Abstract
Study objectives:
To examine whether change in job strain leads to change in insomnia symptoms.
Methods:
Among 24873 adults (82% women, mean age 44 years) who participated in a minimum of three consecutive study waves (2000–2012), job strain was assessed at the first and second wave and insomnia symptoms at all three waves. We analyzed observational data as a “pseudo-trial” including participants with no job strain in the first wave and no insomnia symptoms in the first and second wave (n = 7354) to examine whether the onset of job strain between the first and second waves predicted the onset of insomnia symptoms in the third wave. We used a corresponding approach, including those with job strain in the first wave and insomnia symptoms in the first and second wave (n = 2332), to examine whether the disappearance of job strain between the first two waves predicted remission of insomnia symptoms in the third wave.
Results:
The onset of job strain predicted the onset of subsequent insomnia symptoms after adjustment for sex, age, marital status, education, smoking, physical activity, alcohol consumption, body mass index, and comorbidities (odds ratio compared to no onset of job strain 1.32, 95% CI 1.16–1.51). The disappearance of job strain was associated with lower odds of repeated insomnia symptoms (odds ratio compared to no disappearance of job strain 0.78, 95% CI 0.65–0.94). Further adjustment for shift work or sleep apnea did not change these associations.
Conclusions:
These results suggest that job strain is a modifiable risk factor for insomnia symptoms.
Keywords: cohort study, epidemiology, insomnia symptoms, sleep, job strain.
Statement of Significance
When analyzing observational dataas non-randomized trials, we found evidence that the onset of job strain in individuals free of insomnia tends to increase the risk of a subsequent onset of insomnia symptoms. Among those with insomnia symptoms, the disappearance of job strain was associated with remission of insomnia symptoms at follow-up. These findings support the hypothesis that exposure to job strain (ie, high job demands and low job control) affects sleep quality. Workplace modifications aiming to reduce job strain might have the potential to simultaneously reduce insomnia symptoms among employees. However, this needs to be examined further in future intervention studies.
INTRODUCTION
A two-dimensional job strain model was originally described by Karasek1 and further developed in collaboration between Karasek and Theorell.2 The model suggests that work-related psychosocial stress is likely to arise from a combination of high psychological demands (eg, an employee having to work intensively to a tight deadline) and low control (or low decision latitude, eg, not having a say in what tasks are to be done and how).3 This two-dimensional model has been widely used in research that focuses on psychosocial factors at work.4–6 Some studies suggest that an additional third component, low social support, may further increase the disease risk, but this component refers to the quality of interpersonal relations at the workplace rather than the characteristics of the job.1,7–9
Insomnia symptoms tend to increase with age10 and work-life stress has been linked with decreased sleep.11 Disturbed sleep is further linked to increased work disability12–15 and occupational accidents16 as well as ill-health.17 However, relatively little is known about the natural course of insomnia symptoms during work life, particularly about how changes in psychosocial risk factors such as job strain and its components, high job demands, and low job control, contribute to the onset or remission of insomnia symptoms.
There are some limitations to the longitudinal evidence on the association between psychosocial work factors and insomnia symptoms.18–22 Most of these studies have relied on data from two measurement points only while using several measurements would enable the study of temporal relationships and provide a more comprehensive understanding of the direction of the association. One study demonstrated an association between the transition from a non-high-strain job to a high-strain job and an increase in sleep-related complaints, although no association was observed between transitions from a high-strain to a non-high-strain job.18 A limitation of this study was that the temporal relationship between job strain and insomnia symptoms could not be established. Another longitudinal study found that, high job demands predicted subsequent disturbed sleep.22 However, we are not aware of any studies that have examined whether the disappearance of job strain could improve sleep quality.
To address some of these limitations, we sought to examine (1) whether the onset of job strain is associated with a subsequent onset of insomnia symptoms among those free of insomnia symptoms at baseline, and (2) whether the disappearance of job strain is associated with the remission of insomnia symptoms at follow-up among those with insomnia symptoms at baseline. To strengthen the assessment of the temporal order between the changes in job strain and insomnia symptoms, we analyzed observational data as non-randomized trials, using strict a priori inclusion and exclusion criteria.23
METHODS
Study Population
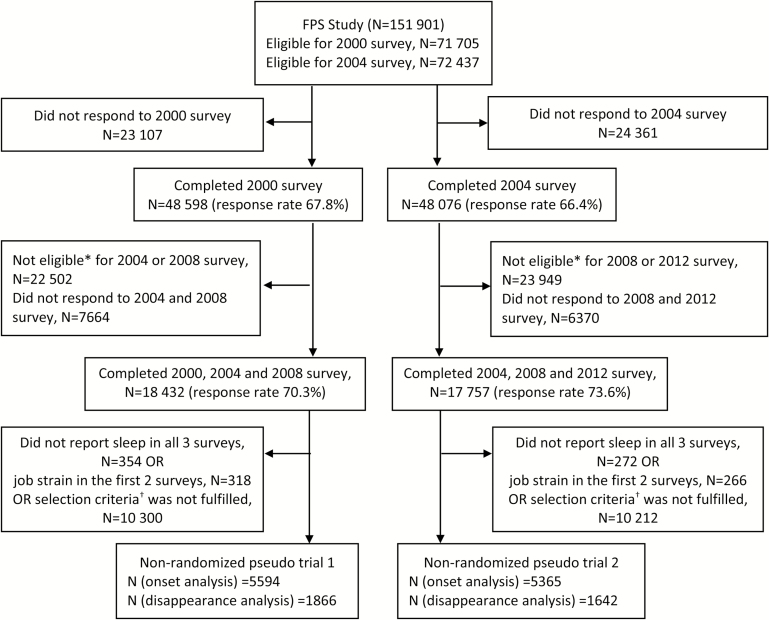
The study population consisted of participants of the Finnish Public Sector (FPS) study, a prospective cohort study of employees from ten towns and six hospital districts in Finland. The original cohort included all participants who had worked in the participating organizations for a minimum of 6 months between 1991 and 2005. The cohort was refreshed to include all participants who were employed by the participating organizations at the time of the study surveys (study waves) conducted at 4-year intervals in 2000 (n = 48 598, response rate 68%), 2004 (n = 48 076, response rate 66%), 2008 (n = 52 891, response rate 71%), and 2012 (n = 53 133, response rate 69%).24 The selection of the participants for the analysis samples of this study is presented in a flow chart (Figure 1). The participants were from a wide range of occupations and varied from semi-skilled cleaners to administrative personnel and physicians. The ethics committees of the Finnish Institute of Occupational Health and the Hospital District of Helsinki and Uusimaa approved the FPS study.
Figure 1.
Selection of study sample for non-randomized pseudo-trials. *not employed by a participating organization. †Selection criteria for the onset analysis: no job strain in first wave and no insomnia symptoms in first two waves; for the disappearance analysis: job strain in first wave and insomnia symptoms in first two waves.
Study Setting
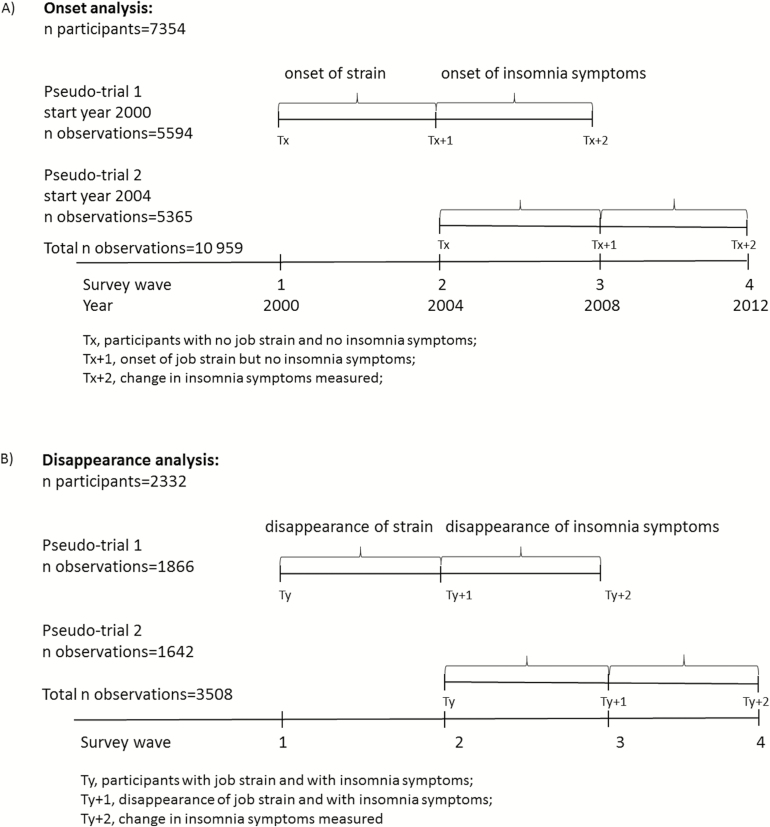
We treated longitudinal observational data as non-randomized “pseudo-trials,” which mimic the selection process of clinical trials (Figure 2). To temporally distinguish the onset/remission of insomnia symptoms from changes in job exposures, our study required participation in three consecutive waves. This setting is in line with procedures used in previous studies23,25 and it enabled us to examine the direction of the associations in observational data by taking into account the temporal order of the onset/disappearance of job strain and the subsequent changes in insomnia symptoms.
Figure 2.
Setting of pseudo-trials used in (A) onset analysis and (B) disappearance analysis.
The four study waves enabled us to create two nested cohorts (“pseudo-trials”) with the baseline in either 2000 (n = 18 432) or in 2004 (n = 17 757). Of the 24 287 participants with three consecutive measurements in either cohort, 11 902 had measurements from all four waves and thus contributed to two cohorts resulting in a total of 36 189 person-observations. For the analyses of the onset of job strain, we used information from participants who (1) reported no job strain (or its components high job demands and low job control) and no insomnia symptoms in the first wave, Tx, (2) either reported or did not report job strain, or its components, but in both cases still had no insomnia symptoms in the second wave, Tx+1, and (3) had information on insomnia symptoms from the third wave, Tx+2 (Figure 2A). In total, 7354 participants with three repeated measures were included in the two nested cohorts, providing 10 959 observations for the analysis. For the analyses of the disappearance of job strain, we included participants who (1) reported job strain (or its components high job demands and low job control) and insomnia symptoms at Ty, (2) either reported or did not report job strain, but in both cases still had insomnia symptoms at Ty+1, and (3) had information about insomnia symptoms at Ty+2 (Figure 2B). In total, 2332 participants with three repeated measures were included in the two nested cohorts providing 3508 observations for the analysis.
Insomnia Symptoms
Information on insomnia symptoms was based on self-reported symptoms during the 4 weeks preceding each study wave. Insomnia symptoms were measured using the Jenkins Sleep Problem Scale with questions on difficulty falling asleep, difficulty maintaining sleep during the night, awakening too early in the morning, and non restorative sleep.26 Participants reported on the frequency (never, once/month, once/week, 2–4 times/wk, 5–6 times/wk, and nearly every night) of each insomnia symptom that we used to create a variable for “any insomnia symptom” based on the most frequent insomnia symptom reported by the participant. This variable was dichotomized using the response category of 2–4 times/wk as the cut point,27 which in the text is referred to as symptoms ≥2 versus <2 times/wk. This roughly corresponds to the cut-off point of 3 times/wk, which is used as one diagnostic criterion for an insomnia disorder in the DSM-5.28
Job Strain and its Components
Job strain and its components were ascertained using questions from the Job Content Questionnaire (JCQ)3 and measured in each study wave. The FPS study surveys included job control and job demands scales from the shorter version of the JCQ, thus information was available for only a selected set of questions.4 “Job demand” was based on three statements: “I have to work very hard,” “I am expected to perform excessive amounts of work,” and “I do not have enough time to get my job done.” “Job control” was based on nine statements about decision freedom and learning at work such as: “I can make independent decisions,” “My job requires learning new skills,” and “I have a lot of say regarding my duties.” Each item had five response categories from “Totally agree” to “Totally disagree.” Each participant’s mean response scores were calculated for job demand and job control. Those who reported higher than the median of the demands scores in the 2000 survey were defined as being exposed to high job demands. Those who reported lower than the median of the job control scores in the 2000 survey were defined as being exposed to low job control. The study-specific median is a commonly used cut-off point for two-dimensional job strain in epidemiological studies.1,4,29,30 The presence of “job strain” in each wave was defined as having high demands and a low control score based on the year 2000 cut-off points. The Cronbach α for the job control scale in these data was 0.82 (in six international data samples it has varied between 0.77 and 0.96).3 For the job demands scale, this index was 0.70 (in six international data samples for five demand items it has varied between 0.51 and 0.72).3
The onset of job strain (high demands and low job control) was defined as reporting no job strain (all other combinations of low/high demands and control) in the first wave, Tx, but reporting job strainin the second wave, Tx+1. Disappearance of these job strain was defined as reporting job strain (high demands and low job control) in the first wave, Ty, but not in the second wave, Ty+1.
Covariates
Covariates were drawn for the year of the baseline survey of each individual (Tx or Ty in Figure 1A and B), that is, from either 2000 or 2004. Information on sex, age, and marital status (married or cohabiting vs. other) was obtained from the employers’ registers. The highest educational degree (high = university degree, intermediate = high school or vocational school, low = comprehensive school) was obtained from Statistics Finland’s register of completed education31 through linkage using personal identification codes. From the baseline study wave questionnaires we obtained information on factors possibly affecting sleep: physical inactivity (based on weekly hours spent on leisure or commuting physical activity multiplied by the activity’s typical energy expenditure expressed as daily metabolic equivalent task hours, <14/wk was used as a cut-off point based on physical activity recommendations32), smoking (current smoker vs. not), and heavy alcohol consumption (>16 drinks/wk for women, >21 drinks/wk for men corresponding to the medium risk levels of daily consumption set by the World Health Organization33), comorbidities (“Has a doctor ever told you have any of the following conditions: asthma, chronic obstructive pulmonary disease, hypertension, diabetes, or depression?” yes (at least one condition) vs. no), as well as height and weight. Using height and weight we calculated body mass index (BMI) as weight in kg/height in meters squared. Information regarding shift work (normal daily working hours vs. not) and sleep apnea (“Have you ever been diagnosed with sleep apnea?” yes vs. no)was also obtained from the questionnaires.
Statistical Methods
We examined whether job strain (a combination of high job demands and low job control) and the individual components of job strain predicted changes in insomnia symptoms. We used a generalized estimating equation (GEE)-based approach (PROC GENMOD in SAS) to account for within-person correlation from those participants who contributed observations to two nested “pseudo-trials.” Due to the observational nature of the FPS study, we were unable to randomize the exposure and we had to analytically adjust for possible confounders to approximate exchangeability between those who remained unexposed and those with onset of exposure between the first two waves. We used two analytical models: (1) a crude model adjusted for trial number only (Model 1), and (2) a model adjusted for trial number, sex and baseline age, marital status, education, physical inactivity, smoking, heavy alcohol consumption, BMI, and comorbidities. As a sensitivity analysis, we also adjusted for shift work and sleep apnea. These variables were only included as additional confounders because we wanted to keep the main model parsimonious and because they had no influence on the effect estimates. To examine the possibility of effect modification by sex or education, we tested the interactions between job strain and sex, and between job strain and education (job strain Tx/y+1 × sex; job strain Tx/y+1 × education). The results are presented as odds ratios (OR) with 95% confidence intervals (CI) using those with “no onset job strain” and “no disappearance of job strain” as the reference groups.
RESULTS
Descriptive statistics of the total study sample and the analytic samples for the onset and disappearance analyses are presented in Table 1. The mean age of the total population was 43.5 (SD = 7.6), of the onset analysis sample 42.9 (SD = 7.5) and that of the disappearance analysis sample 45.0 (SD = 7.1). The mean BMI of the population was 25.0 (SD = 4.1), that of the onset sample 24.9 (SD = 4.0), and that of the disappearance sample 25.5 (SD = 4.3).
Table 1.
Descriptive Statistics of All Participants and Those Included in the Onset and Disappearance Analyses.
| Total (n = 24287) | Onset analysisa (n = 7354) | Disappearance analysisb (n = 2332) | ||||
|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | n | % |
| Men | 4431 | 18.2 | 1601 | 21.8 | 302 | 13.0 |
| Women | 19 856 | 81.8 | 5753 | 78.2 | 2030 | 87.0 |
| Marital status (missing) | (239) | (54) | (33) | |||
| other | 5403 | 22.5 | 1529 | 20.9 | 608 | 26.5 |
| cohabiting | 18 645 | 77.5 | 5771 | 79.1 | 1691 | 73.5 |
| Level of education (missing) | (—) | (—) | (—) | |||
| low | 2040 | 8.40 | 557 | 7.57 | 288 | 12.4 |
| intermediate | 8499 | 35.0 | 2420 | 32.9 | 989 | 42.4 |
| high | 13 748 | 56.6 | 4377 | 59.5 | 1055 | 45.2 |
| Smoking | (632) | (157) | (52) | |||
| no | 19 518 | 82.5 | 5950 | 82.7 | 1839 | 80.7 |
| current | 4137 | 17.5 | 1247 | 17.3 | 441 | 19.3 |
| Alcohol use (missing) | (128) | (18) | (10) | |||
| no/light | 22 170 | 91.8 | 6869 | 93.6 | 2115 | 91.1 |
| moderate/heavy | 1989 | 8.23 | 467 | 6.37 | 207 | 8.91 |
| Physical activity (missing) | (242) | (34) | (10) | |||
| active | 18 286 | 76.0 | 5793 | 79.1 | 1676 | 72.2 |
| inactive | 5759 | 24.0 | 1527 | 20.9 | 646 | 27.8 |
| Comorbidity (missing) | (—) | (—) | (—) | |||
| no | 17 441 | 71.8 | 5877 | 79.9 | 1376 | 59.0 |
| yes | 6846 | 28.2 | 1477 | 20.1 | 956 | 41.0 |
| Shift work (missing) | (—) | (—) | (—) | |||
| no | 16 177 | 66.6 | 5089 | 69.2 | 1406 | 60.3 |
| yes | 8110 | 33.4 | 2265 | 30.8 | 926 | 39.7 |
| Sleep apnoea (missing) | (—) | (—) | (—) | |||
| no | 24 039 | 99.0 | 7319 | 99.5 | 2295 | 98.4 |
| yes | 248 | 1.02 | 35 | 0.48 | 37 | 1.59 |
| Change in exposurec | 873 | 11.9 | 1018 | 43.7 | ||
aNo exposure to job strain and no insomnia symptoms at baseline study wave.
bExposure to job strain and insomnia symptoms at baseline study wave.
cChange in exposure status between wave 1 and 2.
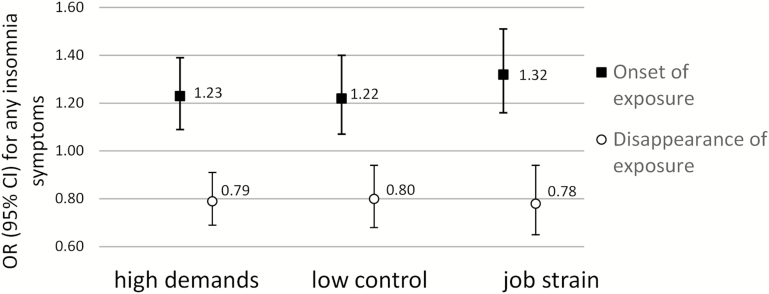
The onset of high job demands, low job control, and job strain (combination of high job demands and low job control) were all predictive of new-onset insomnia symptoms. The ORs for the crude model are presented in Supplementary Table 1. Adjustment for the confounders did not change the estimates (Figure 3): the fully adjusted OR for the onset of insomnia symptoms was 1.23 (95% CI 1.09–1.39, p value .0001) after the onset of high job demands, 1.22 (95% CI 1.07–1.40, p value .004) after the onset of low job control, and 1.32 (95% CI 1.16–1.51, p value <.0001) after the onset of job strain. Goodness of model fit improved with the adjustments; for example, the quasi-likelihood information criterion (QIC)34 for demands model without adjustments was 8170, whereas for the fully adjusted model the QIC was 7797, when smaller value indicates better model fit. All QICs for the onset models are provided in Supplementary Table 1.
Figure 3.
Adjusted associations between onset of exposure and onset of insomnia symptoms (black markers), and between disappearance of exposure and repeated insomnia symptoms (white markers). Models adjusted for trial number, sex, baseline age, marital status, education, body mass index (BMI), smoking, physical activity, heavy alcohol consumption, and comorbidity (asthma or COPD or hypertension or diabetes or depression).
Among participants who reported repeated insomnia symptoms in the first two study waves, disappearance of high job demands, low job control, and job strain were associated with lower odds of repeated insomnia symptoms in the third wave. Adjustment for confounders did not change the crude estimates shown in Supplementary Table 2. The fully adjusted ORs for having repeated insomnia symptoms were 0.79 (95% CI 0.69–0.91, p value .001) among those who no longer experienced high job demands. Corresponding risk estimates were 0.80 (95% CI 0.68–0.94, p value .006) after disappearance of low job control, and 0.78 (95% CI 0.65–0.94, p value .008) after job strain disappeared (Figure 3). Goodness of fit values for all disappearance models are provided in Supplementary Table 2.
In the sensitivity analysis, additionally adjusting for shift work or sleep apnea did not change any of the results (Supplementary Tables 3 and 4). The results obtained from the main analysis were not dependent on sex or education (in the test of interactions all p values > .26).
DISCUSSION
The novel approach used in this observational study allowed us to determine temporality between changes in job strain and insomnia symptoms with high protection against bias. We found that the onset of job strain was associated with an increased risk of a subsequent onset of insomnia symptoms. We also found that among those with insomnia symptoms in the first two waves, the disappearance of job strain was associated with lower odds of repeated insomnia symptoms in the third wave.
Our study can be considered methodically stronger than prior observational studies,19–21 due to the strict inclusion/exclusion criteria we applied, which permitted us to determine the temporality between the onset and disappearance of job strain and changes in insomnia symptoms. One way in which to approximate a test of causality in observational settings would be a case-crossover (or fixed effects) approach that uses data in which each participant has had a change in the outcome measure between the two measurement points making the participants cases as well as their own controls in the analysis.35,36 However, this approach would have been less valid for the current study, in which both exposure and outcome were self-reported at the same time. No previous studies on work and sleep disturbances have been conducted using the present approach and thus, the direction of the associations has so far remained uncertain. Nevertheless, results from previous studies with only two measurement time points support our findings, as they have generally suggested an association between job strain and insomnia symptoms.18–21 Previous FPS research has also linked low job control to an increased risk of insomnia symptoms,37 although one Swedish study did not observe such an association.21 Our study also confirmed the previous findings of a smaller-scale study suggesting that a transition from a non-high-strain to a high-strain job was associated with an increased risk of sleep complaints.18
Our study is among the first to examine whether the disappearance of job strain is associated with a reduction in insomnia symptoms. We are aware of only one study that has examined the transition from high-strain to non-high-strain job, but this study observed no association with sleep outcomes. With sleep measured only twice, the study could not examine the sequence of the changes in the exposure and sleep complaints.18 The potential mechanisms linking lower job strain to an increased likelihood of remission of insomnia symptoms included the alleviation of negative psychological processes that may underlie disturbed sleep, such as perceived stress and worries about work-related issues.38
Strengths and Limitations
The major strength of this study is its large study population with repeated measures of job strain and sleep. Although we could not randomize the exposure, we were able to control for a broad range of individual-level confounding factors.
The generalizability of our findings may be limited by the fact that the vast majority of the study population was of Caucasian ethnicity, and that the study focused on mainly female public sector employees in a country with high social welfare. A further limitation is the use of self-reported data on job strain and insomnia symptoms, which may cause concern regarding common method bias, that is, those who score high on a risk factor measure also tend to score high on the outcome measure. This type of bias was, however, less of a concern in a study that examined changes in job strain and sleep within the same individual.
Self-reported insomnia symptoms are not a specific measure of clinical insomnia, but are commonly used in epidemiological studies.12,20,21,37 We used a summary outcome of any insomnia symptoms, and to confirm the appropriateness of this approach, we conducted similar analyses for individual insomnia symptoms. The results were consistent with those presented. Although the temporal order of the exposure and the outcome were predefined by the study design, the time lag between the study waves was fixed at 4 years. Thus, it is possible that the changes in insomnia symptoms over such a long period of time after the onset/disappearance of job strain were affected by other unmeasured factors that occurred between the study waves.
CONCLUSIONS AND IMPLICATIONS
Our results are consistent with the hypothesis that job strain may affect sleep and that the disappearance of job strain may reduce insomnia symptoms among those with sleeping problems. These findings have important implications for interventions and the prevention of insomnia specifically within the workplace. Job strain is modifiable through interventions involving increased employee participation, training at different levels of the organizational hierarchy, and job redesign.2,39 As work stress has been associated with poor sleep,11 and there is evidence to suggest that such interventions may reduce stress levels among employees,40,41 the alleviation of insomnia symptoms also seems plausible, a hypothesis supported by the present analysis, which mimicked a non-randomized trial design. However, further intervention studies are needed to examine this directly and to determine the extent to which the reduction of job strain might also affect the consequences of disturbed sleep, such as sickness absenteeism, work disability, and occupational accidents.42
SUPPLEMENTARY MATERIAL
Supplementary Material is available at SLEEP online.
FUNDING
The study was supported by the Academy of Finland (projects 287488 and 294096 to TL; 286294 and 294154 to SS; 267727 to JV; 258598 and 292824 to MV) and the participating organizations. SS is supported by the Ministry of Education and Culture. NHR is supported by the Danish Working Environment Foundation. MK is supported by Nordforsk, the Nordic Programme on Health and Welfare, the UK Medical Research Council (K013351) and the Economic and Social Research Council.
DISCLOSURE STATEMENT
No off-label or investigational use. All authors disclose no conflict of interest. Not a clinical trial.
Supplementary Material
REFERENCES
- 1. Karasek R. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979; 24(2): 285–308. [Google Scholar]
- 2. Karasek R, Theorell T. Healthy Work: Stress, Productivity and the Reconstruction of Working Life. New York, NY: Basic Books; 1990. [Google Scholar]
- 3. Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998; 3(4): 322–355. [DOI] [PubMed] [Google Scholar]
- 4. Fransson EI, Nyberg ST, Heikkilä K, et al. Comparison of alternative versions of the job demand-control scales in 17 European cohort studies: the IPD-Work consortium. BMC Public Health. 2012; 12(62). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Theorell T, Hammarström A, Aronsson G, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health. 2015; 15(738). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Steptoe A, Kivimäki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health. 2013; 34: 337–354. [DOI] [PubMed] [Google Scholar]
- 7. Johnson JV, Hall EM. Job strain, work place social support, and cardiovascular disease: a cross-sectional study of a random sample of the Swedish working population. Am J Public Health. 1988; 78(10): 1336–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Johnson JV, Stewart W, Hall EM, Fredlund P, Theorell T. Long-term psychosocial work environment and cardiovascular mortality among Swedish men. Am J Public Health. 1996; 86(3): 324–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Knudsen HK, Ducharme LJ, Roman PM. Job stress and poor sleep quality: data from an American sample of full-time workers. Soc Sci Med. 2007; 64(10): 1997–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Salo P, Vahtera J, Ferrie JE, et al. Trajectories of sleep complaints from early midlife to old age: longitudinal modeling study. Sleep. 2012; 35(11): 1559–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hammer LB, Sauter S. Total worker health and work-life stress. J Occup Environ Med. 2013; 55(12 suppl): S25–S29. [DOI] [PubMed] [Google Scholar]
- 12. Salo P, Oksanen T, Sivertsen B, et al. Sleep disturbances as a predictor of cause-specific work disability and delayed return to work. Sleep. 2010; 33(10): 1323–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Salo P, Vahtera J, Hall M, et al. Using repeated measures of sleep disturbances to predict future diagnosis-specific work disability: a cohort study. Sleep. 2012; 35(4): 559–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lallukka T, Kaikkonen R, Harkanen T, et al. Sleep and sickness absence: a nationally representative register-based follow-up study. Sleep. 2014; 37(9): 1413–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sivertsen B, Björnsdóttir E, Øverland S, Bjorvatn B, Salo P. The joint contribution of insomnia and obstructive sleep apnoea on sickness absence. J Sleep Res. 2013; 22(2): 223–230. [DOI] [PubMed] [Google Scholar]
- 16. Hägg SA, Torén K, Lindberg E. Role of sleep disturbances in occupational accidents among women. Scand J Work Environ Health. 2015. ;41(4): 368–376. [DOI] [PubMed] [Google Scholar]
- 17. Sivertsen B, Lallukka T, Salo P, et al. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res. 2014; 23(2): 124–132. [DOI] [PubMed] [Google Scholar]
- 18. de Lange AH, Kompier MA, Taris TW, et al. A hard day’s night: a longitudinal study on the relationships among job demands and job control, sleep quality and fatigue. J Sleep Res. 2009; 18(3): 374–383. [DOI] [PubMed] [Google Scholar]
- 19. Vleeshouwers J, Knardahl S, Christensen JO. Effects of psychological and social work factors on self-reported sleep disturbance and difficulties initiating sleep. Sleep. 2015; 39(4): 833–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chazelle E, Chastang JF, Niedhammer I. Psychosocial work factors and sleep problems: findings from the French national SIP survey. Int Arch Occup Environ Health. 2016; 89(3): 485–495. [DOI] [PubMed] [Google Scholar]
- 21. Akerstedt T, Garefelt J, Richter A, et al. Work and sleep--aprospective study of psychosocial work factors, physical work factors, and work scheduling. Sleep. 2015; 38(7): 1129–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Magnusson Hanson LL, Chungkham HS, Åkerstedt T, Westerlund H. The role of sleep disturbances in the longitudinal relationship between psychosocial working conditions, measured by work demands and support, and depression. Sleep. 2014; 37(12): 1977–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hernán MA, Alonso A, Logan R, et al. Observational studies analyzed like randomized experiments: an application to postmenopausal hormone therapy and coronary heart disease. Epidemiology. 2008; 19(6): 766–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kivimaki M, Lawlor DA, Davey Smith G, et al. Socioeconomic position, co-occurrence of behavior-related risk factors, and coronary heart disease: the Finnish Public Sector study. Am J Public Health. 2007; 97(5): 874–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Clark AJ, Salo P, Lange T, et al. Onset of impaired sleep as a predictor of change in health-related behaviours; analysing observational data as a series of non-randomized pseudo-trials. Int J Epidemiol. 2015; 44(3): 1027–1037. [DOI] [PubMed] [Google Scholar]
- 26. Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988; 41(4): 313–321. [DOI] [PubMed] [Google Scholar]
- 27. Halonen JI, Vahtera J, Stansfeld S, et al. Associations between nighttime traffic noise and sleep: the Finnish public sector study. Environ Health Perspect. 2012; 120(10): 1391–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 29. Heikkila K, Fransson EI, Nyberg ST, et al. Job strain and health-related lifestyle: findings from an individual-participant meta-analysis of 118,000 working adults. Am J Public Health. 2013; 103(11): 2090–2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kivimaki M, Nyberg ST, Batty GD, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012; 380(9852): 1491–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Statistics Finland. Education 2016. www.stat.fi/til/kou_en.html Accessed June 7, 2016.
- 32. Kouvonen A, Vahtera J, Oksanen T, et al. Chronic workplace stress and insufficient physical activity: a cohort study. Occup Environ Med. 2013; 70(1):3–8. [DOI] [PubMed] [Google Scholar]
- 33. WHO. International Guide for Monitoring Alcohol Consumption and Related Harm Department of Mental Health and Substance Dependence, Noncommunicable Diseases and Mental Health Cluster, WHO; 2000. [Google Scholar]
- 34. Pan W. Akaike’s information criterion in generalized estimating equations. Biometrics. 2001; 57(1): 120–125. [DOI] [PubMed] [Google Scholar]
- 35. Allison PD. Fixed Effects Regression Methods for Longitudinal Data Using SAS: SAS. Cary, NC: SAS Institute Inc; 2005. [Google Scholar]
- 36. Halonen JI, Kivimaki M, Virtanen M, et al. Living in proximity of a bar and risky alcohol behaviours: a longitudinal study. Addiction. 2013; 108(2): 320–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Salo P, Ala-Mursula L, Rod NH, et al. Work time control and sleep disturbances: prospective cohort study of Finnish public sector employees. Sleep. 2014; 37(7): 1217–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Brosschot JF, Van Dijk E, Thayer JF. Daily worry is related to low heart rate variability during waking and the subsequent nocturnal sleep period. Int J Psychophysiol. 2007; 63(1): 39–47. [DOI] [PubMed] [Google Scholar]
- 39. Theorell T, Emdad R, Arnetz B, Weingarten AM. Employee effects of an educational program for managers at an insurance company. Psychosom Med. 2001; 63(5): 724–733. [DOI] [PubMed] [Google Scholar]
- 40. Kvarnström S. From Taylorism to 1000 objective-oriented groups: experiences of a cultural evolution in an industrial concern. In: Cooper CL, Liukkonen P, Catwright S. eds. Stress Prevention in Workplace: Assessing the Cost and Benefits to Organisations. Dublin, OH: European Foundation for the Improvement of Living and Working Conditions; 1996: 12–25. [Google Scholar]
- 41. Ebert DD, Heber E, Berking M, et al. Self-guided internet-based and mobile-based stress management for employees: results of a randomised controlled trial. Occup Environ Med. 2016; 73(5): 315–323. [DOI] [PubMed] [Google Scholar]
- 42. Glendon I, Clarke S, McKenna E. Human Safety and Risk Management, 2nd ed. Boca Raton, FL: Taylor & Francis Group; 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.