Abstract
Study Objectives:
Fatigue from sleep loss is a risk to physician and patient safety, but objective data on physician sleep and alertness on different duty hour schedules is scarce. This study objectively quantified differences in sleep duration and alertness between medical interns working extended overnight shifts and residents not or rarely working extended overnight shifts.
Methods:
Sleep–wake activity of 137 interns and 87 PGY-2/3 residents on 2-week Internal Medicine and Oncology rotations was assessed with wrist-actigraphy. Alertness was assessed daily with a brief Psychomotor Vigilance Test (PVT) and the Karolinska Sleepiness Scale.
Results:
Interns averaged 6.93 hours (95% confidence interval [CI] 6.84–7.03 hours) sleep per 24 hours across shifts, significantly less than residents not working overnight shifts (7.18 hours, 95% CI 7.06–7.30 hours, p = .007). Interns obtained on average 2.19 hours (95% CI 2.02–2.36 hours) sleep during on-call nights (17.5% obtained no sleep). Alertness was significantly lower on mornings after on-call nights compared to regular shifts (p < .001). Naps between 9 am and 6 pm on the first day post‐call were frequent (90.8%) and averaged 2.84 hours (95% CI 2.69–3.00 hours), but interns still slept 1.66 hours less per 24 hours (95% CI 1.56–1.76 hours) compared to regular shift days (p < .001). Sleep inertia significantly affected alertness in the 60 minutes after waking on-call.
Conclusions:
Extended overnight shifts increase the likelihood of chronic sleep restriction in interns. Reduced levels of alertness after on-call nights need to be mitigated. A systematic comparison of sleep, alertness, and safety outcomes under current and past duty hour rules is encouraged.
Keywords: alertness, medical education, shiftwork, medical interns, psychomotor vigilance performance, fatigue, sleep deprivation, actigraphy, effects of sleep restriction on cognition and affect.
Statement of Significance
Extended overnight shifts play an important role in graduate medical education, but can also affect physician and patient safety through acute and chronic sleep restriction. This is one of the largest studies to date objectively assessing intern and resident sleep and alertness on different shift schedules. Average sleep time in interns working extended overnight shifts was only moderately decreased compared to residents not or rarely working night shifts. However, intern alertness on mornings following overnight shifts was profoundly impaired and calls for mitigation strategies. More studies objectively assessing sleep, alertness, educational outcomes, and patient care outcomes are needed to inform duty hour regulations and maximize physician and patient safety.
INTRODUCTION
Fatigue—broadly defined as “a physiological state of reduced mental or physical performance capability”—is a risk factor for errors and accidents and is frequently encountered in operations that need to be sustained 24/7. In the medical profession, fatigue associated with working more than 80 hours per week and extended overnight shifts has been shown to affect both physician and patient safety.1–4 Consequently, the Accreditation Council for Graduate Medical Education (ACGME) established the first national duty hour regulations that included 80-hour weekly limits in 2003.
Following a 2009 Institute of Medicine (IOM) report5 that articulated concerns relative to fatigue during 30-hour duty periods, the ACGME revised its duty hour regulations in 2011 such that duty periods of first year medical residents (interns) must not exceed 16 hours in duration. It is debated whether preventing interns from participating in extended shifts reduces educational opportunities and affects continuity of care6,7 in addition to requiring more cross coverage from upper level residents, which in turn may increase fatigue in those more responsible for clinical decision making.8 Interns can still work night shifts under the new regulations, usually in blocks of 1 or 2 weeks requiring them to transition into and out of a night shift multiple times over the course of the year, which may also result in fatigue from acute and chronic sleep loss and circadian misalignment typically observed during shift work.9 Survey data suggest that the implementation of the 2011 duty hour regulations did not increase sleep duration significantly,10 but adequately designed and powered studies with objective sleep and alertness outcomes are missing.11
Irrespective of the regulatory changes implemented by the ACGME, fatigue from extended work periods and overnight shifts remains a significant challenge in the medical profession. In the period 2009–2011, we performed two randomized controlled trials on the effect of a protected sleep period during extended overnight shifts on sleep and alertness of interns.12,13 The current analysis examines the sleep patterns among participants in the control groups of these trials and adds data collected in PGY2-3 residents providing the first comprehensive characterization of objectively assessed sleep–wake behavior and alertness in a large number of interns and residents working different shift schedules.
METHODS
Subjects and Protocol
Data were collected in two randomized controlled clinical trials on the effects of 5-hour (July 2009 until June 2010) and 3-hour (July 2010 until June 2011) protected sleep periods during extended overnight shifts on intern and senior medical student sleep duration and alertness.12,13 The protocol was approved by the institutional review boards at the Philadelphia VA Medical Center (VA) and the University of Pennsylvania, and registered at clinicaltrials.gov as A Randomized Control Trial of Mandatory Naps for Physicians in Training, ID # NCT00874510.
In each study year, six pairs of consecutive 4-week blocks were randomized to an intervention schedule (protected sleep period) or the standard schedule. Data collection was planned from Monday of the first week through Friday of the final week (25 days). This analysis concentrates on the control groups that had no protected sleep period and also includes residents who worked regular schedules independent of the intervention (first trial only). Residents were scheduled for 2-week or 4-week blocks. All interns and residents from the University of Pennsylvania Health System who were on Internal Medicine rotations at the VA or on the oncology unit of the Hospital of the University of Pennsylvania (HUP) were invited to participate. On-call teams consisted of 2 interns (or 1 intern and 1 senior medical student) and 1 PGY2 or PGY3 night-float resident. Senior medical students and interns worked identical schedules and will be referred to as interns for simplicity throughout the manuscript. Interns started work at 7 am. Each pair of interns was on-call every fourth night, admitted patients throughout the night, was responsible for cross-coverage until the primary team returned around 7 am, and generally worked until approximately 1 pm the next day (a 30-hour duty period). Residents at HUP only performed regular shifts from 7 am to either 5 pm or 8 pm. Residents at VA performed regular shifts from 8 am to either 5 pm or 8 pm, briefer Saturday morning shifts from 8 am to 1 pm, and weekend extended overnight shifts that were scheduled to end either at 1 pm or 5 pm the next day. Both interns and residents were scheduled to average 1 out of 7 days off over 4 weeks. Characteristics of participants who contributed to the analysis are summarized in Table 1.
Table 1.
Subject Characteristics.
| Unique subjects | Age | Female | Number of rotations | |||
|---|---|---|---|---|---|---|
| N | Years (SD) | % | 1 | 2 | 3 | |
| Interns | 137 | 27.6 (2.3) | 50.4 | 58.4% | 32.8% | 8.8% |
| Residents | 87 | 29.1 (2.7) | 57.5 | 49.4% | 43.7% | 6.9% |
Data analysis was based on N = 137 unique interns (N = 70 year 1, N = 63 year 2, N = 4 years 1&2) and 87 unique residents (year 1 only). The group of interns included 32 senior medical students in year 1 and 31 senior medical students in year 2. 41.6% of interns/senior medical students and 50.6% of residents rotated more than once through the control group arm of the study.
Measurement and Outcomes
Subjects met with study staff on the first day of each rotation for orientation, including instructions on continuous use of an actigraph (Actiwatch Spectrum, Philips Respironics), a watch-like accelerometer that measures wrist movement intensity and stores it in 1-minute epochs. Actigraphy is a well-established method for rest-activity measurement14 and has been used previously to successfully study sleep patterns in physicians.15,16 Study participants were also asked to complete a validated 3-minute Psychomotor Vigilance Test (PVT)17,18 each morning they were in the hospital on laptops located throughout the facility (if possible between 6 am and 9 am). The PVT measures alertness based on reaction time to stimuli presented at random inter-stimulus intervals (2–5 seconds). Response speed (a reciprocal transform of reaction time that has superior statistical properties; higher values indicate better performance) and attentional lapses (number of reaction times ≥355 ms) were used as primary PVT outcomes.19,20 Before each PVT, participants filled out an electronic sleep log that contained the Karolinska Sleepiness Scale (KSS),21 a 9 point verbally anchored scale ranging from “extremely alert” (score = 1) to “extremely sleepy-fighting sleep” (score = 9). At the end of the rotation research assistants collected the actigraphs and distributed $25 gift cards for every week of adherence to study measures.
Data Analysis
A total of 239 subjects consented to participate in the study. Five subjects never started data acquisition. Actiwatches failed to collect valid data in another 10 subjects. Acquisition of 5951 days of actigraphy was scheduled from the remaining 224 participants (excluding the first and the last study day, when watches were handed out or collected). As interns were instructed to take off the actiwatch during sports, swimming/bathing, and medical procedures that would be affected by wearing the watch, we did not expect 100% wear time. The result was that 89.3% of all possible actigraphy data was acquired. One minute actigraphy epochs were automatically classified into wake and sleep with the Respironics Actiware software (Version 5.59.0015, standard settings). Sleep periods recorded in sleep logs were used to impute missing data (accounting for 1.5% of the expected data). We used single imputation based on subject type (intern/resident), hospital (HUP/VA), shift type (eg, on-call, off, etc.) and minute of the day if both actigraphy and sleep log data were missing. Daytime nap analyses were restricted to subjects with valid actigraphy or sleep log data in the period 9 pm on the previous day to 9 pm on the nap day.
Interns and residents were scheduled to perform 5610 morning PVTs; 4297 PVTs (76.6%) were collected; 139 PVTs collected before 5 am or after 2 pm were not included in the analyses, which left 4158 PVTs (74.1% adherence) for data analysis. PVT adherence did not differ between interns (73.7%) and residents (74.9%; p = .82); between regular shifts (74.3%) and extended overnight shifts (73.3%; p = 0.80) in interns; between residents working regular shifts at VA (75.1%) and at HUP (75.1%; p = .95); and between regular shifts (75.1%) and weekend shifts (72.4%; p = .63) in residents working at VA. Therefore, the pattern of missing PVT data was expected to be missing at random. Mixed model maximum likelihood estimates account for this type of missing data, thus PVT and KSS data were not imputed.22 Unless stated otherwise, linear mixed effect models with random subject intercept were used for data analysis to account for the clustered nature of the data (Proc Mixed in SAS, Version 9.3, SAS Institute, Carey, NC). All regression models with PVT outcome variables were adjusted for age (continuous variable), sex, and whether or not the subject indicated to have been distracted during the PVT (25.7% of PVTs). For KSS, regression models were only adjusted for age (continuous variable) and sex. For sleep time analyses, the 24-hour day was divided into a daytime (9 am–9 pm) and nighttime period (9 pm–9 am).
RESULTS
Sleep
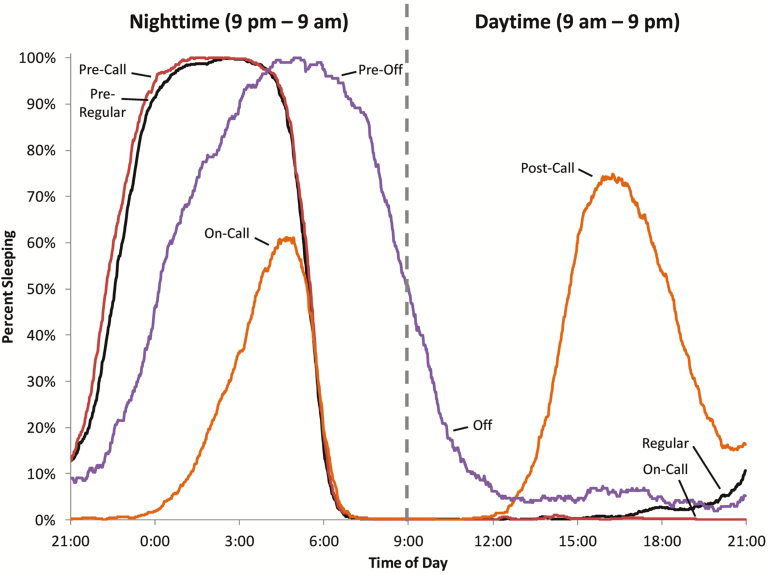
As there were no significant differences in sleep time for interns between study sites (p for all shift types > 0.1), intern data were pooled for analyses. During on‐call nights, interns obtained on average 2.19 hours sleep (95% CI 2.08–2.29 hours, Table 2), significantly less compared to regular shift days (6.93 hours, 95% CI 6.83–7.03 hours, p < .001, Table 2). In 17.5% of nights, interns obtained no sleep at all, 33.3% slept ≤ 2 hours, 34.6% > 2 and ≤4 hours, and 14.5% > 4 hours during on-call nights (9 pm–9 am). Some of the sleep lost during on-call nights was recuperated by napping during the post call day (Figure 1). Daytime sleep on the first day post‐call averaged 3.26 hours (95% CI 3.19–3.33 hours), but interns still slept 1.66 hours (95% CI 1.56–1.76 hours) less per 24 hours on on-call nights and post-call days compared to regular shift days (p < .001). On days off, interns slept 1.94 hours (95% CI 1.81–2.07 hours) longer than on regular shift days (p < .001). Interns went to bed much later on nights preceding days off compared to nights preceding work days, but also got up considerably later (Figure 1).
Table 2.
Sleep Time Depending on Shift Type and Time of Day.
| Night 9 pm–9 am | Day 9 am–9 pm | Night + Day (9 pm–9 pm) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nights (N) | Shift type | Sleep time hours (95% CI) | p | Shift type | Sleep time hours (95% CI) | p | Sleep time hours (95% CI) | p | |
| InternsHUP & VA | 1731 | Before regular shift | 6.93 (6.83;7.03) | Ref. | On regular shift | 0.18 (0.12;0.25) | Ref. | 7.11 (7.00;7.22) | Ref. |
| 1118 | Before call | 7.12 (7.01;7.22) | <.001 | On-call | 0.02 (0.00; 0.09) | <.001 | 7.14 (7.02;7.26) | .60 | |
| 1088 | On-call | 2.19 (2.08;2.29) | <.001 | Post call | 3.26 (3.19; 3.33) | <.001 | 5.45 (5.33;5.57) | <.001 | |
| 513 | Before day off | 8.07 (7.94;8.20) | <.001 | On day off | 0.98 (0.89;1.08) | <.001 | 9.05 (8.91;9.20) | <.001 | |
| 4450 | All shift types | 5.95 (5.86;6.03) | — | All shift types | 0.99 (0.94;1.04) | — | 6.93 (6.84;7.03) | — | |
| ResidentsHUP | 434 | Before shift 7 am–5 pm | 6.75 (6.62;6.89) | Ref. | On shift 7 am–5 pm | 0.05 (0.01;0.08) | Ref. | 6.80 (6.67;6.94) | Ref. |
| 524 | Before Shift 7 am–8 pm | 7.00 (6.87;7.13) | <.001 | On shift 7 am–8 pm | 0.03 (0.00;0.07) | .569 | 7.03 (6.90;7.16) | <.001 | |
| 103 | Before day off | 8.29 (8.11;8.48) | <.001 | On day off | 1.25 (1.17;1.32) | <.001 | 9.55 (9.34;9.75) | <.001 | |
| 1061 | All shift types | 7.02 (6.90;7.14) | — | All shift types | 0.15 (0.12;0.18) | — | 7.18 (7.06;7.30) | — | |
| ResidentsVA | 649 | Before shift 8 am–5 pm | 6.80 (6.62;6.98) | Ref. | On shift 8 am–5 pm | 0.18 (0.11;0.26) | Ref. | 6.99 (6.80;7.18) | Ref. |
| 214 | Before shift 8 am–8 pm | 7.22 (7.01;7.44) | <.001 | On shift 8 am–8 pm | 0.02 (0.00;0.12) | .002 | 7.24 (7.01;7.48) | .015 | |
| 31 | Before Sat 8 am–1 pm | 6.17 (5.75;6.59) | .002 | On Sat 8 am–1 pm | 0.13 (0.00;0.37) | .67 | 6.31 (5.82;6.80) | .005 | |
| 67 | Before call | 7.10 (6.79;7.40) | .037 | On-call | 0.06 (0.00;0.23) | .144 | 7.16 (6.81;7.51) | .31 | |
| 65 | On-call | 3.16 (2.85;3.47) | <.001 | Post call | 3.47 (3.30;3.63) | <.001 | 6.63 (6.27;6.98) | .033 | |
| 100 | Before day off | 8.22 (7.95;8.49) | <.001 | On day off | 1.00 (0.86;1.13) | <.001 | 9.22 (8.92;9.52) | <.001 | |
| 1126 | All shift types | 6.81 (6.63;6.98) | — | All shift types | 0.40 (0.34;0.47) | — | 7.21 (7.03;7.38) | — | |
CI = Confidence Interval; Ref. = Reference Category; Sat = Saturday.
Figure 1.
Percent of interns sleeping by time of day and shift type. Interns obtained significantly less sleep during on-call nights but recovered some of the sleep lost during post-call days. Interns retired later prior to days off, but also slept later on days off. Interns retired somewhat earlier on nights prior to and in anticipation of on-call days.
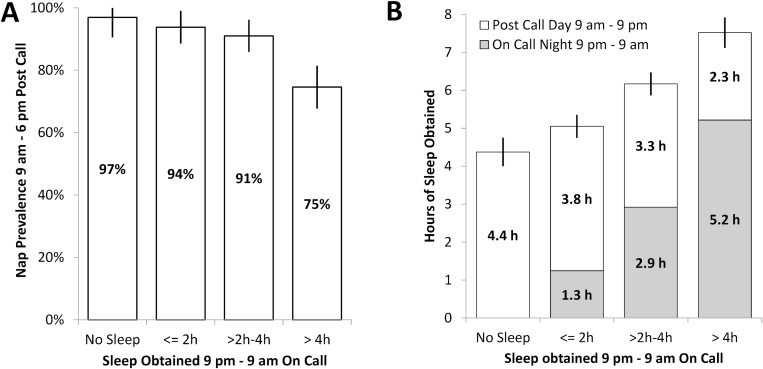
On average, 90.7% (95% CI 87.0–94.4%) of interns napped during the post‐call day in the period 9 am–6 pm, while only 6.0% (95% CI 3.6–8.4%) and 11.7% (95% CI 8.0–15.4%) napped on the second and third post‐call days, respectively. More sleep obtained during the on‐call night was associated with lower nap prevalence on the post‐call day (Figure 2A). Nap duration averaged 2.84 hours (95% CI 2.69–3.00 hours) in the period 9 am–6 pm. However, compared to a regular shift, interns were only able to fully recuperate the sleep lost during on-call nights on post call days (relative to a regular shift in which they slept an average of 7.11 hours, 95% CI 7.00–7.22 hours) if they obtained more than 4 hours sleep during on-call nights (Figure 2B). Those who napped during the post‐call day did not differ from those who did not nap relative to next day PVT performance or subjective sleepiness (all p > .5).
Figure 2.
Post call napping in interns. (A) The prevalence of napping in the period 9 am–6 pm on the first day post-call was inversely related to the amount of sleep obtained during the on-call night. (B) Sleep lost during the on-call night was partially recuperated by interns through naps on the first day post call. The more sleep interns lost during the on-call night (9 pm–9 am), the more sleep they obtained during the first day post call (9 am–9 pm). However, compared to a regular shift day (7.11 hours sleep per 24 hours), interns were only able to fully recuperate the sleep lost during on-call nights during post call days if they obtained more than 4 hours sleep during on-call nights. All error bars reflect 95% confidence intervals.
Across all shifts, residents at HUP and VA obtained similar amounts of sleep per 24 hours (7.18 vs. 7.21 hours, respectively; p = .177). Interns working extended overnight shifts averaged 6.93 hours sleep per 24 hours (95% CI 6.84–7.03 hours) across all shifts, which was significantly less compared to both HUP residents (7.18 hours, 95% CI 7.06–7.30 hours, p = .007) and VA residents (7.21 hours, 95% CI 7.03–7.38 hours, p = .007). Compared to VA residents (who started regular shifts at 8 am), HUP residents (who started at 7 am) slept 0.24 hours (95% CI 0.18–0.30 hours, p < .001) less in the period 3 am–9 am prior to the start of their shift. In residents at both HUP and VA, the shift ended either at 5 pm or at 8 pm on regular shift days. Compared to shifts ending at 5 pm, residents whose shift ended at 8 pm slept 0.40 hours (95% CI 0.32–0.47 hours, p < .001) less in the period 9 pm–3 am following their shift end. Compared to regular shifts, we found increased nocturnal sleep time in anticipation of on-call nights in interns (+0.18 hours, 95% CI 0.10–0.27 hours, p < .001) and VA residents (+0.29 hours, 95% CI 0.02–0.57 hours, p = .037), and also in anticipation of shifts ending late in VA residents (+0.42 hours; 95% CI 0.25–0.59 hours, p < .001) and HUP residents (+0.24 hours, 95% CI 0.14–0.34 hours, p < .001). Both interns and residents averaged > 9 hours sleep on days off.
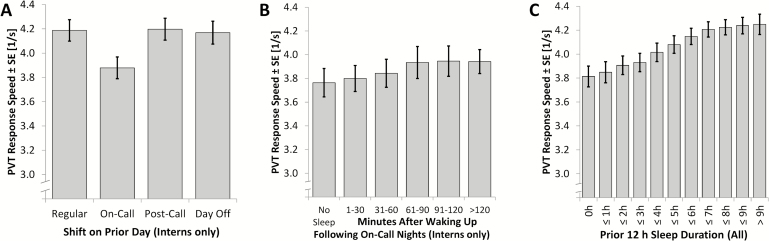
Alertness
Psychomotor speed, the number of attentional lapses, and subjective sleepiness were all significantly worse on mornings after on‐call nights compared to all other shifts in interns (Figure 3A, Supplementary Figures S1A and S2A; all p < .001). Alertness was most severely affected in interns who did not sleep at all on-call (Figure 3B, Supplementary Figures S1B and S2B). Sleep inertia23 affected alertness in the first hour after waking up. In fact, there was no significant difference in alertness assessed by the PVT between interns that did not sleep and those that slept but tested within 60 minutes after waking up (all p > .1). In those interns who did get some sleep on call, sleep duration did not modify the sleep inertia effect for PVT response speed (p = .0685), PVT lapses (p = .2434), and subjective sleepiness assessed with the KSS (p = .1822). In a pooled analysis of intern and resident data across shifts, alertness improved monotonically with the amount slept in the prior night, leveling off for sleep durations >7 hours (Figure 3C, Supplementary Figures S1C and S2C). The lowest levels of alertness were observed after nights without any sleep (0 h).
Figure 3.
Psychomotor Vigilance Test (PVT) response speed analyses. A 3-minute PVT was performed each morning in the hospital (average time PVT was taken was 07:56 am). Higher response speed values reflect faster reaction times on the PVT and higher levels of alertness. The 3/s starting point of the ordinate was chosen as 97% of the observed response speed values fell above this value. Error bars reflect standard errors (SE). (A) PVT response speed was significantly slower in interns after on-call nights compared to all other shifts (all p < .001). (B) PVT response speed in interns depending on minutes elapsed after waking up and relative to those who did not sleep in the 12 hours prior to PVT administration. Response speed was lowest in those who did not sleep at all. In those who did sleep on-call, response speed was decreased in the first hour after waking up due to sleep inertia. It did not differ significantly during this first hour compared to response speed of interns who did not sleep at all (p > .18). (C) PVT response speed in interns and residents increased strictly monotonic with sleep obtained in the 12 hours prior to PVT administration. It was lowest in those who did not sleep at all (0 hours).
DISCUSSIONS
As humans have limited insight into how sleep loss affects their performance,24,25 it is important to obtain objective measures of sleep and alertness in physicians to assess the impact of shift schedules on acute and chronic sleep loss and the resulting effects on cognitive performance. This is one of the most comprehensive studies objectively assessing sleep and alertness in medical interns and residents to date.
Across all shifts, sleep time averaged 7.18 hours and 7.21 hours per 24 hours among residents who did not work or only sporadically worked extended overnight shifts, respectively, which is within the range of sleep time that does not result in cognitive deficits.25–27 In comparison, interns working extended overnight shifts every fourth day averaged 6.93 hours sleep per 24 hours across all shifts. The effects of sleep restriction are cumulative.25,26 Despite the modest average difference of 15–17 minutes between intern and resident sleep per 24 hours, the extra sleep observed in residents may be crucial to sustain a higher level of alertness and performance. Chronically restricted sleep to 7 hours or less per 24 hours has been shown to lead to escalating deficits in vigilant attention with potential adverse effects for errors and safety.25,26 This sleep deficit was generated during on-call nights and post call days, where interns lost 1.66 hours sleep per 24 hours compared to regular shifts. Our data suggest it could be offset by providing interns with one day off (+1.94 hours sleep relative to regular shifts) for every overnight shift. Interns were scheduled to have 1 out of 7 days off in this study.
These findings agree in general with previous similar studies that mostly reported sleep durations between 6 and 8 hours per 24 hours across different shift days.6,28–32 However, studies measuring sleep duration in interns or residents with sleep logs and/or actigraphy are scarce, and only a subset of those reported sleep duration across different shifts. The wide range of sleep duration estimates can likely be explained by differences in residency programs and the small sample size of the majority of previous studies, underlining the importance of the findings reported here.
Although 82.5% of interns obtained at least some sleep during on-call nights, both objective and subjective measures of morning alertness were significantly diminished compared to regular shifts. Decreases in psychomotor performance similar in magnitude to those observed in this study induced by staying up beyond normal bed time or by not sleeping at all for a full night, have been shown to be comparable to the effects of blood alcohol concentrations of 0.05%–0.1%.33,34 They should thus not be easily dismissed, and call for mitigation strategies to prevent negative consequences for physician and patient safety.1–3
The most powerful countermeasure to overcome the effects of acute and chronic sleep loss is sleep itself.35–39 In this study, we found a monotonic increase in alertness with sleep duration in the preceding 12 hours, demonstrating that even brief sleep periods (ie, prophylactic naps) have beneficial recuperative effects.40 We have already demonstrated that 5-hour and 3-hour protected sleep periods during extended overnight shifts are both feasible and associated with increased sleep time and alertness during and following overnight shifts, the latter without the requirement of additional resident cross coverage.12,13 However, our data also demonstrate that sleep inertia (ie, a period of reduced performance capability after waking up) poses a potential risk to physician and patient safety, as alertness was reduced during the first 60 minutes after waking up on-call and did not differ significantly relative to interns who obtained no sleep at all. Prior sleep duration did not modify this sleep inertia effect on alertness. In a paradigm where residents are provided with a protected nocturnal sleep period during the overnight call, this could be addressed by asking them to get up at least 30 minutes before the end of the protected sleep period. In addition, caffeine and bright light administered after waking up from a nap have been shown to overcome the effects of sleep inertia.41,42 Another strategy for mitigating the effects of acute sleep loss is to limit shift duration as practiced by interns under the current ACGME rules, where shift duration is limited to 16 hours for PGY-1 residents only.7,11,43 This reduces the likelihood of working during the circadian nadir with a high homeostatic sleep pressure. However, interns still need to transition into and out of night shifts, which are often scheduled on consecutive days, with potential shifts in circadian phase and shorter and disturbed sleep periods during the day. Studies investigating the effects of novel shift schedules (eg, rapid cycle rotation schedules44) on sleep, alertness, and educational outcomes are needed to optimize physician and patient safety, while minimizing additional staff cost due to shift coverage.
Interns and residents also behaved adaptively by increasing sleep time on nights prior to extended overnight shifts or late ending shifts. Additionally, most of the interns decreased the sleep deficit obtained during on-call nights by napping during the post call day, which resulted in a greater total sleep time per 24 hours. This split-sleep strategy is known to reduce sleep debt and prevent performance deficits,38 and it appears to effectively mitigate the sleep loss associated with call. It should therefore be promoted among physicians.
The large sample size, the investigation of both interns and PGY-2/3 residents under a variety of shift schedules, and the fact that we used both sleep logs and actigraphy to objectively assess sleep duration are strengths of our study. Limitations of this study include its generalizability to interns and residents at other internal medicine residency programs as well as to interns and residents in different specialties, though it is not obvious that the general patterns of sleep relative to call cycles and the basic physiological relationship between sleep deprivation and cognitive performance would differ for residents in different programs. We did not record physician (eg, needle sticks) or patient (eg, mortality) safety outcomes. Instead, we used a brief version of the PVT as a sensitive and objective essay of daily morning alertness.17,45 It measures vigilant attention, which is a prerequisite for all more complex cognitive tasks. It also has face validity in the sense that the inability to respond to changes in the environment in a timely fashion is not compatible with safe operations. Furthermore, performance decrements on the PVT have been shown to predict performance decrements on complex operational tasks under sleep deprivation.18 Finally, adherence to the PVT and sleep logs was moderate, which is not uncommon in operational settings. Adherence rates did, however, not differ between interns and residents and between the different shift types. It is therefore unlikely that adherence rates systematically biased our findings.
In conclusion, we found a moderate degree of chronic sleep restriction in interns performing extended overnight shifts without mandatory nap periods as well as significantly reduced levels of alertness in the morning after on-call nights that need to be mitigated. Due to the lack of safety outcomes in this study, it is unclear whether the observed levels of acute and chronic sleep loss in interns and the associated decrements in alertness also affected physician and patient safety, or whether they were offset by supervision, increased continuity of care, and more educational opportunities. Future studies are needed to determine whether frequent transitions in and out of a night shift (as currently practiced by interns under the 2011 ACGME rules) which challenge circadian timing are superior in mitigating the effects of acute and chronic sleep loss on alertness and physician and patient safety compared to extended overnight shifts with no protected sleep periods.
SUPPLEMENTARY MATERIAL
Supplementary data are available at SLEEP online.
FUNDING
This work was funded by Veterans Health Administration Health Services Research and Development grant EDU 08-429. Drs. MB and DFD were also funded through the National Institutes of Health grant NR004281 and by the National Space Biomedical Research Institute (NSBRI) through NASA NCC 9–58.
DISCLOSURE STATEMENT
There are no known financial conflicts of interest among any of the authors including but not limited to employment/affiliation, all grants or funding, honoraria, paid consultancies, expert testimony, stock ownership or options, and patents filed, received or pending. Dr. DFD served as a committee member on the 2008 IOM report. Dr. KGV served as an unpaid member of the ACGME Committee on Innovations from 2005 to 2009. We thank Jessica Dine, Ilene Rosen, Karen Warburton, and Daniel Mollicone for their assistance in conducting the study.
Supplementary Material
ACKNOWLEDGMENTS
Dr. MB confirms that everyone who contributed significantly to the work was listed in the acknowledgements. Dr. MB had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Off-label or investigational use: N/A. Registration: At clinicaltrials.gov as A Randomized Control Trial of Mandatory Naps for Physicians in Training, ID # NCT00874510. This work was performed at the University of Pennsylvania, Philadelphia, PA.
REFERENCES
- 1. Barger LK, Cade BE, Ayas NT, et al. ; Harvard Work Hours, Health, and Safety Group. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005; 352(2): 125–134. [DOI] [PubMed] [Google Scholar]
- 2. Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006; 3(12): e487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006; 296(9): 1055–1062. [DOI] [PubMed] [Google Scholar]
- 4. Lockley SW, Landrigan CP, Barger LK, Czeisler CA. When policy meets physiology: the challenge of reducing resident work hours. Clin Orthop Relat Res. 2006; 449: 116–127. [DOI] [PubMed] [Google Scholar]
- 5. Ulmer C, Wolman DM, Johns MME. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: National Academies Press; 2008 [PubMed] [Google Scholar]
- 6. Desai SV, Feldman L, Brown L, et al. Effect of the 2011 vs 2003 duty hour regulation-compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013; 173(8): 649–655. [DOI] [PubMed] [Google Scholar]
- 7. Levine AC, Adusumilli J, Landrigan CP. Effects of reducing or eliminating resident work shifts over 16 hours: a systematic review. Sleep. 2010; 33(8): 1043–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Spellberg B, Sue D, Chang D, Witt M. Change in intern calls at night after a work hour restriction process change. JAMA Intern Med. 2013; 173(8): 707–709; discussion 663. [DOI] [PubMed] [Google Scholar]
- 9. Barger LK, Lockley SW, Rajaratnam SM, Landrigan CP. Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions. Curr Neurol Neurosci Rep. 2009; 9(2): 155–164. [DOI] [PubMed] [Google Scholar]
- 10. Sen S, Kranzler HR, Didwania AK, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013; 173(8): 657–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Reed DA, Fletcher KE, Arora VM. Systematic review: association of shift length, protected sleep time, and night float with patient care, residents’ health, and education. Ann Intern Med. 2010; 153(12): 829–842. [DOI] [PubMed] [Google Scholar]
- 12. Volpp KG, Shea JA, Small DS, et al. Effect of a protected sleep period on hours slept during extended overnight in-hospital duty hours among medical interns: a randomized trial. JAMA. 2012; 308(21): 2208–2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shea JA, Dinges DF, Small DS, et al. A randomized trial of a three-hour protected nap period in a medicine training program: sleep, alertness, and patient outcomes. Acad Med. 2014; 89(3): 452–459. [DOI] [PubMed] [Google Scholar]
- 14. Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003; 26(3): 342–392. [DOI] [PubMed] [Google Scholar]
- 15. Malmberg B, Kecklund G, Karlson B, Persson R, Flisberg P, Ørbaek P. Sleep and recovery in physicians on night call: a longitudinal field study. BMC Health Serv Res. 2010; 10: 239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Arora V, Dunphy C, Chang VY, Ahmad F, Humphrey HJ, Meltzer D. The effects of on-duty napping on intern sleep time and fatigue. Ann Intern Med. 2006; 144(11): 792–798. [DOI] [PubMed] [Google Scholar]
- 17. Basner M, Mollicone D, Dinges DF. Validity and sensitivity of a brief Psychomotor Vigilance Test (PVT-B) to total and partial sleep deprivation. Acta Astronaut. 2011; 69(11–12): 949–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Basner M, Rubinstein J. Fitness for duty: a 3-minute version of the Psychomotor Vigilance Test predicts fatigue-related declines in luggage-screening performance. J Occup Environ Med. 2011; 53(10): 1146–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Basner M, Dinges DF. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep. 2011; 34(5): 581–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Basner M, Mcguire S, Goel N, Rao H, Dinges DF. A new likelihood ratio metric for the psychomotor vigilance test and its sensitivity to sleep loss. J Sleep Res. 2015; 24(6): 702–713. [DOI] [PubMed] [Google Scholar]
- 21. Akerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990; 52(1–2): 29–37. [DOI] [PubMed] [Google Scholar]
- 22. Ibrahim JG, Molenberghs G. Missing data methods in longitudinal studies: a review. Test (Madr). 2009; 18(1): 1–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jewett ME, Wyatt JK, Ritz-De Cecco A, Khalsa SB, Dijk DJ, Czeisler CA. Time course of sleep inertia dissipation in human performance and alertness. J Sleep Res. 1999; 8(1): 1–8. [DOI] [PubMed] [Google Scholar]
- 24. Zhou X, Ferguson SA, Matthews RW, et al. Mismatch between subjective alertness and objective performance under sleep restriction is greatest during the biological night. J Sleep Res. 2012; 21(1): 40–49. [DOI] [PubMed] [Google Scholar]
- 25. Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003; 26(2): 117–126. [DOI] [PubMed] [Google Scholar]
- 26. Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003; 12(1): 1–12. [DOI] [PubMed] [Google Scholar]
- 27. Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American academy of sleep medicine and sleep research society. Sleep. 2015; 38(6): 843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McCormick F, Kadzielski J, Landrigan CP, Evans B, Herndon JH, Rubash HE. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg. 2012; 147(5): 430–435. [DOI] [PubMed] [Google Scholar]
- 29. Arora VM, Georgitis E, Woodruff JN, Humphrey HJ, Meltzer D. Improving sleep hygiene of medical interns: can the sleep, alertness, and fatigue education in residency program help? Arch Intern Med. 2007; 167(16): 1738–1744. [DOI] [PubMed] [Google Scholar]
- 30. Amirian I, Andersen LT, Rosenberg J, Gögenur I. Working night shifts affects surgeons’ biological rhythm. Am J Surg. 2015; 210(2): 389–395. [DOI] [PubMed] [Google Scholar]
- 31. Anderson C, Sullivan JP, Flynn-Evans EE, Cade BE, Czeisler CA, Lockley SW. Deterioration of neurobehavioral performance in resident physicians during repeated exposure to extended duration work shifts. Sleep. 2012; 35(8): 1137–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004; 351(18): 1829–1837. [DOI] [PubMed] [Google Scholar]
- 33. Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature. 1997; 388(6639): 235. [DOI] [PubMed] [Google Scholar]
- 34. Maruff P, Falleti MG, Collie A, Darby D, McStephen M. Fatigue-related impairment in the speed, accuracy and variability of psychomotor performance: comparison with blood alcohol levels. J Sleep Res. 2005; 14(1): 21–27. [DOI] [PubMed] [Google Scholar]
- 35. Milner CE, Cote KA. Benefits of napping in healthy adults: impact of nap length, time of day, age, and experience with napping. J Sleep Res. 2009; 18(2): 272–281. [DOI] [PubMed] [Google Scholar]
- 36. Takahashi M. The role of prescribed napping in sleep medicine. Sleep Med Rev. 2003; 7(3): 227–235. [DOI] [PubMed] [Google Scholar]
- 37. Dinges DF, Whitehouse WG, Orne EC, Orne MT. The benefits of a nap during prolonged work and wakefulness. Work Stress 1988; 2(2): 139–153. [Google Scholar]
- 38. Mollicone DJ, Van Dongen HP, Rogers NL, Dinges DF. Response surface mapping of neurobehavioral performance: testing the feasibility of split sleep schedules for space operations. Acta Astronaut. 2008; 63(7–10): 833–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mollicone DJ, van Dongen HPA, Dinges DF. Optimizing sleep/wake schedules in space: Sleep during chronic nocturnal sleep restriction with and without diurnal naps. Acta Astronaut. 2007; 60 (4–7): 354–361. [Google Scholar]
- 40. Dinges DF, Orne MT, Whitehouse WG, Orne EC. Temporal placement of a nap for alertness: contributions of circadian phase and prior wakefulness. Sleep. 1987; 10(4): 313–329. [PubMed] [Google Scholar]
- 41. Van Dongen HP, Price NJ, Mullington JM, Szuba MP, Kapoor SC, Dinges DF. Caffeine eliminates psychomotor vigilance deficits from sleep inertia. Sleep. 2001; 24(7): 813–819. [DOI] [PubMed] [Google Scholar]
- 42. Hayashi M, Masuda A, Hori T. The alerting effects of caffeine, bright light and face washing after a short daytime nap. Clin Neurophysiol. 2003; 114(12): 2268–2278. [DOI] [PubMed] [Google Scholar]
- 43. Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004; 351(18): 1838–1848. [DOI] [PubMed] [Google Scholar]
- 44. Klerman EB, Beckett SA, Landrigan CP. Applying mathematical models to predict resident physician performance and alertness on traditional and novel work schedules. BMC Med Educ. 2016; 16(1): 239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Balkin TJ, Bliese PD, Belenky G, et al. Comparative utility of instruments for monitoring sleepiness-related performance decrements in the operational environment. J Sleep Res. 2004; 13(3): 219–227. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.