Abstract
Purpose: Heart failure (HF) is common in older adults. With increases in technology use among older adults, mobile applications may provide a solution for older adults to self-manage symptoms of HF. This article discusses the development and acceptability of a HF symptom-tracking mobile application (HF app).
Methodology: The HF app was developed to allow patients to track their symptoms of HF. Thirty (N = 30) older adults completed an acceptability survey after using the mobile app. The survey used Likert items and open-ended feedback questions.
Results: Overall, the acceptability feedback from users was positive with participants indicating that the HF app was both easy to use and understand. Participants identified recommendations for improvement including additional symptoms to track and the inclusion of instructions and reminders.
Conclusion: HF is common in older adults, and acceptability of mobile apps is of key importance. The HF app is an acceptable tool for older patients with HF to self-manage their symptoms, identify patterns, and changes in symptoms, and ultimately prevent HF readmission.
Keywords: : m-health, older adults, symptoms, heart failure, telemedicine
Introduction
Approximately 915,000 individuals are newly diagnosed with heart failure (HF) each year, with incident rates highest among older adults, particularly males and people of color.1 With a booming aging population, it is estimated that nearly 8 million people will have HF by 2030.2 HF is the leading discharge diagnosis and the number one reason for hospital readmission among Medicare beneficiaries, and is a main driver of cost.3–6 With HF, patients often experience multiple symptoms simultaneously, and a change in symptoms can indicate impending HF decompensation.7,8 HF self-management can be critical for many patients to control the disease and avoid decompensation.9–11 This requires self-monitoring of daily weight for fluid accumulation and symptom recognition. Early identification of weight gain and potentially problematic symptoms allows a patient and their caregivers to intervene before hospitalization is needed.
Older adults are increasingly using smart phones and mobile applications (apps).12 As such, providing self-management mobile apps to help older adults with HF monitor their symptoms may improve HF health outcomes and decrease healthcare utilization.13–15 However, there may be biases against using such tools given misperceptions about capacity and desire for use among the elderly. To overcome these biases, it is critical to overcome likely barriers to the use of mobile apps among older adults,16,17 through assessment of the acceptability of proposed tools to improve design and user engagement. The purpose of this project was to develop a HF symptom-tracking mobile application (the HF app) and to test the acceptability of the app among potential older users.
Materials and Methods
Prototype Development
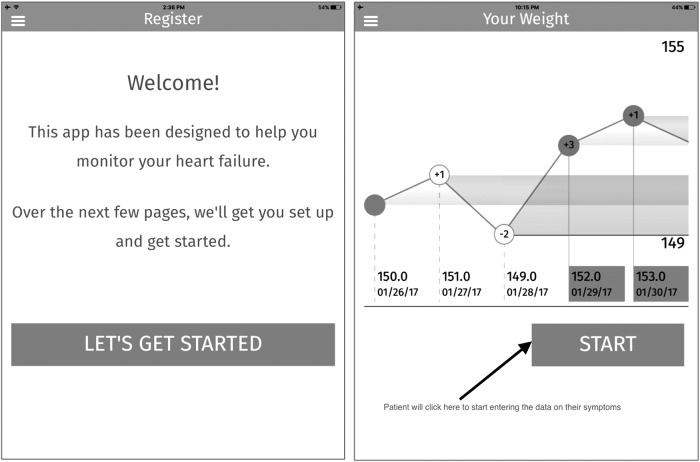
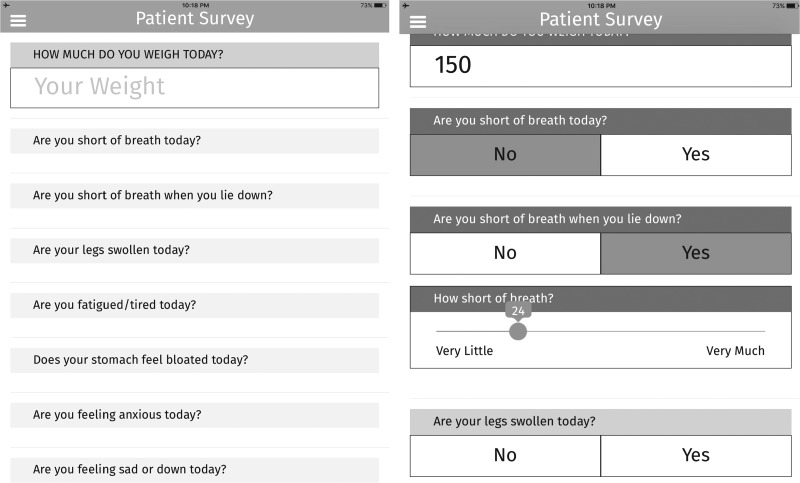
The HF symptom-tracker application (HF app) was initially developed with the overall goal to monitor the effect of research interventions. The HF app was designed to allow older adults with HF to record their weight, log their symptoms, and symptom severity (Fig. 1). Areas monitored included weight, fatigue, edema, shortness of breath, cough, stomach bloat, feeling sad, and feeling anxious (Fig. 2). Each item was dichotomous and only in cases of an affirmative response would a slider appear to indicate the symptom severity.
Fig. 1.
Heart Failure Application Start Screen and Weight Tracking Report.
Fig. 2.
Heart Failure Application Symptom Tracking Screens.
The HF app was available on the iPad and downloaded from the Apple app store. There was no identifying information used in HF app; a six-digit username and four-digit pin were used to connect patient information to a separate database. The backend used to collect data from the application and export it for use in external reporting tools ran on an Amazon commercial, HIPPA-compliant Web Services EC2 t2.Micro instance with 128 bit SSL encryption.
Acceptability Testing
The HF app was evaluated for acceptability by patients more than the age of 60 with a pen and paper survey. The survey comprised two sections. The first section included 18 items measured on a 5-point Likert scale from strongly agree to strongly disagree. Questions inquired about their understanding of the app, ability to use the app, and ability to report symptoms through the app. The second section included open-ended questions for specific changes or additions and potential caregivers' use of the app. We examined the differences in responses by participant characteristics (age, race/ethnicity, and gender) using chi-square and correlation as appropriate. The open-ended responses were analyzed using magnitude coding, a process that quantifies participants' answers, highlighting the most frequent comments.
Results
Participants
To evaluate the prototype, 30 patients were recruited from HF clinics in Denver at the University of Colorado Hospital and at the University Hospital Cleveland Medical Center in Cleveland, Ohio. Participants were mostly female (60%), black (63%), and a mean of 66 ± 18 years of age (Table 1).
Table 1.
Participant Characteristics (N = 30)
| CHARACTERISTIC | n |
|---|---|
| Age, mean ± SD | 66 ± 18 |
| Female, n (%) | 18 (60) |
| Site, n (%) | |
| Cleveland | 23 (77) |
| Denver | 7 (23) |
| Race, n (%) | |
| American Indian | 1 (0.03) |
| Black | 19 (63) |
| Caucasian | 10 (33) |
| Ethnicitya, n (%) | |
| Hispanic | 1 (0.03) |
| Non-Hispanic | 6 (20) |
| Unknown | 23 (77) |
| Years with HF, mean ± SD | 8.8 ± 10.6 |
| Caregiver helps, n (%) | |
| Manage HF | 10 (33) |
| Medication adherence | 8 (27) |
| Monitor symptoms | 4 (13) |
Denver site only.
HF, heart failure; SD, standard deviation.
Acceptability
Overall, the acceptability feedback from users was positive with participants indicating that the HF app was easy to use, understand, and navigate (Table 2). Participants liked the general design, but sought the addition of specific symptoms, improvement of navigation features, and enhanced instructions. There were no differences in responses by race, ethnicity, or gender. Older age was significantly associated with a self-identified need for help in ongoing use of the HF app (r = 0.462, p = 0.010).
Table 2.
Acceptability Summary
| QUESTION (1 = STRONGLY DISAGREE, 5 = STRONGLY AGREE) | MEAN |
|---|---|
| I was able to use the app without much of a problem | 3.9 |
| I was able to understand the questions | 4.6 |
| I felt confident using this app | 4.2 |
| I liked the way the app looks | 4.4 |
| I was able to see changes in my weight over time | 4.1 |
| I can read the words easily on the iPad | 4.7 |
| I was able to use the slider without difficulty | 4.3 |
| I understood what information the slider collected | 4.5 |
| I had difficulty navigating the app | 2.0 |
| I had difficulty understanding how to use the app | 1.7 |
| I felt that the app was confusing | 1.8 |
| I needed someone to explain to me how to use the app | 2.7 |
| I learned something from the app | 3.7 |
| I can understand why I would use this app | 3.9 |
| I would imagine that most people would learn to use this app very quickly | 4.5 |
| I can see how this app would help me monitor my heart failure | 4.2 |
| I think that I would use the app daily | 3.6 |
| I would need someone to help me with the app | 2.4 |
There were several potential improvements identified by participants. First, some participants suggested tracking additional items, including heart palpitations, blood pressure, exercise, and water intake. Two participants also noted that they did not understand the word “fatigued.” Participants recommended adding specific features, such as reminders, instructions for using the HF app, patient-specific symptoms, and HF information to support symptom management.
Discussion
Currently there are few high-quality, commercially available mobile apps for the management of HF.18 Also, there is little peer-reviewed literature assessing the acceptability, functionality, and efficacy of such apps.18,19 We developed a HF symptom-tracking app and, as a critical first step, assessed the acceptability of the app with older adults. Because HF results in high healthcare utilization, specifically hospital readmissions, mobile apps such as the HF app may help patients, caregivers, and providers better manage HF symptoms, care utilization, and costs.20 The HF app is a usable program for tracking symptoms of HF, which is central to HF management. The feasibility of the HF app should be examined to determine whether older adults will use the program and enter symptom data over time.
Several improvements to the app should be incorporated for future use, and instructions for use should be provided to future users. Because age was associated with a need for assistance to use the app, instructions and support from caregivers will be important to engage older patients with the HF app. Final changes to the HF app should also include improvements in mobile platform capability (in addition to iPad) and specific HF information important to the patient.
HF is common in older adults, and acceptability of mobile apps is of key importance. Current barriers to mobile apps among older adults should not deter the development of digital programs that can be used to improve HF care. The HF app is a useful tool to help older patients with HF self-manage their symptoms, identify patterns and changes in symptoms, and ultimately prevent HF readmission. Next steps in this process will require updates to the HF app, followed by usability testing to observe and document standard usability metrics,21 followed by a randomized trial of the app efficacy for improving HF self-management and reduced hospital admissions and readmissions.
Acknowledgments
The authors thank DXY, Inc. for its assistance with the development of the HF symptom-tracker mobile application. This research was funded by the McGregor Foundation and the National Institute on Aging (T32AG044296-02).
Disclosure Statement
No competing financial interests exist.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: A report from the American Heart Association. Circulation 2015;131:e38-360. CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: A policy statement from the American Heart Association. Circ Heart Fail 2013;6:606–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Chronic diseases: The leading causes of death and disability in the United States. 2015. Available at: www.cdc.gov/chronicdisease/overview/index.htm (last accessed May16, 2016)
- 4.Centers for Disease Control and Prevention. Hospitalizations for patients aged 85 and over in the United Stated, 2000–2010. 2015. Available at: www.cdc.gov/nchs/products/databriefs/db182.htm (last accessed May16, 2016)
- 5.Anderson G. Chronic care: Making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation, 2010. Available at: www.rwjf.org/content/dam/farm/reports/reports/2010/rwjf54583 (last accessed May16, 2016) [Google Scholar]
- 6.Fitch PM, Pelizzari P, Pyenson FSA. The high cost of heart failure for the medicare population: An actuarial cost analysis. Milliman, 2015. Available at: http://us.milliman.com/uploadedFiles/insight/2015/heart-failure-cost-medicare-analysis.pdf (last accessed November29, 2016)
- 7.Bekelman DB, Havranek EP, Becker DM, Kutner JS, Peterson PN, Wittstein IS, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail 2007;13:643–648 [DOI] [PubMed] [Google Scholar]
- 8.Jurgens CY, Moser DK, Armola R, Carlson B, Sethares K, Riegel B, et al. Symptom clusters of heart failure. Res Nurs Health 2009;32:551–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-Management aspects of the improving chronic illness care breakthrough series: Implementation with diabetes and heart failure teams. Ann Behav Med 2002;24:80–87 [DOI] [PubMed] [Google Scholar]
- 10.Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: A systematic review of randomized controlled trials. BMC Cardiovasc Disord 2006;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schiff GD, Fung S, Speroff T, McNutt RA. Decompensated heart failure: symptoms, patterns of onset, and contributing factors. Am J Med 2003;114:625–630 [DOI] [PubMed] [Google Scholar]
- 12.Older Adults and Technology Use. Pew Research Center. 2014. Available at: www.pewinternet.org/files/2014/04/PIP_Seniors-and-Tech-Use_040314.pdf (last accessed May12, 2016)
- 13.Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Mobile phone-based telemonitoring for heart failure management: A randomized controlled trial. J Med Internet Res 2012;14:e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zan S, Agboola S, Moore SA, Parks KA, Kvedar JC, Jethwani K. Patient engagement with a mobile web-based telemonitoring system for heart failure self-management: A pilot study. JMIR MHealth UHealth 2015;3:e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alnosayan N, Lee E, Alluhaidan A, Chatterjee S, Houston-Feenstra L, Kagoda M, et al. MyHeart: An intelligent mHealth home monitoring system supporting heart failure self-care. In IEEE, 2014. Available at: http://ieeexplore.ieee.org/lpdocs/epic03/wrapper.htm?arnumber=7001860 (last accessed August26, 2016)
- 16.Baig MM, Gholamhosseini H, Connolly MJ. mHealth monitoring system for hospitalised older adults—Current issues and challenges. In: Adibi S, ed. Mobile health. Cham: Springer International Publishing, 2015. Available at: http://link.springer.com/10.1007/978-3-319-12817-7_14 (last accessed May10, 2016) [Google Scholar]
- 17.United Nations Foundation. Using mobile technologies for healthier aging. 2013. Available at: www.mhealthknowledge.org/sites/default/files/16_mhealth-and-aging-report.pdf (last accessed May10, 2016)
- 18.Masterson Creber RM, Maurer MS, Reading M, Hiraldo G, Hickey KT, Iribarren S. Review and analysis of existing mobile phone apps to support heart failure symptom monitoring and self-care management using the Mobile Application Rating Scale (MARS). JMIR MHealth UHealth 2016;4:e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cajita MI, Gleason KT, Han H-R. A systematic review of mHealth-based heart failure interventions: J Cardiovasc Nurs 2016;31:E10–E22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ketel C. Potentials of internet-based patient engagement and education programs to reduce hospital readmissions. Nurs Clin North Am 2015;50:283–291 [DOI] [PubMed] [Google Scholar]
- 21.Rajput ZA, Mbugua S, Amadi D, Chepngeno V, Saleem JJ, Anokwa Y, et al. Evaluation of an Android-based mHealth system for population surveillance in developing countries. J Am Med Inform Assoc 2012;19:655–659 [DOI] [PMC free article] [PubMed] [Google Scholar]