Abstract
Background
This study aimed to determine whether there were sensitive periods when a first exposure to trauma was most associated with emotion dysregulation in adulthood.
Methods
Adult participants came from a public urban hospital in Atlanta, GA (n=1,944). Lifetime trauma exposure was assessed using the Traumatic Events Inventory (TEI). Multiple linear regression models were used to assess the association between the developmental timing of first trauma exposure, classified as early childhood (ages 0-5), middle childhood (ages 6-10), adolescence (ages 11-18), and adulthood (ages 19+), on adult emotion dysregulation symptoms, measured using the abbreviated Emotion Dysregulation Scale.
Results
Participants exposed to trauma at any age had higher emotion dysregulation scores than their unexposed peers. However, participants first exposed to child maltreatment or interpersonal violence during middle childhood had higher emotion dysregulation scores relative to those first exposed during other developmental stages; these developmental timing differences were detected even after controlling for sociodemographic factors, exposure to other trauma, and frequency of exposure to trauma. Further, after controlling for current psychiatric symptoms, the effect of other interpersonal trauma exposure in middle childhood was diminished and first exposure to other interpersonal violence in early childhood was associated with significantly lower emotion dysregulation symptoms.
Limitations
Limitations of this study include the use of retrospective reports and absence of complete information about trauma severity or duration.
Conclusion
These findings should be replicated in other population-based samples with prospective designs to confirm the importance of developmental timing of trauma on later emotion dysregulation.
Keywords: sensitive periods, emotion regulation, emotion dysregulation, child maltreatment, trauma
Introduction
Emotion regulation, or the ability to effectively regulate one’s emotions, is a critical component of healthy social functioning and mental health (M. Berking & Wupperman, 2012; Gross & Thompson, 2007; Hu et al., 2014). Conversely, deficits in emotion regulation, or emotion dysregulation, have been linked to many psychiatric disorders (Powers, Etkin, Gyurak, Bradley, & Jovanovic, 2015; Sheppes, Suri, & Gross, 2015), including borderline personality disorder (Carpenter & Trull, 2013), anxiety disorders (Jazaieri, Morrison, Goldin, & Gross, 2015), eating disorders (Lavender et al., 2015), substance-use disorders (Matthias Berking et al., 2011; Fox, Axelrod, Paliwal, Sleeper, & Sinha, 2007), depression (Ehring & Quack, 2010) and non-suicidal self-injury (Andover & Morris, 2014). Emotion dysregulation is defined by deficits in several areas, including the ability to monitor and evaluate one’s emotional experiences, modulate the intensity or duration of emotions, and/or to adaptively manage emotional reactions in order to meet situational demands (Cole, Michel, & Teti, 1994; Gross & Thompson, 2007). Indeed, the importance of emotion dysregulation for psychopathology risk is reflected in the fact that emotion regulation is encompassed in the negative valence, cognition, and social processing domain of the Research Domain Criteria (Murdock, Guarnaccia, Hayslip, & McKibbin) Initiative, a National Institutes of Mental Health (NIMH) effort to identify underlying transdiagnostic biobehavioral mechanisms responsible for psychopathology (Insel et al., 2010; Sanislow et al., 2010).
Trauma exposure, particularly child maltreatment (e.g., neglect, emotional, physical and sexual abuse), is one of the primary determinants of emotion dysregulation and as is also a known risk factor for psychiatric disorders, especially depression and PTSD (K.A. McLaughlin et al., 2012; K. A. McLaughlin et al., 2013). Prior studies have shown that trauma exposure is associated with deficits in emotion regulation across the lifespan, including during preschool (Langevin, Hebert, Allard-Dansereau, & Bernard-Bonnin, 2016), adolescence (Shields & Cicchetti, 1997; Vettese, Dyer, Li, & Wekerle, 2011) and adulthood (Briere & Rickards, 2007; Thompson, Hannan, & Miron, 2014). For example, preschool-age children exposed to sexual abuse have been shown to have emotion regulation scores that are, on average, one standard deviation below their unexposed peers (Langevin et al., 2016). These deficits appear patterned by frequency of trauma exposure, with children exposed to more chronic or frequent maltreatment having significantly worse outcomes relative to those who were never exposed or exposed to less chronic maltreatment (Thompson et al., 2014). Notably, relatively few studies have examined the relationship between other interpersonal or non-interpersonal trauma and emotion dysregulation. Efforts to understand the effects of trauma exposure on emotion dysregulation are needed, as epidemiological studies estimate that 70% of the world’s population (Benjet et al., 2016), including 40% of children under age thirteen (Koenen, Roberts, Stone, & Dunn, 2010), have experienced one or more traumatic events at some point in their lifetime.
Although these studies document the importance of trauma exposure, few studies have examined whether the effect of trauma exposure on emotion dysregulation varies based on the developmental timing of the trauma occurrence. Thus, it remains unclear whether there are “sensitive periods” (Bornstein, 1989; Dunn, McLaughlin, Slopen, Rosand, & Smoller, 2013; Hensch, 2004) for the development of emotion dysregulation, or windows of time when the developing human brain is especially vulnerable or sensitive to trauma and when trauma exposure thus leads to greater levels of emotion dysregulation. Greater insights about the possible existence of sensitive periods for emotion dysregulation are needed to help guide the investment of limited public health dollars towards possible “high-risk” stages when trauma may be particularly harmful and thus the “high-reward” periods when interventions could be most efficacious in promoting emotion regulation abilities.
The developmental timing of trauma exposure may be important in shaping emotion regulation for several reasons. Emotion regulation is known to develop in conjunction with cognition, rapidly maturing during early childhood (Calkins, 1994) and through the influence of observational learning, modeling, and social referencing (Morris, Silk, Steinberg, Myers, & Robinson, 2007). Broadly, exposure to stressful stimuli, such as a chaotic home environment and childhood maltreatment, may reduce exposure to adaptive emotional labeling, expression, and regulation behaviors often modeled in families (Parke, 1994) and thus disrupt, delay, or impede normative emotion regulation development (B. Bradley, DeFife, et al., 2011; Dvir, Ford, Hill, & Frazier, 2014; Kolk & Fisler, 1994). While parental responsiveness and encouragement of emotional expression promotes emotional development (Roberts & Strayer, 1987), living in an invalidating environment where emotional expression is ignored, rejected, or punished may lead to emotion dysregulation (Linehan, 1993). Prior studies have shown that physical and emotional availability of the mother in infancy are critical to emotion regulation development. Thus, infancy and early childhood may be a developmental period when emotional development is particularly malleable and highly affected by trauma exposure (Field, 1994). Conversely, trauma exposure during adolescence may be more deleterious, as adolescence is a period characterized by increased executive functioning and heightened social sensitivity, which can interact with changing social environments to greatly influence behavior and emotion regulation (Blakemore & Mills, 2014).
It is also possible that the developmental timing of trauma exposure from infancy to adolescence is unrelated to emotion dysregulation or that it depends on the type of trauma. Indeed, social adversities have been shown to disrupt maturing mechanisms of emotional regulation at multiple phases of development (in preschoolers: differentiation of basic emotions; in school-age children: elaboration on emotional expression; in adolescence: understanding of the origins and consequences of negative emotions) (Pynoos, Steinberg, & Piacentini, 1999). Collectively, these findings indicate there may be multiple sensitive periods to adversity in childhood and adolescence, perhaps depending on the type of trauma exposure, whereby the interaction between emotion regulation development and negative social exposures have differential, negative effects on future emotion dysregulation.
To our knowledge, only three studies have examined the effect of the developmental timing of trauma exposure on emotion dysregulation. In one prospective cohort study, Kim and colleagues found that children exposed to maltreatment between birth and 36 months (infancy and toddlerhood), but not those exposed after age 3 (preschool and school-age), had higher levels of emotion dysregulation at age 6-12 compared their unexposed peers (Kim & Cicchetti, 2010). A second study of children adopted from institutional care found that children adopted after age 15 months had higher levels of emotion dysregulation at age 8 compared to both those adopted before 15 months and a control group who was never institutionalized (Nim Tottenham et al., 2010; N. Tottenham & Sheridan, 2010). A third retrospective study found that children exposed to interpersonal trauma exposure between birth to age 14 had higher emotion dysregulation in adulthood, compared to children exposed to interpersonal trauma after age 14 or non-interpersonal traumas (Ehring & Quack, 2010). Taken together, these results suggest there may be differential effects of trauma on emotion dysregulation depending on timing of exposure as well as type of trauma.
The current study aimed to build upon prior work by assessing the impact of the developmental timing of trauma exposure on emotion dysregulation in adulthood using data from a cohort of urban African American adults with high trauma exposure. By studying adults, we could increase the likelihood that observed emotion regulation deficits are stable, and not potentially transient or confounded by variations in emotion regulation capabilities seen during their development (Calkins, 1994; McRae et al., 2012; Pynoos et al., 1999; Raffaelli, Crockett, & Shen, 2005). Our goals were to: 1) determine the extent to which different types of trauma exposure were associated with emotion dysregulation in adulthood; and 2) investigate whether timing of first trauma exposure was associated with emotion dysregulation in adulthood.
Methods
Sample and Procedures
Data came from the Grady Trauma Project (GTP), an ongoing NIMH-funded study of the genetic and environmental risk and protective factors for posttraumatic stress disorder (PTSD) and other psychiatric disorders (Binder et al., 2008; R. G. Bradley et al., 2008; B. M. Gillespie, Chaboyer, & Wallis, 2009; C. F. Gillespie, Phifer, Bradley, & Ressler, 2009). The GTP study recruited adults (ages 18-90) from general medical and obstetric/gynecological clinic waiting rooms at Grady Hospital in Atlanta, Georgia, a large public non-profit healthcare center. Grady Hospital primarily serves an African American, urban population from low socioeconomic backgrounds. This particular sample is beneficial to trauma research as there are high rates of trauma exposure, African Americans are an understudied population, and the sample is relatively homogeneous in terms of socioeconomic status. Eligibility criteria for participation included being at least 18 years old, not actively psychotic, and able to give written and verbal consent. Consenting individuals completed in-person interviews about their trauma history, current psychiatric symptoms, and general demographic information. Interviews were administered by trained research assistants and lasted approximately 45–75 minutes. Participants received $15 for their participation. All study procedures were approved by Emory University’s Institutional Review Board and the Grady Health Care System Research Oversight Committee.
The current analysis included 1944 African American adults who had complete data on all measures relevant to this analysis. This analytic sample represents 21.9% of the total GTP sample, who completed at least one item in the GTP study battery (N=8886). Participants were excluded from the analytic sample if they had incomplete exposure, outcome, or covariate data. Interviews were conducted in clinic waiting rooms and continued until participants or their family members were seen by the clinic, thus the majority of participants did not complete all study measures. Therefore, due to this unique design, we suspect it is unlikely that those who were excluded were systematically different from those who were included. Indeed, the distribution of age, education, and income did not differ significantly between the analytic sample and the total GTP sample (all p>0.05). However, relative to the analytic sample, the excluded sample did include more females (74.2% in analytic sample; 71.3% total sample; p=0.014) and people who were unemployed (28.9% in analytic sample; 32.8% total sample; p=0.0003). These analyses were restricted to African Americans because individuals from other racial/ethnic groups comprised only 7.1% of the sample. By restricting to one racial/ethnic group, we more effectively control for confounding by eliminating variability associated with race, which was important as the distribution of trauma exposure, covariates, and outcome varied significantly by race. Stratification by race would have resulted in low power to detect associations due to small cell counts.
Measures
Exposure to Trauma
Presence vs. absence of trauma exposure, age at first trauma exposure, and frequency of trauma occurrence were collected using the Traumatic Events Inventory (TEI), a 14-item screening measure that assessed lifetime history of trauma exposure (C. F. Gillespie, B. Bradley, et al., 2009; C. F. Gillespie, J. Phifer, et al., 2009; Schwartz et al., 2006; Schwartz, Bradley, Sexton, Sherry, & Ressler, 2005). We focused on 11 events that could plausibly occur in multiple developmental stages; the additional three events that were excluded from current analyses were military trauma, attacked by a romantic partner, and attacked by someone besides a romantic partner. These events were grouped into four trauma types, consistent with prior research (Breslau et al., 1998; K.A. McLaughlin et al., 2012): (1) child maltreatment (i.e., witnessing violence between parents or caregivers; being beaten; experiencing emotional abuse; or experiencing sexual abuse); (2) other interpersonal violence (i.e., witnessing or being confronted with a friend or family member being murdered; witnessing a family member or friend being attacked with or without a weapon; witnessing a non-family member or friend attacked with or without a weapon); (3) non-interpersonal trauma (i.e., experiencing a natural disaster; witnessing or experiencing a serious accident or injury; experiencing a sudden life threatening illness; and (4) other trauma (i.e., any other event or experience not covered by the previously stated categories that participants self-identified as a traumatic experience, including witnessing a death or suicide, bereavement, divorce or familial disruption, etc).
If a participant reported being exposed to a traumatic event, their age at first exposure (in years) was recorded. We grouped these ages of first exposure for each traumatic event into four stages: early childhood (age 0-5 years), middle childhood (6-10 years), adolescence (11-18 years), and adulthood (19+ years). These categories were used to match previous research and minimize recall bias, relative to studying specific years of age (Dunn et al., 2013).
Participants also reported the number of times they were exposed to a given traumatic event, on a categorical scale ranging from 0 (unexposed) to 8 (greater than 20 times). We used this information to create a frequency indicator for each traumatic event, designating low versus high frequency of occurrence. High frequency of occurrence was defined as greater than or equal to the 75th percentile for that specific trauma event. These frequency indicators were used as covariates in models examining developmental timing of exposure to account for the possibility that people exposed at younger ages were more likely have more occurrences of a given trauma and in acknowledgment that trauma exposure features (e.g., timing, frequency and severity) may have independent effects on psychopathology risk (Manly, Cicchetti, & Barnett, 1994; Manly, Kim, Rogosch, & Cicchetti, 2001).
Emotion Dysregulation
Emotion dysregulation was assessed using a shortened version of the Emotion Dysregulation Scale (Powers, Stevens, Fani, & Bradley, 2015), a 12-item scale that captures aspects of experiencing emotion, cognition, and behavior. The 12-item scale was adapted from an original 24-item version based on a clinician-rated Affect Regulation and Experience Q-sort Questionnaire (Conklin, Bradley, & Westen, 2006; Westen, Muderrisoglu, Fowler, Shedler, & Koren, 1997). Participants indicated on a Likert-type scale (1=not true; 7=very true) the extent to which they thought the item describes them. In this sample, total emotion dysregulation scores were calculated by averaging all individual items (where at least 11 were completed) and then multiplying that mean by 12 (range=12-84). Higher scores therefore indicated greater emotion dysregulation. The 12-item scale demonstrated excellent internal consistency reliability in this sample (standardized α coefficient=0.94) and good construct validity relative to the original scale (Powers, Stevens, et al., 2015). Sample items on this 12-item scale included: “When I’m upset, I have trouble thinking clearly,” “I have trouble soothing myself when I am upset,” and “When my emotions are strong, I often make bad decisions.”
Covariates
The following covariates were included in all analytic models: sex; age (continuous); highest level of education (less than 12th grade; high school graduate or GED; greater than high school graduate or GED/college graduate); household monthly income ($0-499; $500-999; $1,000+), and employment status (unemployed; unemployed receiving disability support; employed with or without disability support). We also adjusted for high (vs. low) levels of current depressive and posttraumatic symptoms based on responses to the Beck’s Depression Inventory - Second Edition (Beck, Steer, & Carbin, 1988) and (2): the Modified Posttraumatic Symptom Scale to assess PTSD symptoms (American Psychiatric Association, 2000; Coffey, Dansky, Falsetti, Saladin, & Brady, 1998). While emotion dysregulation is closely related to multiple forms of psychopathology, it is important to distinguish between the deficits in emotion regulation capacity and symptoms of mental illness. In particular, emotion dysregulation is found in individuals with high depressive and posttraumatic stress symptomatology (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Tull, Barrett, McMillan, & Roemer, 2007), two forms of psychopathology greatly impacted by early trauma exposure (Copeland, Keeler, Angold, & Costello, 2007; K.A. McLaughlin et al., 2010). Therefore, assessments of relationships between trauma exposure and later emotion dysregulation should control for psychiatric symptoms.
Data Analyses
First, we conducted univariate and bivariate analyses to examine the distribution of emotion dysregulation and trauma exposure in the sample and compare emotion dysregulation values by each covariate. Second, we conducted a series of linear regressions, separately for each traumatic event and trauma type, to determine the association between trauma exposure and emotion dysregulation after controlling for covariates. Model 1 assessed the effect of trauma exposure (1=exposed vs. 0=never exposed) on emotion dysregulation. Model 2 assessed the effect of age at first exposure (1=early childhood; 2=middle childhood; 3=adolescence; 4=adulthood vs. 0=never exposed) on emotion dysregulation. In this second model, we adjusted for exposure to any other trauma (beyond the focal trauma examined), as trauma exposures were moderately correlated in this sample (tetrachoric correlation: r=0.06 to r=0.63 for individual traumatic events; average correlation for child maltreatment events: r=0.48) and prior studies have shown that failure to account for co-occurring trauma exposure may overemphasize the impact of a single trauma (K.A. McLaughlin et al., 2010). Model 3 expanded upon Model 2 by additionally adjusting for frequency of each trauma event (0=low frequency; 1=high frequency). Model 4 built upon Model 3 by additionally controlling for current level of depressive and posttraumatic symptoms as described above.
Third, we conducted tests of homogeneity for all models assessing the role of developmental timing (Models 2, 3 and 4) to determine whether the beta coefficients, which indicated the effect of age at first exposure relative to never exposed, were significantly different from each other. When significant omnibus differences were found in the homogeneity test, we then performed post hoc Tukey comparisons to determine whether individual beta coefficients indicating the effect of age at first trauma exposure were significantly different from each other. A significant Tukey value signifies differences in effect of exposure during different age periods after correcting for multiple testing. All analyses were performed using SAS Version 9.4 (SAS Institute, Inc, Cary, North Carolina).
Results
In the analytic sample of 1944 African American adults, 74.2% of the sample were female, the mean age was 40.2 years (SD=13.6; range 18-78) and the mean emotion dysregulation score was 38.26 (SD=21.63). Emotion dysregulation scores varied significantly across all covariates (Table 1), with women, middle aged individuals, and those with lower education, income, and employment status having higher emotion dysregulation scores. Slightly less than half of the sample (40.7%; n=791) had high depressive symptoms, PTSD symptoms or both. High depressive and posttraumatic symptoms were significantly associated with higher emotion dysregulation scores (tetrachoric correlation: r=0.66, p<.0001).
Table 1.
Distribution of covariates and emotion dysregulation symptoms in the Grady Trauma Project (GTP) analytic sample (N=1944)
| Covariate | Total Sample | Emotion Dysregulation Symptoms | ||
|---|---|---|---|---|
|
| ||||
| N (%) | Mean (SD) | F value | p value | |
| Age | ||||
| 18–25 | 408 (21.0) | 38.71 (20.3) | 7.88 | <0.0001 |
| 26–35 | 366 (18.8) | 39.22 (21.8) | ||
| 36–45 | 354 (18.2) | 41.28 (22.9) | ||
| 46–55 | 535 (27.5) | 38.52 (22.0) | ||
| 56+ | 281 (14.5) | 32.05 (19.6) | ||
| Sex | ||||
| Male | 501 (25.8) | 36.37 (21.3) | 5.16 | 0.023 |
| Female | 1443 (74.2) | 38.91 (21.7) | ||
| Education | ||||
| Less than 12th grade | 432 (22.2) | 43.30 (22.9) | 19.42 | <0.0001 |
| High school graduate or GED | 842 (43.3) | 38.22 (21.6) | ||
| Greater than high school or GED/College graduate | 670 (34.5) | 35.06 (20.2) | ||
| Income | ||||
| $0–499 | 618 (31.8) | 41.93 (22.5) | 16.59 | <0.0001 |
| $500–999 | 526 (27.1) | 38.43 (21.9) | ||
| $1,000 or more | 800 (41.1) | 35.31 (20.2) | ||
| Employment Status | ||||
| Unemployed | 1047 (53.9) | 39.33 (21.9) | 14.78 | <0.0001 |
| Unemployed (with disability) | 336 (17.3) | 41.55 (22.9) | ||
| Employed (with or without disability) | 561 (22.8) | 34.30 (19.7) | ||
| Depressive and posttraumatic stress symptoms | ||||
| Low symptoms | 1153 (59.3) | 28.65 (17.0) | 785.01 | <0.0001 |
| High symptoms | 791 (40.7) | 52.27 (20.0) | ||
Descriptive statistics are presented for the analytic sample. Linear regressions were performed for each outcome by covariate, with F-statistics and corresponding p-values listed. High depressive and posttraumatic symptoms are based on measures of depression (Beck’s Depression Inventory - Second Edition (BDI-II) and posttraumatic stress symptoms (Modified Posttraumatic Symptom Scale (MPSS)). Participants were coded as having high depressive and posttraumatic stress symptoms (vs. low psychiatric symptoms) if BDI scores were 20 or greater or if on the MPSS the participated reported the presence of at least one re-experiencing symptom (scored 1 or higher), two avoidance/numbing symptoms, and two hyperarousal symptoms and low PTSD was any lower levels of symptoms).
Trauma Exposure: Distribution, Age at First Exposure, and Frequency of Exposure
Nearly all participants (94.9% of the sample) reported at least one trauma exposure; 84.3% reported at least two event exposures. The most commonly reported trauma was serious accident or injury.
The distribution of age at first trauma exposure varied by trauma type (Table 2). For example, about half (50.5%) of individuals exposed to child maltreatment were first exposed in middle childhood, whereas only 20.3% of individuals were first exposed to any type of other interpersonal violence in middle childhood. Non-interpersonal trauma was most often reported as first occurring during adulthood.
Table 2.
Distribution of exposure to each traumatic event in total sample and by age at first trauma exposure among those who were exposed
| Exposed | Age at First Exposure (year) |
Age at First Exposure (category) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Ages 0–5 | Ages 6–10 | Ages 11–18 | Ages 19+ | |||||||||
|
| ||||||||||||
| Exposure | % | N | Mean | SD | % | N | % | N | % | N | % | N |
| Trauma Exposure | ||||||||||||
| Child Maltreatment | ||||||||||||
| Violence between Caregivers | 30.1 | 585 | 8.10 | 3.3 | 24.6 | 144 | 53.8 | 315 | 21.6 | 126 | – | – |
| Physical Abuse | 19.1 | 371 | 8.19 | 3.3 | 23.7 | 88 | 55.0 | 204 | 21.3 | 79 | – | – |
| Emotional Abuse | 24.4 | 474 | 9.99 | 3.8 | 13.9 | 66 | 43.9 | 208 | 42.2 | 200 | – | – |
| Sexual Abuse | 29.8 | 579 | 9.68 | 3.8 | 15.0 | 87 | 44.2 | 256 | 40.8 | 236 | – | – |
| Any of the Above | 54.4 | 1058 | 8.08 | 3.5 | 27.1 | 287 | 50.5 | 533 | 22.5 | 238 | – | – |
| Other Interpersonal Violence | ||||||||||||
| Family/friend Murdered | 54.0 | 1049 | 22.22 | 11.8 | 1.6 | 17 | 11.0 | 115 | 37.1 | 389 | 50.3 | 528 |
| Witness Attack (Family or friend) | 42.0 | 817 | 17.49 | 10.0 | 5.1 | 42 | 20.0 | 163 | 39.9 | 326 | 35.0 | 286 |
| Witness Attack (non-family/friend) | 43.4 | 843 | 19.16 | 10.3 | 2.7 | 23 | 14.9 | 126 | 42.8 | 361 | 39.5 | 333 |
| Any of the Above | 77.6 | 1509 | 17.81 | 10.4 | 4.6 | 70 | 20.3 | 307 | 40.9 | 616 | 34.2 | 516 |
| Non-Interpersonal Trauma | ||||||||||||
| Natural Disaster | 26.1 | 507 | 20.19 | 13.5 | 5.1 | 26 | 24.6 | 125 | 28.4 | 144 | 41.8 | 212 |
| Serious Accident or Injury | 64.2 | 1247 | 20.33 | 11.7 | 4.1 | 51 | 18.0 | 224 | 30.7 | 383 | 47.2 | 589 |
| Life Threatening Illness | 22.3 | 433 | 33.81 | 15.6 | 5.1 | 22 | 3.7 | 16 | 10.1 | 44 | 81.1 | 351 |
| Any of the Above | 74.4 | 1446 | 18.84 | 11.9 | 6.7 | 97 | 22.5 | 325 | 30.1 | 435 | 40.7 | 589 |
| Any other trauma | 29.1 | 566 | 27.42 | 13.9 | 2.7 | 15 | 6.2 | 35 | 21.0 | 119 | 70.1 | 397 |
There was a gradient in the relationship between age at first exposure and frequency of exposure, suggesting that those first exposed in earlier developmental periods also tended to report more frequent occurrences of exposure (Figure 1).
Figure 1. Percent of respondents exposed to frequent trauma by age at first exposed to trauma.
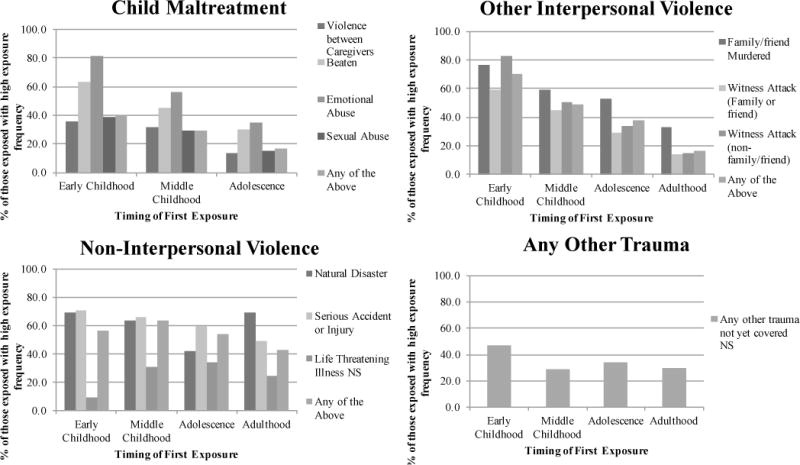
The figure presents the percentage of those exposed to frequent trauma, within each age category, among those exposed. All Chi Square Goodness of Fit models for each trauma event, which evaluated whether there were significant differences between the frequencies of exposure to each trauma by age at first exposure, are significant (p<0.0001) unless indicated with NS (p>0.05).
Frequency of each trauma event occurrence was ascertained on a scale ranging from 0 (unexposed) to 8 (greater than 20 times). Using this data, we generated indicator variables for each traumatic event denoting low versus high frequency of trauma exposure, with high being at or above the top quartile of frequency for a specific event. High frequency was defined as greater than or equal to the following values for each individual trauma event: natural disaster ≥ 2; serious accident or injury ≥ 2; and sudden life threatening illness ≥ 2; a friend or family member being murdered ≥ 2; a family member or friend being attacked ≥ 4; a non-family member or friend attacked ≥ 5; violence between parents or caregivers ≥ 8; beaten ≥ 8; emotional abuse ≥ 8; or sexual abuse ≥ 5. For the trauma categories, the 75th percentile for reported frequency of exposure was taken for all events included in the category and high frequency was defined as greater than or equal to the following values for trauma categories: child maltreatment ≥ 7, interpersonal trauma ≥ 3, non-interpersonal trauma ≥ 2; and any other trauma not reported ≥ 2.
Trauma Exposure and Emotion Dysregulation Symptoms: The Role of Exposure Type and Timing of Exposure
As shown in Table 3, where the results from Model 1 are reported in the row for each bolded trauma type, exposure to child maltreatment, interpersonal violence, and non-interpersonal trauma were all associated with increases in emotion dysregulation symptoms in adulthood. The largest observed effect was for child maltreatment, where we found that people exposed to maltreatment scored 9.94 points higher than their unexposed peers on the emotion dysregulation symptoms measure, even after adjusting for covariates and other trauma exposure (β=9.94; 95% CI=8.04, 11.83, p<0.0001).
Table 3.
Results of linear regression analyses examining the effect of age at first trauma exposure on emotion dysregulation symptoms, adjusting for multiple covariates
| Model 2 (adjustment for socio-demographic factors and other trauma exposure) |
Model 3 (adjustment for Model 2 plus frequency of trauma) |
Model 4 (adjustment for Model 3 plus depressive or posttraumatic stress symptoms) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| N (%) | Beta | 95% CI | Homogeneity F-statistic (p-value) |
Beta | 95% CI | Homogeneity F-statistic (p-value) |
Beta | 95% CI | Homogeneity F-statistic (p-value) |
|
|
|
||||||||||
| Child Maltreatment | 9.936 | (8.04, 11.83) | 5.45 (0.004) | 8.421 | (6.38, 10.47) | 3.65 (0.026) | 3.479 | (1.65, 5.31) | 3.36 (0.035) | |
| Early Childhood | 287 (14.8) | 11.868b | (9.08, 14.65) | 10.028 | (7.04, 13.01) | 3.698 | (1.04, 6.36) | |||
| Middle Childhood | 533 (27.4) | 10.543d | (8.30, 12.79) | 9.201 | (6.83, 11.58) | 4.655d | (2.55, 6.76) | |||
| Adolescence | 238 (12.2) | 6.389 | (3.43, 9.35) | 5.603 | (2.62, 8.59) | 1.058 | (−1.58, 3.69) | |||
| Other Interpersonal Violence | 2.913 | (0.65, 5.18) | 3.99 (0.008) | 2.499 | (0.24, 4.66) | 3.81 (0.010) | 0.326 | (−1.74, 2.39) | 4.33 (0.005) | |
| Early Childhood | 70 (3.6) | −0.751 | (−6.02, 4.52) | −1.560 | (−7.03, 3.91) | 5.529a | (−10.32, −0.74) | |||
| Middle Childhood | 307 (15.8) | 6.368d, e | (3.26, 9.48) | 5.807d, e | (2.53, 9.08) | 2.647 | (−0.23, 5.52) | |||
| Adolescence | 616 (31.7) | 2.308 | (−0.29, 4.91) | 1.886 | (−0.82, 4.60) | 0.046 | (−2.42, 2.33) | |||
| Adulthood | 516 (26.5) | 2.262 | (−0.39, 4.91) | 2.095 | (−0.57, 4.76) | 0.080 | (−2.25, 2.42) | |||
| Non-Interpersonal Trauma | 2.542 | (0.34, 4.75) | 2.32 (0.074) | 1.706 | (−0.71, 4.12) | 2.01 (0.111) | 0.085 | (−2.03, 2.20) | 2.44 (0.063) | |
| Early Childhood | 97 (5.0) | |||||||||
| Middle Childhood | 325 (16.7) | |||||||||
| Adolescence | 435 (22.4) | |||||||||
| Adulthood | 589 (30.3) | |||||||||
| Any trauma not yet covered | 1.682 | (−0.39, 3.75) | 1.14 (0.330) | 1.448 | (−0.92, 3.81) | 1.12 (0.342) | 0.463 | (−2.53, 1.61) | 1.90 (0.128) | |
| Early Childhood | 15 (0.8) | |||||||||
| Middle Childhood | 35 (1.8) | |||||||||
| Adolescence | 119 (6.0) | |||||||||
| Adulthood | 397 (20.4) | |||||||||
The table presents results from Models 2, 3, and 4 which examined exposure to trauma (v. unexposed) and age at first exposure to trauma (early childhood = age 0-5, middle childhood = age 6-10, adolescence = age 11-18, adulthood = age 19+; v. unexposed) on emotion dysregulation symptoms. Model 2 controlled age, sex, education, income, employment status, and exposure to any other traumatic event. Model 3 controlled for all covariates included in Model 2 plus frequency of each trauma event occurrence (0=low frequency; 1=high reported number of occurrences of that trauma exposure). Model 4 controlled for all covariates in Model 3 plus presence (vs. absence) of current high levels of either depressive or posttraumatic stress symptoms. Each trauma type was examined separately, thus the table includes results of twelve separate multiple regression models (three models for each exposure).
Cell entries are beta coefficients and 95% confidence intervals (CI) estimating the association between exposure to trauma type (exposed vs. unexposed) and timing of exposure to maltreatment (e.g., exposed first during early childhood vs. unexposed), relative to the reference of never exposed in any developmental period. Effects are significant at p<0.05 when CI does not include 0. Omnibus tests for homogeneity (F-tests and p-values) indicate the overall main effect of age at first exposure categories; these test the null hypothesis that the beta coefficients were equivalent across all groups (i.e., early childhood beta = middle childhood beta = adolescence beta = adult beta).
refers to a significant difference (p<0.05) between early childhood vs. middle childhood, based on the Tukey post-hoc test.
refers to a significant difference (p<0.05) between early childhood vs. adolescence, based on the Tukey post-hoc test.
refers to a significant difference (p<0.05) between early childhood vs. adulthood, based on the Tukey post-hoc test.
refers to a significant difference (p<0.05) between middle childhood vs. adolescence, based on the Tukey post-hoc test.
refers to a significant difference (p<0.05) between middle childhood vs. adulthood, based on the Tukey post-hoc test.
Child Maltreatment
As shown in the columns of Table 3 and Figure 2, which presents results from Models 2-4, the effect of developmental timing of trauma on emotion dysregulation varied by trauma type. Differences in the magnitude of association were observed for both child maltreatment (homogeneity p-value=0.0004) and other interpersonal violence trauma (homogeneity p-value=0.008). Specifically, although child maltreatment beginning at any age was associated with increased emotion dysregulation symptoms relative to no exposure, people first exposed in early childhood (β=11.868, 95% CI=9.08, 14.65) or middle childhood (β=10.543, 95% CI=8.30, 12.79) had higher emotion dysregulation symptoms relative to people first exposed in adolescence (β=6.389, 95% CI=3.43, 9.35; Tukey post-hoc pairwise p-values <0.05). These differences were no longer significant after adjustment for frequency of exposure (Model 3). After controlling for depressive and posttraumatic symptoms (Model 4), effect estimates were attenuated, though the differences in magnitude of effect persisted in comparing those first exposed first in middle childhood to those first exposed in adolescence (Tukey post-hoc pairwise p-value <0.05).
Figure 2. Regression coefficients for the effect of age at first trauma exposure on emotion dysregulation symptoms, adjusting for multiple covariates.
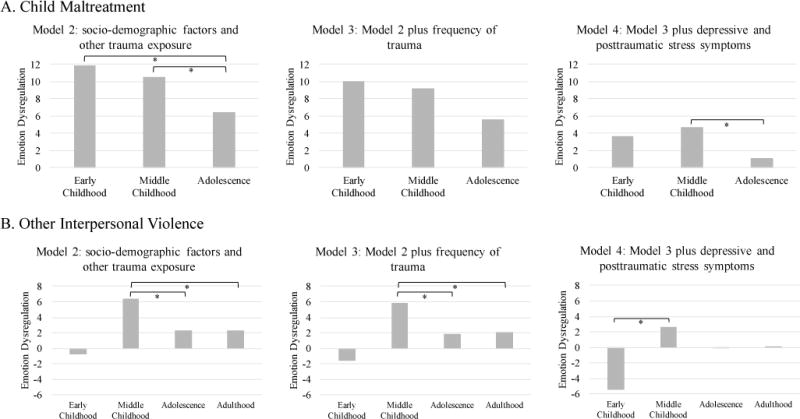
The figures presents results from Models 2, 3, and 4 which examined exposure to trauma (v. unexposed) and age at first exposure to trauma (early childhood = age 0-5, middle childhood = age 6-10, adolescence = age 11-18, adulthood = age 19+; v. unexposed) on emotion dysregulation symptoms. Model 2 controlled age, sex, education, income, employment status, and exposure to any other traumatic event. Model 3 controlled for all covariates included in Model 2 plus frequency of each trauma event occurrence (0=low frequency; 1=high reported number of occurrences of that trauma exposure). Model 4 controlled for all covariates in Model 3 plus presence (vs. absence) of current high levels of either depressive or posttraumatic stress symptoms.
The y-axis indicates the beta coefficient from the regression models, or the effect of exposure to trauma during an age group compared to those unexposed on emotion dysregulation symptoms. All omnibus tests for homogeneity were significant, indicating that the beta coefficients were not equivalent across all groups (i.e., early childhood beta = middle childhood beta = adolescence beta = adult beta).
Brackets and * indicate a significant difference (p<0.05) between age at first exposure group effect size, based on the Tukey post-hoc test (e.g., in A. Child Maltreatment, Model 2, the effect of early childhood was significantly different from the effect of adolescence, and the effect of middle childhood significantly different from the effect of adolescence).
Other Interpersonal Violence
For other interpersonal violence, only middle childhood was associated with increased emotion dysregulation symptoms in adulthood after controlling for covariates, other trauma exposure (Model 2: middle childhood β=6.368, 95% CI=3.26, 9.48) and frequency of the trauma occurrence (Model 3: middle childhood β=5.807, 95% CI=2.53, 9.08) (Table 3 and Figure 2). The effect of first exposure in middle childhood was significantly higher than first exposure in adolescence or adulthood (Tukey post-hoc pairwise p-values <0.05). After controlling for depressive and posttraumatic symptoms (Model 4), these differences were no longer observed. However, we did find that first exposure during early childhood was associated with lower emotion dysregulation symptoms in adulthood relative to first exposure in middle childhood (Model 4: early childhood β=−5.529, 95% CI=−10.32, −0.74).
Non-Interpersonal Trauma
There were no significant developmental timing differences by age at first exposure to non-interpersonal trauma on emotion dysregulation (all effects p>0.05).
Any trauma Not Yet Covered
No significant developmental timing differences were found for age at first exposure to other trauma and emotion dysregulation (all effects p>0.05).
Discussion
In this study, we examined the association between different types of trauma and levels of emotion dysregulation in adulthood. Conducting these analyses in a sample with high trauma exposure allowed for both between group (exposed and unexposed individuals) and within group (exposed) comparisons. A particularly unique focus of this work was to investigate the role of developmental timing of trauma exposure on emotion dysregulation scores before and after controlling for potentially confounding factors, including frequency of trauma occurrence as well as other trauma types, which facilitated the identification of potential sensitive periods when trauma was most likely to affect emotion dysregulation.
Our results suggest that people exposed to trauma were generally more likely than their unexposed peers to have higher emotion dysregulation. However, the effect of trauma varied as a function of not just trauma type, but also when in course of the lifespan the trauma first occurred. Specifically, three findings related to trauma type and developmental timing emerged from this study. First, we found that exposure to child maltreatment beginning in middle childhood was most associated with adult emotion dysregulation symptoms, compared to other developmental time points, and that this relationship persisted after controlling for socioeconomic factors, frequency of trauma occurrence, and current depressive and posttraumatic symptoms. Second, other interpersonal trauma exposure beginning in middle childhood was also the developmental period most associated with emotion dysregulation, even after accounting for frequency of trauma occurrence. Thirdly, after controlling for current depressive and posttraumatic symptoms, the effect of other interpersonal trauma exposure in middle childhood was diminished and first exposure to other interpersonal violence in early childhood was associated with significantly lower emotion dysregulation symptoms.
Collectively, these results are consistent with prior literature showing increased levels of emotion dysregulation in adulthood among adults exposed to child maltreatment or interpersonal trauma (Briere & Rickards, 2007; Thompson et al., 2014), particularly when the trauma was interpersonal in nature, chronic, and began prior to adolescence (Ehring & Quack, 2010). However, our findings differ from previous studies assessing the role of developmental timing of exposure to maltreatment and emotion dysregulation. For example, early maltreatment exposure (between birth to age 3), but not later maltreatment (between ages 3-5) (Kim & Cicchetti, 2010), and longer institutional care (after age 15 months), compared to shorter institutional care (adopted prior to 15 months) (N. Tottenham & Sheridan, 2010) have been previously associated with higher emotion dysregulation in early adolescence. Our findings may differ from these two studies because both of them assessed emotion dysregulation in early adolescence, a time when emotion regulation capabilities are still developing; we, instead, focused on adulthood, when emotion regulation capabilities are likely more fixed. Furthermore, differences between our study and these two prior ones could be explained by differences in the measurement of trauma features (e.g., frequency, chronicity, severity, etc.) and methods to adjust for covariates (e.g., controlling for psychiatric symptoms, stratifying by psychiatric status, assessing emotion dysregulation as a mediator or moderator, etc.).
Child maltreatment during middle childhood could be especially harmful for emotion regulation capacities for several reasons. As noted previously, emotion regulation depends on an individual’s cognitive capabilities as well as his or her positive interpersonal, familial, and other social relationships (Calkins, 1994; Morris et al., 2007). Emotion regulation skills rapidly develop during middle childhood and once children reach older childhood (about age 8-12), these skills have developed and children can effectively use multiple emotional coping strategies (Fields & Prinz, 1997). Therefore, disruptions of attachment with caregivers and other social relationships and the failure to receive appropriate modeling of behavior, at a time when the cognitive and emotional capabilities to navigate such relationships are developing (B. Bradley, Westen, et al., 2011; Dvir et al., 2014), may be therefore especially damaging. There is also evidence of a stress-hyporesponsive period characterized by lower stress reactivity and lower glucocorticoid activity that occurs approximately from ages one to six (Gunnar & Quevedo, 2007), which may contribute to the relative lack of negative impact of early childhood trauma. Further, memory is not fully developed in early childhood, thus individuals mostly remember and report traumatic exposures beginning around middle childhood. These observations may also explain our finding that after accounting for current depressive and posttraumatic symptoms, first exposure to other interpersonal violence during early childhood was associated with less emotion dysregulation as compared to first exposure during middle childhood.
Results from this study should be evaluated in light of several limitations. First, lifetime trauma exposure was assessed retrospectively in the context of a cross-sectional design. Retrospective reports of child maltreatment, in particular, may be less reliable and valid compared to prospective reports due to the influence of current psychiatric state, inaccurate memory, and reluctance to report sensitive personal information (Hardt & Rutter, 2004). However, recent work has found similar effect estimates for psychiatrically-relevant outcomes with both retrospective and prospective measures of trauma (Scott, McLaughlin, Smith, & Ellis, 2012). Further, with retrospective reporting, adults have been shown to minimize their degree of exposure, suggesting that false negative reports may be more common than false positive reports (Brewin, Andrews, & Gotlib, 1993; Shaffer, Huston, & Egeland, 2008). Relatedly, due to recall bias, there may be potential inaccuracies in the reported age at first exposure to trauma. We aimed to minimize these inaccuracies by grouping exposure ages into developmental time periods. Prospective research would be ideal to replicate our cross-sectional findings and further assess the impact of developmental timing of trauma exposure.
Second, the characteristics of trauma assessed in this study were limited to exposure, age at first exposed, and frequency of trauma occurrence, thereby potentially overlooking other important aspects of trauma such as its severity or duration. However, the frequency of trauma occurrence information allows us to distinguish between individuals exposed only once or twice from those exposed multiple times, potentially yielding new insight into the role of these characteristics. Third, generalizability of results may be limited due to the nature of our sample. However, low-income African American women are generally underserved (Carrington, 2006) and research is needed to understand risks within this population due to their high burden of trauma exposure. Finally, the assessment of psychiatric symptoms was exclusively based on self-reported questionnaires, rather than interviewer-based measures or clinician-based diagnostic assessments.
In conclusion, results from this study suggest that the effects of child maltreatment and other interpersonal violence on emotion dysregulation in adulthood vary as a function of when in the lifecourse these traumas first occurred. Evidence in support of possible sensitive periods could inform policy and practice to guide implementation and increase effectiveness of early interventions for individuals exposed to trauma. Specifically, new knowledge about the timing of sensitive periods could lead clinicians to deliver interventions at specific age stages when these interventions would be more likely to yield stronger impacts in terms of offsetting the negative sequela of trauma. However, for these types of clinical possibilities to be realized, these findings should be replicated in other population-based samples with prospective designs to confirm the importance of developmental timing of trauma on later emotion dysregulation.
Highlights.
People exposed to trauma have higher emotion dysregulation scores compared to their unexposed peers.
Exposure to child maltreatment in middle childhood is most associated with elevated emotion dysregulation symptoms in adulthood.
Other interpersonal trauma exposure in middle childhood was also highly associated with elevated emotion dysregulation symptoms, but this effect was diminished after controlling for current psychiatric symptoms.
After controlling for current psychiatric symptoms, exposure to interpersonal violence in early childhood was associated with significantly lower emotion dysregulation symptoms.
Acknowledgments
Research reported in this publication was supported by the National Institute of Mental Health within the National Institutes of Health under Award Numbers K01 MH102403 (Dunn) and F32 MH102890 (Powers) and the National Institute of Child Health and Human Development under Award Number R01 HD071982 (Bradley). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the contents of this report do not represent the views of the Department of Veterans Affairs or the United States Government. The authors thank Alice Renaud for her assistance in preparing this manuscript for publication.
Role of the Funding
Research reported in this publication was supported by the National Institute of Mental Health within the National Institutes of Health under Award Numbers K01 MH102403 (Dunn) and F32 MH102890 (Powers) and the National Institute of Child Health and Human Development under Award Number R01 HD071982 (Bradley). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the contents of this report do not represent the views of the Department of Veterans Affairs or the United States Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest:
none
Contributors
I, Dr. Dunn, created the analytic plan, supervised the data analysis, interpreted the results, and drafted the manuscript. I also had access to all data and take responsibility for the accuracy of the data analysis. Ms. Nishimi conducted the literature search, performed the data analysis, and assisted in drafting the manuscript. Ms. Gomez conducted the literature search and assisted in drafting the manuscript. Dr. Powers contributed to the original data collection, provided early comments regarding the data analysis plan, interpreted the results, and read early drafts of the manuscript. Dr. Bradley oversaw the original data collection and provided early comments regarding the data analysis plan. All authors contributed to and approve of the final manuscript.
References
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Arlington, VA: American Psychiatric Publishing; 2000. [Google Scholar]
- Andover MS, Morris BW. Expanding and clarifying the role of emotion regulation in nonsuicidal self-injury. The Canadian Journal of Psychiatry. 2014;59(11):569–575. doi: 10.1177/070674371405901102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical psychology review. 1988;8(1):77–100. [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Koenen KC. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. 2016;46(2):327–343. doi: 10.1017/s0033291715001981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive–behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology. 2011;79(3):307. doi: 10.1037/a0023421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M, Wupperman P. Emotion regulation and mental health: recent findings, current challenges, and future directions. Curr Opin Psychiatry. 2012;25(2):128–134. doi: 10.1097/YCO.0b013e3283503669. [DOI] [PubMed] [Google Scholar]
- Binder EB, Bradley RG, Liu W, Epstein MP, Deveau TC, Mercer KB, et al. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. Journal of the American Medical Association. 2008;299(11):1291–1305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore SJ, Mills KL. Is adolescence a sensitive period for sociocultural processing? Annual review of psychology. 2014;65:187–207. doi: 10.1146/annurev-psych-010213-115202. [DOI] [PubMed] [Google Scholar]
- Bornstein MH. Sensitive periods in development: Structural characteristics and causal interpretations. Psychol Bull. 1989;105(2):179–197. doi: 10.1037/0033-2909.105.2.179. [DOI] [PubMed] [Google Scholar]
- Bradley B, DeFife JA, Guarnaccia C, Phifer J, Fani N, Ressler KJ, Westen D. Emotion dysregulation and negative affect: association with psychiatric symptoms. J Clin Psychiatry. 2011;72(5):685–691. doi: 10.4088/JCP.10m06409blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley B, Westen D, Mercer KB, Binder EB, Jovanovic T, Crain D, Heim C. Association between childhood maltreatment and adult emotional dysregulation in a low-income, urban, African American sample: moderation by oxytocin receptor gene. Dev Psychopathol. 2011;23(2):439–452. doi: 10.1017/s0954579411000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, Kessler RC. Influence of child abuse on adult depression: Moderation by the corticotropin-releasing hormone receptor gene. Archives of General Psychiatry. 2008;65(2):190–200. doi: 10.1001/archgenpsychiatry.2007.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: a reappraisal of retrospective reports. Psychol Bull. 1993;113(1):82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- Briere J, Rickards S. Self-awareness, affect regulation, and relatedness: differential sequels of childhood versus adult victimization experiences. J Nerv Ment Dis. 2007;195(6):497–503. doi: 10.1097/NMD.0b013e31803044e2. [DOI] [PubMed] [Google Scholar]
- Calkins SD. Origins and outcomes of individual differences in emotion regulation. Monographs of the Society for Research in Child Development. 1994;59(2-3):53–72. [PubMed] [Google Scholar]
- Carpenter RW, Trull TJ. Components of emotion dysregulation in borderline personality disorder: A review. Current psychiatry reports. 2013;15(1):335. doi: 10.1007/s11920-012-0335-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrington CH. Clinical depression in African American women: Diagnoses, treatment, and research. Journal of Clinical Psychology. 2006;62(7):779–791. doi: 10.1002/jclp.20289. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Dansky BS, Falsetti SA, Saladin ME, Brady KT. Screening for PTSD in a substance abuse sample: psychometric properties of a modified version of the PTSD Symptom Scale Self-Report. Posttraumatic stress disorder. J Trauma Stress. 1998;11(2):393–399. doi: 10.1023/A:1024467507565. [DOI] [PubMed] [Google Scholar]
- Cole PM, Michel MK, Teti LOD. The development of emotion regulation and dysregulation: A clinical perspective. Monographs of the Society for Research in Child Development. 1994;59(2-3):73–102. [PubMed] [Google Scholar]
- Conklin CZ, Bradley R, Westen D. Affect regulation in borderline personality disorder. The Journal of nervous and mental disease. 2006;194(2):69–77. doi: 10.1097/01.nmd.0000198138.41709.4f. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiatry. 2007;64(5):577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Dunn EC, McLaughlin KA, Slopen N, Rosand J, Smoller JW. Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: results from the National Longitudinal Study of Adolescent Health. Depress Anxiety. 2013;30(10):955–964. doi: 10.1002/da.22102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvir Y, Ford JD, Hill M, Frazier JA. Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harvard Review of Psychiatry. 2014;22(3):149–161. doi: 10.1097/HRP.0000000000000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T, Quack D. Emotion regulation difficulties in trauma survivors: the role of trauma type and PTSD symptom severity. Behav Ther. 2010;41(4):587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Field T. The effects of mother’s physical and emotional unavailability on emotion regulation. Monographs of the Society for Research in Child Development. 1994;59(2-3):208–227. [PubMed] [Google Scholar]
- Fields L, Prinz RJ. Coping and adjustment during childhood and adolescence. Clinical psychology review. 1997;17(8):937–976. doi: 10.1016/s0272-7358(97)00033-0. [DOI] [PubMed] [Google Scholar]
- Fox H, Axelrod S, Paliwal P, Sleeper J, Sinha R. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug and alcohol dependence. 2007;89(2):298–301. doi: 10.1016/j.drugalcdep.2006.12.026. [DOI] [PubMed] [Google Scholar]
- Gillespie BM, Chaboyer W, Wallis M. The influence of personal characteristics on the resilience of operating room nurses: a predictor study. Int J Nurs Stud. 2009;46(7):968–976. doi: 10.1016/j.ijnurstu.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, Ressler KJ. Trauma exposure and stress-related disorders in inner city primary care patients. Gen Hosp Psychiatry. 2009;31(6):505–514. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie CF, Phifer J, Bradley B, Ressler KJ. Risk and resilience: genetic and environmental influences on development of the stress response. Depress Anxiety. 2009;26(11):984–992. doi: 10.1002/da.20605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, Thompson RA. Emotion regulation: Conceptual foundations 2007 [Google Scholar]
- Gunnar M, Quevedo K. The neurobiology of stress and development. Annu Rev Psychol. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hensch TK. Critical period regulation. Annual Review of Neuroscience. 2004;27:549–579. doi: 10.1146/annurev.neuro.27.070203.144327. [DOI] [PubMed] [Google Scholar]
- Hu T, Zhang D, Wang J, Mistry R, Ran G, Wang X. Relation between emotion regulation and mental health: a meta-analysis review. Psychological Reports. 2014;114(2):341–362. doi: 10.2466/03.20.PR0.114k22w4. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jazaieri H, Morrison AS, Goldin PR, Gross JJ. The role of emotion and emotion regulation in social anxiety disorder. Curr Psychiatry Rep. 2015;17(1):531. doi: 10.1007/s11920-014-0531-3. [DOI] [PubMed] [Google Scholar]
- Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. J Child Psychol Psychiatry. 2010;51(6):706–716. doi: 10.1111/j.1469-7610.2009.02202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenen KC, Roberts A, Stone D, Dunn EC. The epidemiology of early childhood trauma. In: Lanius R, Vermetten E, editors. The hidden epidemic: The impact of early life trauma on health and disease. New York, NY: Oxford University; 2010. pp. 13–24. [Google Scholar]
- Kolk BA, Fisler RE. Childhood abuse and neglect and loss of self-regulation. Bulletin of the Menninger Clinic. 1994;58(2):145. [PubMed] [Google Scholar]
- Langevin R, Hebert M, Allard-Dansereau C, Bernard-Bonnin AC. Emotion Regulation in Sexually Abused Preschoolers: The Contribution of Parental Factors. J Trauma Stress. 2016;29(2):180–184. doi: 10.1002/jts.22082. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical psychology review. 2015;40:111–122. doi: 10.1016/j.cpr.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Dialectical behavior therapy for treatment of borderline personality disorder: implications for the treatment of substance abuse. NIDA Res Monogr. 1993;137:201–216. [PubMed] [Google Scholar]
- Manly JT, Cicchetti D, Barnett D. The impact of subtype, frequency, chronicity, and severity of child maltreatment on social competence and behavior problems. Development and psychopathology. 1994;6(01):121–143. [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, Cicchetti D. Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and psychopathology. 2001;13(04):759–782. [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. JAMA Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, Kessler RC. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2013;52(8):815–830 e814. doi: 10.1016/j.jaac.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Kubzansky LD, Dunn EC, Waldinger R, Vaillant G, Koenen KC. Childhood social environment, emotional reactivity to stress, and mood and anxiety disorders across the life course. Depression and Anxiety. 2010;27(12):1087–1094. doi: 10.1002/da.20762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRae K, Gross JJ, Weber J, Robertson ER, Sokol-Hessner P, Ray RD, Ochsner KN. The development of emotion regulation: an fMRI study of cognitive reappraisal in children, adolescents and young adults. Social Cognitive and Affective Neuroscience. 2012;7(1):11–22. doi: 10.1093/scan/nsr093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The Role of the Family Context in the Development of Emotion Regulation. Soc Dev. 2007;16(2):361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murdock ME, Guarnaccia CA, Hayslip B, Jr, McKibbin CL. The contribution of small life events to the psychological distress of married and widowed older women. J Women Aging. 1998;10(2):3–22. doi: 10.1300/J074v10n02_02. [DOI] [PubMed] [Google Scholar]
- Parke RD. Progress paradigms, and unresolved problems: A commentary on recent advances in our understanding of children’s emotions. Merrill-Palmer Quarterly (1982-) 1994:157–169. [Google Scholar]
- Powers A, Etkin A, Gyurak A, Bradley B, Jovanovic T. Associations Between Childhood Abuse, Posttraumatic Stress Disorder, and Implicit Emotion Regulation Deficits: Evidence From a Low-Income, Inner-City Population. Psychiatry. 2015;78(3):251–264. doi: 10.1080/00332747.2015.1069656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers A, Stevens J, Fani N, Bradley B. Construct validity of a short, self report instrument assessing emotional dysregulation. Psychiatry Res. 2015;225(1-2):85–92. doi: 10.1016/j.psychres.2014.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pynoos RS, Steinberg AM, Piacentini JC. A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biological psychiatry. 1999;46(11):1542–1554. doi: 10.1016/s0006-3223(99)00262-0. [DOI] [PubMed] [Google Scholar]
- Raffaelli M, Crockett LJ, Shen YL. Developmental stability and change in self-regulation from childhood to adolescence. J Genet Psychol. 2005;166(1):54–75. doi: 10.3200/GNTP.166.1.54-76. [DOI] [PubMed] [Google Scholar]
- Roberts WL, Strayer J. Parents’ responses to the emotional distress of their children: Relations with children’s competence. Developmental psychology. 1987;23(3):415–422. [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, Cuthbert BN. Developing constructs for psychopathology research: research domain criteria. Journal of Abnormal Psychology. 2010;119(4):631. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Schwartz AC, Bradley R, Penza KM, Sexton M, Jay D, Haggard PJ, Ressler KJ. Pain medication use among patients with posttraumatic stress disorder. Psychosomatics. 2006;47(2):136–142. doi: 10.1176/appi.psy.47.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz AC, Bradley RL, Sexton M, Sherry A, Ressler KJ. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatr Serv. 2005;56(2):212–215. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- Scott KM, McLaughlin KA, Smith DA, Ellis PM. Childhood maltreatment and DSM-IV adult mental disorders: comparison of prospective and retrospective findings. Br J Psychiatry. 2012;200(6):469–475. doi: 10.1192/bjp.bp.111.103267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer A, Huston L, Egeland B. Identification of child maltreatment using prospective and self-report methodologies: a comparison of maltreatment incidence and relation to later psychopathology. Child Abuse Negl. 2008;32(7):682–692. doi: 10.1016/j.chiabu.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppes G, Suri G, Gross JJ. Emotion regulation and psychopathology. Annu Rev Clin Psychol. 2015;11:379–405. doi: 10.1146/annurev-clinpsy-032814-112739. [DOI] [PubMed] [Google Scholar]
- Shields A, Cicchetti D. Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology. 1997;33(6):906–916. doi: 10.1037/0012-1649.33.6.906. [DOI] [PubMed] [Google Scholar]
- Thompson KL, Hannan SM, Miron LR. Fight, flight, and freeze: Threat sensitivity and emotion dysregulation in survivors of chronic childhood maltreatment. Personality and Individual Differences. 2014;69:28–32. doi: 10.1016/j.paid.2014.05.005. [DOI] [Google Scholar]
- Tottenham N, Hare TA, Quinn BT, McCarry TW, Nurse M, Gilhooly T, Casey BJ. Prolonged institutional rearing is associated with atypically large amygdala volume and difficulties in emotion regulation. Developmental Science. 2010;13(1):46–61. doi: 10.1111/j.1467-7687.2009.00852.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, Sheridan MA. A review of adversity, the amygdala and the hippocampus: A consideration of developmental timing. Frontiers in Human Neuroscience. 2010;3:1–18. doi: 10.3389/neuro.09.068.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behav Ther. 2007;38(3):303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Vettese LC, Dyer CE, Li WL, Wekerle C. Does self-compassion mitigate the association between childhood maltreatment and later emotion regulation difficulties? A preliminary investigation. International Journal of Mental Health and Addiction. 2011;9(5):480–491. doi: 10.1007/s11469-011-9340-7. [DOI] [Google Scholar]
- Westen D, Muderrisoglu S, Fowler C, Shedler J, Koren D. Affect regulation and affective experience: individual differences, group differences, and measurement using a Q-sort procedure. Journal of Consulting and Clinical Psychology. 1997;65(3):429. doi: 10.1037//0022-006x.65.3.429. [DOI] [PubMed] [Google Scholar]


