Abstract
Linear scleroderma en coup de sabre (LSCS) is the most common form of morphea on the scalp and its trichoscopic features have not been described yet. We report 2 adult women with LSCS with distinct dermoscopic findings. They both had an atrophic well-defined linear patch of alopecia on the frontotemporal scalp. Dermoscopy showed loss of follicular openings on a whitish skin surface; scattered black dots, broken hairs, and pili torti; and short thick linear and branching tortuous vessels on the periphery of the lesion. Pathology confirmed the diagnosis of LSCS in the 2 cases. This description of dermoscopic features in LSCS on the scalp may help in the early diagnosis of the disease.
Keywords: Scleroderma, Linear scleroderma en coup de sabre, Dermoscopy, Alopecia, Pili torti, Scarring alopecia, Cicatricial alopecia
Established Facts
Trichoscopic features of linear scleroderma on the scalp have not been described.
Novel Insights
This is the first description of the trichoscopic features of linear scleroderma on the scalp. We present thick telangiectatic vessels as a new trichoscopic sign of this disease.
Introduction
Linear scleroderma en coup de sabre (LSCS) is a form of morphea on the scalp and forehead characterized by linear sclerotic patches of the skin with fibrosis of the subcutaneous tissue. Mean age of onset is 13.6 years; it affects mainly children and more frequently males than females (2:1). Adult onset is uncommon, but also possible. Without treatment, the natural history of the disease is to cause local atrophy and, in some cases, deep involvement of the underlying muscle, bone and central nervous system with eventually additional morbidity. Early lesions may be clinically subtle, as patches of hair loss with varying erythema and hyperpigmentation [1]. However, despite scalp involvement with the consequent development of alopecia, trichoscopic features of LSCS have not been described yet.
We report 2 patients with LSCS with distinct dermoscopic features. Dermoscopic images were obtained with a dermatoscope connected to a smartphone (iPhone 6; Silicon Valley, CA, USA; and FotoFinder Handyscope®, Bad Birnbach, Germany).
Case Report
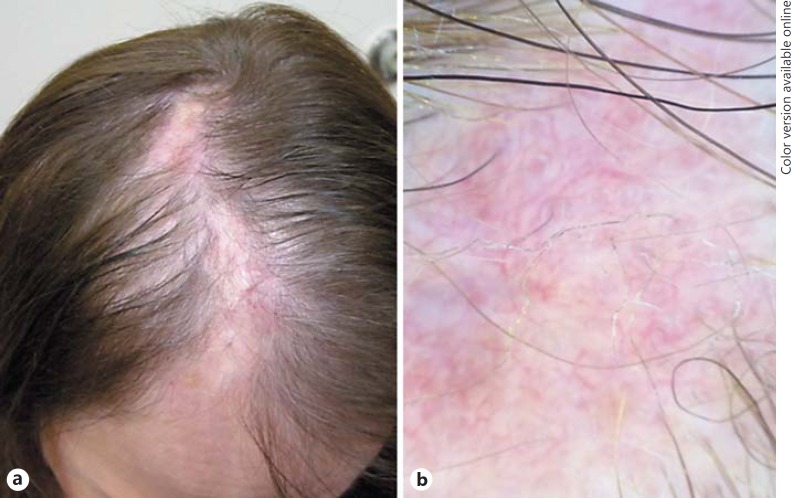
Two Caucasian women (54 and 63 years old) presented with progressive asymptomatic hair loss on the scalp. On examination, they both had an atrophic linear patch of alopecia on the frontotemporal scalp, well defined, without scaling or significant erythema. Some thin hairs could be observed in the center of the lesion. Trichoscopy showed loss of follicular openings on a whitish skin surface. Black dots, broken hairs and pili torti were also observed in a diffuse distribution. On the periphery of the lesion, we found a visible vascular pattern consisting of short thick linear and branching tortuous vessels (Fig. 1). A 4-mm scalp biopsy from the margin of the patches revealed thickening of the dermis and perivascular infiltrates of lymphocytes. Vessel walls showed endothelial swelling and edema. Diagnosis of LSCS was established in the 2 cases (Fig. 2).
Fig. 1.
a Well-defined linear patches of alopecia on the frontoparietal scalp. b Thick linear and branching vessels and loss of follicular opening on the scalp surface; isolated pili torti can be observed.
Fig. 2.
a Linear patch of alopecia on the frontal scalp. b Pili torti, broken hairs, and black dots broken hairs on a whitish skin surface.
Discussion
Dermoscopy has proven to be useful in the differential diagnosis of cicatricial alopecia and autoimmune diseases [2,3]. Dermatoscopic features of morphea have been reported in the literature. Campione et al. [4] described fibrotic beams and small whitish patches crossed by linear branching vessels that may exhibit a lilac ring. These findings correspond histopathologically to dermal sclerosis that is present in advanced fibrotic lesions [5,6]. In our case, the whitish skin surface was a clue of underlying fibrosis, and also other dermoscopic signs suggested the presence of dermal fibrosis. The identification of pili torti, black dots and broken hairs is correlated with the presence of perifollicular fibrosis. This fibrosis may distort the hair shaft inducing formation of pili torti that may easily break, leaving black dots or broken hairs [7]. The progressive sclerosis in LSCS causes a scarring alopecia that is confirmed by the lack of follicular openings in dermoscopy.
Interestingly, we observed in our 2 cases an ectatic subpapillary plexus consisting of thick telangiectatic vessels. This dermoscopic feature is similar to the vascular pattern observed in discoid lupus and dermatomyositis [8], but it has not been described in morphea lesions before. One possible explanation for this dermoscopic finding is that scalp vascularization is more prominent than in other anatomic locations and inflammatory changes of early LSCS could make it more visible to dermoscopy examination.
In conclusion, we describe the dermoscopic features of 2 cases of LSCS and present the thick telangiectatic vessels as a new dermoscopic sign in this disease. This dermoscopic feature may help in the early diagnosis of LSCS on the scalp enabling earlier treatment of patients.
Statement of Ethics
Verbal photographic and informed consent was obtained from the patients described in this article. The study protocol has been approved by the institute's committee on human research.
Disclosure Statement
The authors declare that they have no conflict of interest regarding this study. This article has no funding source.
References
- 1.Fett N, Werth VP. Update on morphea: part I. Epidemiology, clinical presentation, and pathogenesis. J Am Acad Dermatol. 2011;64:217–228. doi: 10.1016/j.jaad.2010.05.045. [DOI] [PubMed] [Google Scholar]
- 2.Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67:1040–1048. doi: 10.1016/j.jaad.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Lallas A, Giacomel J, Argenziano G, García-García B, González-Fernández D, Zalaudek I, Vázquez-López F. Dermoscopy in general dermatology: practical tips for the clinician. Br J Dermatol. 2014;170:514–526. doi: 10.1111/bjd.12685. [DOI] [PubMed] [Google Scholar]
- 4.Campione E, Paternò EJ, Diluvio L, Orlandi A, Bianchi L, Chimenti S. Localized morphea treated with imiquimod 5% and dermoscopic assessment of effectiveness. J Dermatolog Treat. 2009;20:10–13. doi: 10.1080/09546630802132668. [DOI] [PubMed] [Google Scholar]
- 5.Shim WH, Jwa SW, Song M, Kim HS, Ko HC, Kim MB, Kim BS. Diagnostic usefulness of dermatoscopy in differentiating lichen sclerous et atrophicus from morphea. J Am Acad Dermatol. 2012;66:690–691. doi: 10.1016/j.jaad.2011.06.042. [DOI] [PubMed] [Google Scholar]
- 6.Vázquez-López F, Kreusch J, Marghoob AA. Dermoscopic semiology: further insights into vascular features by screening a large spectrum of nontumoral skin lesions. Br J Dermatol. 2004;150:226–231. doi: 10.1111/j.1365-2133.2004.05753.x. [DOI] [PubMed] [Google Scholar]
- 7.Mirmirani P, Samimi SS, Mostow E. Pili torti: clinical findings, associated disorders, and new insights into mechanisms of hair twisting. Cutis. 2009;84:143–147. [PubMed] [Google Scholar]
- 8.Tosti A. Systemic diseases. In: Tosti A, editor. Dermoscopy of the Hair and Nails. Boca Raton: CRC Press; 2016. p. 107. [Google Scholar]