Stem Cell Development
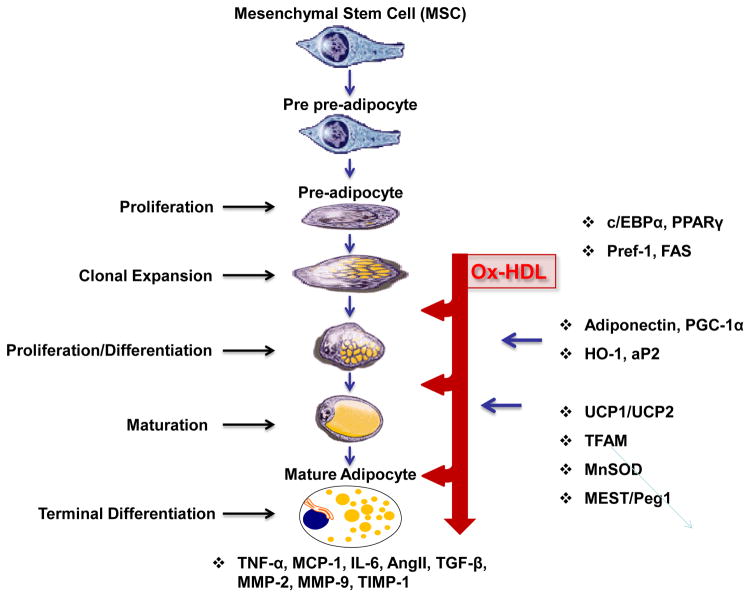
The development of adipocytes in mice and humans follows a well-defined pathway that commences with a common pluripotent mesenchymal stem cell (MSC), ie., adipogenesis [1]. The early steps of the pathway leading to the generation and the commitment of MSCs to an adipocyte lineage are unknown. Hypothetically, the determination of the fate of MSCs occurs early in cell differentiation (“commitment”) and involves the interplay of intrinsic (genetic) and environmental (local and systemic) conditions that ultimately define the fate of the cell. Factors that determine MSC proliferation and differentiation also govern early adipocyte development and function. Currently, little is known about this process; from MSC-to-preadipocyte differentiation. However, the steps governing the transition from preadipocyte to adipocyte differentiation are not well defined (Figure 1). During adipogenesis MSCs or preadipocytes differentiate into lipid-laden adipocytes [2]. Ox-HDL increases adipogenic properties with a marked effect on the last step of adipocyte-terminal differentiation and release of adipokines including 20-HETE and Ang II.
Figure 1.
Schematic presentation of MSCs giving rise to adipocyte differentiation.
MSCs can differentiate into adipocytes when placed in the adipogenesis medium in vitro. Various adipokines including Ang II, Leptin, TGFβ, VEGF, FGF, HGF, TNF, Adiponectin, MMP-2, MMP-9 and IGF-1 are secreted from adipocytes. Particular molecular events accompanying each stage of differentiation are indicated to the right, with the imprecise interval in each stage reflected as indicated.
MSCs were initially identified in postnatal human bone marrow and have been used to model differentiating mesoderm. It is believed that the MSCs give rise to a common early precursor (pre-adipocyte, Adipoblast), which, in turn, develops into the committed white and brown preadipocyte that under appropriate stimulatory conditions, differentiate into mature adipocytes of different types [3]. The transition from preadipocyte to adipocyte involves four stages: growth arrest, clonal expansion, early differentiation and terminal differentiation [4]. Adipocytes regulate glucose homeostasis [5] and adipocyte dysfunction results in the secretion of decreased levels of adiponectin and decreased glucose uptake, leading to insulin resistance [6].
Obesity and Ox-HDL
Obesity is also linked to the metabolic syndrome, which is associated with a dyslipidemic profile that includes hypertriglyceridemia and low plasma high-density lipoprotein cholesterol (HDL-C). Accumulated evidence suggests that HDL enhancement plays a beneficial role in maintaining glucose homeostasis via insulin dependent and independent pathways. Low Density Lipoprotein Cholesterol (LDL-C) and HDL-C levels have become the accepted biomarkers in the evaluation of the risk of CVD, CAD, and even CKD [7,8]. Recent studies have suggested that HDL function is more important than total levels of HDL and that remodeling and dysfunction likely contribute to increased risk of CVD, CKD, and CRS.
High fat diets increase LDL and glucose levels [9] which are both reversed by an increased expression of the antioxidant gene, heme oxygenase (HO-1). In another model of high fat (HF) diets in hypertensive rats, LDL is increased and this is prevented by induction of HO-1 by a number of cobalt compounds including cobalt protoporphyrin [10]. Similar observations are described for male and female mice [11]. These observations are attributed to increases in ROS in adipose tissue and liver that may involve increases in Ang II and 20-HETE, which are major sources of ROS [12]. Deletion of angiotensinogen in hepatocytes markedly decreased blood pressure [13]. Angiotensinogen has been synthesized by 3T3-F442A cells and hydrolyzed to ANG l and ANG II in adipocytes [14], and its deletion from adipose tissue resulted in a decrease in blood pressure elevation in obese mice [15]. In another study, increases in antioxidants decrease the Ang II-mediated increase in ROS [16–18]. These reports suggest that targeting the Ang II system may have therapeutic value. The increase in ROS is considered a contributing factor in Ox-LDL [19] in contrast to an increase of HO-1, which inhibits atherogenesis [20] and atherosclerotic lesion in LDL receptor (−/−) mice [21], reviewed in [22].
Dysfunctional HDL can result from both free radical attack and oxidation of ‘good’ HDL, leading to Ox-HDL (‘bad’ HDL) [23–25]. Lipids and lipoproteins are the primary targets of free radical damage [26], which results in lity and CVD and cardiac events.
Process of MSCs differentiation to Adipocytes
HO-1 effect Plasma LDL and HDL
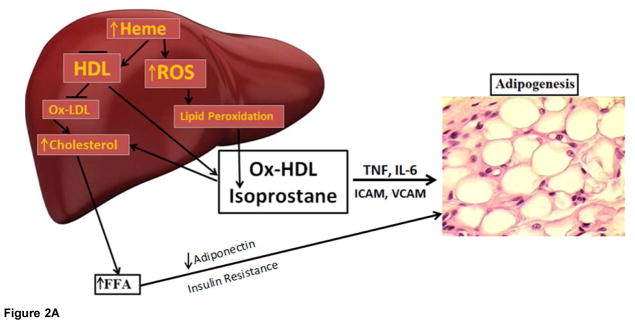
We believe that levels of antioxidants will change the ratio of LDL and HDL in mice. As shown in figure 2A and 2B, the ratios of plasma LDL and HDL is significantly higher in obese mice than in lean mice (0.41 + 0.15 vs 0.05 + 0.02, *p<0.05). An increase of HO-1 and antioxidant properties [12,39] by CoPP decreased the ratio (0.15 + 0.01 vs 0.41 + 0.15, *p<0.05). Inhibition of HO-1 and increase of antioxidant by SnMP blocked the effect of CoPP on obese mice.
Figure 2.
Figure 2A. HO-1 decrease ratios of LDL/HDL in obese mice treated with CoPP, obese mice display high levels of LDL, while treatment with CoPP, for 4 weeks decrease LDL, that is reversed by inhibition of antioxidant HO-1
Figure 2B. HO-1 decreases ratios of LDL/HDL in obese mice treated with CoPP, obese mice display high levels of LDL, while treatment with CoPP, for 4 weeks decreases LDL, that is reversed by inhibition of antioxidant HO-1.
The Effect of Ox-HDL and Isoprostanes on Adipogenesis
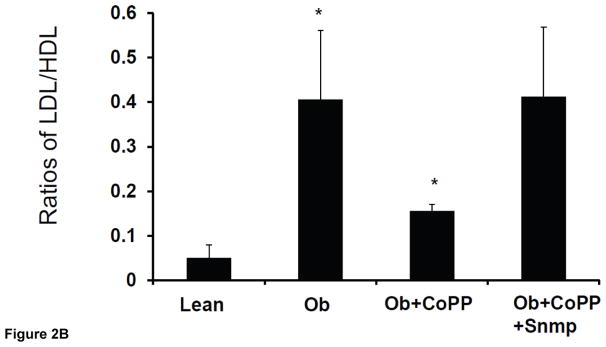
We examined the levels of LDL to HDL in mice treated with CoPP, which increases HO-1-derived bilirubin levels. Since obesity is associated with a ISSN 2472-6990 decrease of antioxidants, we propose that this will result in an increase in levels of Ox-HDL as Ox-HDL is increased in cardiac events. We examined the effect of Ox-HDL and isoprostanes on adipogenesis in the human adipocyte by measuring Oil Red O stained lipid droplet area after 10 days of treatment (Figure 3). The level of Oil Red O stained lipid droplets increased after treatment with Ox-HDL, isoprostanes, and a combination of the two. Quantification of Oil Red O stained cells showed an increase in lipid droplets in the presence of both Ox-HDL and isoprostanes compared with control p<0.05 and Ox-HDL. This effect proved to be synergistic, p<0.05 (Figure 3). These results were confirmed in mice (results not shown).
Figure 3.
Adipogenic effect of oxidized HDL and isoprostane on MSC-derived adipocytes. Adipogenesis from human MSC was detected by Oil Red O staining and absorbance was measured as described [37,39]. *p<0.05 versus control.
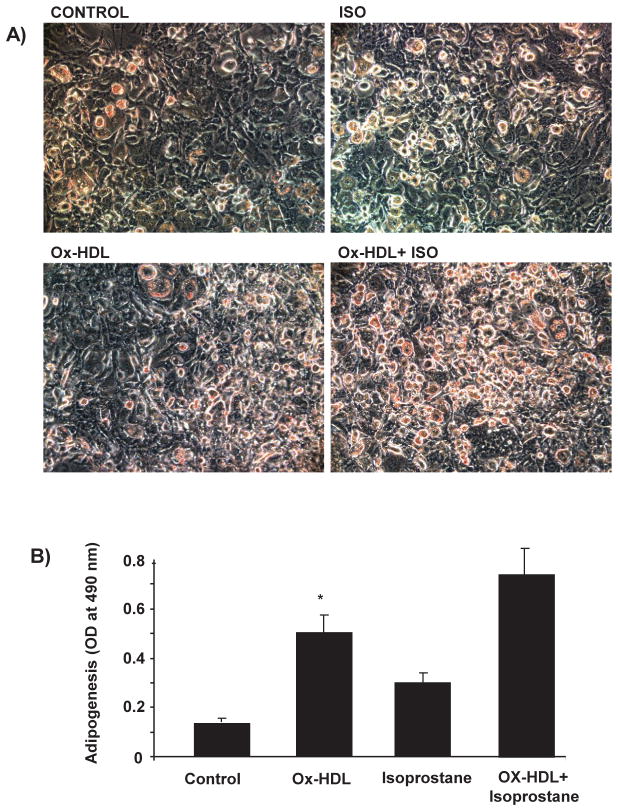
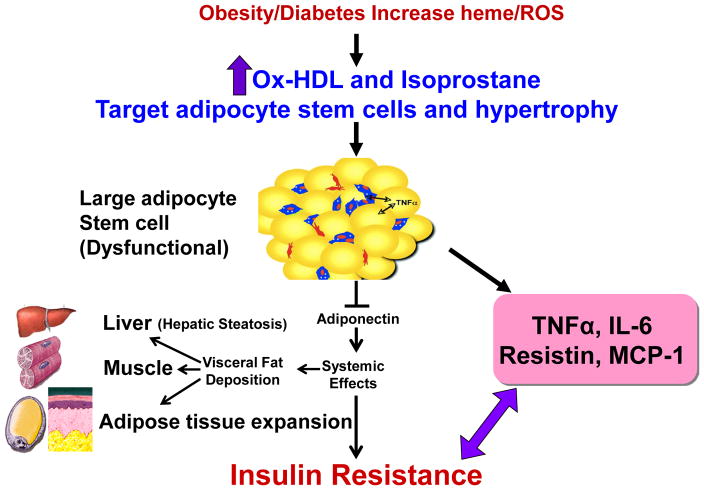
Figure 4 is a schematic that shows the release of the inflammatory cytokines IL-6, and TNF and ROS. ROS increases lipid peroxidation with increased levels of Ox-HDL, LDL and isoprostane. Excess heme, needed for adipocyte differentiation and terminal differentiation, also increases ROS. Hyperglycemia in the obese will also increase the levels of ROS (Reviewed in [12]). With the down regulation of HO-1 in obesity, heme catabolism is decreased. ROS targeting adipocyte stem cells and hypertrophy occurs in several animal models of obesity which leads to an increase of inflammatory adipokines, a decrease in adiponectin, liver and muscle fat deposit and insulin resistance.
Figure 4.
Schematic representing the increase in ROS by high fat, glucose or excessive heme levels that in turn increase the generation of oxidized HDL and isoprostane. Enlargement of adipocytes causes alterations in the secretion of adipokines. Increased adipocyte size can lead to deleterious alterations in insulin sensitivity caused by a decrease in adiponectin secretion and the induction of inflammatory mediators.
This review demonstrates that Ox-HDL and isoprostane exert marked increases in adipogenesis in human adipocyte stem cells. Ox-HDL is associated with an increase in adipocyte expansion and adiposity and, as such, is a determinant of obesity and its related disorders. There are several ways in which Ox-HDL can be formed. One way is during the process of differentiating adipocytes. This process begins with a high food intake, early hyperglycemia occurs resulting in an increase in cellular heme due to a decrease in the levels of HO-1 (reviewed in [12]). Heme is a pro-oxidant and a source of ROS which contribute to an increase in NO uncoupling by iNOS induction. The induction of iNOS causes the formation of peroxynitrite which is responsible for lipid peroxidation and inhibition of protein and enzyme function and increased Ox-HDL levels. A prime example is a decrease in the levels of HO-1 which, in turn, decreases bilirubin levels. Bilirubin is a potent antioxidant and patients with elevated bilirubin levels display a lower risk of cardiovascular disease and have higher levels of HDL (reviewed in [31]).
There are a number of mechanisms by which obesity increases the levels of Ox-HDL. These occur during the process of differentiating adipocytes that requires glucose, which is a major source of ROS. Furthermore, myeloperoxidase is responsible for generating excessive levels of ROS [32] with a resultant increase in lipid peroxidation which converts LDL and HDL to oxidized products with an expansion of adipogenesis.
We and others have shown that an excess of heme in adipocyte stem cells and in the fat of obese mice is necessary in order for adiposity [11,33–37]. Therefore, increased heme levels in obese subjects, is a major source of ROS, contributing to lipid peroxidation and production of Ox-HDL and Ox-LDL. Additionally, hemoglobin influences LDL and HDL in obesity and diabetes. Hemoglobin increases the levels of proinflammatory HDL, in other words, increases the oxidation of HDL. We believe that HDL dysfunction is not the cause of adipogenesis, but it is the oxidation of the HDL itself [38].
Obesity is a growing epidemic in the United States as well as worldwide. Many of the cardiovascular complications associated with obesity are, in part, due to dysfunctional adipocytes and endothelial damage. Several clinical conditions such as diabetes mellitus and obesity, are characterized by both increased inflammation and oxidative stress, and are associated with increased risk of cardiovascular complications. An increase in Ox-HDL negatively correlated with adiponectin levels in morbidly obese subjects (unpublished data). Thus, HDL and Ox-HDL may prove of particular relevance, in the maintenance and regulation of cardiovascular health and as targets for the prevention of cardiovascular events.
In conclusion, this communication suggests that the novel finding that Ox-HDL and isoprostane act at the three points presented in figure 1, and that it appears that Ox-HDL enhances adipogenesis and/or the recruitment of stem cells in adipose tissue, and increases the adipogenic lineage and exacerbates obesity and the metabolic syndrome. In support of this conclusion, isoprostane, another oxidant found in the plasma of obese subjects increases adipogenesis and, with Ox-HDL, synergistically increases adipocyte stem cell proliferation, differentiation and hypertrophy. Thus Ox-HDL function, due to its adipogenic effect on adipocyte stem cells, should be re-evaluated to address the metabolic derangements associated with the metabolic syndrome.
Acknowledgments
This work was supported by National Institutes of Health grants HL55561, HL34300, HL 109015, The Brickstreet Foundation and The Huntington Foundation (NGA, JIS). We thank Jennifer Brown for her outstanding editorial assistance in the preparation of the manuscript.
References
- 1.Vazquez-Vela ME, Torres N, Tovar AR. White adipose tissue as endocrine organ and its role in obesity. Arch Med Res. 2008;39:715–728. doi: 10.1016/j.arcmed.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Lefterova MI, Lazar MA. New developments in adipogenesis. Trends Endocrinol Metab. 2009;20:107–114. doi: 10.1016/j.tem.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Kadoya C, Domino EF, Yang GY, Stern JD, Betz AL. Preischemic but not post ischemic zinc protoporphyrin treatment reduces infarct size and edema post ischemic zinc protoporphyrin treatment reduces infarct size and edema accumulation after temporary focal cerebral ischemia in rats. Stroke. 1995;26:1035–1038. doi: 10.1161/01.str.26.6.1035. [DOI] [PubMed] [Google Scholar]
- 4.Graven KK, Zimmerman LH, Dickson EW, Weinhouse GL, Farber HW. Endothelial cell hypoxia associated proteins are cell and stress specific. J Cell Physiol. 1993;157:544–554. doi: 10.1002/jcp.1041570314. [DOI] [PubMed] [Google Scholar]
- 5.Yu F, Takahashi T, Moriya J, Kawaura K, Yamakawa J, et al. Angiotensin-II receptor antagonist alleviates non-alcoholic fatty liver in KKAy obese mice with type 2 diabetes. J Int Med Res. 2006;34:297–302. doi: 10.1177/147323000603400309. [DOI] [PubMed] [Google Scholar]
- 6.Guzik TJ, Mangalat D, Korbut R. Adipocytokines-novel link between inflammation and vascular function? J Physiol Pharmacol. 2006;57:505–528. [PubMed] [Google Scholar]
- 7.Navab M, Anantharamaiah GM, Reddy ST, Van Lenten BJ, Fogelman AM. HDL as a biomarker, potential therapeutic target, and therapy. Diabetes. 2009;58:2711–2717. doi: 10.2337/db09-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaziri ND, Navab M, Fogelman AM. HDL metabolism and activity in chronic kidney disease. Nat Rev Nephrol. 2010;6:287–296. doi: 10.1038/nrneph.2010.36. [DOI] [PubMed] [Google Scholar]
- 9.Peterson SJ, Husney D, Kruger AL, Olszanecki R, Ricci F, et al. Long-term treatment with the apolipoprotein A1 mimetic peptide increases antioxidants and vascular repair in type I diabetic rats. J Pharmacol Exp Ther. 2007;322:514–520. doi: 10.1124/jpet.107.119479. [DOI] [PubMed] [Google Scholar]
- 10.Cao J, Inoue K, Sodhi K, Puri N, Peterson SJ, et al. High-fat diet exacerbates renal dysfunction in SHR: reversal by induction of HO-1-adiponectin axis. Obesity (Silver Spring) 2012;20:945–953. doi: 10.1038/oby.2011.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burgess A, Li M, Vanella L, Kim DH, Rezzani R, et al. Adipocyte heme oxygenase-1 induction attenuates metabolic syndrome in both male and female obese mice. Hypertension. 2010;56:1124–1130. doi: 10.1161/HYPERTENSIONAHA.110.151423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abraham NG, Junge JM, Drummond GS. Translational Significance of Heme Oxygenase in Obesity and Metabolic Syndrome. Trends Pharmacol Sci. 2016;37:17–36. doi: 10.1016/j.tips.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yiannikouris F, Wang Y, Shoemaker R, Larian N, Thompson J, et al. Deficiency of angiotensinogen in hepatocytes markedly decreases blood pressure in lean and obese male mice. Hypertension. 2015;66:836–842. doi: 10.1161/HYPERTENSIONAHA.115.06040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saye JA, Cassis LA, Sturgill TW, Lynch KR, Peach MJ. Angiotensinogen gene expression in 3T3-L1 cells. Am J Physiol. 1989;256:C448–C451. doi: 10.1152/ajpcell.1989.256.2.C448. [DOI] [PubMed] [Google Scholar]
- 15.Yiannikouris F, Karounos M, Charnigo R, English VL, Rateri DL, et al. Adipocyte-specific deficiency of angiotensinogen decreases plasma angiotensinogen concentration and systolic blood pressure in mice. Am J Physiol Regul Integr Comp Physiol. 2012;302:R244–R251. doi: 10.1152/ajpregu.00323.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Botros FT, Laniado-Schwartzman M, Abraham NG. Regulation of cyclooxygenase-and cytochrome p450-derived eicosanoids by heme oxygenase in the rat kidney. Hypertension. 2002;39:639–644. doi: 10.1161/hy0202.103420. [DOI] [PubMed] [Google Scholar]
- 17.Quan S, Yang L, Shenouda S, Schwartzman ML, Nasjletti A, et al. Expression of human heme oxygenase-1 in the thick ascending limb attenuates angiotensin II-mediated increase in oxidative injury. Kidney Int. 2004;65:1628–1639. doi: 10.1111/j.1523-1755.2004.00562.x. [DOI] [PubMed] [Google Scholar]
- 18.Yang L, Quan S, Nasjletti A, Laniado-Schwartzman M, Abraham NG. Heme oxygenase-1 gene expression modulates angiotensin II-induced increase in blood pressure. Hypertension. 2004;43:1221–1226. doi: 10.1161/01.HYP.0000126287.62060.e6. [DOI] [PubMed] [Google Scholar]
- 19.Ishikawa K, Navab M, Leitinger N, Fogelman AM, Lusis AJ. Induction of heme oxygenase-1 inhibits the monocyte transmigration induced by mildly oxidized LDL. J Clin Invest. 1997;100:1209–1216. doi: 10.1172/JCI119634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ishikawa K, Sugawara D, Goto J, Watanabe Y, Kawamura K, et al. Heme oxygenase-1 inhibits atherogenesis in Watanabe heritable hyperlipidemic rabbits. Circulation. 2001;104:1831–1836. doi: 10.1161/hc3901.095897. [DOI] [PubMed] [Google Scholar]
- 21.Ishikawa K, Sugawara D, Wang X, Suzuki K, Itabe H, et al. Heme oxygenase-1 inhibits atherosclerotic lesion formation in ldl-receptor knockout mice. Circ Res. 2001;88:506–512. doi: 10.1161/01.res.88.5.506. [DOI] [PubMed] [Google Scholar]
- 22.Ansell BJ, Fonarow GC, Fogelman AM. The paradox of dysfunctional high-density lipoprotein. Curr Opin Lipidol. 2007;18:427–434. doi: 10.1097/MOL.0b013e3282364a17. [DOI] [PubMed] [Google Scholar]
- 23.Pan B, Yu B, Ren H, Willard B, Pan L, et al. High-density lipoprotein nitration and chlorination catalyzed by myeloperoxidase impair its effect of promoting endothelial repair. Free Radic Biol Med. 2013;60:272–281. doi: 10.1016/j.freeradbiomed.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Proudfoot JM, Barden AE, Loke WM, Croft KD, Puddey IB, et al. HDL is the major lipoprotein carrier of plasma F2-isoprostanes. J Lipid Res. 2009;50:716–722. doi: 10.1194/jlr.M800607-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicholls SJ, Zheng L, Hazen SL. Formation of dysfunctional high-density lipoprotein by myeloperoxidase. Trends Cardiovasc Med. 2005;15:212–219. doi: 10.1016/j.tcm.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Vazzana N, Ganci A, Cefalu AB, Lattanzio S, Noto D, et al. Enhanced lipid peroxidation and platelet activation as potential contributors to increased cardiovascular risk in the low-HDL phenotype. J Am Heart Assoc. 2013;2:e000063. doi: 10.1161/JAHA.113.000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cazzola R, Cassani E, Barichella M, Cestaro B. Impaired fluidity and oxidizability of HDL hydrophobic core and amphipathic surface in dyslipidemic men. Metabolism. 2013;62:986–991. doi: 10.1016/j.metabol.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 28.Puchades MJ, Saez G, Munoz MC, Gonzalez M, Torregrosa I, et al. Study of oxidative stress in patients with advanced renal disease and undergoing either hemodialysis or peritoneal dialysis. Clin Nephrol. 2013;80:177–186. doi: 10.5414/CN107639. [DOI] [PubMed] [Google Scholar]
- 29.Montuschi P, Barnes PJ, Roberts LJ. Isoprostanes: markers and mediators of oxidative stress. FASEB J. 2004;18:1791–1800. doi: 10.1096/fj.04-2330rev. [DOI] [PubMed] [Google Scholar]
- 30.Montuschi P, Barnes P, Roberts LJ. Insights into oxidative stress: the isoprostanes. Curr Med Chem. 2007;14:703–717. doi: 10.2174/092986707780059607. [DOI] [PubMed] [Google Scholar]
- 31.Vitek L. The role of bilirubin in diabetes, metabolic syndrome, and cardiovascular diseases. Front Pharmacol. 2012;3:55. doi: 10.3389/fphar.2012.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ansell BJ, Fonarow GC, Navab M, Fogelman AM. Modifying the anti-inflammatory effects of high-density lipoprotein. Curr Atheroscler Rep. 2007;9:57–63. doi: 10.1007/BF02693941. [DOI] [PubMed] [Google Scholar]
- 33.Kumar N, Solt LA, Wang Y, Rogers PM, Bhattacharyya G, et al. Regulation of adipogenesis by natural and synthetic REV-ERB ligands. Endocrinology. 2010;151:3015–3025. doi: 10.1210/en.2009-0800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.London IM, West R, Shemin D, Rittenberg D. On the origin of bile pigment in normal man. J Biol Chem. 1950;184:351–358. [PubMed] [Google Scholar]
- 35.Puri N, Sodhi K, Haarstad M, Kim DH, Bohinc S, et al. Heme induced oxidative stress attenuates sirtuin1 and enhances adipogenesis in mesenchymal stem cells and mouse pre-adipocytes. J Cell Biochem. 2012;113:1926–1935. doi: 10.1002/jcb.24061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vanella L, Sodhi K, Kim DH, Puri N, Maheshwari M, et al. Increased heme-oxygenase 1 expression decreases adipocyte differentiation and lipid accumulation in mesenchymal stem cells via upregulation of the canonical Wnt signaling cascade. Stem Cell Res Ther. 2013;4:28. doi: 10.1186/scrt176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vanella L, Kim DH, Sodhi K, Barbagallo I, Burgess AP, et al. Crosstalk between EET and HO-1 downregulates Bach1 and adipogenic marker expression in mesenchymal stem cell derived adipocytes. Prostaglandins Other Lipid Mediat. 2011;96:54–62. doi: 10.1016/j.prostaglandins.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watanabe J, Grijalva V, Hama S, Barbour K, Berger FG, et al. Hemoglobin and its scavenger protein haptoglobin associate with apoA-1-containing particles and influence the inflammatory properties and function of high density lipoprotein. J Biol Chem. 2009;284:18292–18301. doi: 10.1074/jbc.M109.017202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim DH, Vanella L, Inoue K, Burgess A, Gotlinger K, et al. Epoxyeicosatrienoic acid agonist regulates human mesenchymal stem cell-derived adipocytes through activation of HO-1-pAKT signaling and a decrease in PPARgamma. Stem Cells Dev. 2010;19:1863–1873. doi: 10.1089/scd.2010.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]