Abstract
The objective of this article is to systematically review the evidence on the effectiveness of vestibular rehabilitation (VR) in patients with benign paroxysmal positional vertigo (BPPV). Relevant published studies about VR in BPPV were searched in PubMed, Google Scholar and Ovid using various keywords. We included trials that were available in the English language and did not apply publication year or publication status restrictions. Studies based on the VR in other peripheral and/or central balance disorders are excluded. Primary outcome was the effect on vertigo attacks and balance. Of 42 identified trials, only 12 trials fulfilled our inclusion criteria and were included in this review. Three of them investigated the role of VR in patients with BPPV comparing with no treatment, two of them evaluated the efficacy of VR versus medications, seven of them have highlighted the benefits of the VR alone or in combination with canalith repositioning procedure (CRP) compared to CRP alone. The studies differed in type of intervention, type of outcome and follow-up time. VR improves balance control, promoting visual stabilization with head movements, improving vestibular–visual interaction during head movement and expanding static and dynamic posture stability. CRP and VR seem to have a synergic effect in patients with BPPV, especially in elderly patients. VR does not reduce the recurrence rate, but it seems to reduce the unpleasantness. So VR can substitute CRP when spine comorbidities contraindicate CRP and can reduce the uptake of anti-vertigo drugs post CRP. Further studies are needed to confirm these encouraging results.
Keywords: benign paroxysmal positional vertigo, systematic review, vertigo, vestibular rehabilitation
Introduction
Benign paroxysmal positional vertigo (BPPV) has been recognized as the most common vestibular disorders and was first described by Bàrany in 1921, but the term was coined in 1952 by Dix and Hallpike.
BPPV is a clinical syndrome characterized by brief (<40 s) rotating vertigo triggered by changes in head position with respect to gravity, without hearing loss and/or tinnitus. The vertigo sometimes is associated with nausea, vomiting, pallor and/or sweating; the nystagmus typically has a latency of few seconds and is of limited duration (10–20 s), transient and fatigable.
The lifetime prevalence of BPPV has been reported to 10%.1 The incidence of BPPV increases with age; it is known that 9% of geriatric patients had an episode that interferes with the quality of life and increased risk of falling and depression.2
The exact aetiology of BPPV is still debatable: the most of BPPV is idiopathic (58%) in nature; other potential causes are head trauma (6%–18%) and inner-ear disease including infection, inflammation or dysfunction of inner ear microcirculation (3%–9%).3
The disorder generally involves two topographical variants:
BPPV of the posterior semicircular canal (PSC-BPPV);
BPPV of the horizontal semicircular canal (HSC-BPPV).
PSC-BPPV is more common than HSC-BPPV and constituted approximately 85%–95% of BPPV.4 The duration, frequency and intensity of BPPV symptoms are quite variable, and it is possible a spontaneous recovery.5
The BPPV diagnosis is based on history and physical examination. It is important to observe nystagmus carefully and to recognize manifestations that accompany other diagnoses (unilateral hearing loss, tinnitus, atypical nystagmus or other neurologic deficit).
Nowadays, canalith repositioning procedure (CRP) is the gold standard for the treatment of PSC-BPPV and for HSC-BPPV.6 Not rarely, regardless of the semicircular canal involved, the BPPV patients show, for some weeks after CRP, an increased postural instability especially in some static and dynamic conditions where there are altered proprioceptive input combined with altered or absent visual inputs.7 The decrease of postural control is associated with an increased risk of falls, fractures and other damage related to falls especially in older adults.8 For this ‘instability period’, repeated CRP could not be enough to reactivate or improve the postural control in BPPV patients, and some authors suggest vestibular suppressant drugs (diazepam, promethazine, etc.) or calcium antagonists (especially flunarizine), but such medical treatment is not always helpful and can sometimes be associated with side effects.9
The vestibular rehabilitation (VR) is a form of physical therapy using head and trunk movements and improves balance by developing vestibular system stimulation and central compensation:10 the Brandt-Daroff (B-D) and Cawthorne-Cooksey are the most common forms of VR exercises. The use of a customized VR therapy programme adapted to suit the specific needs of the individual was widely accepted in the 1990s, and it became the primary modality of treatment for patients with vestibular disorders.
Several studies have shown the effectiveness of VR on the balance;7 for this reason, its indication is not only in otorhinolaryngology but also in other branches of medicine, such as in neurology for the treatment of patients with multiple sclerosis.11
The main aims of VR are as follows:
To improve the visual–vestibular interaction and increase static and dynamic postural stability;
To contribute to an improvement in daily quality of life and a reduction in symptoms of dizziness and anxiety.6
Many authors, first of all Brandt and Darroff,12 Norrè and Beckers13 and McCabe,14 showed how VR could be useful in patients affected by BPPV.15 The aim of this review was to systematically search the potential role of VR in patients with BPPV.
Methods
Relevant published studies were searched in PubMed, Google Scholar and Ovid, using either the following keywords or, in case of PubMed database, Medical Subject Headings: (‘Benign paroxysmal positional vertigo’ or ‘BPPV’) AND (‘physical therapy modalities’ OR ‘exercise therapy’ OR ‘exercise’ OR ‘habituation exercises’ OR ‘rehabilitation’ OR vestibular rehabilitation) with no limit for the year of publication. Only studies in English, published in peer-reviewed journals, reporting data on the role of VR in BPPV were included. Literature reviews, technical notes, letters to editors and instructional course were excluded. The reference lists of the selected articles were fully and accurately reviewed to identify articles not included during the first electronic search. Studies that were based on the use of VR in overall peripheral and/or central balance vestibular disorder, acute vestibular disorders, VR after traumatic injuries are excluded. At the end of our selection process, 12 publications have been included (Figure 1).
Figure 1.
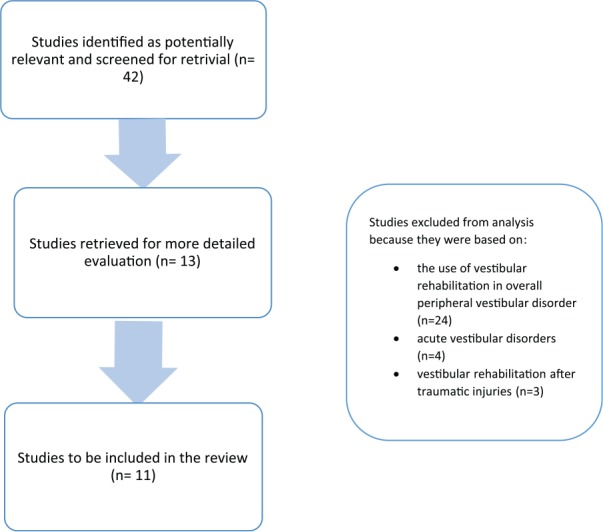
Flow chart of article research.
Results
A total of 12 publications, which investigated the role of VR, have been included in the present review, as reported in Table 1.
Table 1.
Included studies.
| Participants (male/female, age) | Type and duration of vestibular rehabilitation | Results | |
|---|---|---|---|
| VR vs no treatment | |||
| Norrè and Beckers13 | 40 patients (16 males/24 females). Mean age: 50.2 years (range: 20–80 years). 11 patients were over 60 years of age (4 males/7 females). |
Exercises, selected according to the results obtained by the VHT test battery, are executed actively and vigorously two or three sessions daily at home and repeated five times successively. | The cumulative percentages of cured cases increased from 27% to 93% for the total group. For patients older than 60 years, this progression was slower from 9% to 73%. |
| Banfield et al.16 | 25 patients Mean age of the group followed up was 53 (range: 26–80) years |
The exercise consists of seating the patient and then laying him on the affected side. Then patient returns to the upright position and the exercise is repeated. This exercise must be repeated three times a day for a month. | Good short-term response to treatment, recurrence in 76% of cases. 12 of 19 patients with recurrent symptoms have been performing the exercises on their own initiative. |
| Tanimoto et al.17 | 80 patients (55 women and 25 men). Mean age: 64 years |
Patients received illustrated instructions for self-treating manoeuvre. | The rates of resolution of both symptoms and nystagmus were 69% in the Epley-alone group and 88% in the self-treatment group. |
| VR versus medications | |||
| Fujino et al.18 | 61 patients divided. Group 1: 20 patients; Group 2: 21 patients; and Group 3: 20 patients Mean age – Group 1: 51.8 years; Group 2: 47 years; and Group 3: 53.6 years |
VT consists of Brandt-Daroff and Dix-Hallpike modified exercises. | The global rate of improvement is significantly improved in Groups 2 and 3 compared to Group 1 (62% in Group 2, 70% in Group 3 and only 30% in Group 1). |
| Kulcu et al.19 | 38 patients (10 males/28 females). Mean age: 46 years |
The exercise group was instructed in modified Cawthorne-Cooksey exercises six times a day for 4 weeks. Exercises were composed of a series of exercises that encourage head and eye movements. | There were significant differences between groups in the mean scores of the VDI and the VSS at the end of the study in favour of the exercise group. |
| VR vs CRP | |||
| Steenerson and Cronin20 | 40 patients – control group: 6 men and 14 women; treatment groups: 7 men and 13 women. Mean age: CRP group 53 years, VHT group 48 years and control group 51 years. |
VHT group patients were provided habituation movements. The second group of patients was treated with CRP as described by Epley. |
14 (82%) patients in the CRP group were symptom free after 3 months. In the VHT group, 63% of patients were symptom free at 3 months. |
| Soto Varela et al.21 | 106 patients Mean age of the group followed up was 55.5 (range: 18–77) years |
VR (Brandt-Daroff (B-D) habituations exercises) was performed at home three times daily until disappearance of symptoms. In Groups B and C, the manoeuvres were repeated weekly until the symptoms disappeared. | At the 1-week follow-up, similar cure rates were obtained with the Semont and Epley manoeuvre (74% and 71%, respectively), both cure rates being significantly higher than that obtained with B-D exercises (24%). |
| Angeli et al.22 | 47 patients (>70 years old) – control group: 9 men and 10 women; treatment group: 12 men and 16 women. Mean age: control group 74 years and treatment group 73 years. |
VR included particle-dispersing exercises and VHT. | CRP is more effective than no treatment, VR can be added to improve the results in the treatment of BPPV. |
| Chang et al.23 | 26 patients (15 females/11 males) Mean age: control group 54 years and experimental group 57 years. |
Subjects in the experimental group received an additional 40-min vestibular-stimulated exercise programme, three times a week for 4 weeks. The exercises included oculomotor exercises, repeated head movement exercises, balance training exercise and functional activities. |
Additional exercise training for patients with BVPP increased patients’ static and dynamic balance performance and enhanced functional gait ability. |
| Helminski et al.24 | 39 patients (11 males/28 females). Mean age: control group 64 years and treatment group 55 years. |
Subjects in treatment were trained in and instructed to perform two cycles of the self-CRP 1 time per day and were provided an illustrated handout and digital video disc of the exercises. | There was no significant difference in response to treatment. Of the 16 subjects where symptoms had recurred, 6 initiated self-treatment before evaluation in the clinic and treated themselves. 100% of these patients successfully resolved their symptoms by themselves. |
| Amor-Dorado et al.25 | 81 patients: 41 males/40 females Mean age: CRP group 58 years, B-D exercise group 60 years. |
Treatment B was based on B-D exercise, and it was self-performed domiciliary. | At Day 7, DHM was negative in 80.5% of the CRP treated patients and in 25% of those treated by B-D exercise. At Month 1: 92.7% in CRP vs 42.5% in the B-D exercise had a negative DHM. The recurrence rate at 48 months was 35.5% (15/41) in B-D exercise and 36.6% (9/31) in the CRP group. |
| Ribeiro et al.26 | 14 patients: 11 females/3 males. Mean age: experimental group 69 years and control group 73 years. |
VRT was performed twice a week, 50 min each, over a 12-week period. The balance VRT included oculomotor exercises, habituation exercises standing and dynamic balance training, along with lower-limb muscles strengthening |
No differences in dizziness, quality of life and standing balance. Significant differences were observed in dynamic balance measures between groups at 9 and 13 weeks. No significant differences in dizziness symptoms through VAS. |
VHT: vestibular habituation training; VR: vestibular rehabilitation; VSS: Vertigo Symptom Scale; VDI: Vertigo, Dizziness, Imbalance Questionnaire; CRP: canalith repositioning procedure; DHM: Dix-Hallpike manoeuvre.
Three of them investigated the role of VR in patients with BPPV comparing with no treatment, two of them evaluated the efficacy of VR versus medications and seven of them have highlighted the benefits of the VR alone or in combination with CRP compared to CRP alone.
Norrè and Beckers13 have proven the value of VR in elderly patients with BPPV. VR exercises consists of 19 manoeuvres (not specified) that patients should be executed actively and vigorously. The rehabilitation programme consists of two or three sessions per day repeated at home five times successively. These exercises stimulate the central adaptive mechanisms of compensation and habituation in order to recalibrate the central processing. Elderly patients treated by VR also showed very satisfying results, although the therapeutic effect developed somewhat slower than in the younger patients.
Banfield et al.16 have analysed prospectively the response to VR treatment in patients with diagnosis of BPPV and a history of positional vertigo for at least 13 months. The average follow-up was 3 years, 8 months to determine their long-term response to treatment.
The exercise consists of seating the patient and then laying him on the affected side. This position probably will cause dizziness, but the patient should stay in this position until these symptoms have regressed, then the patient returns to the upright position. This exercise must be repeated three times a day for a month.
Banfield’s exercise differs both from the Cawthorne-Cooksey exercises as they are more complex exercises involving the head, neck and chest and from the B-D exercises because it does not involve the movement on the healthy side. At the end of the treatment, 96% of patients responded to treatment and satisfaction scores were high (92%). At the long-term follow-up, 76% of the patients referred the return of their symptoms, but 63% were able to self-care and returned to the exercises of their own accord with benefit. The study showed that VR provides long-term self-reliance as well as short-term cure.
Helminski et al.24 analysed if a daily routine of the self-CRP increases the time to recurrence and significantly reduce the rate of recurrence of BPPV in patients previously treated with CRP. A total of 22 patients were assigned to no-treatment group (control group) and 17 patients to the ‘self-CRP daily’ group (experimental group).
Patients in the experimental group were instructed to perform two cycles of self-CRP one time per day, with the help of a print and digital media to perform the exercises. Every 2 months the patients were asked with a questionnaire whether they showed recurred vertigo and whether they were performing the exercises.
If patients were asymptomatic, they were followed for up 2 years. The symptoms have recurred in 43% patients of the control group and in 38% patients of the experimental group. There were no statistically significant results both in the frequency and in the time of recurrence. So daily routine of self-CRP does not affect the time to recurrence and the rate of vertigo, but the self-CRP makes the patient independent and able to deal independently with a recurrence.
Fujino et al.18 evaluated the effectiveness of VR in patients with BPPV comparing three groups: (1) Betahistine Group, (2) VR Group, (3) VR + betahistine Group.
Each VR patient has performed B-D exercise and Dix-Hallpike modified (move the head repeatedly, rest for 1 min and try to make 50 steps with eyes open and eyes closed). These exercises were performed 15 min three times a day for 8 weeks. The evaluation of the patients was carried out once a week or once every 2 weeks for 8 weeks.
After 2 weeks of treatment, the Groups 2 and 3 have shown a marked improvement rates in vertigo, positional nystagmus and other symptoms than Group 1. The improvement was slightly higher in Group 3 than in Group 2: the global improvement rate was 62% in Group 2, 70% in Group 3 and only 30% in Group 1.
Kulcu et al.19 evaluated the efficacy of a VR exercise by comparing it with medication in patients with BPPV who had already undergone CRP and were still complaining of disequilibrium and vertigo. A total of 38 patients were assigned two groups: (1) Medication group and (2) Experimental (or exercise) group.
Medication group took 8 mg of betahistine three times a day for 1 month. The experimental group was required to perform Cawthorne-Cooksey exercises six times a day for 4 weeks. The follow-up was done at baseline and at the second, fourth and eighth weeks. After the treatment period, patients in both groups were evaluated for another month.
Home-based exercise programme is composed of a series of exercises that stimulate head and eye movements. In case of exacerbation of symptoms, patients have reduced the repetitions or stop the exercise until the symptoms disappeared. Patients continued to perform the exercises until the end of the study, even if the symptoms disappeared.
During the study, patients were asked to record symptoms and document the treatment programme in a diary. In the exercise group, the average of VDI (Vertigo, Dizziness, Imbalance Questionnaire) and VSS (Vertigo Symptom Scale) significantly decreased until the fourth week. Between the fourth and eighth weeks, there were poor improvements.
In medication group, mean scores of VSS diminished earlier but lesser compared with the exercise group. In this study, patients in the exercise group improved more than patients in the medication group.
Steenerson and Cronin20 were aimed at comparing the effectiveness, patient compliance and speed of recovery of BPPV patients, analysing three groups: (1) BPPV patients treated with CRP, (2) BPPV patients treated with VR and (3) No-treatment group.
The first group of BPPV patients was treated with CRP twice weekly, second group performed 15 head position VR assessments (not better specified), asking to repeat these exercises 5–10 times twice daily. Control group included patients who refused treatment. Each patient was evaluated for a 3-month period: all patients were evaluated once a week for the first month and then once a month the next 2 months.
In the CRP group, 70% of patients were asymptomatic after 3 months; in VR group, 63% of patients were free of symptoms at 3 months; and in the control group, 75% of patients showed no improvement. These results showed that CRP is as effective as VR for treatment of BPPV, but a combination of CRP and VR could be better tolerated by BPPV patients.
Soto Varela et al.21 performed a prospective study to evaluate the efficacy of three different physical treatments for BPPV: B-D exercises, the Semont manoeuvre and the Epley manoeuvre. A total of 106 BPPV patients were randomly assigned to three groups: (A) VR group (29 patients), (B) Semont comparator group (35 patients) and (C) Epley comparator group (42 patients).
B-D habituations exercises performed at home three times daily until disappearance of symptoms. The exercises consist of brusque adoption of the supine position, first looking straight ahead, then with the head turned to the right and to the left. Each position is maintained for 30 s.
In Groups B and C, the manoeuvres were repeated weekly until the symptoms disappeared. Patient’s subjective assessment of treatment outcome (cure, partial improvement, stabilization), intensity and duration of nystagmus were evaluated 1 week, 1 month and 3 months after treatment. By the 3-month follow-up, the symptoms in Group C were little more improved than in Group B, though both remained higher than that obtained with the B-D exercises.
Varela et al. found that manoeuvres (either Epley or Semont) were more effective in producing resolution than VR. Angeli et al.22 evaluated the effectiveness of a management approach that combines CRP and VR in elderly patients (>70 years old) with the diagnosis of unilateral PSC-BPPV and with persistence of the BPPV vertigo or nystagmus.
First, the patients (47 patients) were randomly divided in two groups: CRP group (28 patients) and no-treatment group (19 patients), respectively. After 1 month, the patients unresponsive to treatment in CRP group (18/28 patients) were treated with a combination of CRP and VR, and then were re-evaluated 3 months later.
The VR programme included the particle-dispersing exercises and habituation exercises (not better specified), customized for each patient by a physical therapist two or three times a week for 4–6 weeks. Patients were instructed to perform the exercises at home twice a day. At the end of exercise period, patients underwent a re-evaluation that included the Dix-Hallpike test, the electronystagmography test and the evaluation of symptoms.
After 6 weeks, 77% of subjects were cured with CRP plus VR, while 23% either dropped out or failed treatment with CRP and VR. These findings suggest that CRP is more effective than no treatment and VR can be added to improve the results in the treatment of BPPV. A combination of CRP and VR greatly improves symptoms in the elderly.
Tanimoto et al.17 compared the efficacy of modified Epley procedure (MEP) with or without self-treatment in patients with BPPV of the PSC. A total of 80 patients were randomly assigned to (1) Epley-alone group and (2) Self- treatment group.
In first group, MEP was performed once, while self-treatment group underwent MEP plus self-treatment at home. After a week, the patients have made a second visit that included an assessment of symptoms and the Dix-Hallpike test.
Self-treatment included exercises in which the position of the head-hanging is obtained by supporting the shoulder with a pillow and this position must be maintained for 30 s; this procedure was repeated three times daily until there is a resolution of symptoms for at least 24 h.
After 1 week, the Dix-Hallpike test was negative in 72% of patients in the first group and in 90% of patients in the self-treatment group. In total, 69% of patients in the Epley-alone group and 88% of patients in the self-treatment group had an improvement of symptoms and nystagmus. Home-treatment associated with MEP gave significantly better results than MEP alone, as assessed by the Dix-Hallpike test and by both symptoms and nystagmus.
Chang et al.7 investigated the effect of an additional VR exercise programme on balance compared to CRP alone in patients with first attack of BPPV involving the unilateral PSC. A total of 26 patients were divided randomly into two groups of 13 patients each: (1) Control group and (2) Experimental group.
Patients in the control group received the MEP over either one or two sessions during a 2-week period. Subjects in the experimental group received MEP plus 40 min of vestibular-stimulated exercise training three times a week for 4 weeks.
The exercises included oculomotor exercises, head movement, balance exercises and functional activities to improve the balance and reduce vertigo and gaze instability, vertigo and instability of the gaze. Static balance tests, tandem walk test, Dynamic Gait Index (DGI) and subjective rating of the intensity of vertigo were measured at baseline, 2-week and 4-week assessments.
Experimental group showed a marked improvement in these measures than control group, in particular: at 2-week assessment, results reported a statistically significant improvement in single leg stance with eyes closed. At the 4-week assessment stance on foam surface with eyes closed, DGI was significantly improved in favour of experimental group. VR in patients in addition to CRP with BPPV increased patients’ static and dynamic balance and enhanced functional gait ability.
Amor-Dorado et al.25 compared the efficacy of CRP versus VR exercises for treatment of unilateral idiopathic BPPV of the posterior canal. Patients included in Group A were treated with CRP, patients included in Group B performed B-D exercises. Follow-up at Day 7 and 1, 6, 12, 24, 36 and 48 months was carried out.
Group A received modified Epley’s manoeuvre, only one manoeuvre per session. Group B was based on B-D exercise, and it was self-performed domiciliary by the patient with previous instruction given by the otolaryngologists. Five cycles per session three times daily were performed, one movement to each side completed a cycle. Efficacy of the treatment was evaluated using goggles by Dix-Hallpike manoeuvre (DHM) at 1 week; if no nystagmus was visualized, treatment was considered effective.
The differences were statistically significant at 1 month: 92.7% in the CRP group compared to 42.5% in the VR group had a negative DHM. The recurrence rate at 48 months was 35.5% in the VR group and 36.6% in CRP group. The patients included in the CRP group showed a significantly longer time interval between the first and the second episode of recurrence. CRP is more effective treatment than B-D exercise in the short term although exercise may be also considered as an alternative treatment in selected cases.
Ribeiro et al.26 evaluated short-term effects of VR exercises on balance, dizziness symptoms and quality of life in patients aged 65 years or older with BPPV for at least 6 months. The participants were randomly assigned to two groups: the control group, which underwent CRP, and the experimental group, which underwent VR in addition to CRP. Patients were evaluated at the baseline, and at 1, 5, 9 and 13 weeks.
CRP was performed at baseline and repeated up to three times during a session, as necessary. VR exercises were performed twice a week for 50 min each for a period of 12 weeks. The rehabilitation programme included oculomotor exercises, habituation exercises (head movements and repeated trunk), exercises to stimulate balance and strengthen muscles. The main objective of the exercise programme is to stimulate the vestibular system and promote sensory reweighting.
Concerning dynamic balance, there were significant differences between groups: in the experimental group, all dynamic balance parameters significantly improved. There were no significant differences in dizziness symptoms through visual analogue scale (VAS) scores and quality of life according to all Duruoz Hand Index (DHI) subscales evaluations (physical, functional, emotional and total scores) at baseline, 1, 5, 9 and 13 weeks. The patients who received VR demonstrated better results in dynamic balance than those who received only CRP.
Discussion
In this review, we assessed the effectiveness of VR in young and elderly patients with BPPV. Patients after CRP may show an insufficient postural stability control27 and an increased risk of falls, fractures and other damage related to falls.8 Patients show dizziness after ‘liberatory’ CRP also for weeks and have a lower healing because of their expected decrease in vestibular function, multisystem ‘physiologic’ degeneration and less movement in daily activity3 so this post-CRP balance impairment should be managed.28
In our systematic review, the best results of VR were reported in elderly patients with BPPV:26 patients who undergoing VR showed a significant improvement in dynamic balance and self- reliance than patients only treated with CRP.
The first study that shows the efficacy of VR in geriatric BPPV population was carried out in 1989 by Norrè and Beckers.13 Angeli et al.22 confirmed Norrè’s results and underlined that it is very important to rule out the other causes of dizziness and/or comorbidity in the elderly who can compromise the efficacy of VR.
Banfield et al.16 noticed that patients treated with VR showed similar recurrence rate in comparison to patients treated only with CRP, but the recurrence symptoms were less severe and more tolerable by the patient. As showed by Helminski et al.,24 VR increases the patient’s control of the disease process and reduces healthcare cost. VR is an exercise-based group of approaches that began with the aim of maximizing central nervous system compensation for vestibular pathology.29
Currently, protocols differentiate across several key features with differing physiological mechanisms proposed. These include the following:
Compensatory responses (for positional or motion-provoked symptoms), based on the inherent plasticity of the central nervous system and using motion to habituate or reduce responsiveness to repetitive stimuli and to re-balance tonic activity within the vestibular nuclei.
The oculomotor exercises are designed to improve balance stability and visual–vestibular interaction.
The repeated head movement exercises are used to promoting visual stabilization and reducing individual sensitivity.
The balance training exercise emphasizes the use of the vestibular system inputs by altering visual or proprioceptive sensory inputs.
The functional activities facilitate the vestibulospinal response, help regain balance and improve physical function through exercises that took place during walking in different environments.23
Postural control exercises, falls prevention, relaxation training.30
Regarding the comparison between VR and medications to reduce disequilibrium in BPPV patients, the results are contrasting. It has already been widely proven that rehabilitation programmes have an important role in the treatment of BPPV and could be alternative to medications because they have longer lasting efficacy and are lack of side effects;31 in the long-term treatment, the combination of VR and medication could make a greater improvement than the treatment with only medication or only VR.
Thanks to these properties, a combination between CRP and VR could improve, especially in the elderly (>60 years old), static and dynamic balance performance and enhance functional gait ability.23
But what form of VR is most effective? A Systematic Review published in August 2016 in The European Journal of Physical and Rehabilitation Medicine30 tried to determine which type of VR could be more effective than the others in the domains of symptoms (dizziness) or function (activities, quality of life); however, there is insufficient evidence to discriminate between differing forms of VR. Their results are also according to our findings in this systematic review: CRPs are more effective in the short term than VR alone, although a combination of the two is effective for longer term functional recovery.
Conclusion
VR is a simple, low-cost and effective treatment method for improving balance control and quality of life in patients with BPPV, promoting visual stabilization with head movements, improving vestibular–visual interaction during head movement and expanding static and dynamic posture stability.
Our review proves that a hierarchy of interventions should be offered to people with BPPV, starting with CRP followed by post-treatment exercises. CRP and VR seem to have a synergic effect in patients with BPPV because they improve the symptoms in a short time. VR can play a pivotal role in patients affected by comorbidities (cervical or thoracic spine diseases) that contraindicate CRP and can reduce the uptake of anti-vertigo drugs. VR does not reduce the recurrence rate, probably because it does not act on the pathophysiological mechanisms underlying BPPV, but it increases the pleasantness of BPPV episodes.
We certainly reiterate that BPPV requires a multidisciplinary approach in which the collaboration between otolaryngologist, physiatrist, orthopaedics and physical therapist is crucial.
Because no consensus on the VR protocol was found, in particular, with regard to the type of exercises and duration, on the basis of literature and our experience, we propose that further studies are needed to identify a specific VR protocol and type of outcome, and follow-up on larger populations are needed to confirm these encouraging results.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- 1. von Brevern M, Bertholon P, Brandt T, et al. (2015) Benign paroxysmal positional vertigo: Diagnostic criteria. Journal of Vestibular Research: Equilibrium & Orientation 25: 105–117. [DOI] [PubMed] [Google Scholar]
- 2. Oghalai JS, Manolidis S, Barth JL, et al. (2000) Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngology–Head and Neck Surgery 122: 630–634. [DOI] [PubMed] [Google Scholar]
- 3. Salvinelli F, Firrisi L, Casale M, et al. (2004) Benign paroxysmal positional vertigo: Diagnosis and treatment. La Clinica Terapeutica 155: 395–400. [PubMed] [Google Scholar]
- 4. Bhattacharyya N, Baugh RF, Orvidas L, et al. (2008) Clinical practice guideline: Benign paroxysmal positional vertigo. Otolaryngology–Head and Neck Surgery 139: S47–S81. [DOI] [PubMed] [Google Scholar]
- 5. Fife TD, Iverson DJ, Lempert T, et al. (2008) Practice parameter: Therapies for benign paroxysmal positional vertigo (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 70: 2067–2074. [DOI] [PubMed] [Google Scholar]
- 6. Beynon GJ. (1997) A review of management of benign paroxysmal positional vertigo by exercise therapy and by repositioning manoeuvres. British Journal of Audiology 31: 11–26. [DOI] [PubMed] [Google Scholar]
- 7. Chang WC, Hsu LC, Yang YR, et al. (2006) Balance ability in patients with benign paroxysmal positional vertigo. Otolaryngology–Head and Neck Surgery 135: 534–540. [DOI] [PubMed] [Google Scholar]
- 8. Shumway-Cook A, Baldwin M, Polissar NL, et al. (1997) Predicting the probability for falls in community-dwelling older adults. Physical Therapy 77: 812–819. [DOI] [PubMed] [Google Scholar]
- 9. Baloh RW. (1998) Vertigo. The Lancet 352: 1841–1846. [DOI] [PubMed] [Google Scholar]
- 10. Herdman SJ. (1998) Role of vestibular adaptation in vestibular rehabilitation. Otolaryngology–Head and Neck Surgery 119: 49–54. [DOI] [PubMed] [Google Scholar]
- 11. Hebert JR, Corboy JR, Manago MM, et al. (2011) Effects of vestibular rehabilitation on multiple sclerosis-related fatigue and upright postural control: A randomized controlled trial. Physical Therapy 91: 1166–1183. [DOI] [PubMed] [Google Scholar]
- 12. Brandt T, Daroff RB. (1980) Physical therapy for benign paroxysmal positional vertigo. Archives of Otolaryngology 106: 484–485. [DOI] [PubMed] [Google Scholar]
- 13. Norrè ME, Beckers A. (1989) Vestibular habituation training: Exercise treatment for vertigo based upon the habituation effect. Otolaryngology–Head and Neck Surgery 101: 14–19. [DOI] [PubMed] [Google Scholar]
- 14. McCabe BF. (1970) Labyrinthine exercises in the treatment of diseases characterized by vertigo: Their physiologic basis and methodology. The Laryngoscope 80: 1429–1433. [DOI] [PubMed] [Google Scholar]
- 15. Ricci NA, Aratani MC, Dona F, et al. (2010) A systematic review about the effects of the vestibular rehabilitation in middle-age and older adults. Revista Brasileira de Fisioterapia 14: 361–371. [PubMed] [Google Scholar]
- 16. Banfield GK, Wood C, Knight J. (2000) Does vestibular habituation still have a place in the treatment of benign paroxysmal positional vertigo? Journal of Laryngology and Otology 114: 501–505. [DOI] [PubMed] [Google Scholar]
- 17. Tanimoto H, Doi K, Katata K, et al. (2005) Self-treatment for benign paroxysmal positional vertigo of the posterior semicircular canal. Neurology 65: 1299–1300. [DOI] [PubMed] [Google Scholar]
- 18. Fujino A, Tokumasu K, Yosio S, et al. (1994) Vestibular training for benign paroxysmal positional vertigo. Its efficacy in comparison with antivertigo drugs. Archives of Otolaryngology–Head & Neck Surgery 120: 497–504. [DOI] [PubMed] [Google Scholar]
- 19. Kulcu DG, Yanik B, Boynukalin S, et al. (2008) Efficacy of a home-based exercise program on benign paroxysmal positional vertigo compared with betahistine. Journal of Otolaryngology–Head & Neck Surgery 37: 373–379. [PubMed] [Google Scholar]
- 20. Steenerson RL, Cronin GW. (1996) Comparison of the canalith repositioning procedure and vestibular habituation training in forty patients with benign paroxysmal positional vertigo. Otolaryngology–Head and Neck Surgery 114: 61–64. [DOI] [PubMed] [Google Scholar]
- 21. Soto Varela A, Bartual Magro J, Santos Perez S, et al. (2001) Benign paroxysmal vertigo: A comparative prospective study of the efficacy of Brandt and Daroff exercises, Semont and Epley maneuver. Revue De Laryngologie - Otologie - Rhinologie 122: 179–183. [PubMed] [Google Scholar]
- 22. Angeli SI, Hawley R, Gomez O. (2003) Systematic approach to benign paroxysmal positional vertigo in the elderly. Otolaryngology–Head and Neck Surgery 128: 719–725. [DOI] [PubMed] [Google Scholar]
- 23. Chang WC, Yang YR, Hsu LC, et al. (2008) Balance improvement in patients with benign paroxysmal positional vertigo. Clinical Rehabilitation 22: 338–347. [DOI] [PubMed] [Google Scholar]
- 24. Helminski JO, Janssen I, Hain TC. (2008) Daily exercise does not prevent recurrence of benign paroxysmal positional vertigo. Otology & Neurotology 29: 976–981. [DOI] [PubMed] [Google Scholar]
- 25. Amor-Dorado JC, Barreira-Fernandez MP, Aran-Gonzalez I, et al. (2012) Particle repositioning maneuver versus Brandt-Daroff exercise for treatment of unilateral idiopathic BPPV of the posterior semicircular canal: A randomized prospective clinical trial with short- and long-term outcome. Otology & Neurotology 33: 1401–1407. [DOI] [PubMed] [Google Scholar]
- 26. Ribeiro KM, Freitas RV, Ferreira LM, et al. (2017) Effects of balance vestibular rehabilitation therapy in elderly with benign paroxysmal positional vertigo: A randomized controlled trial. Disability and Rehabilitation 39: 1198–1206. [DOI] [PubMed] [Google Scholar]
- 27. Di Girolamo S, Paludetti G, Briglia G, et al. (1998) Postural control in benign paroxysmal positional vertigo before and after recovery. Acta Oto-Laryngologica 118: 289–293. [DOI] [PubMed] [Google Scholar]
- 28. Zucca G, Valli S, Valli P, et al. (1998) Why do benign paroxysmal positional vertigo episodes recover spontaneously? Journal of Vestibular Research: Equilibrium & Orientation 8: 325–329. [PubMed] [Google Scholar]
- 29. Hoffer ME, Balaban CD. (2011) Vestibular rehabilitation: Ready for the mainstream. NeuroRehabilitation 29: 125. [DOI] [PubMed] [Google Scholar]
- 30. Hillier S, McDonnell M. (2016) Is vestibular rehabilitation effective in improving dizziness and function after unilateral peripheral vestibular hypofunction? An abridged version of a Cochrane Review. European Journal of Physical and Rehabilitation Medicine 52: 541–556. [PubMed] [Google Scholar]
- 31. McClure JA, Willett JM. (1980) Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. Journal of Otolaryngology 9: 472–477. [PubMed] [Google Scholar]


