental Disease. 2007;195:861–865. doi: 10.1097/NMD.0b013e3181568612. ( http://www.ncbi.nlm.nih.gov/pubmed/18043528) [DOI] [PubMed] [Google Scholar]
- DiGrande L, Neria Y, Brackbill RM, Pulliam P, Galea S. Long-term posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. American Journal of Epidemiology. 2011;173:271–281. doi: 10.1093/aje/kwq372. ( http://aje.oxfordjournals.org/cgi/doi/10.1093/aje/kwq372) [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV, Axis I Disorders, Non-Patient Edition (SCID-N/P, Version 2.0) New York State Psychiatric Institute, Department of Biometrics Research; New York, NY: 1995. [Google Scholar]
- Foa EB, Cahill SP, Boscarino JA, Hobfoll SE, Lahad M, Mcnally RJ, Solomon Z. Social, psychological, and psychiatric interventions following terrorist attacks: recommendations for practice and research. Neuropsychopharmacology. 2005;30:1806–1817. doi: 10.1038/sj.npp.1300815. [DOI] [PubMed] [Google Scholar]
- Galea S, Maxwell AR. Methodological challenges in studying the mental health consequences of disasters. In: Neria Y, Galea S, Norris FH, editors. Mental Health and Disasters. Cambridge University Press; Cambridge: 2009. [Accessed 13 March 2017]. pp. 579–593. ( http://ebooks.cambridge.org/ref/id/CBO9780511730030A049) [Google Scholar]
- Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. [Accessed 16 May 2016];Epidemiologic Reviews. 2005 27:78–91. doi: 10.1093/epirev/mxi003. ( http://epirev.oxfordjournals.org/content/27/1/78.full) [DOI] [PubMed] [Google Scholar]
- Galea S, Vlahov D, Resnick H, Ahern J, Susser E, Gold J, Bucuvalas M, Kilpatrick D. Trends of probable post-traumatic stress disorder in New York City after the September 11 terrorist attacks. American Journal of Epidemiology. 2003;158:514–524. doi: 10.1093/aje/kwg187. [DOI] [PubMed] [Google Scholar]
- Garcia-Vera MP, Sanz J, Gutierrez S. A systematic review of the literature on posttraumatic stress disorder in victims of terrorist attacks. [Accessed 22 March 2017];Psychological Reports. 2016 119:328–359. doi: 10.1177/0033294116658243. ( http://prx.sagepub.com/lookup/doi/10.1177/0033294116658243) [DOI] [PubMed] [Google Scholar]
- Haugen PT, Evces M, Weiss DS. Treating posttraumatic stress disorder in first responders: a systematic review. Clinical Psychology Review. 2012;32:370–380. doi: 10.1016/j.cpr.2012.04.001. ( http://dx.doi.org/10.1016/j.cpr.2012.04.001) [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. [Accessed 10 July 2014];Archives of General Psychiatry. 2005 62:593–602. doi: 10.1001/archpsyc.62.6.593. ( http://www.ncbi.nlm.nih.gov/pubmed/15939837) [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. [Accessed 20 July 2015];Archives of General Psychiatry. 1995 52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. ( http://www.ncbi.nlm.nih.gov/pubmed/7492257) [DOI] [PubMed] [Google Scholar]
- Kunreuther H, Michel-Kerjan E, Porter B. [Accessed 16 February 2016];Assessing, Managing, and Financing Extreme Events: Dealing with Terrorism. 2003 ( http://www.nber.org/papers/w10179)
- Levitt JT, Malta LS, Martin A, Davis L, Cloitre M. The flexible application of a manualized treatment for PTSD symptoms and functional impairment related to the 9/11 World Trade Center attack. Behaviour Research and Therapy. 2007;45:1419–1433. doi: 10.1016/j.brat.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Liu B, Tarigan LH, Bromet EJ, Kim H. World trade center disaster exposure-related probable posttraumatic stress disorder among responders and civilians: a meta-analysis. PLoS ONE. 2014;9:e101491. doi: 10.1371/journal.pone.0101491. ( http://dx.plos.org/10.1371/journal.pone.0101491) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes AP, Macedo TF, Coutinho ESF, Figueira I, Ventura PR. Systematic review of the efficacy of cognitive-behavior therapy related treatments for victims of natural disasters: a worldwide problem L. Chao, ed. [Accessed 23 March 2017];PLoS ONE. 2014 9:e109013. doi: 10.1371/journal.pone.0109013. ( http://dx.plos.org/10.1371/journal.pone.0109013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaslin SE, Inslicht SS, Henn-Haase C, Chemtob C, Metzler TJ, Neylan TC, Marmar CR. Uniformed rescue workers responding to disaster. In: Neria Y, Galea S, Norris FH, editors. Mental Health and Disasters. Cambridge University Press; Cambridge: 2009. [Accessed 22 March 2017]. pp. 302–318. ( http://ebooks.cambridge.org/ref/id/CBO9780511730030A030) [Google Scholar]
- Neria Y, DiGrande L, Adams BG. Posttraumatic stress disorder following the September 11, 2001, terrorist attacks: a review of the literature among highly exposed populations. American Psychologist. 2011;66:429–446. doi: 10.1037/a0024791. ( http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3386850&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. [Accessed 17 May 2016];Psychological Medicine. 2008 38:467–480. doi: 10.1017/S0033291707001353. ( http://www.ncbi.nlm.nih.gov/pubmed/17803838) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y, Olfson M, Gameroff MJ, DiGrande L, Wickramaratne P, Gross R, Pilowsky DJ, Neugebaur R, Manetti-Cusa J, Lewis-Fernandez R, Lantigua R, Shea S, Weissman MM. Long-term course of probable PTSD after the 9/11 attacks: a study in urban primary care. Journal of Traumatic Stress. 2010;23:474–482. doi: 10.1002/jts.20544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- Perrin MA, Digrande L, Wheeler K, Thorpe L. Differences in PTSD prevalence and associated risk factors among world trade. American Journal of Psychiatry. 2007;164:1385–1394. doi: 10.1176/appi.ajp.2007.06101645. ( http://www.ncbi.nlm.nih.gov/pubmed/17728424) [DOI] [PubMed] [Google Scholar]
- Pfeffer CR, Altemus M, Heo M, Jiang H. Salivary cortisol and psychopathology in children bereaved by the September 11, 2001 terror attacks. Biological Psychiatry. 2007;61:957–965. doi: 10.1016/j.biopsych.2006.07.037. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum BJ, Devoe ER, Stuber J, Schiff M, Klein TP, Fairbrother G. Psychological impact of terrorism on children and families in the United States. Journal of Aggression, Maltreatment & Trauma. 2004;9:305–317. ( http://www.tandfonline.com/doi/abs/10.1300/J146v09n03_01) [Google Scholar]
- Pfefferbaum BJ, Weems CF, Scott BG, Nitiéma P, Noffsinger MA, Pfefferbaum RL, Varma V, Chakraburtty A. Research methods in child disaster studies: a review of studies generated by the September 11, 2001, terrorist attacks; the 2004 Indian Ocean Tsunami; and Hurricane Katrina. Child & Youth Care Forum. 2013;42:285–337. doi: 10.1007/s10566-013-9211-4. ( http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3892998&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, Reissman DB, Ozbay F, Sharma V, Crane M, Harrison D, Herbert R, Levin SM, Luft BJ, Moline JM, Stellman JM, Udasin IG, Landrigan PJ, Southwick SM. Trajectories of PTSD risk and resilience in World Trade Center responders: an 8-year prospective cohort study. Psychological Medicine. 2014;44:205–219. doi: 10.1017/S0033291713000597. ( http://journals.cambridge.org/action/displayFulltext?type=6&fid=9111650&jid=PSM&volumeId=44&issueId=01&aid=9111649&bodyId=&membershipNumber=&societyETOCSession=&fulltextType=RA&fileId=S0033291713000597) [DOI] [PubMed] [Google Scholar]
- Schneier FR, Neria Y, Pavlicova M, Hembree E, Suh EJ, Amsel L, Marshall RD. Combined prolonged exposure therapy and paroxetine for PTSD related to the World Trade Center attack: a randomized controlled trial. American Journal of Psychiatry. 2012;169:80–89. doi: 10.1176/appi.ajp.2011.11020321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V, Pizarro J. Coping with a national trauma: a nationwide longitudinal study of responses to the terrorist attacks of September 11th. In: Danieli Y, Brom D, Sills J, editors. 9/11: Mental Health in the Wake of Terrorist Attacks. The Haworth Maltreatment & Trauma Press, an imprint of The Haworth Press, Inc; 2005a. pp. 45–70. Trauma of Terrorism: Sharing Knowledge and Shared Care, An International Handbook. 2005. [Google Scholar]
- Silver SM, Rogers S, Knipe J, Colelli G. EMDR therapy following the 9/11 terrorist attacks: a community-based intervention project in New York City. International Journal of Stress Management. 2005b;12:29–42. [Google Scholar]
- Susser E, Schwartz S, Morabia A, Bromet EJ. Psychiatric Epidemiology. 1. Oxford University Press; New York: 2006. [Google Scholar]
- Tapp LC, Baron S, Bernard B, Driscoll R, Mueller C, Wallingford K. Physical and mental health symptoms among NYC transit workers seven and one-half months after the WTC attacks. American Journal of Industrial Medicine. 2005;47:475–483. doi: 10.1002/ajim.20177. [DOI] [PubMed] [Google Scholar]
- Wilson LC. A systematic review of probable posttraumatic stress disorder in first responders following man-made mass violence. Psychiatry Research. 2015;229:21–26. doi: 10.1016/j.psychres.2015.06.015. ( http://linkinghub.elsevier.com/retrieve/pii/S0165178115003637) [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Schechter CB, Gonzalez A, Vujanovic A, Pietrzak RH, Crane M, Kaplan J, Moline J, Southwick SM, Feder A, Udasin I, Reissman DB, Luft BJ. Post-disaster stressful life events and WTC-related posttraumatic stress, depressive symptoms, and overall functioning among responders to the World Trade Center disaster. Journal of Psychiatric Research. 2015;61:97–105. doi: 10.1016/j.jpsychires.2014.11.010. ( http://www.sciencedirect.com/science/article/pii/S0022395614003203) [DOI] [PubMed] [Google Scholar]