Moyamoya disease (MMD) is an idiopathic intracranial vasculopathy characterized by progressive bilateral stenosis or occlusion of the terminal internal carotid arteries (ICA) and their main branches with compensatory collateral angiogenesis. It is more prevalent among Asian populations and has a typical angiographic appearance. A similar angiographic pattern is associated with vasculopathy due to several medical conditions including Down syndrome and is termed Moyamoya syndrome [1].
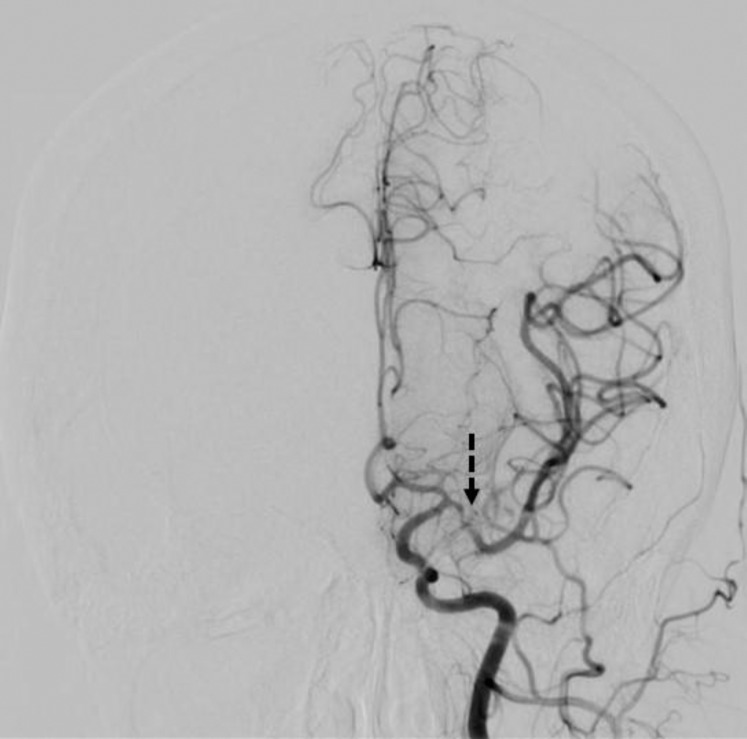
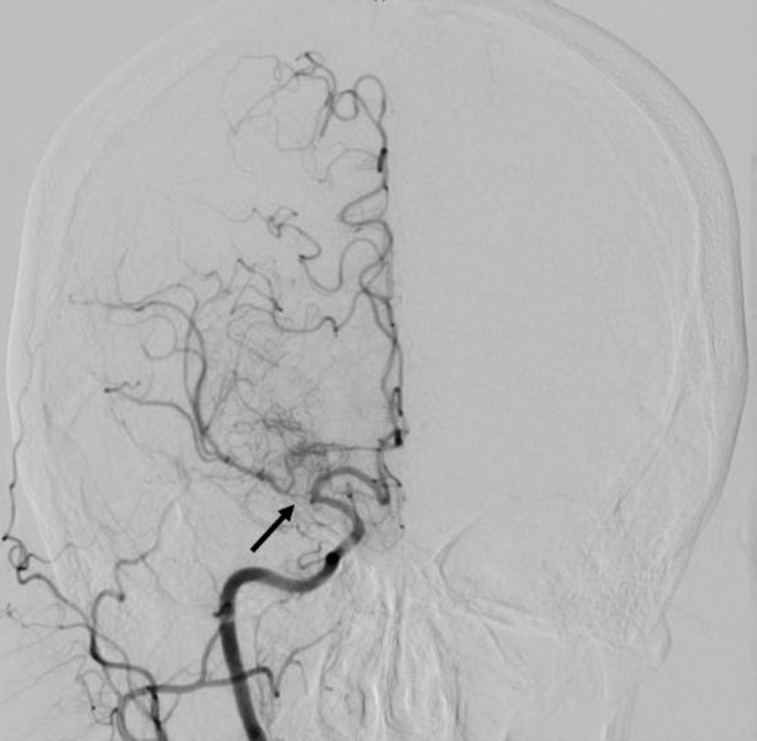
A 29-year-old non-Asian woman with Down syndrome was presented with acute headache, transient visual loss, and transient confusion for two days prior to admission. MRI confirmed acute infarction in the left middle cerebral artery (MCA) territory, mainly in the left parietal lobe. CT angiography suggested bilateral MCA stenosis and near occlusion, and asymmetric vascular blush. Diagnostic cerebral angiography confirmed MMS pattern with high grade focal stenosis of M1 segment of left MCA (Figure 1), and near occlusion of proximal M1 segment of right MCA with reconstitution via collateral arteries, and prominence of the lenticulostriate perforating vessels with significantly reduced capillary filling distally (Figure 2). Collateral circulation was from leptomeningeal vessels from the posterior cerebral artery filling the temporal and parietal lobes. There was sparing of the terminal ICAs, the external carotid artery branches, and posterior circulation suggesting an early stage disease. At 4 months follow up, there was no recurrence of symptoms after three months of dual antiplatelet therapy (Aspirin 325 mg and Clopidogrel 75 mg daily) following by single antiplatelet. At nine months, a follow-up MRI brain showed new lacunar infarct in the right medial frontal lobe white matter. Patients did not develop new neurological deficits.
Figure 1. Posteroanterior view (left ICA angiogram). The left ICA bifurcates normally into left MCA and ACA. The opacification pattern of the left MCA demonstrates high-grade stenosis of the left M1 segment (dashed arrow).
Figure 2. Posteroanterior view (right ICA angiogram). The right ICA bifurcates normally into right MCA and ACA. The opacification pattern of the right MCA demonstrates proximal M1 near occlusion (arrow) with reconstitution via collateral vessels and prominence of perforating vessels (Moyamoya like pattern).
Diagnostic criteria for MMD include stenosis or occlusion of the terminal ICA and proximal MCA or anterior cerebral artery (ACA), abnormal vascular network around the occlusive or stenotic lesions in the arterial phase, bilateral findings, and excluding Down syndrome, arteriosclerosis, autoimmune disease, neoplasm, history of irradiation, head trauma, neurofibromatosis, and meningitis [2].
Ring finger gene (RNF 213) was recently found to be linked to MMD in East Asians [3]. Our patient did not have access to genetic testing; however, it might not be of great value in her case since it has shown susceptibility only to East Asian individuals.
Recent prospective studies concluded there are no pathognomonic criteria to establish a diagnosis of MMD. In early stages, the distal ICA disease might not be observed, no objective criteria to call for prominent basal collaterals, and in some cases, the disease is unilateral. These findings support careful consideration of MMD when intracranial atherosclerotic disease is considered to avoid misdiagnosis [4, 5].
REFERENCES
- Scott RM, Smith ER. Moyamoya disease and Moyamoya syndrome. N Engl J Med. 2009;360(12):1226–1237. doi: 10.1056/NEJMra0804622. [DOI] [PubMed] [Google Scholar]
- Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis; Health Labour Sciences Research Grant for Research on Measures for Intractable Diseases Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis) Neurol Med Chir. 2012;52(5):245–266. doi: 10.2176/nmc.52.245. [DOI] [PubMed] [Google Scholar]
- Kamada F, et al. A genome-wide association study identifies RNF213 as the first Moyamoya disease gene. J Hum Genet. 2011;56(1):34–40. doi: 10.1038/jhg.2010.132. [DOI] [PubMed] [Google Scholar]
- Kim YJ, et al. Nonatheroscleotic isolated middle cerebral artery disease may be early manifestation of Moyamoya disease. Stroke. 2016;47(9):2229–2235. doi: 10.1161/STROKEAHA.116.012751. [DOI] [PubMed] [Google Scholar]
- Bang OY, et al. Adult Moyamoya disease: a burden of intracranial stenosis in East Asians? PLoS One. 2015;10(6):e0130663. doi: 10.1371/journal.pone.0130663. [DOI] [PMC free article] [PubMed] [Google Scholar]