Abstract
Beard trichotillomania (TTM) is a rather uncommon entity. Hair is not easily plucked from the beard area, as patients need forceps or tweezers to perform their task. The diagnosis of beard TTM can be quite tricky as the location is not the most frequent one. Dermoscopy might in these cases be helpful to achieve the correct diagnosis. In this article, we describe for the first time the “pluck out sign” for beard TTM.
Keywords: Trichotillomania, Beard, Hair pulling, Dermoscopy, Impulse control disorder, Obsessive-compulsive disorder, Pluck out sign
Established Facts
Trichotillomania can be diagnosed by dermoscopy.
The differential diagnosis of trichotillomania and alopecia areata is tricky.
Novel Insights
Beard trichotillomania can be confusing.
Dermoscopy may be helpful to make the correct diagnosis.
Introduction
Trichotillomania (TTM) has previously been classified as an impulse control disorder in the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [1]. This criterion, applied to adults and children, includes an increased sense of tension immediately prior to hair pulling and subsequent pleasure or gratification when the hair has been pulled out. However, many patients, and in particular children, do not describe this phenomenon of tension and gratification related to hair pulling [2,3,4,5]. Therefore, in the recently released DSM-V criteria, TTM is included in “obsessive-compulsive and related disorders” [6].
Beard TTM is a very uncommon condition. Most patients affected by auto-induced alopecia choose a more easily accessible location to pluck out hair. In beard TTM, external devices, such as forceps or tweezers, might be needed in order to successfully fulfill the task.
We have recently seen a 14-year-old boy who presented with a rather peculiar type of beard TTM, which allowed us to describe for the first time the trichoscopic findings for beard TTM.
Clinical Case
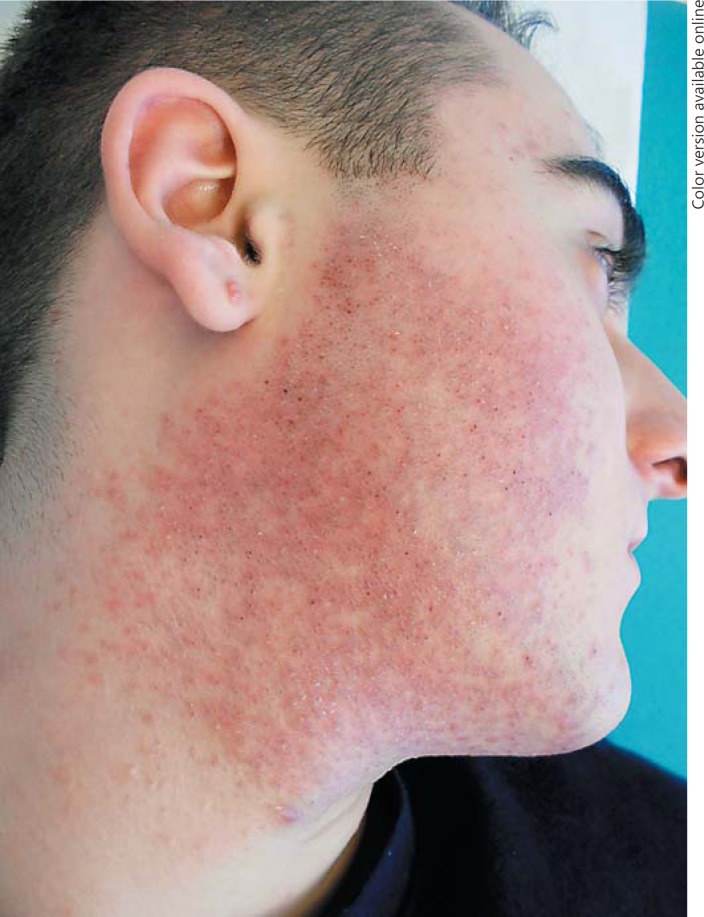
A 14-year-old boy presented to one of the authors (M.C.) with a peculiar dermatitis affecting the face which started 4 months previously. The first clinical impression was a type of irritant contact dermatitis or a rather extensive type of folliculitis (Fig. 1).
Fig. 1.
Clinical image of our patient who is affected by beard trichotillomania. The first clinical impression was an extensive irritant contact dermatitis or a widely located folliculitis.
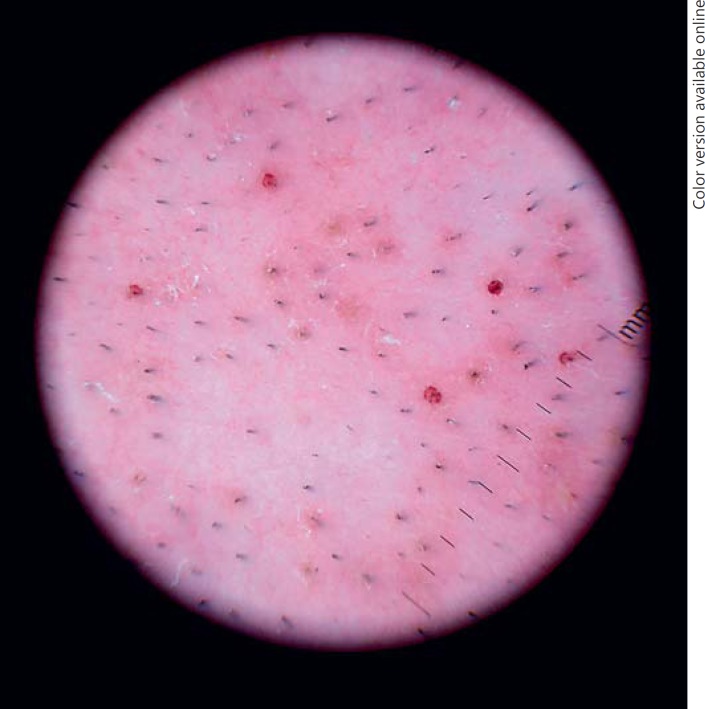
On a detailed clinical observation, the skin presented multiple erythematous papules and some pustules in a clearly demarcated beard location. In some areas, pseudo-folliculitis aspects were also observed. Under the dermatoscope, we observed typical round hemorrhages around the hair shafts that could be called the “pluck out sign” and are very suggestive of TTM (Fig. 2).
Fig. 2.
Dermoscopy revealed the presence of hemorrhages around the hair follicles; the “pluck out sign” is highly suggestive of trichotillomania.
We asked about the boy's shaving habits, and he denied any shaving: “I have never shaved before,” he stated. When we were talking with the mother, she said that he has a peculiar timetable as he usually gets up at 4 a.m., and after a very long shower, he studies until the time to go to school.
After a long talk with the boy, he admitted spending hours in front of the mirror after the shower and, using eyebrow tweezers (borrowed from his mother), plucking out all beard hair he could reach with the small depilatory device. Looking at his previous clinical history, we found that he had recovered on 2 occasions from acute abdominal pain that solved without treatment. He had also been examined for severe recurrent headaches that were not resolving with normal anti-inflammatory drugs and needed a scalp MRI that showed no significant findings. Both episodes were finally classified as somatic.
Discussion
In the past decade, increased attention has been paid to TTM, mainly within psychiatric and psychological circles. Not many papers have appeared in the dermatological literature [7,8,9]. In the case of a child with nonscarring alopecia of uncertain etiology, the differential diagnosis needs to explore other underlying causes of hair loss.
The most typical retroauricular locations of TTM may be very easy to diagnose, but in some peculiarly or weirdly located cases, the differential diagnosis with alopecia areata can be rather difficult. Classical pictures of alopecia areata reveal smooth and shiny alopecia patches with sharply limited borders. TTM, in turn, reveals multifocal and irregular alopecia patches formed by multiple broken hairs. Some reports, however, associate the two diseases which pose a diagnostic challenge to clinicians [7]. In this scenario, dermoscopy has emerged as a noninvasive and useful tool for the diagnosis of the disease [10,11,12,13]. Black dots, coiled hairs, shafts of various lengths, broom fibers, and V-sign (trichoptilosis) are suggestive of TTM. On the other hand, exclamation point hairs, which are suggestive of alopecia areata, are commonly absent in TTM [14,15,16]. Follicular microhemorrhages are a unique dermoscopic sign for the detection of coexisting TTM in cases of alopecia areata [11] and can be extremely useful in doubtful cases. In this paper, we describe the “pluck out sign” for beard TTM, which can be added to the previously described aspects of scalp TTM and could be helpful in the diagnosis.
The majority of studies on TTM to date have focused primarily on adults and adolescents and indicate that the most common age of onset is pre- or early adolescence (9–13 years) [8]. However, it is known that TTM frequently occurs in early childhood and has been reported from as early as 12 months of age [8]. A patient's age can influence the mechanism of his/her hair pulling. Two distinct types of hair pulling have been described for TTM: automatic and focused pulling [8]. Automatic pulling occurs outside of one's own awareness, while focused pulling, in contrast, occurs in awareness and in response to negative emotional states (stress, sadness, anger, or anxiety), intense thoughts or urges, or in an attempt to establish asymmetry [8]. Children more often fall within the automatic category, and therefore, they do not recall the actual pulling but may admit to “playing with hair” or they may have been noted to pull out their hair in a trance-like, disengaged state [8]. Our case could clearly be included in the focused pulling category, in this case with the idea to hide an early puberty that was not yet present in the rest of his classmates.
Panza et al. [4] demonstrated a developmental progression of the symptoms, with a significant increase in focused hair pulling with advancing age, while automatic pulling remained constant. Older children became more aware of their hair pulling urges and were less able to refrain from pulling [8].
In this article, we described for the first time the dermoscopic “pluck out sign” for beard TTM that hopefully will, in the future, help other physicians to achieve a correct diagnosis in difficult cases.
Statement of Ethics
The patient's consent was obtained for the pictures and eventual publication.
Disclosure Statement
The authors declare that they have no conflicts of interest.
References
- 1.American Psychiatric Association . ed 4, Text Revision. Washington: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 2.Oranje AP, Peereboom-Wynia JD, De Raeymaecker DM. Trichotillomania in childhood. J Am Acad Dermatol. 1986;15:614–619. doi: 10.1016/s0190-9622(86)70213-2. [DOI] [PubMed] [Google Scholar]
- 3.Stein DJ, Grant JE, Franklin ME, Keuthen N, Lochner C, Singer HS, et al. Trichotillomania (hair pulling disorder), skin picking disorder, and stereotypic movement disorder: toward DSM-V. Depress Anxiety. 2010;27:611–626. doi: 10.1002/da.20700. [DOI] [PubMed] [Google Scholar]
- 4.Panza KE, Pittenger C, Bloch MH. Age and gender correlates of pulling in pediatric trichotillomania. J Am Acad Child Adolesc Psychiatry. 2013;52:241–249. doi: 10.1016/j.jaac.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lochner C, Stein DJ, Woods D, Pauls DL, Franklin ME, Loerke EH, et al. The validity of DSM-IV-TR criteria B and C of hair-pulling disorder (trichotillomania): evidence from a clinical study. Psychiatry Res. 2011;189:276–280. doi: 10.1016/j.psychres.2011.07.022. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association . ed 5. Washington: American Psychiatric Association; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 7.Alves R, Grimalt R. Hair loss in children. Curr Probl Dermatol. 2015;47:55–66. doi: 10.1159/000369405. [DOI] [PubMed] [Google Scholar]
- 8.Chandran NS, Novak J, Iorizzo M, Grimalt R, Oranje AP. Trichotillomania in children. Skin Appendage Disord. 2015;1:18–24. doi: 10.1159/000371809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moreno-Romero JA, Grimalt R. Hair loss in infancy. G Ital Dermatol Venereol. 2014;149:55–78. [PubMed] [Google Scholar]
- 10.Abraham LS, Torres FN, Azulay-Abulafia L. Pistas dermatoscópicas para diferenciar a tricotilomania da alopecia areata em placa. An Bras Dermatol. 2010;85:723–726. doi: 10.1590/s0365-05962010000500022. [DOI] [PubMed] [Google Scholar]
- 11.Ise M, Amagai M, Ohyama M. Follicular microhemorrhage: a unique dermoscopic sign for the detection of coexisting trichotillomania in alopecia areata. J Dermatol. 2014;41:518–520. doi: 10.1111/1346-8138.12500. [DOI] [PubMed] [Google Scholar]
- 12.Shelleh HH, Khan SA, Al-Hatiti HS. Trichotillomania or alopecia areata. Int J Dermatol. 2006;45:1196–1198. doi: 10.1111/j.1365-4632.2006.02764.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee DY, Lee JH, Yang JM, Lee ES. The use of dermoscopy for the diagnosis of trichotillomania. J Eur Acad Dermatol Venereol. 2009;23:731–732. doi: 10.1111/j.1468-3083.2009.03193.x. [DOI] [PubMed] [Google Scholar]
- 14.Khunkhet S, Vachiramon V, Suchonwanit P. Trichoscopic clues for diagnosis of alopecia areata and trichotillomania in Asians. Int J Dermatol. 2017;56:161–165. doi: 10.1111/ijd.13453. [DOI] [PubMed] [Google Scholar]
- 15.Pinto ACVD, de Andrade TCPC, de Brito FF, da Silva GV, Cavalcante MLLL, Martelli ACC. Trichotillomania: a case report with clinical and dermatoscopic differential diagnosis with alopecia areata. An Bras Dermatol. 2017;92:118–120. doi: 10.1590/abd1806-4841.20175136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ankad BS, Naidu MV, Beergouder SL, Sujana L. Trichoscopy in trichotillomania: a useful diagnostic tool. Int J Trichology. 2014;6:160–163. doi: 10.4103/0974-7753.142856. [DOI] [PMC free article] [PubMed] [Google Scholar]