Abstract
Purpose
We characterized the neighborhood obesogenic environment in the Multiethnic Cohort (MEC) by examining the associations of obesity with attributes of the social and built environment, establishing a multi-level infrastructure for future cancer research.
Methods
For 102,906 African American, Japanese American, Latino, and white MEC participants residing predominately in Los Angeles County, baseline residential addresses (1993–1996) were linked to census and geospatial data, capturing neighborhood socioeconomic status (nSES), population density, commuting, food outlets, amenities, walkability, and traffic density. We examined neighborhood attributes and obesity (body mass index ≥30 kg/m2) associations using multinomial logistic regression, adjusting for individual-level (e.g., demographics, physical activity, and diet) and neighborhood-level factors.
Results
NSES was associated with obesity among African Americans, Latinos, and whites (p-trend≤0.02), with two-fold higher odds (adjusted odds ratios, 95% confidence intervals) for living in the lowest versus highest quintile among African American women (2.07, 1.62–2.65), white men (2.11, 1.29–3.44), and white women (2.50, 1.73–3.61). Lower density of businesses among African American and white women and lower traffic density among white men were also associated with obesity (p-trends≤0.02).
Conclusions
Our study highlights differential impacts of neighborhood factors across racial/ethnic groups and establishes the foundation for multi-level studies of the neighborhood context and obesity-related cancers.
Keywords: environment: neighborhood environment, obesity, race/ethnicity, socioeconomic status
INTRODUCTION
While considerable progress and success has been made in identifying individual-level risk factors for cancer, the contextual environments in which these risk factors operate remain poorly understood. The neighborhood obesogenic environment, encompassing the socioeconomic and built environments relevant to energy imbalance that promote obesity (1), has only recently been considered for its role across the cancer continuum (2). Moreover, the neighborhood obesogenic environment may be particularly relevant for racial/ethnic minorities and low-socioeconomic status (SES) populations, who often live in poorer neighborhoods and experience a higher prevalence of obesity and obesity-related cancers. Neighborhood environments are recognized social determinants of health and racial/ethnic disparities in health outcomes (3) and may be related to health outcomes independent of individual-level risk factors (4, 5). An emerging body of literature has begun to document independent neighborhood associations with risk of breast cancer (6–9) and colorectal cancer (10, 11) and breast cancer survival (12–15). As obesity is a risk factor for these cancers and associated with worse cancer outcomes (16, 17), a better understanding of the neighborhood obesogenic environments, especially within minority groups, will inform contextual studies of cancer incidence and mortality and potential intervention efforts (18–20).
In the last decade, there has been a growing recognition of the contextual impact of residential neighborhoods on obesity (reviewed in: (21–24)). Specific neighborhood environments associated with obesity include lower socioeconomic status (SES) (25–27), unhealthy food environments (28–32), lower walkability (e.g., street connectivity, walkable destinations, higher population density) (33, 34), more commuting (e.g., automobile dependency, proportion of residents who commute by car/motorcycle, or average time spent commuting ) (35, 36), and higher perceived traffic density (37, 38). Proximity to recreational facilities and parks is also associated with lower body mass index (BMI) (39, 40). Few studies have specifically examined racial/ethnic differences and most focused only on nSES without considering the built environment (27, 41–45). No study has comprehensively examined the obesogenic environment and obesity across multiple racial/ethnic groups.
To address this gap and provide a multi-level infrastructure for future epidemiologic studies on the neighborhood environment and obesity-related cancers, we characterized the neighborhood obesogenic environment for 102,906 California Multiethnic Cohort (MEC) participants at baseline and examined the likelihood of being obese or overweight. The MEC, a large population-based prospective study, was established to investigate risk factors for cancer, largely focusing on diet, health-related behaviors, and biological and genetic factors, among five U.S. racial/ethnic groups: African Americans, Japanese Americans, Latinos, Native Hawaiians, and whites (46, 47). The MEC provides a diverse study population with well-characterized follow-up information on residential histories, questionnaire data, and health outcomes that allows for a rigorous prospective evaluation of the role of neighborhood- and individual-level risk factors across the cancer continuum. In concert, the California Neighborhoods Data System, an integrated system of small area-level measures of the social and built environment for California, offers a unique resource to investigate neighborhood associations through linkage with residential geocodes (48). We hypothesize that lower nSES, lower population density, higher proportion of residents commuting by car/motorcycle, more unhealthy food outlets, fewer neighborhood amenities measured by number of businesses, and fewer parks, and higher traffic density are associated with obesity and associations differ across racial/ethnic groups.
MATERIALS AND METHODS
Study Subjects
Methodological details of the MEC have been described previously (47). Briefly, from 1993 through 1996, 215,831 men and women between 45 and 75 years of age from Hawaii and California (primarily Los Angeles County) were enrolled in the MEC. At cohort entry, participants completed a 26-page questionnaire with items pertaining to demographic characteristics, anthropometrics, medical history, family history, reproductive history, cancer screening practices, occupational history, physical activity, and diet. For this study of California MEC participants (n=107,635) that included four racial/ethnic groups (African Americans, Japanese Americans, Latinos, and whites), we excluded participants with missing or extreme/outlier values for self-reported height or weight that resulted in extreme body mass index (BMI, <15, >50 kg/m2, n=2,411) and those with residential addresses that could not be geocoded (n=2,318). Data on the remaining 102,906 MEC participants were available for the present analysis. This study was approved by the institutional review boards at participating institutions.
Address History and Geocoding
The MEC, which recruited participants via personal mailings, actively maintains accurate and up-to-date addresses on all participants since its inception via periodic mailings of newsletters and questionnaires, as well as linkages with administrative and other databases. For this current analysis, residential baseline addresses of California MEC participants were geocoded to latitude and longitude coordinates using parcel data, and then street centerline data for those that failed to geocode to a parcel.
California Neighborhoods Data System
Characterization of the neighborhood obesogenic environment was based on nSES and built environment attributes (i.e. population density, % commute by car/motorcycle, Restaurant Environment Index (REI), Retail Food Environment Index (RFEI), number of businesses, number of parks, traffic density, number or recreational facilities, and street connectivity). These ten neighborhood attributes were defined using census, business, farmers markets, parks, and traffic data curated in the California Neighborhoods Data System (48). For census data, geocodes of baseline addresses were linked to 7,947 unique 1990 U.S. Census block groups, an area with an average of 1,500 residents and representing our neighborhood unit. Census data included: nSES, a validated composite measure created by principal component analysis of data on education, housing, employment, occupation, income, and poverty (49); population density (persons per km2); and commute patterns (proportion of residents who commute to work by car/motorcycle). These measures were categorized into quintiles based on their distributions across Los Angeles County block groups (95% of the California MEC sample resides in Los Angeles County). For businesses, farmers’ markets, and parks data, geocodes of baseline addresses were used to create a one-mile pedestrian network distance to quantify the neighborhood environment. The REI was defined as the ratio of the number of fast-food restaurants to other restaurants. The RFEI was defined as the ratio of the number of convenience stores, liquor stores, and fast-food restaurants to supermarkets and farmers’ markets (50). Information on the number/type of businesses was based on business listings derived from Walls & Associates’ National Establishment Time-Series Database from 1990–2008 (51) and a three-year business activity window (i.e., for each MEC participant, one year prior to study entry, study entry year, one-year post study entry). Parks and street connectivity were based on data from Navteq’s NavStreets database (52), and farmers’ markets listings from the California Department of Food and Agriculture (53). Street connectivity (54) was measured using the gamma index, a commonly used measure of walkability, and defined as the ratio of actual number of street segments to maximum possible number of intersections. Traffic density, within a 500 meter radius buffer of a participant’s geocoded residence, was based on traffic counts from the California Department of Transportation (2000) (55) and previously described methods (56). These neighborhood business and traffic-related attributes were categorized into quartiles or quintiles according to the overall study participant distribution (Table 1).
Table 1.
Distribution of neighborhood environment characteristics among men and women residing in California by race/ethnicity, Multiethnic Cohort, 1993–1996.
| Neighborhood Attributes |
Men
|
Women
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All (n=44,223) |
African Americans (n=11,466) |
Japanese Americans (n=6,042) |
Latinos (n=21,625) |
Whites (n=5,090) |
All (n=58,683) |
African Americans (n=20,266) |
Japanese Americans (n=6,296) |
Latinos (n=23,006) |
Whites (n=9,115) |
|
|
|
|
|||||||||
| % | % | % | % | % | % | % | % | % | % | |
| Neighborhood SESa,b | ||||||||||
| Quintile 1: low | 23.0 | 33.8 | 5.1 | 25.6 | 9.3 | 25.2 | 37.7 | 4.8 | 26.9 | 7.3 |
| Quintile 2 | 25.4 | 28.6 | 12.4 | 29.7 | 15.6 | 26.2 | 29.5 | 12.4 | 31.3 | 15.9 |
| Quintile 3 | 20.1 | 16.5 | 24.2 | 21.0 | 19.8 | 20.0 | 15.5 | 24.7 | 21.6 | 22.7 |
| Quintile 4 | 18.2 | 15.6 | 30.0 | 14.5 | 26.1 | 17.4 | 13.5 | 30.6 | 13.3 | 27.1 |
| Quintile 5: high | 13.1 | 5.5 | 28.3 | 9.1 | 29.1 | 11.2 | 3.9 | 27.5 | 6.9 | 26.9 |
| Population density (persons per km2)b | ||||||||||
| Quintile 1: low | 16.5 | 11.8 | 22.1 | 14.2 | 30.6 | 14.7 | 9.2 | 21.8 | 12.5 | 27.9 |
| Quintile 2 | 17.0 | 12.6 | 24.0 | 16.8 | 19.7 | 16.1 | 11.5 | 23.7 | 15.9 | 21.4 |
| Quintile 3 | 22.8 | 23.3 | 26.5 | 22.3 | 19.4 | 22.6 | 22.2 | 26.7 | 22.1 | 21.6 |
| Quintile 4 | 23.3 | 29.5 | 17.1 | 23.2 | 16.9 | 25.1 | 31.7 | 18.1 | 24.3 | 17.5 |
| Quintile 5: high | 20.3 | 22.8 | 10.3 | 23.5 | 13.4 | 21.5 | 25.5 | 9.8 | 25.1 | 11.5 |
| % commute by car/motorcycleb | ||||||||||
| Quintile 1: low | 18.4 | 25.2 | 9.1 | 19.0 | 11.8 | 19.7 | 27.1 | 8.9 | 20.4 | 9.3 |
| Quintile 2 | 18.9 | 22.1 | 13.4 | 19.5 | 16.0 | 19.9 | 23.8 | 14.6 | 19.8 | 15.3 |
| Quintile 3 | 18.9 | 17.7 | 19.4 | 19.6 | 18.3 | 18.9 | 17.4 | 19.0 | 19.9 | 19.3 |
| Quintile 4 | 22.1 | 18.2 | 27.9 | 21.5 | 26.2 | 21.3 | 17.1 | 28.3 | 20.7 | 27.5 |
| Quintile 5: high | 21.6 | 16.8 | 30.0 | 20.4 | 27.6 | 20.1 | 14.6 | 29.1 | 19.2 | 28.6 |
| REIc,d | ||||||||||
| 0 | 17.2 | 10.6 | 20.2 | 18.8 | 22.4 | 15.8 | 8.7 | 20.2 | 18.0 | 22.8 |
| Quartile 1: low | 20.1 | 13.3 | 28.1 | 21.0 | 21.8 | 19.4 | 13.2 | 28.4 | 21.6 | 21.2 |
| Quartile 2 | 19.4 | 17.9 | 21.9 | 19.7 | 18.8 | 20.0 | 19.0 | 22.3 | 20.5 | 19.5 |
| Quartile 3 | 19.7 | 23.2 | 13.9 | 20.5 | 14.9 | 20.2 | 23.7 | 13.5 | 21.2 | 14.7 |
| Quartile 4: high, <1 | 17.6 | 28.4 | 9.6 | 15.5 | 11.2 | 19.2 | 30.3 | 9.5 | 14.8 | 12.2 |
| Quartile 4: high, ≥1 | 2.3 | 2.9 | 2.1 | 2.0 | 2.3 | 2.1 | 2.6 | 2.2 | 1.6 | 2.2 |
| No restaurant | 3.8 | 3.8 | 4.3 | 2.5 | 8.6 | 3.4 | 2.5 | 4.0 | 2.3 | 7.4 |
| RFEIe,d | ||||||||||
| 0 | 3.6 | 1.6 | 4.9 | 3.6 | 6.6 | 3.0 | 1.2 | 4.6 | 3.0 | 5.9 |
| Quartile 1: low | 23.0 | 18.4 | 18.1 | 27.8 | 18.3 | 22.4 | 18.6 | 17.8 | 29.1 | 17.1 |
| Quartile 2 | 22.2 | 23.6 | 18.7 | 23.1 | 19.3 | 22.9 | 24.5 | 19.1 | 24.1 | 19.0 |
| Quartile 3 | 22.5 | 24.4 | 23.8 | 21.1 | 22.2 | 23.1 | 25.4 | 23.8 | 21.0 | 22.8 |
| Quartile 4: high | 25.7 | 28.8 | 30.7 | 22.8 | 25.8 | 25.8 | 28.1 | 30.9 | 21.4 | 28.4 |
| No retail food | 3.1 | 3.3 | 3.7 | 1.7 | 7.7 | 2.8 | 2.2 | 3.8 | 1.4 | 6.7 |
| Number of businessesd | ||||||||||
| Quintile 1: low | 18.6 | 17.3 | 14.1 | 19.8 | 21.6 | 17.5 | 15.3 | 14.1 | 18.4 | 22.3 |
| Quintile 2 | 20.7 | 20.2 | 14.0 | 23.4 | 18.3 | 20.5 | 19.7 | 13.0 | 23.6 | 19.6 |
| Quintile 3 | 19.7 | 24.9 | 14.1 | 19.1 | 17.4 | 21.2 | 26.7 | 13.5 | 19.6 | 18.5 |
| Quintile 4 | 20.2 | 23.0 | 22.3 | 19.0 | 16.5 | 21.0 | 24.3 | 23.3 | 19.3 | 16.4 |
| Quintile 5: high | 20.8 | 14.6 | 35.6 | 18.7 | 26.2 | 19.8 | 14.0 | 36.0 | 19.1 | 23.3 |
| Number of parksd | ||||||||||
| 0 | 25.4 | 26.2 | 22.4 | 25.0 | 28.8 | 25.0 | 25.1 | 21.5 | 24.8 | 28.1 |
| 1 | 37.4 | 35.4 | 35.7 | 39.9 | 33.6 | 37.6 | 36.8 | 36.4 | 39.3 | 35.6 |
| 2 | 23.5 | 23.0 | 23.5 | 23.8 | 22.8 | 23.7 | 23.5 | 24.4 | 24.5 | 21.9 |
| ≥3 | 13.8 | 15.4 | 18.4 | 11.4 | 14.8 | 13.7 | 14.6 | 17.7 | 11.5 | 14.3 |
| Traffic density (vehicle miles/mile2)d | ||||||||||
| Quintile 1: low | 19.1 | 15.7 | 22.7 | 18.5 | 25.5 | 17.5 | 13.3 | 21.8 | 17.1 | 24.7 |
| Quintile 2 | 20.7 | 19.9 | 20.5 | 22.0 | 16.9 | 20.5 | 19.7 | 20.5 | 21.8 | 18.8 |
| Quintile 3 | 20.1 | 22.5 | 17.2 | 20.4 | 17.1 | 20.9 | 22.8 | 17.7 | 20.8 | 18.9 |
| Quintile 4 | 19.7 | 24.0 | 21.4 | 16.7 | 20.2 | 21.0 | 26.1 | 21.3 | 17.4 | 18.6 |
| Quintile 5: high | 20.4 | 17.9 | 18.1 | 22.3 | 20.4 | 20.1 | 18.0 | 18.7 | 22.9 | 19.0 |
| Number of recreational facilitiesd | ||||||||||
| 0 | 25.7 | 29.8 | 18.0 | 24.9 | 29.2 | 25.6 | 28.2 | 18.0 | 24.4 | 27.7 |
| 1 | 23.3 | 22.9 | 20.7 | 25.5 | 18.2 | 24.0 | 24.7 | 20.4 | 25.9 | 19.9 |
| 2 | 18.8 | 22.2 | 16.1 | 18.7 | 15.1 | 19.2 | 22.2 | 16.1 | 18.8 | 15.7 |
| ≥3 | 32.1 | 25.0 | 45.2 | 30.9 | 37.5 | 31.3 | 24.9 | 45.5 | 30.9 | 36.7 |
| Street connectivity, Gamma indexd,f | ||||||||||
| Quintile 1: low | 25.7 | 13.8 | 31.5 | 28.5 | 34.0 | 23.7 | 12.0 | 31.5 | 27.4 | 34.5 |
| Quintile 2 | 22.0 | 17.1 | 27.1 | 23.5 | 21.0 | 21.1 | 15.7 | 27.2 | 23.5 | 22.9 |
| Quintile 3 | 17.8 | 17.5 | 17.0 | 18.3 | 16.9 | 18.1 | 18.0 | 16.7 | 19.4 | 16.2 |
| Quintile 4 | 17.4 | 24.1 | 12.4 | 16.0 | 13.9 | 18.3 | 25.1 | 12.1 | 16.0 | 13.3 |
| Quintile 5: high | 17.1 | 27.5 | 12.0 | 13.7 | 14.2 | 18.8 | 29.2 | 12.5 | 13.6 | 13.1 |
Based on SES composite index of seven indicator variables for Census block groups (Liu education index, proportion with a blue collar job, proportion older than age 16 in the workforce without a job, median household income, percent below 200% of the poverty line, median rent, median house value).
U.S. Census block group-level measure; categories based on distribution for block groups in Los Angeles County.
Ratio of the number of fast-food restaurants to other restaurants.
Businesses/parks within walking distance of residence (1.6 km pedestrian network) or traffic density within 0.5 km radius of residence; quintiles/quartiles based on study participant distribution.
Ratio of the average number of convenience stores, liquor stores, and fast-food restaurants to supermarkets and farmers’ markets.
Ratio of actual number of street segments to maximum possible number of intersections.
BMI and health behaviors at baseline
Self-reported height and weight were used to calculate BMI, which was categorized as normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2). Smoking status was assessed by asking participants if they had ever smoked more than 20 packs of cigarettes in their lifetime. Those reporting ‘no’ were considered to be never smokers; those reporting ‘yes, but I quit smoking’ were former smokers; and those reporting ‘yes, and I currently smoke’ were classified as current smokers. Physical activity was estimated as self-reported number of hours per day spent engaging in moderate or vigorous activities, on average, in the year prior to MEC cohort entry. In a MEC validation study, self-reported physical activity showed reasonably good correlation with an objective measure of total energy expenditure based on a doubly-labeled water standard (57).
Dietary assessment
Dietary intake information was obtained using a self-administered Quantitative Food Frequency Questionnaire (QFFQ) designed for this multiethnic population. Food items were identified from 3 days of measured food records as the minimum set that could explain ≥ 85% of the nutrient intake for each racial/ethnic group (47). Foods traditionally consumed by each targeted racial/ethnic population were added to the questionnaire regardless of their contribution to nutrient intake. A calibration study of the QFFQ was conducted using three 24-hour recalls from a random subsample of participants and revealed an acceptable correlation between the QFFQ and 24-hour recalls for energy-adjusted nutrients for each sex-ethnic group (58). Nutrient and food intake values were computed from the QFFQ using the food composition database designed and maintained by the University of Hawaii Cancer Center (47).
Statistical Analyses
Associations of the neighborhood obesogenic attributes and BMI categories at study baseline were examined using multivariable multinomial regression models to estimate odds ratios (OR) and 95% confidence intervals (CI) of being overweight or obese versus normal weight, with adjustment for clustering by block group. Potential neighborhood (Table 1) and individual-level (Supplemental Table 1) factors of interest were selected a priori, but only factors that reached statistical significance in age-adjusted models were retained in the multivariable model (see footnotes for Tables 2 and 3 for variables included in models). Due to evidence of significant heterogeneity, results are presented separately by sex (p-heterogeneity<0.01 for all neighborhood factors, except parks) and race/ethnicity (p-heterogeneity<0.05 for all neighborhood factors, except REI and traffic density). Trend tests were performed by entering the categorical variable as an ordinal parameter in the corresponding model. We also applied multivariable linear regression models to examine associations with continuous BMI, with adjustment for clustering by block group (Supplemental Table 2). Subgroup analyses were conducted that included models for Latinos categorized by location of birth (U.S. versus foreign) (15, 59) and Asian-specific BMI categories for Japanese Americans (normal weight (18.5–22.9 kg/m2), overweight (23.0–27.4 kg/m2), obese (≥ 27.5 kg/m2)) (60, 61). All p values presented are two-sided. A P threshold < 0.05 was used to determine statistical significance. Analyses were conducted using SAS (version 9.3, Cary, NC).
Table 2.
Association between the neighborhood environment and being overweight or obesea among men residing in California by race/ethnicity, Multiethnic Cohort, 1993–1996.
| Neighborhood Attributes | African Americans (n=11,466) | Japanese Americans (n=6,042) | Latinos (n=21,625) | Whites (n=5,090) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Overweight vs. Normal Weight | Obese vs. Normal Weight | Overweight vs. Normal Weight | Obese vs. Normal Weight | Overweight vs. Normal Weight | Obese vs. Normal Weight | Overweight vs. Normal Weight | Obese vs. Normal Weight | |
|
| ||||||||
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Neighborhood SESb,c | ||||||||
| Quintile 5: high | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 4 | 1.01 (0.80–1.26) | 1.13 (0.85–1.51) | 1.03 (0.88–1.20) | 1.69 (1.15–2.49) | 1.01 (0.89–1.16) | 1.16 (0.95–1.40) | 1.09 (0.9–1.31) | 1.48 (1.13–1.95) |
| Quintile 3 | 1.15 (0.92–1.44) | 1.51 (1.11–2.04) | 1.05 (0.88–1.25) | 1.06 (0.66–1.69) | 1.12 (0.98–1.29) | 1.33 (1.09–1.61) | 1.29 (1.03–1.61) | 1.75 (1.27–2.41) |
| Quintile 2 | 1.09 (0.87–1.37) | 1.37 (1.02–1.85) | 1.02 (0.79–1.32) | 0.86 (0.45–1.63) | 1.08 (0.93–1.24) | 1.43 (1.17–1.74) | 1.33 (1.03–1.73) | 2.00 (1.39–2.88) |
| Quintile 1: low | 1.21 (0.94–1.55) | 1.48 (1.07–2.06) | 0.99 (0.69–1.42) | 1.78 (0.77–4.13) | 1.17 (0.98–1.39) | 1.52 (1.21–1.91) | 1.34 (0.94–1.91) | 2.11 (1.29–3.44) |
| Ptrend | 0.07 | 0.02 | 0.79 | 0.89 | 0.08 | <0.01 | 0.02 | <0.01 |
| Population density (persons per km2)c | ||||||||
| Quintile 5: high | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 4 | 1.07 (0.93–1.23) | 1.13 (0.94–1.35) | 1.02 (0.79–1.32) | 0.70 (0.36–1.33) | 1.03 (0.93–1.16) | 1.11 (0.97–1.27) | 0.81 (0.63–1.05) | 0.87 (0.59–1.27) |
| Quintile 3 | 1.11 (0.94–1.30) | 1.02 (0.81–1.28) | 1.22 (0.93–1.60) | 0.65 (0.35–1.22) | 1.00 (0.88–1.13) | 1.07 (0.92–1.24) | 0.79 (0.60–1.06) | 0.78 (0.52–1.17) |
| Quintile 2 | 1.00 (0.83–1.20) | 1.10 (0.86–1.42) | 1.13 (0.86–1.49) | 0.69 (0.36–1.31) | 0.93 (0.82–1.06) | 1.01 (0.86–1.20) | 0.82 (0.61–1.09) | 0.77 (0.50–1.18) |
| Quintile 1: low | 1.03 (0.84–1.27) | 1.10 (0.81–1.49) | 1.11 (0.83–1.50) | 0.88 (0.45–1.71) | 0.92 (0.80–1.05) | 0.99 (0.83–1.18) | 0.87 (0.65–1.16) | 0.76 (0.50–1.15) |
| Ptrend | 0.96 | 0.69 | 0.59 | 0.82 | 0.07 | 0.52 | 0.71 | 0.21 |
| % commute by car/motorcyclec | ||||||||
| Quintile 1: low | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 2 | 1.00 (0.87–1.15) | 1.07 (0.89–1.28) | 0.88 (0.67–1.16) | 0.92 (0.47–1.77) | 1.03 (0.92–1.16) | 0.97 (0.84–1.12) | 1.28 (0.96–1.69) | 1.31 (0.87–1.98) |
| Quintile 3 | 1.07 (0.92–1.25) | 1.01 (0.82–1.23) | 0.93 (0.71–1.23) | 1.19 (0.59–2.40) | 0.96 (0.84–1.08) | 0.96 (0.82–1.12) | 1.09 (0.80–1.47) | 1.47 (0.98–2.18) |
| Quintile 4 | 1.12 (0.94–1.32) | 1.21 (0.97–1.52) | 0.89 (0.67–1.19) | 1.02 (0.52–2.00) | 0.98 (0.86–1.12) | 1.03 (0.87–1.21) | 1.40 (1.03–1.89) | 1.54 (1.02–2.34) |
| Quintile 5: high | 1.10 (0.92–1.31) | 1.02 (0.80–1.30) | 0.96 (0.71–1.29) | 1.08 (0.53–2.18) | 0.97 (0.84–1.13) | 1.09 (0.91–1.30) | 1.42 (1.03–1.96) | 1.78 (1.15–2.76) |
| Ptrend | 0.15 | 0.54 | 0.80 | 0.90 | 0.57 | 0.21 | 0.03 | 0.01 |
| REId,e | ||||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quartile 1: low | 0.90 (0.72–1.11) | 0.81 (0.61–1.07) | 1.10 (0.89–1.35) | 0.89 (0.55–1.45) | 0.91 (0.81–1.03) | 0.89 (0.76–1.05) | 1.01 (0.79–1.30) | 1.10 (0.79–1.52) |
| Quartile 2 | 1.01 (0.82–1.23) | 0.89 (0.69–1.15) | 1.04 (0.85–1.28) | 0.85 (0.49–1.46) | 0.93 (0.82–1.04) | 1.04 (0.89–1.22) | 1.05 (0.82–1.35) | 1.03 (0.75–1.43) |
| Quartile 3 | 0.97 (0.80–1.17) | 0.88 (0.68–1.12) | 1.02 (0.82–1.27) | 0.74 (0.44–1.27) | 0.91 (0.81–1.03) | 0.96 (0.82–1.13) | 1.00 (0.77–1.29) | 0.85 (0.60–1.21) |
| Quartile 4: high, <1 | 0.90 (0.74–1.10) | 0.78 (0.61–1.01) | 1.01 (0.79–1.31) | 0.74 (0.41–1.32) | 0.88 (0.77–1.00) | 0.91 (0.77–1.09) | 0.93 (0.71–1.21) | 0.81 (0.57–1.17) |
| Quartile 4: high, ≥1 | 1.20 (0.83–1.73) | 1.16 (0.73–1.83) | 0.96 (0.63–1.48) | 2.24 (0.92–5.48) | 0.84 (0.64–1.11) | 0.90 (0.64–1.25) | 1.37 (0.84–2.23) | 1.32 (0.71–2.46) |
| No restaurant | 0.72 (0.49–1.06) | 0.76 (0.46–1.26) | 1.07 (0.72–1.58) | 0.89 (0.44–1.82) | 0.87 (0.65–1.15) | 0.74 (0.53–1.04) | 1.02 (0.76–1.37) | 0.93 (0.60–1.45) |
| Ptrendg | 0.94 | 0.46 | 0.71 | 0.77 | 0.09 | 0.65 | 0.86 | 0.16 |
| RFEIe,f | ||||||||
| 0 | 1.33 (0.88–2.03) | 0.93 (0.52–1.66) | 1.08 (0.82–1.42) | 0.95 (0.47–1.90) | 0.89 (0.72–1.10) | 0.90 (0.68–1.19) | 1.06 (0.74–1.51) | 0.95 (0.55–1.63) |
| Quartile 1: low | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quartile 2 | 0.84 (0.73–0.97) | 0.79 (0.66–0.95) | 1.01 (0.83–1.23) | 1.06 (0.64–1.74) | 1.10 (1.00–1.21) | 1.08 (0.96–1.22) | 0.98 (0.78–1.22) | 1.25 (0.92–1.71) |
| Quartile 3 | 0.95 (0.82–1.11) | 0.84 (0.69–1.02) | 1.16 (0.96–1.41) | 1.18 (0.72–1.93) | 1.02 (0.92–1.13) | 1.07 (0.94–1.21) | 0.94 (0.75–1.17) | 1.06 (0.78–1.45) |
| Quartile 4: high | 0.99 (0.84–1.16) | 0.95 (0.78–1.16) | 1.10 (0.91–1.33) | 1.10 (0.69–1.75) | 1.11 (1.00–1.25) | 1.05 (0.91–1.21) | 1.10 (0.89–1.37) | 1.23 (0.91–1.67) |
| No retail food | 1.02 (0.67–1.57) | 0.89 (0.52–1.53) | 1.04 (0.66–1.66) | 1.83 (0.84–3.97) | 1.10 (0.76–1.60) | 1.29 (0.87–1.91) | 1.15 (0.81–1.65) | 1.14 (0.61–2.12) |
| Ptrendg | 0.87 | 1.00 | 0.27 | 0.61 | 0.05 | 0.32 | 0.61 | 0.34 |
| Number of businessese | ||||||||
| Quintile 5: high | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 4 | 1.05 (0.89–1.24) | 1.09 (0.88–1.34) | 1.09 (0.93–1.27) | 1.26 (0.83–1.90) | 1.07 (0.96–1.19) | 1.11 (0.96–1.28) | 0.96 (0.76–1.21) | 0.82 (0.59–1.14) |
| Quintile 3 | 0.97 (0.82–1.16) | 1.18 (0.95–1.47) | 0.90 (0.75–1.09) | 1.16 (0.73–1.85) | 1.10 (0.99–1.24) | 1.05 (0.91–1.22) | 0.79 (0.62–1.00) | 1.01 (0.72–1.41) |
| Quintile 2 | 0.98 (0.81–1.18) | 1.12 (0.88–1.43) | 0.87 (0.70–1.08) | 1.28 (0.79–2.09) | 1.12 (1.00–1.26) | 1.04 (0.89–1.20) | 0.92 (0.71–1.19) | 1.11 (0.78–1.58) |
| Quintile 1: low | 1.02 (0.82–1.27) | 1.24 (0.93–1.66) | 0.89 (0.69–1.14) | 0.75 (0.41–1.35) | 1.17 (1.03–1.33) | 1.17 (0.99–1.38) | 0.83 (0.63–1.09) | 0.96 (0.64–1.42) |
| Ptrend | 0.73 | 0.18 | 0.13 | 0.79 | 0.02 | 0.26 | 0.21 | 0.67 |
| Number of parkse | ||||||||
| ≥3 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 0.79 (0.68–0.91) | 0.86 (0.71–1.04) | 0.92 (0.77–1.10) | 1.08 (0.71–1.63) | 1.01 (0.89–1.14) | 0.88 (0.75–1.02) | 0.99 (0.80–1.22) | 0.85 (0.63–1.14) |
| 1 | 0.88 (0.76–1.01) | 0.88 (0.74–1.06) | 1.12 (0.95–1.33) | 1.42 (0.96–2.10) | 0.97 (0.87–1.10) | 0.88 (0.76–1.01) | 0.91 (0.74–1.12) | 0.82 (0.62–1.10) |
| 0 | 0.86 (0.74–0.99) | 0.82 (0.68–1.00) | 1.04 (0.87–1.25) | 0.81 (0.51–1.27) | 0.96 (0.85–1.09) | 0.84 (0.72–0.98) | 0.88 (0.70–1.09) | 0.88 (0.65–1.20) |
| Ptrend | 0.54 | 0.13 | 0.47 | 0.99 | 0.28 | 0.06 | 0.33 | 0.44 |
| Traffic density (vehicle miles/mile2)e | ||||||||
| Quintile 1: low | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 2 | 1.14 (0.98–1.34) | 1.02 (0.84–1.26) | 1.00 (0.85–1.19) | 1.16 (0.76–1.78) | 1.01 (0.90–1.12) | 0.97 (0.84–1.12) | 0.99 (0.79–1.25) | 0.90 (0.66–1.21) |
| Quintile 3 | 1.06 (0.89–1.26) | 0.99 (0.79–1.25) | 1.05 (0.85–1.28) | 1.16 (0.72–1.87) | 1.02 (0.91–1.15) | 0.93 (0.80–1.08) | 0.90 (0.71–1.15) | 0.85 (0.61–1.18) |
| Quintile 4 | 1.02 (0.86–1.22) | 1.01 (0.81–1.26) | 0.84 (0.69–1.03) | 1.04 (0.64–1.69) | 0.97 (0.86–1.10) | 0.92 (0.79–1.08) | 0.91 (0.71–1.17) | 0.79 (0.56–1.11) |
| Quintile 5: high | 0.96 (0.80–1.15) | 1.04 (0.81–1.32) | 0.96 (0.79–1.17) | 1.44 (0.88–2.35) | 0.95 (0.85–1.06) | 0.93 (0.81–1.07) | 0.85 (0.67–1.09) | 0.66 (0.48–0.91) |
| Ptrend | 0.25 | 0.86 | 0.28 | 0.26 | 0.23 | 0.25 | 0.16 | 0.01 |
NOTE: Values in bold represent P < 0.05.
Multinomial logistic regression models for OR and 95% CI for being overweight (BMI 25–29.9) or obese (BMI ≥30) versus normal weight (BMI 18.5–24.9) adjusted for age, marital status, BMI at age 21, education, smoking and cigarette pack years, alcohol intake, hours of moderate and vigorous activity per day, density of red meat, density of processed red meat, density of total vegetables, density of all fruits plus juice, density of all dairy products, total calories, all variables listed in the table, and clustering by block group.
Based on SES composite index of seven indicator variables for Census block groups (Liu education index, proportion with a blue collar job, proportion older than age 16 in the workforce without a job, median household income, percent below 200% of the poverty line, median rent, median house value).
U.S. Census block group-level measure; categories based on distribution for block groups in Los Angeles County.
Ratio of the number of fast-food restaurants to other restaurants.
Businesses/parks within walking distance of residence (1.6 km pedestrian network) or traffic density within 0.5 km radius of residence; quintiles/quartiles based on study participant distribution.
Ratio of the average number of convenience stores, liquor stores, and fast-food restaurants to supermarkets and farmers’ markets.
No business (restaurant or retail food) was excluded in linear trend analysis.
Table 3.
Association between the neighborhood environment and being overweight or obesea among women residing in California by race/ethnicity, Multiethnic Cohort, 1993–1996.
| Neighborhood Attributes | African Americans (n=20,266) | Japanese Americans (n=6,296) | Latinos (n=23,006) | Whites (n=9,115) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Overweight vs. Normal Weight | Obese vs. Normal Weight | Overweight vs. Normal Weight | Obese vs. Normal Weight | Overweight vs. Normal Weight | Obese vs. Normal Weight | Overweight vs. Normal Weight | Obese vs. Normal Weight | |
|
| ||||||||
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Neighborhood SESb,c | ||||||||
| Quintile 5: high | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 4 | 1.07 (0.90–1.27) | 1.36 (1.08–1.73) | 1.23 (1.01–1.50) | 1.27 (0.85–1.90) | 1.01 (0.87–1.16) | 1.01 (0.84–1.21) | 1.30 (1.13–1.49) | 1.48 (1.21–1.80) |
| Quintile 3 | 1.36 (1.14–1.61) | 1.80 (1.42–2.29) | 1.30 (1.05–1.60) | 1.60 (1.04–2.45) | 1.15 (1.00–1.33) | 1.28 (1.07–1.55) | 1.27 (1.08–1.48) | 1.69 (1.36–2.08) |
| Quintile 2 | 1.36 (1.14–1.62) | 2.02 (1.60–2.56) | 1.39 (1.03–1.89) | 1.58 (0.91–2.75) | 1.20 (1.03–1.39) | 1.36 (1.12–1.64) | 1.44 (1.17–1.76) | 1.92 (1.48–2.48) |
| Quintile 1: low | 1.31 (1.08–1.59) | 2.07 (1.62–2.65) | 1.03 (0.60–1.78) | 1.12 (0.49–2.59) | 1.24 (1.04–1.47) | 1.45 (1.17–1.79) | 1.80 (1.32–2.46) | 2.50 (1.73–3.61) |
| Ptrend | <0.01 | <0.01 | 0.08 | 0.11 | <0.01 | <0.01 | <0.01 | <0.01 |
| Population density (persons per km2)c | ||||||||
| Quintile 5: high | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 4 | 0.97 (0.86–1.09) | 0.95 (0.84–1.07) | 0.89 (0.65–1.21) | 0.58 (0.33–1.03) | 0.96 (0.87–1.07) | 1.00 (0.89–1.13) | 0.97 (0.78–1.21) | 0.92 (0.71–1.20) |
| Quintile 3 | 0.97 (0.84–1.12) | 0.95 (0.82–1.11) | 0.84 (0.62–1.16) | 0.55 (0.31–0.97) | 0.93 (0.83–1.05) | 0.95 (0.83–1.09) | 0.87 (0.69–1.09) | 0.83 (0.63–1.10) |
| Quintile 2 | 0.89 (0.76–1.04) | 1.01 (0.86–1.20) | 0.79 (0.57–1.09) | 0.56 (0.31–1.00) | 1.03 (0.91–1.18) | 1.08 (0.93–1.25) | 0.92 (0.73–1.17) | 0.87 (0.65–1.16) |
| Quintile 1: low | 0.95 (0.79–1.14) | 0.92 (0.74–1.13) | 0.78 (0.55–1.11) | 0.49 (0.26–0.92) | 1.06 (0.92–1.22) | 1.11 (0.93–1.31) | 0.81 (0.63–1.03) | 0.76 (0.56–1.03) |
| Ptrend | 0.31 | 0.77 | 0.14 | 0.13 | 0.26 | 0.14 | 0.08 | 0.09 |
| % commute by car/motorcyclec | ||||||||
| Quintile 1: low | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 2 | 0.91 (0.80–1.03) | 0.91 (0.80–1.03) | 1.00 (0.71–1.39) | 1.06 (0.56–2.00) | 1.02 (0.91–1.15) | 0.99 (0.87–1.13) | 1.02 (0.81–1.29) | 1.03 (0.78–1.37) |
| Quintile 3 | 0.86 (0.75–0.98) | 0.85 (0.73–0.98) | 1.05 (0.75–1.47) | 0.64 (0.31–1.31) | 0.97 (0.86–1.10) | 0.90 (0.78–1.04) | 1.18 (0.93–1.49) | 1.16 (0.86–1.56) |
| Quintile 4 | 0.88 (0.76–1.03) | 0.87 (0.75–1.02) | 1.24 (0.88–1.74) | 0.89 (0.43–1.84) | 0.92 (0.81–1.05) | 0.81 (0.69–0.95) | 1.27 (1.00–1.61) | 1.14 (0.84–1.55) |
| Quintile 5: high | 0.89 (0.76–1.04) | 0.95 (0.80–1.12) | 1.32 (0.93–1.87) | 1.00 (0.49–2.03) | 0.91 (0.79–1.05) | 0.80 (0.68–0.94) | 1.38 (1.08–1.76) | 1.31 (0.96–1.80) |
| Ptrend | 0.16 | 0.38 | 0.01 | 0.71 | 0.06 | <0.01 | <0.01 | 0.04 |
| REId,e | ||||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quartile 1: low | 1.17 (0.96–1.42) | 1.08 (0.89–1.31 | 1.37 (1.08–1.74 | 0.78 (0.49–1.25) | 0.90 (0.80–1.01) | 0.90 (0.78–1.03) | 1.01 (0.84–1.21) | 0.98 (0.78–1.24) |
| Quartile 2 | 1.20 (1.02–1.4)2 | 0.99 (0.83–1.18 | 1.27 (1.00–1.62 | 1.12 (0.72–1.74) | 1.02 (0.91–1.14) | 0.95 (0.82–1.08) | 1.12 (0.94–1.34) | 1.02 (0.82–1.27) |
| Quartile 3 | 1.12 (0.95–1.33) | 1.00 (0.84–1.20 | 1.22 (0.94–1.59 | 1.24 (0.75–2.04) | 0.97 (0.86–1.09) | 0.96 (0.83–1.10) | 1.16 (0.95–1.40) | 1.10 (0.87–1.39) |
| Quartile 4: high, <1 | 1.24 (1.05–1.46) | 1.01 (0.85–1.20 | 1.37 (1.03–1.83 | 1.39 (0.81–2.39) | 0.99 (0.87–1.13) | 1.05 (0.90–1.23) | 1.05 (0.87–1.28) | 0.90 (0.70–1.16) |
| Quartile 4: high, ≥1 | 1.12 (0.85–1.48) | 1.13 (0.82–1.55) | 1.19 (0.68–2.08) | 1.52 (0.63–3.66) | 1.09 (0.80–1.47) | 0.93 (0.66–1.30) | 0.92 (0.65–1.30) | 0.89 (0.57–1.36) |
| No restaurant | 1.43 (1.02–2.00) | 1.29 (0.87–1.91) | 1.00 (0.63–1.59) | 0.77 (0.22–2.63) | 0.79 (0.61–1.02) | 0.85 (0.65–1.12) | 1.14 (0.91–1.44) | 0.98 (0.69–1.38) |
| Ptrendg | 0.10 | 0.97 | 0.23 | 0.04 | 0.46 | 0.34 | 0.39 | 0.67 |
| RFEIe,f | ||||||||
| 0 | 0.85 (0.60–1.22) | 0.67 (0.43–1.05) | 1.12 (0.80–1.58) | 0.42 (0.12–1.46) | 1.09 (0.88–1.35) | 1.11 (0.86–1.42) | 0.91 (0.71–1.18) | 0.84 (0.59–1.21) |
| Quartile 1: low | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quartile 2 | 0.95 (0.84–1.08) | 1.05 (0.92–1.19) | 0.91 (0.73–1.13) | 0.85 (0.55–1.32) | 1.08 (0.99–1.19) | 1.08 (0.97–1.19) | 0.98 (0.83–1.16) | 0.94 (0.76–1.16) |
| Quartile 3 | 1.01 (0.89–1.15) | 1.00 (0.87–1.14) | 0.90 (0.73–1.12) | 0.98 (0.64–1.50) | 1.04 (0.94–1.15) | 1.13 (1.00–1.27) | 0.98 (0.84–1.16) | 1.08 (0.88–1.33) |
| Quartile 4: high | 1.09 (0.94–1.25) | 1.06 (0.91–1.23) | 0.94 (0.77–1.17) | 0.79 (0.53–1.19) | 0.97 (0.87–1.08) | 1.07 (0.95–1.22) | 0.83 (0.71–0.98) | 0.76 (0.62–0.95) |
| No retail food | 1.01 (0.70–1.48) | 0.89 (0.57–1.41) | 1.11 (0.67–1.86) | 0.77 (0.25–2.38) | 1.26 (0.91–1.75) | 1.02 (0.67–1.55) | 0.79 (0.60–1.04) | 0.87 (0.60–1.25) |
| Ptrendg | 0.09 | 0.34 | 0.50 | 0.78 | 0.39 | 0.29 | 0.04 | 0.06 |
| Number of businessese | ||||||||
| Quintile 5: high | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 4 | 1.05 (0.91–1.21) | 1.12 (0.97–1.30) | 0.98 (0.81–1.18) | 1.31 (0.90–1.91) | 1.04 (0.93–1.15) | 1.11 (0.98–1.26) | 0.94 (0.79–1.11) | 1.16 (0.93–1.46) |
| Quintile 3 | 1.15 (0.99–1.35) | 1.21 (1.03–1.42) | 1.15 (0.91–1.46) | 1.06 (0.66–1.71) | 1.00 (0.89–1.12) | 1.09 (0.96–1.24) | 1.14 (0.95–1.36) | 1.30 (1.03–1.63) |
| Quintile 2 | 1.20 (1.02–1.40) | 1.27 (1.07–1.50) | 1.20 (0.94–1.53) | 1.09 (0.67–1.78) | 1.11 (0.99–1.24) | 1.25 (1.10–1.43) | 1.02 (0.85–1.24) | 1.32 (1.04–1.67) |
| Quintile 1: low | 1.16 (0.95–1.41) | 1.22 (0.99–1.51) | 1.08 (0.81–1.44) | 0.85 (0.48–1.53) | 1.00 (0.88–1.14) | 1.09 (0.94–1.26) | 1.12 (0.91–1.38) | 1.45 (1.11–1.90) |
| Ptrend | 0.03 | 0.02 | 0.20 | 0.67 | 0.46 | 0.06 | 0.22 | 0.01 |
| Number of parkse | ||||||||
| ≥3 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.10 (0.96–1.24) | 1.00 (0.87–1.15) | 0.83 (0.67–1.02) | 0.47 (0.30–0.72) | 1.08 (0.96–1.21) | 0.95 (0.84–1.09) | 0.90 (0.75–1.08) | 1.10 (0.89–1.37) |
| 1 | 1.02 (0.90–1.14) | 0.96 (0.85–1.09) | 0.96 (0.79–1.15) | 0.82 (0.58–1.17) | 1.03 (0.92–1.15) | 0.96 (0.84–1.08) | 0.78 (0.66–0.91) | 0.95 (0.77–1.17) |
| 0 | 1.03 (0.91–1.17) | 0.94 (0.82–1.08) | 0.90 (0.73–1.11) | 0.78 (0.51–1.18) | 1.07 (0.96–1.21) | 0.93 (0.81–1.06) | 0.84 (0.71–0.99) | 0.90 (0.72–1.12) |
| Ptrend | 0.58 | 0.18 | 0.69 | 0.44 | 0.52 | 0.49 | 0.01 | 0.12 |
| Traffic density (vehicle miles/mile2)e | ||||||||
| Quintile 1: low | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quintile 2 | 0.99 (0.87–1.13) | 0.93 (0.80–1.08) | 1.11 (0.88–1.39) | 0.76 (0.49–1.17) | 0.96 (0.86–1.07) | 1.02 (0.90–1.16) | 0.92 (0.77–1.09) | 1.00 (0.82–1.22) |
| Quintile 3 | 1.06 (0.93–1.21) | 1.05 (0.90–1.22) | 1.14 (0.90–1.45) | 0.74 (0.46–1.20) | 0.92 (0.83–1.03) | 0.99 (0.87–1.13) | 1.02 (0.86–1.22) | 1.02 (0.82–1.26) |
| Quintile 4 | 1.04 (0.90–1.19) | 0.98 (0.84–1.15) | 1.19 (0.94–1.51) | 0.63 (0.39–1.04) | 0.94 (0.84–1.06) | 0.95 (0.82–1.09) | 1.05 (0.87–1.26) | 1.12 (0.88–1.42) |
| Quintile 5: high | 1.03 (0.89–1.20) | 1.05 (0.90–1.24) | 0.99 (0.77–1.26) | 0.76 (0.47–1.22) | 0.94 (0.84–1.05) | 1.00 (0.88–1.14) | 1.05 (0.88–1.26) | 1.07 (0.86–1.34) |
| Ptrend | 0.53 | 0.31 | 0.93 | 0.23 | 0.28 | 0.70 | 0.27 | 0.38 |
NOTE: Values in bold represent P < 0.05
Multinomial logistic regression models for odds ratio (OR) and 95% confidence interval (CI) for being overweight (BMI 25–29.9) or obese (BMI ≥30) versus normal weight (BMI 18.5–24.9) adjusted for age, marital status, BMI at age 21, age at menarche, age at first live birth, number of children, menopausal status, hormone replacement therapy, education, smoking and cigarette pack years, alcohol intake, hours of moderate and vigorous activity per day, density of red meat, density of processed red meat, density of total vegetables, density of all fruits plus juice, density of all dairy products, total calories, all variables listed in the table, and clustering by block group.
Based on SES composite index of seven indicator variables for Census block groups (Liu education index, proportion with a blue collar job, proportion older than age 16 in the workforce without a job, median household income, percent below 200% of the poverty line, median rent, median house value).
U.S. Census block group-level measure; categories based on distribution for block groups in Los Angeles County.
Ratio of the number of fast-food restaurants to other restaurants.
Businesses/parks within walking distance of residence (1.6 km pedestrian network) or traffic density within 0.5 km radius of residence; quintiles/quartiles based on study participant distribution.
Ratio of the average number of convenience stores, liquor stores, and fast-food restaurants to supermarkets and farmers’ markets.
No business (restaurant or retail food) was excluded in linear trend analysis.
RESULTS
The racially/ethnically diverse study population includes 44,631 (43%) Latinos, 31,732 (31%) African Americans, 14,205 (14%) whites, and 12,338 (12%) Japanese Americans. Mean age at baseline was 61 years for men and 60 years for women (Supplemental Table 1). The prevalence of being overweight was 50% in men and 36% in women, while the prevalence of obesity was 19% in men and 28% in women. African American men and women were more likely to be obese, while Japanese American men and women were more likely to be of normal weight. Japanese American men and white women had higher daily moderate/vigorous activity, while Latino women were more likely to have no moderate/vigorous activity.
Distributions of neighborhood obesogenic attributes varied by race/ethnicity (Table 1). Most African American and Latino men and women (55–67%) lived in low-SES (quintiles 1–2) neighborhoods, and approximately half lived in more densely populated (quintiles 4–5) neighborhoods. The majority of Japanese American and white men and women (54–58%) lived in high-SES (quintiles 4–5) neighborhoods or neighborhoods with high proportion of residents commuting to work by car/motorcycle (quintiles 4–5). Compared to other racial/ethnic groups, African American men and women were more likely to live in neighborhoods with a higher REI (quintiles 3–4) or higher street connectivity/walkability (quintiles 4–5); Japanese American men and women were more likely to live in areas with higher number of businesses (quintile 5), ≥ 3 parks, and ≥ 3 recreational facilities.
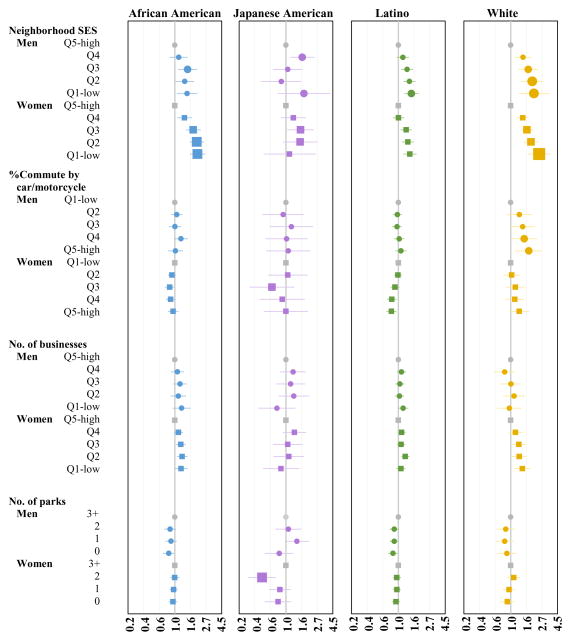
After adjustment for individual- and neighborhood-level factors, African American, Latino, and white men living in low- versus high-SES neighborhoods had higher odds of being overweight or obese (Table 2). The odds of obesity for living in neighborhoods with the lowest versus highest nSES quintile were roughly 50% higher for African American men (OR 1.48, 95% CI 1.07–2.06, p-trend=0.02) and Latino men (OR 1.52, 95% CI 1.21–1.91, p-trend<0.01) and twofold higher (OR 2.11, 95% CI 1.29–3.44; p-trend<0.01) for white men (Figure 1). Significant nSES-overweight associations were seen among white men (p-trend=0.02), and similar patterns were observed among African American (p-trend=0.07) and Latino (p-trend=0.08) men. In contrast, there was no consistent nSES-overweight or -obesity association among Japanese American men, even when using modified Asian-specific BMI categories (data not shown). White men living in neighborhoods with higher proportion of residents commuting by car or motorcycle had higher odds of being overweight (p-trend=0.03) or obese (p-trend=0.01), and those living in neighborhoods with higher traffic density had lower odds of obesity (p-trend=0.01). Latino men living in neighborhoods with fewer nearby walkable destinations (i.e., smaller density of businesses) had higher odds of obesity (p-trend=0.02); yet, this association was limited to U.S.-born Latinos (p-trend<0.01 U.S.-born versus p-trend=0.73 foreign-born; data not shown).
Figure 1.
Odds ratios and 95% confidence intervals for being obese [body mass index (BMI) ≥ 30] compared to normal weight (BMI < 25) among men (circles) and women (squares) in the Multiethnic Cohort residing in California at baseline (1993–1996). Models adjusted for age, marital status, BMI at age 21, smoking and cigarette pack years, alcohol intake, education, moderate and vigorous activity, diet intake (red meat, processed red meat, vegetables and fruits, dairy products, total calories), neighborhood attributes (all variables listed, population density, restaurant environment index, retail food environment index, traffic density), and clustering effect of block group. Neighborhood socioeconomic status (SES) and commute patterns are U.S. Census block group-level measures, with quintiles (Q) based on distribution for block groups in Los Angeles County. Businesses/parks are within walking distance of residence (1.6 km pedestrian network), with categories based on study participant distribution. Symbol size proportional to effect size. Odds ratios on the natural logarithmic scale.
Similar patterns of nSES-overweight or -obesity associations, but with greater magnitude of effects, were observed in women, after adjustment for individual- and neighborhood-level factors (Table 3). African American, Latino, and white women living in low- versus high-SES neighborhoods had statistically significant higher odds of being overweight or obese (p-trends<0.01). The odds of obesity for living in neighborhoods with the lowest versus highest nSES quintile were two-fold higher for African American women (OR 2.07, 95% CI 1.62–2.65), 45% higher (OR 1.45, 95% CI 1.17–1.79) for Latino women, and 2.5-fold higher for white women (OR 2.50, 95% CI 1.73–3.61, Figure 1). Significant nSES-overweight or -obesity associations were seen among Japanese American women. Japanese American women living in less- versus highly-populated neighborhoods had lower odds of obesity [quintile 1 (<1,981 people/km2) vs. 5 (≥6,394 people/km2): OR 0.49, 95% CI 0.26–0.92]. Japanese American and white women living in neighborhoods with higher versus lower level of commuting by car or motorcycle had higher odds of being overweight (p-trends≤0.01), and white women also had higher odds of obesity (p-trend=0.04). Yet, an opposite pattern of association was seen for Latino women, with higher versus lower level of commuting by car or motorcycle associated with decreasing odds of obesity (p-trend≤0.01). African Americans and Japanese American women living in neighborhoods with more fast food restaurants had higher odds of being overweight (quintile 4 with REI<1 vs. no restaurant: OR 1.24, 95% CI 1.05–1.46 among African Americans; OR 1.37, 95% CI 1.03–1.83 among Japanese Americans). Living in neighborhoods with lower density of businesses was associated with increasing odds of being overweight (p-trend=0.03) among African American women and being obese among African American (p-trend=0.02) and white (p-trend=0.01) women. White women living in neighborhoods with no parks compared with ≥3 parks within walking distance of their residence had lower odds of being overweight (OR 0.84, 95% CI 0.71–0.99, p-trend=0.01). Sensitivity analyses using Asian-specific BMI categories showed similar results (data not shown). Additionally, when Latinas were stratified by nativity (U.S.-born and foreign-born); results were similar across these strata (data not shown).
Obesity-related health behaviors (i.e., smoking, alcohol intake, physical activity, dietary intake) and built environment attributes explain, in part, the nSES-obesity association, with a more pronounced association among women than men (Supplemental Table 3). For example, among Latinos and whites, the addition of health behaviors (model 1) to minimally adjusted models (model 0) attenuated ORs (quintile 1 vs. 5) 5–6% among men compared with 19–26% among women (all associations remained significant). Further adjustment for built environment characteristics (Model 2) strengthened associations among men while attenuating associations among women; particularly, associations became significant among African American men (p-trend=0.14 model 1 vs. p-trend=0.02 model 2), while associations among Japanese American women were attenuated toward the null (p-trend<0.01 model 1 vs. p-trend=0.11 model 2).
DISCUSSION
By leveraging existing geospatial data, we efficiently appended neighborhood obesogenic environmental factors to the Multiethnic Cohort, thereby creating a multilevel resource to facilitate prospective studies of the impact of neighborhood environments on cancer health disparities. We characterized the neighborhood obesogenic environment for California MEC participants and examined associations between neighborhood attributes and being overweight or obese. This study demonstrates the potential utility of examining the independent influence of the neighborhood environment for studies of obesity-related cancers and provides a framework for examining neighborhood attributes within a large, epidemiologic cohort study. Overall, the strongest association we observed was between nSES and overweight or obesity, independent of individual-level education, diet, physical activity and other individual- and neighborhood-level factors. In sex and racial/ethnic specific analysis, African American, Latino, and white men and women living in low- versus high-SES neighborhoods had statistically significant higher odds of obesity (p-trends≤0.02 for all; OR ranging from 1.45–2.50 for the lowest vs. highest nSES quintile), with a larger magnitude of effect among women than men. Furthermore, we identified independent associations between obesity and the following neighborhood attributes: higher population density (among Japanese American women), lower number of businesses (among African American and white women), and lower traffic density (among white men). To our knowledge, this is the first study to simultaneously assess the potential obesogenic role of a comprehensive suite of neighborhood environment attributes across multiple racial/ethnic groups.
Our observations of higher odds of being overweight or obese for those living in low-SES neighborhoods, independent of individual-level risk factors, are consistent with other cross-sectional studies (26, 27, 41–44, 62–64). Yet, only a few studies have specifically examined racial/ethnic differences (27, 41–44). We observed the largest effect estimates between nSES (quintile 5 vs. 1) and obesity among white women (OR 2.5), followed by white men (OR 2.1) and African American women (OR 2.1), and then Latino men (OR 1.5) and women (OR 1.4) and African American men (OR 1.5). The larger magnitude of effect for the nSES-obesity association among whites compared with African American women (p-Mantel-Haenszel<0.01) have also been suggested by other studies (42–44).
The larger estimated effect size between nSES and obesity among women in comparison to men, independent of individual-level SES, is consistent with other studies (41–43, 62, 65, 66). In particular, living in low-SES neighborhoods was associated with greater odds of obesity in African American and white women compared with African American and white men (p-Mantel-Haenszel<0.01). Other studies observed associations between low-SES neighborhoods and increased BMI (23, 41–43, 62, 65, 66), waist circumference (65), or weight change (62) in women, yet there were small or null effects in men. Studies have reported these differential associations after adjustment for individual-level factors beyond SES, including health behaviors (23, 41, 62, 65), chronic and acute stress (41), positive social support (41), physical and mental health status (65), and neighborhood factors, including neighborhood-level racial/ethnic composition (43, 66), walkability (66), and perceived physical and social disorder (65).
In women, the stronger nSES influence on being overweight or obese could be related to more time spent in residential neighborhoods due to time constraints and smaller spheres of daily movement, resulting from greater residence-related duties of housework and childcare (67) and lower participation in the work force (68) in comparison to men. This notion is supported by a lower proportion of women compared with men in the MEC reporting ever working (68% versus 83%, respectively). Subsequently, women may be more reliant on the physical and social contextual features of their residential neighborhoods and, thus, impacted by obesogenic attributes to a greater degree than men as supported by the attenuation of associations with adjustment for built environment characteristics among women but not men in the present study. We also observed some evidence of stronger independent associations among women than men between being overweight or obese and high population density, low density of businesses, and high density of fast-food restaurants. Similarly, middle-late aged women living in neighborhoods with better walkability had lower BMI, with weaker associations observed in men, in the Multi-Ethnic Study of Atherosclerosis (45) and in the Health and Retirement Study (69). Women compared with men are more susceptible to physiological stress, especially those without social support (70), and living in more socially cohesive neighborhoods has been shown to be associated with lower overweight/obesity after adjustment for individual-level SES and neighborhood characteristics (e.g., walkability, neighborhood safety, material deprivation) (71). It could be hypothesized that the neighborhood associations we identified may be related to factors such as lack of social cohesion/support that may have a greater impact on eating behaviors and being overweight/obese for women (72) in comparison with men (73).
Opposite patterns of associations in whites compared with other racial/ethnic groups were noted for commute patterns and the number of parks. Living in neighborhoods with a higher proportion of residents commuting by car/motorcycle was associated with obesity in white men and women, but was associated with a lower odds of obesity in Latino women. However, individual-level commuting habits were not accounted for in this study and may explain this differential association by race/ethnicity. Contrary to the theory that proximity to parks contributes to reducing obesity, we identified living in neighborhoods with no parks to be associated with a lower odds of being overweight among white women; however, this may be a spurious finding as a consistent association between parks and obesity was not observed among white women. Furthermore, inconsistent and mixed associations have been reported in a review of access to parks/green spaces and obesity (74). It is plausible that other metrics unavailable to our study, such as park characteristics (75), perceived park quality (76), size of parks (39), and access to walking trails may be more important determinants for obesity, and/or parks may promote physical activity only among certain populations (e.g., children).
It is widely accepted that environmental context affects health outcomes, following several conceptual frameworks (77) that have been extended to obesity (78) and cancer (2). The contextual mechanisms that influence obesity likely represent a complex interaction between social and built environment features, health-related behaviors, and individual characteristics (biological response, genetic susceptibility, sex, race/ethnicity) (78, 79). In addition to availability of healthy food, walkability, or recreational environments, living in low-SES neighborhoods may promote chronic activation of physiological stress response (80–83) that, in turn, contributes to neuroendocrine-autonomic nervous system response leading to the accumulation of excess body fat (84).
There are several strengths of this study. Our large, population-based sample of racial/ethnic minorities allows for a well-powered study of differences in associations by sex and race/ethnicity. The extensive questionnaire data and substantial variation in the distribution of dietary intake and lifestyle factors provide a broad representation of individual-level risk factors. California MEC participants resided primarily in Los Angeles County and their residential neighborhoods represent diverse geographic areas, providing a wide spectrum of variation in nSES and built-environment attributes.
Several limitations should be considered in relation to characterizing the neighborhood obesogenic environment. The use of aggregated census data, census boundaries, pedestrian networks, or buffers may lead to misclassification of neighborhood exposures for individuals (85) and may not represent the entire obesogenic experience as our study was unable to account for non-residential environments, such as the workplace that may influence obesity (86). Other contextual features unavailable in the present study are important to consider in relation to obesity risk, such as social and physical disorder (87), collective efficacy (88), or physiological distress (80, 82). Exploring neighborhood- and individual-level characteristics related to acculturation in future studies may help to explain some of the differential associations by specific racial/ethnic groups (e.g., population density association among Japanese American women)(89). Detailed information on occupation (e.g., working at home) were not available in the MEC and future studies are needed to examine potential modification by work status. Lastly, we recognize that some of our findings may be due to chance. Yet, our consistent findings of nSES-obesity associations across multiple sex-racial/ethnic groups indicate a true association.
Our study provides further evidence of the importance of neighborhood contextual attributes on health and obesity-related disparities, especially among disadvantaged populations (i.e., racial/ethnic minorities, low-income populations, and women) (90–92). Current public health strategies targeting the obesity epidemic should adopt a multi-level and intersectional approach, addressing racial/ethnic- and sex-specific contextual factors that enable healthy behaviors in neighborhoods with limited resources. In characterizing the obesogenic environment of California MEC participants, we have demonstrated a valuable approach for accounting for neighborhood context within a large cohort study, thereby enhancing the value and impact of future studies of obesity-related cancers.
Supplementary Material
Acknowledgments
Financial Support: This work was supported by the National Cancer Institute grant R01 CA154644. The Multiethnic Cohort Study was supported by the National Cancer Institute grants R01 CA54281, R37CA54281, and UM1 CA164973 to L. Le Marchand, L.R. Wilkens, and C.A. Haiman. The development of the California Neighborhoods Data System was supported by the National Cancer Institute grant (R03 CA117324) and by a Rapid Response Surveillance Study from the SEER program under a modification to contract N01-PC-35136.
Footnotes
Conflicts of Interest: None
References
- 1.Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med. 1999;29:563–70. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 2.Gomez SL, Shariff-Marco S, DeRouen M, et al. The impact of neighborhood social and built environment factors across the cancer continuum: Current research, methodological considerations, and future directions. Cancer. 2015;121:2314–30. doi: 10.1002/cncr.29345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Research Council (US) Panel on Race, Ethnicity, and Health in Later Life. What Makes a Place Healthy? Neighborhood Influences on Racial/Ethnic Disparities in Health over the Life Course. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington (DC): National Academies Press (US); 2004. [PubMed] [Google Scholar]
- 4.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55:111–22. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–45. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 6.Conroy SM, Clarke C, Yang J, et al. Contextual impact of neighborhood obesogenic factors on postmenopausal breast cancer: The Multiethnic Cohort. Cancer Epidemiol Biomarkers Prev. 2017;26(4):480–489. doi: 10.1158/1055-9965.EPI-16-0941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conroy SM, Shariff-Marco S, Koo J, et al. Racial/Ethnic Differences in the Impact of Neighborhood Social and Built Environment on Breast Cancer Risk: The Neighborhoods and Breast Cancer Study. Cancer Epidemiol Biomarkers Prev. 2017;26(4):541–552. doi: 10.1158/1055-9965.EPI-16-0935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Webster TF, Hoffman K, Weinberg J, Vieira V, Aschengrau A. Community- and individual-level socioeconomic status and breast cancer risk: multilevel modeling on Cape Cod, Massachusetts. Environ Health Perspect. 2008;116:1125–9. doi: 10.1289/ehp.10818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robert SA, Strombom I, Trentham-Dietz A, et al. Socioeconomic risk factors for breast cancer: distinguishing individual- and community-level effects. Epidemiology. 2004;15:442–50. doi: 10.1097/01.ede.0000129512.61698.03. [DOI] [PubMed] [Google Scholar]
- 10.Doubeni CA, Laiyemo AO, Major JM, et al. Socioeconomic status and the risk of colorectal cancer: an analysis of more than a half million adults in the National Institutes of Health-AARP Diet and Health Study. Cancer. 2012;118:3636–44. doi: 10.1002/cncr.26677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim D, Masyn KE, Kawachi I, Laden F, Colditz GA. Neighborhood socioeconomic status and behavioral pathways to risks of colon and rectal cancer in women. Cancer. 2010;116:4187–96. doi: 10.1002/cncr.25195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng I, Shariff-Marco S, Koo J, et al. Contribution of the neighborhood environment and obesity to breast cancer survival: the California Breast Cancer Survivorship Consortium. Cancer Epidemiol Biomarkers Prev. 2015;24:1282–90. doi: 10.1158/1055-9965.EPI-15-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shariff-Marco S, Yang J, John EM, et al. Impact of neighborhood and individual socioeconomic status on survival after breast cancer varies by race/ethnicity: the Neighborhood and Breast Cancer Study. Cancer Epidemiol Biomarkers Prev. 2014;23:793–811. doi: 10.1158/1055-9965.EPI-13-0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shariff-Marco S, Gomez SL, Sangaramoorthy M, et al. Impact of neighborhoods and body size on survival after breast cancer diagnosis. Health Place. 2015;36:162–72. doi: 10.1016/j.healthplace.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keegan TH, Shariff-Marco S, Sangaramoorthy M, et al. Neighborhood influences on recreational physical activity and survival after breast cancer. Cancer Causes Control. 2014;25:1295–308. doi: 10.1007/s10552-014-0431-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lauby-Secretan B, Scoccianti C, Loomis D, et al. Body Fatness and Cancer--Viewpoint of the IARC Working Group. N Engl J Med. 2016;375:794–8. doi: 10.1056/NEJMsr1606602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demark-Wahnefried W, Platz EA, Ligibel JA, et al. The role of obesity in cancer survival and recurrence. Cancer Epidemiol Biomarkers Prev. 2012;21:1244–59. doi: 10.1158/1055-9965.EPI-12-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315:477–80. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan LK, Sobush K, Keener D, et al. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58:1–26. [PubMed] [Google Scholar]
- 20.Lynch SM, Rebbeck TR. Bridging the gap between biologic, individual, and macroenvironmental factors in cancer: a multilevel approach. Cancer Epidemiol Biomarkers Prev. 2013;22:485–95. doi: 10.1158/1055-9965.EPI-13-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackenbach JD, Rutter H, Compernolle S, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health. 2014;14:233. doi: 10.1186/1471-2458-14-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12:217–30. doi: 10.1111/j.1467-789X.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- 23.Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16:175–90. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 24.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29:129–43. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 25.Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes--a randomized social experiment. N Engl J Med. 2011;365:1509–19. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corriere MD, Yao W, Xue QL, et al. The association of neighborhood characteristics with obesity and metabolic conditions in older women. J Nutr Health Aging. 2014;18:792–8. doi: 10.1007/s12603-014-0477-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeigler-Johnson C, Weber A, Glanz K, Spangler E, Rebbeck TR. Gender- and ethnic-specific associations with obesity: individual and neighborhood-level factors. J Natl Med Assoc. 2013;105:173–82. doi: 10.1016/s0027-9684(15)30107-3. [DOI] [PubMed] [Google Scholar]
- 28.Polsky JY, Moineddin R, Dunn JR, Glazier RH, Booth GL. Absolute and relative densities of fast-food versus other restaurants in relation to weight status: Does restaurant mix matter? Prev Med. 2016;82:28–34. doi: 10.1016/j.ypmed.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 29.Pruchno R, Wilson-Genderson M, Gupta AK. Neighborhood food environment and obesity in community-dwelling older adults: individual and neighborhood effects. Am J Public Health. 2014;104:924–9. doi: 10.2105/AJPH.2013.301788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones-Smith JC, Karter AJ, Warton EM, et al. Obesity and the food environment: income and ethnicity differences among people with diabetes: the Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2013;36:2697–705. doi: 10.2337/dc12-2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Auchincloss AH, Mujahid MS, Shen M, Michos ED, Whitt-Glover MC, Diez Roux AV. Neighborhood health-promoting resources and obesity risk (the Multi-ethnic Study of Atherosclerosis) Obesity (Silver Spring) 2013;21:621–8. doi: 10.1038/oby.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the Atherosclerosis Risk in Communities Study. Am J Prev Med. 2006;30:333–9. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Creatore MI, Glazier RH, Moineddin R, et al. Association of Neighborhood Walkability With Change in Overweight, Obesity, and Diabetes. JAMA. 2016;315:2211–20. doi: 10.1001/jama.2016.5898. [DOI] [PubMed] [Google Scholar]
- 34.Muller-Riemenschneider F, Pereira G, Villanueva K, et al. Neighborhood walkability and cardiometabolic risk factors in Australian adults: an observational study. BMC Public Health. 2013;13:755. doi: 10.1186/1471-2458-13-755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang X, Holt JB, Lu H, et al. Neighborhood commuting environment and obesity in the United States: an urban-rural stratified multilevel analysis. Prev Med. 2014;59:31–6. doi: 10.1016/j.ypmed.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 36.Shariff-Marco S, Von Behren J, Reynolds P, et al. Impact of Social and Built Environment Factors on Body Size among Breast Cancer Survivors: The Pathways Study. Cancer Epidemiol Biomarkers Prev. 2017 doi: 10.1158/1055-9965.EPI-16-0932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Powell-Wiley TM, Ayers CR, de Lemos JA, et al. Relationship between perceptions about neighborhood environment and prevalent obesity: data from the Dallas Heart Study. Obesity (Silver Spring) 2013;21:E14–21. doi: 10.1002/oby.20012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Putrik P, van Amelsvoort L, De Vries NK, et al. Neighborhood Environment is Associated with Overweight and Obesity, Particularly in Older Residents: Results from Cross-Sectional Study in Dutch Municipality. J Urban Health. 2015;92:1038–51. doi: 10.1007/s11524-015-9991-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rundle A, Quinn J, Lovasi G, et al. Associations between body mass index and park proximity, size, cleanliness, and recreational facilities. Am J Health Promot. 2013;27:262–9. doi: 10.4278/ajhp.110809-QUAN-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mobley LR, Root ED, Finkelstein EA, Khavjou O, Farris RP, Will JC. Environment, obesity, and cardiovascular disease risk in low-income women. Am J Prev Med. 2006;30:327–32. doi: 10.1016/j.amepre.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 41.Robert SA, Reither EN. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Soc Sci Med. 2004;59:2421–34. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 42.Mujahid MS, Diez Roux AV, Borrell LN, Nieto FJ. Cross-sectional and longitudinal associations of BMI with socioeconomic characteristics. Obes Res. 2005;13:1412–21. doi: 10.1038/oby.2005.171. [DOI] [PubMed] [Google Scholar]
- 43.Do DP, Dubowitz T, Bird CE, Lurie N, Escarce JJ, Finch BK. Neighborhood context and ethnicity differences in body mass index: a multilevel analysis using the NHANES III survey (1988–1994) Econ Hum Biol. 2007;5:179–203. doi: 10.1016/j.ehb.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scott MM, Dubowitz T, Cohen DA. Regional differences in walking frequency and BMI: what role does the built environment play for Blacks and Whites? Health Place. 2009;15:882–7. doi: 10.1016/j.healthplace.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mujahid MS, Diez Roux AV, Shen M, et al. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:1349–57. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 46.Kolonel LN, Altshuler D, Henderson BE. The multiethnic cohort study: exploring genes, lifestyle and cancer risk. Nat Rev Cancer. 2004;4:519–27. doi: 10.1038/nrc1389. [DOI] [PubMed] [Google Scholar]
- 47.Kolonel LN, Henderson BE, Hankin JH, et al. A multiethnic cohort in Hawaii and Los Angeles: baseline characteristics. Am J Epidemiol. 2000;151:346–57. doi: 10.1093/oxfordjournals.aje.a010213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gomez SL, Glaser SL, McClure LA, et al. The California Neighborhoods Data System: a new resource for examining the impact of neighborhood characteristics on cancer incidence and outcomes in populations. Cancer Causes Control. 2011;22:631–47. doi: 10.1007/s10552-011-9736-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12:703–11. doi: 10.1023/a:1011240019516. [DOI] [PubMed] [Google Scholar]
- 50.Babey SH, Diamant AL, Hastert TA, Harvey S, Goldstein H, Fluornoy R, et al. Designed for disease: the link between local food environments and obesity and diabetes. California Center for Public Health Advocacy, Policy-Link, and the UCLA Center for Health Policy Research; 2008. [Google Scholar]
- 51.Walls & Associates. National Establishment Time-Series (NETS) Database, 2009. Oakland, CA: Walls & Associates; 2008. [Google Scholar]
- 52.NavTeq. NAVSTREETS Street Data Reference Manual v3.7. 1. Chicago, IL: NavTeq; 2010. [Google Scholar]
- 53.California Department of Food and Agriculture. California certified farmers’ market database. Sacramento, CA: California Department of Food and Agriculture; 2010. [Google Scholar]
- 54.Berrigan D, Pickle LW, Dill J. Associations between street connectivity and active transportation. Int J Health Geogr. 2010;9:20. doi: 10.1186/1476-072X-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.California Department of Transportation. Highway Performance and Monitoring System. 2004. [Google Scholar]
- 56.Gunier RB, Hertz A, Von Behren J, Reynolds P. Traffic density in California: socioeconomic and ethnic differences among potentially exposed children. J Expo Anal Environ Epidemiol. 2003;13:240–6. doi: 10.1038/sj.jea.7500276. [DOI] [PubMed] [Google Scholar]
- 57.Wilkens LR, Murphy SP, Jardack P, White KK, Kolonel LN, Arab L. Validation of a physical activity questionnaire against the doubly-labeled water standard among a multiethnic population. FASEB J. 2011;25:978–9. [Google Scholar]
- 58.Stram DO, Hankin JH, Wilkens LR, et al. Calibration of the dietary questionnaire for a multiethnic cohort in Hawaii and Los Angeles. Am J Epidemiol. 2000;151:358–70. doi: 10.1093/oxfordjournals.aje.a010214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Keegan TH, Hurley S, Goldberg D, et al. The association between neighborhood characteristics and body size and physical activity in the California teachers study cohort. Am J Public Health. 2012;102:689–97. doi: 10.2105/AJPH.2011.300150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hsu WC, Araneta MR, Kanaya AM, Chiang JL, Fujimoto W. BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care. 2015;38:150–8. doi: 10.2337/dc14-2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 62.Stafford M, Brunner EJ, Head J, Ross NA. Deprivation and the development of obesity a multilevel, longitudinal study in England. Am J Prev Med. 2010;39:130–9. doi: 10.1016/j.amepre.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 63.Wang MC, Kim S, Gonzalez AA, MacLeod KE, Winkleby MA. Socioeconomic and food-related physical characteristics of the neighbourhood environment are associated with body mass index. J Epidemiol Community Health. 2007;61:491–8. doi: 10.1136/jech.2006.051680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wen M, Kowaleski-Jones L. The built environment and risk of obesity in the United States: racial-ethnic disparities. Health Place. 2012;18:1314–22. doi: 10.1016/j.healthplace.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bell JA, Hamer M, Shankar A. Gender-specific associations of objective and perceived neighborhood characteristics with body mass index and waist circumference among older adults in the English longitudinal study of ageing. Am J Public Health. 2014;104:1279–86. doi: 10.2105/AJPH.2014.301947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rundle A, Field S, Park Y, Freeman L, Weiss CC, Neckerman K. Personal and neighborhood socioeconomic status and indices of neighborhood walk-ability predict body mass index in New York City. Soc Sci Med. 2008;67:1951–8. doi: 10.1016/j.socscimed.2008.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schwanen T, Kwan MP, Ren F. How fixed is fixed? Gendered rigidity of space–time constraints and geographies of everyday activities. Geoforum. 2008;39:2109–21. [Google Scholar]
- 68.Robert SA. Socioeconomic position and health: The independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 69.Grafova IB, Freedman VA, Kumar R, Rogowski J. Neighborhoods and obesity in later life. Am J Public Health. 2008;98:2065–71. doi: 10.2105/AJPH.2007.127712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McLeod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesirable life events. J Health Soc Behav. 1990;31:162–72. [PubMed] [Google Scholar]
- 71.Guilcher SJ, Kaufman-Shriqui V, Hwang J, et al. The association between social cohesion in the neighborhood and body mass index (BMI): An examination of gendered differences among urban-dwelling Canadians. Prev Med. 2017;99:293–8. doi: 10.1016/j.ypmed.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 72.Pham do Q, Ommerborn MJ, Hickson DA, Taylor HA, Clark CR. Neighborhood safety and adipose tissue distribution in African Americans: the Jackson Heart Study. PLoS One. 2014;9:e105251. doi: 10.1371/journal.pone.0105251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barrington WE, Stafford M, Hamer M, Beresford SA, Koepsell T, Steptoe A. Neighborhood socioeconomic deprivation, perceived neighborhood factors, and cortisol responses to induced stress among healthy adults. Health Place. 2014;27:120–6. doi: 10.1016/j.healthplace.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lachowycz K, Jones AP. Greenspace and obesity: a systematic review of the evidence. Obes Rev. 2011;12:e183–9. doi: 10.1111/j.1467-789X.2010.00827.x. [DOI] [PubMed] [Google Scholar]
- 75.Stark JH, Neckerman K, Lovasi GS, et al. The impact of neighborhood park access and quality on body mass index among adults in New York City. Prev Med. 2014;64:63–8. doi: 10.1016/j.ypmed.2014.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bai H, Wilhelm Stanis SA, Kaczynski AT, Besenyi GM. Perceptions of neighborhood park quality: associations with physical activity and body mass index. Ann Behav Med. 2013;45(Suppl 1):S39–48. doi: 10.1007/s12160-012-9448-4. [DOI] [PubMed] [Google Scholar]
- 77.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30:668–77. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- 78.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62:1650–71. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 79.Institute of Medicine (US) Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. In: Hernandez LM, Blazer DG, editors. Institute of Medicine (US) Committee on Assessing Interactions Among Social, Behavioral, and Genetic Factors in Health. Washington (DC): National Academies Press (US); 2006. [PubMed] [Google Scholar]
- 80.Burdette AM, Hill TD. An examination of processes linking perceived neighborhood disorder and obesity. Soc Sci Med. 2008;67:38–46. doi: 10.1016/j.socscimed.2008.03.029. [DOI] [PubMed] [Google Scholar]
- 81.Matthews SA, Yang TC. Exploring the role of the built and social neighborhood environment in moderating stress and health. Ann Behav Med. 2010;39:170–83. doi: 10.1007/s12160-010-9175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Glass TA, Rasmussen MD, Schwartz BS. Neighborhoods and obesity in older adults: the Baltimore Memory Study. Am J Prev Med. 2006;31:455–63. doi: 10.1016/j.amepre.2006.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Taylor SE, Repetti RL, Seeman T. Health psychology: what is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–47. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- 84.Kyrou I, Chrousos GP, Tsigos C. Stress, visceral obesity, and metabolic complications. Ann N Y Acad Sci. 2006;1083:77–110. doi: 10.1196/annals.1367.008. [DOI] [PubMed] [Google Scholar]
- 85.Kwan MP. From place-based to people-based exposure measures. Soc Sci Med. 2009;69:1311–3. doi: 10.1016/j.socscimed.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 86.Barrington WE, Beresford SA, Koepsell TD, Duncan GE, Moudon AV. Worksite neighborhood and obesogenic behaviors: findings among employees in the Promoting Activity and Changes in Eating (PACE) trial. Am J Prev Med. 2015;48:31–41. doi: 10.1016/j.amepre.2014.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chang VW, Hillier AE, Mehta NK. Neighborhood Racial Isolation, Disorder and Obesity. Soc Forces. 2009;87:2063–92. doi: 10.1353/sof.0.0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cohen DA, Finch BK, Bower A, Sastry N. Collective efficacy and obesity: the potential influence of social factors on health. Soc Sci Med. 2006;62:769–78. doi: 10.1016/j.socscimed.2005.06.033. [DOI] [PubMed] [Google Scholar]
- 89.Park Y, Neckerman KM, Quinn J, Weiss C, Rundle A. Place of birth, duration of residence, neighborhood immigrant composition and body mass index in New York City. Int J Behav Nutr Phys Act. 2008;5:19. doi: 10.1186/1479-5868-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Do DP, Finch BK, Basurto-Davila R, Bird C, Escarce J, Lurie N. Does place explain racial health disparities? Quantifying the contribution of residential context to the Black/white health gap in the United States. Soc Sci Med. 2008;67:1258–68. doi: 10.1016/j.socscimed.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Braveman P. A health disparities perspective on obesity research. Prev Chronic Dis. 2009;6:A91. [PMC free article] [PubMed] [Google Scholar]
- 92.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.