Abstract
Introduction
We reviewed the safety and effectiveness of our hospital’s urologic telemedicine (TM) program that has been utilized for the Iowa prisoner population for over a decade.
Methods
A retrospective review of TM visits of male prisoners from 2007 to 2014 was performed. Effectiveness of TM visits was assessed by 1) concordance of TM and in-person diagnoses, 2) compliance with radiologic and medication orders and 3) in-person visits saved with TM. Safety was assessed by analyzing the number of patients in which an ED visit was required after TM visit and missed or delayed cases of malignancy. Estimates were then made of the number of patients that could safely be managed with TM alone.
Results
The most common diagnosis was voiding dysfunction (24%) followed by genitourinary pain (23%). Diagnoses were concordant in 90% of patients; compliance was high (radiology 91%, medications 89%); in-person visits were estimated to be saved in 80-94%. No men required peri-TM ED visits and no cases of malignancy were missed in the population that returned for an in-person visit. We estimated that over 50% of urologic complaints in this cohort could have been managed with TM alone.
Conclusions
TM was shown to be a safe and effective method to provide general urologic care that obviated the initial in-person visits in nearly 90% of patients. It is likely that TM could safely replace in-person visits for many urologic conditions, especially in younger men and those in which access to specialized care may be limited.
Keywords: telemedicine, prisoners, cost-benefit analysis
Introduction
As the U.S. population continues to age, the need for urologists has never been greater. However, due to a multitude of factors, including a relatively high rate of retirement1, 2 and low rate of training for urologists, the number of urologists per capita continues to decline.2 As of 2013, there were 3.09 urologists per 100,000 population,3 decreasing from 3.18 in 20104 and representing the lowest per capita since 1981.1 Patients in rural U.S. areas already have decreased access to healthcare,5-11 including urologic care. A recent survey of urologists revealed that those under the age of 45 were three times less likely to practice in nonmetropolitan or rural counties.12
Telemedicine (TM) has been used and studied in other medical disciplines as a means to reach access-poor populations, including those in rural settings. There are many potential advantages to TM for both patients and providers, including a significant decrease in both direct and indirect medical costs.13 However, the inability to perform a physical exam and persistent concerns about the inability to bill and receive reimbursement for the provided care have thus far limited the widespread use of TM in surgical subspecialties such as urology.
The University of Iowa Hospitals and Clinics (UIHC) provides medical care to our state’s prison population and because of many logistical concerns with caring for this unique population, much of the initial, non-emergent urologic care is provided using TM. The purpose of this study was to review the urologic TM program at UIHC. We hypothesized that TM urologic care can improve access in this underserved population without compromising safety or effectiveness.
Materials and Methods
Background
TM care for our state’s prison population has been conducted by a urologic advanced practice provider (APP) since 2000 and has been performed using both teleconferencing (i.e. phone only) and videoconferencing. In most cases, a primary care provider at the prison has been available to perform a basic physical examination before or during the TM visit as requested by the urology APP. A staff urologist is also immediately available on call, typically for urologic complaints or conditions that might be considered urgent by the APP and/or the prison health care worker.
Importantly, the overarching goal of these TM consultations has not been to completely replace in-person visits, but rather to triage the patient’s complaint to maximize the efficiency and effectiveness of the eventual in-person visit. Thus, a major tenet of our TM care is to order the appropriate radiographic and laboratory tests to be completed prior to an in-person visit and minimize travel of the prisoner to and from the prison.
Study Population
An IRB-approved, retrospective review of the medical records of all Iowa male prison urology patients initially evaluated with TM at our institution from January 2007 to July 2014 was performed. This start date was chosen as it represented the first year (January 2007) in which the EPIC electronic medical record was fully integrated into our healthcare system, thus full records, including lab and medication orders, were immediately available.
Study Methodology
We first analyzed the specifics of the TM visit only, including urologic complaints provided to the APP, the eventual diagnosis (or differential diagnosis) provided by the APP to the patient, management suggested including diagnostic tests ordered, medications and/or treatments provided, and suggested follow-up.
The effectiveness of the TM visits was determined by analyzing the men that were eventually seen for in-person visits by evaluating two separate variables: 1) concordance of the TM diagnosis (or differential diagnosis) with the diagnosis provided at the in-person visit and 2) compliance with radiologic and pharmacologic orders suggested during the TM visit prior to in-person visit.
The efficiency of TM was determined by analyzing the number of in-person visits obviated by utilizing TM, which was determined by identifying patients who met one or more of the following criteria: 1) orders placed at the time of the TM visit were completed prior to the in-person visit, 2) follow-up was not required after the initial TM consultation (i.e., APP discharged patient from further care) or 3) additional TM visits were performed prior to or in place of a follow-up in-person visit to evaluate initial care provided and/or progression of the chief complaint.
We then estimated the number of men that could have been managed with TM alone by determining which of our patients met one or more of the following criteria: 1) the patient’s urologic condition was completely and successfully managed by TM (i.e., sufficient assessment and plan made during TM visit alone), 2) a urologic diagnostic procedure (e.g. cystoscopy, urodynamics, or biopsy) was not required, or 3) surgery or other interventional treatment was not required. The determination that the patient could be managed with TM alone also assumed the following: 1) radiology and lab testing can be performed locally, 2) radiology and lab results can be read remotely by the APP/urologist, and 3) given remote access to radiology and face-to-face video conference capabilities, a primary care provider’s physical examination is deemed safe and sufficient.
Statistical Analysis
All data were stored in a REDCap® database. Descriptive statistics (mean, +/− standard deviations) were performed within the REDCap® database platform as well as with Microsoft Excel 2013 (Redwood, WA) after transferring spreadsheets from the REDCap software.
Results
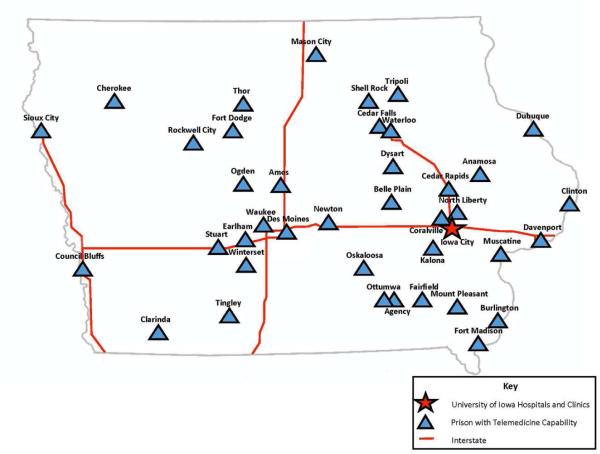
A total of 376 unique and 154 repeat TM encounters occurred during the study time period. Mean patient age was 42.3 (±13.2 years). Prison locations relative to our institution are shown in Figure 1, with driving distances from the prison to our hospital ranging from 3 to 311 miles and averaging 186 (±151) miles.
Figure 1.
Locations of Iowa prisons participating in TM.
Initial Telemedicine Visit
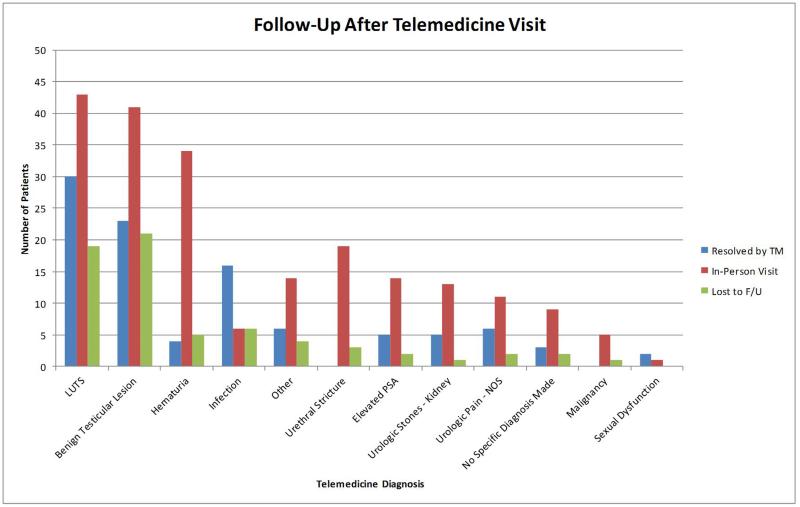
The most common chief complaint of the male prisoners prompting the TM consultation was voiding/storage complaint (53% of patients), followed by genitourinary pain (40%), and hematuria (20%). The most common TM diagnoses made at the end of the consultation were benign prostatic hyperplasia/lower urinary tract symptoms (BPH/LUTS; 24%), benign testicular lesions (23%), and hematuria (11%; Table 1). Orders placed after the TM visit were most commonly radiologic (47%), followed by medication (40%), and labs (38%; Table 1). Follow-up appointments were scheduled after 87% of initial TM visits, of which 50% were to be in-person visits at our clinic and 37% by TM only (See Table 1 and Figure 2 for actual follow-up).
Table 1.
All telemedicine encounters
| Demographics | Ordered Tests at TM | Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| TM Diagnosis | n | Age (±SD) | Radiology | Meds | Labs |
Resolved
by TM |
In-person
Visit |
Lost to
F/U |
Estimated In-
person Visit Not Required |
|
| |||||||||
| Overall | 376 (100%) | 42.3 (13.2) | 178 (47%) | 152 (40%) | 144 (38%) | 100 (27%) | 210 (56%) | 66 (18%) | 195 (52%) |
| LUTS | 92 (24%) | 46.7 (13.0) | 14 (15%) | 62 (67%) | 36 (39%) | 30 (33%) | 43 (47%) | 19 (21%) | 46 (50%) |
| Benign Testicular Lesion | 85 (23%) | 36.0 (10.1) | 64 (75%) | 15 (18%) | 12 (14%) | 23 (27%) | 41 (48%) | 21 (25%) | 64 (75%) |
| Hematuria | 43 (11%) | 44.9 (13.9) | 38 (88%) | 5 (12%) | 23 (53%) | 4 (9%) | 34 (79%) | 5 (12%) | 6 (14%) |
| Infection | 28 (7%) | 43.0 (11.4) | 11 (39%) | 25 (89%) | 9 (32%) | 16 (57%) | 6 (21%) | 6 (21%) | 24 (86%) |
| Other | 24 (6%) | 36.2 (15.2) | 7 (29%) | 9 (38%) | 6 (25%) | 6 (25%) | 14 (58%) | 4 (17%) | 12 (50%) |
| Urethral Stricture | 22 (6%) | 37.8 (9.3) | 9 (41%) | 7 (32%) | 10 (45%) | 0 (0%) | 19 (86%) | 3 (14%) | 4 (18%) |
| Elevated PSA | 21 (6%) | 60.0 (8.5) | 1 (5%) | 14 (67%) | 20 (95%) | 5 (24%) | 14 (67%) | 2 (10%) | 6 (29%) |
| Urologic Stones - Kidney | 19 (5%) | 43.3 (10.1) | 15 (79%) | 3 (16%) | 12 (63%) | 5 (26%) | 13 (68%) | 1 (5%) | 6 (32%) |
| Urologic Pain - NOS | 19 (5%) | 33.4 (12.7) | 11 (58%) | 5 (26%) | 3 (16%) | 6 (32%) | 11 (58%) | 2 (11%) | 15 (79%) |
| No Diagnosis Made | 14 (4%) | 43.4 (12.3) | 5 (36%) | 6 (43%) | 9 (64%) | 3 (21%) | 9 (64%) | 2 (14%) | 9 (64%) |
| Malignancy | 6 (2%) | 49.4 (13.3) | 3 (50%) | 0 (0%) | 4 (67%) | 0 (0%) | 5 (83%) | 1 (17%) | 1 (17%) |
| Sexual Dysfunction | 3 (1%) | 33.3 (7.6) | 0 (0%) | 1 (33%) | 0 (0%) | 2 (67%) | 1 (33%) | 0 (0%) | 2 (67%) |
Figure 2.
Follow-up after the TM visit.
Effectiveness of Telemedicine
Of the 376 men evaluated via TM, 210 (56%) were eventually seen in our clinic. In these patients, the TM and in-person visit diagnoses were concordant 90% of the time (Table 2). Of the 22 diagnoses that were not concordant, 6 (27%) were assumed to have a recurrence of urethral stricture based on past medical history of stricture that was not found upon objective investigation and 6 (27%) patients diagnosed with BPH/LUTS via TM were found to have a more specific diagnosis upon further work-up, urethral stricture being the most common. Importantly, there were no discordant diagnoses of genitourinary malignancy.
Table 2.
Telemedicine patients who were subsequently seen in an in-person clinic visit
|
Compliance with TM Orders
|
||||||
|---|---|---|---|---|---|---|
| In-person Visit Diagnosis | n |
TM Dx was
Correct |
Radiology | Meds |
Return Visit
Scheduled |
Surgery
Scheduled |
|
| ||||||
| Overall | 210 (56%) | 188 (90%) | 99 (91%) | 68 (89%) | 86 (41%) | 52 (25%) |
| LUTS | 42 (20%) | 38 (90%) | 6 (60%) | 26 (96%) | 24 (57%) | 6 (14%) |
| Benign Testicular Lesion | 39 (19%) | 38 (97%) | 25 (89%) | 4 (80%) | 12 (31%) | 9 (23%) |
| Hematuria | 28 (13%) | 27 (96%) | 24 (96%) | 3 (75%) | 20 (71%) | 1 (4%) |
| No Diagnosis Made | 16 (8%) | 9 (56%) | 5 (83%) | 6 (100%) | 3 (19%) | 0 (0%) |
| Other | 15 (7%) | 12 (80%) | 4 (100%) | 5 (83%) | 4 (27%) | 4 (27%) |
| Urologic Stones - Kidney | 15 (7%) | 15 (100%) | 14 (100%) | 2 (50%) | 5 (33%) | 9 (60%) |
| Malignancy | 13 (6%) | 12 (92%) | 6 (100%) | 4 (100%) | 5 (38%) | 8 (62%) |
| Urologic Pain - NOS | 12 (6%) | 10 (83%) | 8 (100%) | 3 (100%) | 1 (8%) | 1 (8%) |
| Urethral Stricture | 11 (5%) | 10 (91%) | 1 (50%) | 3 (100%) | 3 (27%) | 8 (73%) |
| Infection | 10 (5%) | 8 (80%) | 5 (100%) | 7 (78%) | 5 (50%) | 1 (10%) |
| Elevated PSA | 7 (3%) | 7 (100%) | 0 (0%) | 4 (100%) | 3 (43%) | 5 (71%) |
| Sexual Dysfunction | 2 (1%) | 2 (100%) | 1 (100%) | 1 (100%) | 1 (50%) | 0 (0%) |
Compliance with both radiologic (91%) and medication (89%) orders from the TM visit was high.
Efficiency of Telemedicine
We estimated that TM led to 80% of our patients requiring at least one fewer in-person visit than would have otherwise been necessary to manage the urologic problem. Had TM been fully utilized (i.e. labs/radiology orders been fully executed), we estimated that over 94% could have saved a visit. Given the relatively young and healthy prison population we were managing with TM, it was estimated that under ideal circumstances, 52% of the patient population could have been safely managed by TM alone.
Discussion
Our study objective was to determine the efficiency and effectiveness of telemedicine for urologic care in our state’s male prison population. Overall, we found that a large percentage of the urologic complaints were voiding dysfunction and urologic pain conditions, most commonly testicular pain. The correct urologic diagnosis was reached by our APPs administering the care in over 90% of the cases utilizing TM alone, highlighting the safety of the program for the majority of general urologic conditions. Furthermore, 80% of patients were saved at least one trip to our institution for urologic care by using TM, leading to presumed decreases in both direct and indirect costs. Collectively, these findings demonstrate how TM might safely become a way to address disparities in urologic access in other underserved, and access-poor populations.
Telemedicine in Practice
Telemedicine has been utilized for over 40 years and in many specialties. It has commonly been used to transmit images in radiology14, 15 and pathology16-18, but has more recently been used for real-time patient-physician telephone and video-conferencing. In urology, TM has been shown to be effective for rounding on inpatients.19-21 TM has been used for surgical applications such as preoperative evaluation22 and postoperative follow-up.23 Hwa and Wren reported that a postoperative telephone call by a physician assistant effectively replaced postoperative physician office visits in ambulatory surgery patients following elective open hernia repair or laparoscopic cholecystectomy.24 They noted that the use of this program led to the opening of 110 clinic slots during a 10-month period, which decreased wait time for new patients. It has been shown that TM can increase access to patients in rural areas.25 For patients in rural areas, TM directly saves time and money by decreasing unnecessary travel.13
Improving Access to Care with Telemedicine
We have previously addressed improving access to urologic care in Iowa’s rural populations by utilizing physician outreach clinics.26 These clinics serve a similar purpose as TM clinics as they make the visits more convenient for the patient, with the physician travelling directly to the patient. Our group noted that the percentage of patients that had to travel less than 30 minutes to their urology appointment in Iowa increased from 57% to 84% with the use of outreach clinics, improving the patient’s access to care. However, this improved access was at the expense of nearly 20,400 miles driven by the state’s urologists every month. In addition, these clinics were generally less efficient (i.e. fewer patients were seen secondary to physician travel time), which means that while the distance to access may have improved for the individual rural urology patient, overall access was effectively diminished with fewer overall urology clinic visits in the state.
Telemedicine can improve access to underserved areas by eliminating travel time and associated costs of both the provider and the patient.13 Importantly, attitudes about how healthcare is provided in this country are changing. According to a recent survey by Cisco, 74% of patients surveyed prioritize access to health care over in-person interactions with health care providers. Furthermore, 70% said they were comfortable communicating with providers via text, email, or video, in lieu of an in-office visit.27 Acceptance of TM care has been shown in numerous scientific studies as well.13, 22 Most recently, a study comparing the satisfaction of urology patients seen by TM vs. those seen by in-person clinic visits showed higher satisfaction and preference among those seen by TM, primarily due to travel concerns.28
Telemedicine seems particularly well suited for triage of new patients. In the population studied, we estimated that 80-94% of initial in-person visits could have been replaced with TM, during which imaging, labs, and medications could be ordered and completed prior to an in-person visit. This approach is especially attractive for rural patients and can minimize their travel burden.
Assessing the Safety of Telemedicine for Urologic Care
One of the biggest concerns that patients and providers have with TM is the fear of a missed or delayed diagnosis by not having the ability to perform a physical exam. One option to mitigate this concern is to have a primary care provider present during the TM encounter to perform a physical exam at the direction of the specialist physician. In a study that evaluated this method of performing the physical exam for general surgery TM consults, surgeons felt that 96% of physical examinations performed by a primary care provider were reliable.22
Overall, the lack of performance of the physical exam by the urology APP did not appear to limit the effectiveness of the visits, as determined by the concordance of diagnoses. This may be in part because in most cases, a skilled provider (physician or APP) was available at the prison to perform any necessary exams, and when a more directed exam was required, they were asked to return to our clinic. Furthermore, in most cases where physical exam findings are concerning to the patient and/or referring provider (e.g. testicular mass), the exam required a confirmatory radiologic study that was reviewed by our urologic providers at the time of their in-person visit.
Telemedicine as a Cost-effective Means to Providing Urologic Care
This study did not directly address direct or indirect costs associated with our TM program, though we estimated that nearly 94% of patients could save at least one visit by using TM for the initial urology consultation, decreasing both the direct costs of travel and guard salary in the prison population and the indirect costs of potential loss of income due to missed work in the non-prison population. A prior study estimated that national implementation of TM in correctional facilities could save over 583,000 visits and over $270 million each year, saving almost 75% of total visits and almost 60% of current annual cost.29 Another study of urologic TM in the VA system showed an average direct cost (travel) savings of $67 and an indirect cost (lost income) savings of $126 per visit through the use of TM.13 With decreasing costs of technology in general, the cost of TM system implementation continues to decrease, which will make TM an increasingly cost-effective means of providing urologic care. Incorporation of remote patient-reported outcomes questionnaires into TM practice may also improve its ability to monitor longitudinally.
Study Limitations
This study was limited by its retrospective design, which affected our ability to fully address concerns with lack of physical exam as nearly 50% of patients seen by TM were not seen during an in-person visit to fully validate TM assessments. The design also limited our ability to assess the appropriateness of radiologic and imaging orders made by the APPs. Second, while this study estimates the potential for TM to replace in-person visits, the goal of the TM program at our institution was not to replace in-person visits, but to maximize the effectiveness of in-person visits. Third, while TM is purported to be a cost-effective approach to addressing access concerns, we did not do a full cost-effectiveness study. Finally, this study analyzed a younger cohort of men in prison, with an average age of 42.3 years, which is much lower than that of the patients seen in most urology clinics. Therefore, many urologic conditions that are more common in older populations were not commonly seen in this young sample and thus, estimates of compliance, safety and effectiveness may only be applicable to a younger male population. Furthermore, the unique circumstances with freedom impairment that patients face while in prison may alter presentation pathologies and compliance with prescribed medication and radiologic orders.
Conclusions
We found TM to be a safe and effective method to increase access to urologic care. Telemedicine effectively replaced 80% of initial visits in this access-poor population, with the potential to save over 90% of initial visits if all TM orders are followed. We estimated that with refined, prospective protocols, over 50% of the patients in this younger male population might have been safely managed by TM alone. Continued expansion of TM use in urology appears safe, and assuming access to local radiologic and laboratory care, has potential to increase access to specialized urologic care in areas where providing this care may be otherwise too cost-prohibitive.
Acknowledgments
This work was supported by American Urological Association Data Grant, NIH Institutional Training Grant T35-HL007485-36.
Abbreviations
- TM
telemedicine
- APP
advanced practice provider
- LUTS
lower urinary tract symptoms
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: All authors declare no financial conflicts of interest.
References
- 1.Pruthi RS, Neuwahl S, Nielsen ME, et al. Recent trends in the urology workforce in the United States. Urology. 2013;82:987. doi: 10.1016/j.urology.2013.04.080. [DOI] [PubMed] [Google Scholar]
- 2.Neuwahl S, Fraher E, et al. HPRI data tracks. Urology workforce trends. Bull Am Coll Surgeons. 2012;97:46. T. K. [PubMed] [Google Scholar]
- 3.American Association of Medical Colleges. Center for Workforce Studies 2014 Physician Specialty Data Book [Google Scholar]
- 4.American Association of Medical Colleges Center for Workforce Studies 2012 Physician Specialty Data Book [Google Scholar]
- 5.Gore JL, Litwin MS, Lai J, et al. Use of radical cystectomy for patients with invasive bladder cancer. J Natl Cancer Inst. 2010;102:802. doi: 10.1093/jnci/djq121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finlayson SR, Birkmeyer JD, Tosteson AN, et al. Patient preferences for location of care: implications for regionalization. Med Care. 1999;37:204. doi: 10.1097/00005650-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Tropman SE, Hatzell T, Paskett E, et al. Colon cancer treatment in rural North and South Carolina. Cancer Detect Prev. 1999;23:428. doi: 10.1046/j.1525-1500.1999.99042.x. [DOI] [PubMed] [Google Scholar]
- 8.Tropman SE, Ricketts TC, Paskett E, et al. Rural breast cancer treatment: evidence from the Reaching Communities for Cancer Care (REACH) project. Breast Cancer Res Treat. 1999;56:59. doi: 10.1023/a:1006279117650. [DOI] [PubMed] [Google Scholar]
- 9.Schroen AT, Brenin DR, Kelly MD, et al. Impact of patient distance to radiation therapy on mastectomy use in early-stage breast cancer patients. J Clin Oncol. 2005;23:7074. doi: 10.1200/JCO.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 10.Sankaranarayanan J, Watanabe-Galloway S, Sun J, et al. Age and rural residence effects on accessing colorectal cancer treatments: a registry study. Am J Manag Care. 2010;16:265. [PubMed] [Google Scholar]
- 11.Baldwin LM, Cai Y, Larson EH, et al. Access to cancer services for rural colorectal cancer patients. J Rural Health. 2008;24:390. doi: 10.1111/j.1748-0361.2008.00186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Odisho AY, Fradet V, Cooperberg MR, et al. Geographic distribution of urologists throughout the United States using a county level approach. J Urol. 2009;181:760. doi: 10.1016/j.juro.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 13.Chu S, Boxer R, Madison P, et al. Veterans Affairs Telemedicine: Bringing Urologic Care to Remote Clinics. Urology. 2015;86:255. doi: 10.1016/j.urology.2015.04.038. [DOI] [PubMed] [Google Scholar]
- 14.Zennaro F, Grosso D, Fascetta R, et al. Teleradiology for remote consultation using iPad improves the use of health system human resources for paediatric fractures: prospective controlled study in a tertiary care hospital in Italy. BMC Health Serv Res. 2014;14:327. doi: 10.1186/1472-6963-14-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Platts-Mills TF, Hendey GW, Ferguson B. Teleradiology interpretations of emergency department computed tomography scans. J Emerg Med. 2010;38:188. doi: 10.1016/j.jemermed.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 16.Izquierdo RE, Kasturi R, Khurana K, et al. Feasibility of immediate assessment of fine needle aspirates of thyroid nodules by telecytopathology. Endocr Pract. 2013;19:14. doi: 10.4158/EP11374.OR. [DOI] [PubMed] [Google Scholar]
- 17.Khurana KK, Rong R, Wang D, et al. Dynamic telecytopathology for on-site preliminary diagnosis of endoscopic ultrasound-guided fine needle aspiration of pancreatic masses. J Telemed Telecare. 2012;18:253. doi: 10.1258/jtt.2011.110706. [DOI] [PubMed] [Google Scholar]
- 18.Alsharif M, Carlo-Demovich J, Massey C, et al. Telecytopathology for immediate evaluation of fine-needle aspiration specimens. Cancer Cytopathol. 2010;118:119. doi: 10.1002/cncy.20074. [DOI] [PubMed] [Google Scholar]
- 19.Ellison LM, Nguyen M, Fabrizio MD, et al. Postoperative robotic telerounding: a multicenter randomized assessment of patient outcomes and satisfaction. Arch Surg. 2007;142:1177. doi: 10.1001/archsurg.142.12.1177. [DOI] [PubMed] [Google Scholar]
- 20.Kau EL, Baranda DT, Hain P, et al. Video rounding system: a pilot study in patient care. J Endourol. 2008;22:1179. doi: 10.1089/end.2008.0045. [DOI] [PubMed] [Google Scholar]
- 21.Kaczmarek BF, Trinh QD, Menon M, et al. Tablet telerounding. Urology. 2012;80:1383. doi: 10.1016/j.urology.2012.06.060. [DOI] [PubMed] [Google Scholar]
- 22.Aarnio P, Rudenberg H, Ellonen M, et al. User satisfaction with teleconsultations for surgery. J Telemed Telecare. 2000;6:237. doi: 10.1258/1357633001935301. [DOI] [PubMed] [Google Scholar]
- 23.Gunter RL, Chouinard S, Fernandes-Taylor S, et al. Current Use of Telemedicine for Post-Discharge Surgical Care: A Systematic Review. J Am Coll Surg. 2016 doi: 10.1016/j.jamcollsurg.2016.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148:823. doi: 10.1001/jamasurg.2013.2672. [DOI] [PubMed] [Google Scholar]
- 25.Kruse CS, Bouffard S, Dougherty M, et al. Telemedicine Use in Rural Native American Communities in the Era of the ACA: a Systematic Literature Review. J Med Syst. 2016;40:145. doi: 10.1007/s10916-016-0503-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uhlman MA, Gruca TS, Tracy R, et al. Improving access to urologic care for rural populations through outreach clinics. Urology. 2013;82:1272. doi: 10.1016/j.urology.2013.08.053. [DOI] [PubMed] [Google Scholar]
- 27.Cisco Study Reveals 74 Percent of Consumers Open to Virtual Doctor Visit. Cisco Newsroom; [Google Scholar]
- 28.Safir IJ, Gabale S, David SA, et al. Implementation of a Tele-urology Program for Outpatient Hematuria Referrals: Initial Results and Patient Satisfaction. Urology. 2016 doi: 10.1016/j.urology.2016.04.066. [DOI] [PubMed] [Google Scholar]
- 29.Pan E, Cusack C, Hook J, et al. The value of provider-to-provider telehealth. Telemed J E Health. 2008;14:446. doi: 10.1089/tmj.2008.0017. [DOI] [PubMed] [Google Scholar]