Abstract
Background
Male partner reproductive coercion is defined as male partners' attempts to promote pregnancy through interference with women’s contraceptive behaviors and reproductive decision making. Male partners may try to promote pregnancy through birth control sabotage such as taking away or destroying their partners' contraceptives, refusing to wear condoms, and/or verbally pressuring their partners to abstain from contraceptive use. Reproductive coercion is associated with an elevated risk for unintended pregnancy. Women experiencing intimate partner violence, racial/ethnic minorities and those of lower socioeconomic status, are more likely to experience reproductive coercion. Women veterans who use Veterans Affairs (VA) for health care may be particularly vulnerable to reproductive coercion as they are disproportionally from racial/ethnic minority groups and experience high rates of intimate partner violence.
Objectives
We sought to examine the prevalence, correlates, and impact of reproductive coercion among women veterans served by the VA healthcare system.
Study Design
We analyzed data from a national telephone survey of women veterans aged 18–44, with no history of sterilization or hysterectomy, who had received care within VA in the prior 12 months. Participants who had sex with men in the last year were asked if they experienced male partner reproductive coercion. Adjusted logistic regression was used to examine the relationship between participant characteristics and male partner reproductive coercion and the relationship between reproductive coercion and the outcomes of contraceptive method used at last sex, and pregnancy and unintended pregnancy in the last year.
Results
Among the 1,241 women veterans in our study cohort, 11% reported experiencing male partner reproductive coercion in the past year. Black women, younger women, and single women were more likely to report reproductive coercion than their white, older, and married counterparts. Women who experienced military sexual trauma were also more likely to report reproductive coercion compared to women who did not report military sexual trauma. In adjusted analyses, compared to women who did not experience reproductive coercion, those who did were less likely at last sex to have used any method of contraception (76% vs. 80%; aOR: 0.61, 95% CI: 0.38–0.96), prescription contraception (43% vs. 55%; aOR: 0.62, 95% CI: 0.43–0.91) and their ideal method of contraception (35% vs. 45%; aOR: 0.63, 95% CI: 0.43–0.93). Those who reported coercion were more likely to have had a pregnancy in the last year (14% vs. 10%; aOR: 2.07, 95% CI: 1.17–3.64); there were no significant differences in unintended pregnancy by coercion status (6% vs. 4%; aOR: 1.63, 95% CI: 0.71–3.76).
Conclusion
Eleven percent of women veterans in our sample experienced male partner reproductive coercion, which may impact their use of contraception and ability to prevent pregnancy.
Keywords: contraception, ECUUN, reproductive coercion, VA
Introduction
Reproductive health care, including contraceptive care, for women veterans is an increasing priority for the Veterans Affairs (VA) Healthcare System as women veterans now comprise close to 7% of the over 5 million VA users and approximately 40% are of reproductive age.1 One recently identified factor that impacts reproductive health, yet remains relatively under-recognized in the clinical setting, is male partner reproductive coercion.2,3 Male partner reproductive coercion is defined as male partners’ attempts to promote pregnancy through interference with women’s contraceptive behaviors and reproductive decision making.2,4,5 Male partners may try to promote pregnancy through birth control sabotage such as taking away or destroying their partners’ contraceptives, refusing to wear condoms, and/or verbally pressuring their partners to abstain from contraceptive use.2 Thus, it is not surprising that reproductive coercion is associated with an elevated risk for unintended pregnancy.2,4,5
Research indicates that women experiencing intimate partner violence (IPV), racial/ethnic minorities, those of lower socioeconomic status, and single women are more likely to experience reproductive coercion.6 Given this risk profile, women veterans who use VA for health care may be particularly vulnerable to reproductive coercion as they are disproportionally from racial/ethnic minorities groups and experience high rates of IPV and lifetime sexual abuse.1,7,8 Women veterans often experience sexual violence revictimization, possibly increasing risk for reproductive coercion.8
Currently, there is no information about male partner reproductive coercion among women veterans. Understanding the prevalence, correlates, and impact of reproductive coercion among women veterans is important to ensure high-quality, comprehensive reproductive health care in VA. Thus, using data from the study, “Examining Contraceptive Use and Unmet Need among Women Veterans” (ECUUN), we sought to examine the prevalence of male partner reproductive coercion, the relationship between participant characteristics and reproductive coercion, and associations between reproductive coercion and contraceptive use and pregnancy among women veterans.
Materials and Methods
Study design and sample
Survey methods for the ECUUN study have been previously reported.9 In brief, ECUUN included a national survey of women VA-users to assess women’s contraceptive use, pregnancy history, and experiences with VA reproductive healthcare. A random, national sample of women veterans aged 18–44 who had used VA for primary care in the prior 12 months were sent invitations via mail to participate in the study. Women were asked to express interest in or opt out of the study via a toll-free study telephone number or reply card. All women who did not opt out of the study were called to determine interest in participating, undergo eligibility screening, and provide verbal informed consent. Interviews were conducted from April 2014 through January 2016 by trained interviewers using computer-assisted telephone interview (CATI) technology. Interviews lasted an average of 45 minutes and participants received a $30 honorarium. The University of Pittsburgh and the VA Pittsburgh Institutional Review Boards approved this study.
We sent out 8,198 invitations, 2,769 women were screened and enrolled and a total of 2,302 women completed surveys. Thus, the overall response rate was 28% and the survey completion rate among those enrolled was 83%. Using VA administrative data, participants (n=2,302) were compared to non-participants (n=5,896) from the sampling frame with respect to race/ethnicity, age, income, marital status, medical conditions, and mental illness. All differences between the groups were minimal (standardized differences of 0.07–0.11), suggesting that the ECUUN sample is representative of the larger population of reproductive-aged women VA-users.10 For this analysis, our sample included 1,241 women who had sex with a man in the past year, excluding women who reported a history of hysterectomy or tubal sterilization. In addition, women who reported using male partner sterilization as their contraceptive method at last sex (n=142) were excluded as were 5 women who had missing data on male partner reproductive coercion.
Survey measures
Male partner reproductive coercion was assessed by asking participants if any male sexual partners they had been with in the last year had ever: “taken a condom off during sex, refused to use a condom, or broken a condom so you would get pregnant?”; “taken your birth control away from you or kept you from getting birth control so that you would get pregnant?” and/or “told you not to use any form of birth control?” A positive response to any of these items was defined as having experienced male partner reproductive coercion. These items were adapted from questions developed by Miller et al.4
Independent variables of interest include patient age, race/ethnicity, marital status, education, income, religion; parity, branch of military service, history of military sexual trauma (MST), mental health diagnosis, and medical health diagnosis, and geographic region. Race/ethnicity was categorized as non-Hispanic white, non-Hispanic black, Hispanic and other (e.g., Asian/Pacific Islanders, American Indian and Alaska Natives, and multiracial). In accordance with VA clinical screening recommendations,11 2 items assessed whether women ever received uninvited and unwanted sexual attention or whether someone ever used force or threat of force to have sexual contact with them against their will while they were in the military. A positive response to either or both items indicated a history of MST. For medical conditions, women were asked if they had ever been diagnosed with or received treatment for any of the following conditions that represent relative or absolute contraindications to estrogen use12 or that might otherwise affect contraceptive care: hypertension, history of thromboembolic disease, breast cancer, stroke, liver disease, HIV/AIDs, obesity, diabetes, migraines, systemic lupus erythematosus, and seizure disorders. For mental health conditions, women were asked if they had ever been diagnosed with or received treatment for depression, bipolar disorder, posttraumatic stress disorder or PTSD, schizophrenia, or anxiety or panic disorder.
We were also interested in the association between male partner reproductive coercion and the following outcomes: contraceptive method used at last sex; pregnancy in the last year; and unintended pregnancy in the last year. We assessed 3 measures of contraceptive use at last sex: 1) use of any method of contraception [intrauterine devices (IUDs), subdermal implants, pill, ring, patch, injection, condoms, diaphragm, cervical cap, fertility-awareness methods, spermicides and withdrawal]; 2) use of any prescription method of contraception (IUDs, subdermal implants, pill, ring, patch, injection); and 3) use of ideal method of contraception. We defined ideal contraceptive method by asking women if they could choose any one method of contraception what their ideal choice would be; we then compared this response with the method that women actually used at last sex to determine if they were using their ideal method of contraception. To assess unintended pregnancy, women were asked to characterize each pregnancy in the past year as either unwanted (did not ever want to get pregnant in the future) or as occurring at the right time, later than desired, sooner than desired, or that women didn't know or didn’t care about the timing of their pregnancy. Consistent with convention, pregnancies reported as either unwanted or having occurred sooner than desired were considered to be unintended.13
Analysis
Participant characteristics and frequencies of reproductive coercion were examined for the study cohort. Bivariate analyses using chi-squared tests were performed to assess associations between participant characteristics (age, race/ethnicity, marital status, education, income, parity, military branch, MST, mental illness, and medical condition) and the outcome, reproductive coercion. Adjusted logistic regression was used to examine the relationships between each participant characteristic and reproductive coercion to identify all possible correlates.
Next, we examined the association between reproductive coercion as the key independent variable and 5 outcomes: any contraceptive method use at last sex (yes/no), any prescription contraception method use at last sex (yes/no), ideal contraceptive method use at last sex (yes/no), pregnancy in the last year (yes/no), and unintended pregnancy in the last year (yes/no). We described and compared the rates of the outcomes by reproductive coercion status using chi-squared tests. Adjusted logistic regression was used to model the 5 outcomes separately. We adjusted for participant factors associated with reproductive coercion at the p<0.10 level in bivariable analyses to be inclusive and control for any potential confounders. Unadjusted odds ratios and adjusted odds ratios (aOR) and 95% confidence intervals (CIs) were reported. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC), and statistical significance was set at p < 0.05.
Results
Eleven percent of women in the total sample reported some form of reproductive coercion in the past year. More than 7% of women in the sample reported that a male sexual partner had removed, broken or refused to use a condom during sex; less than 1% of women reported that a male partner had taken their birth control; and 6% of women reported that a partner had told them not to use any type of birth control.
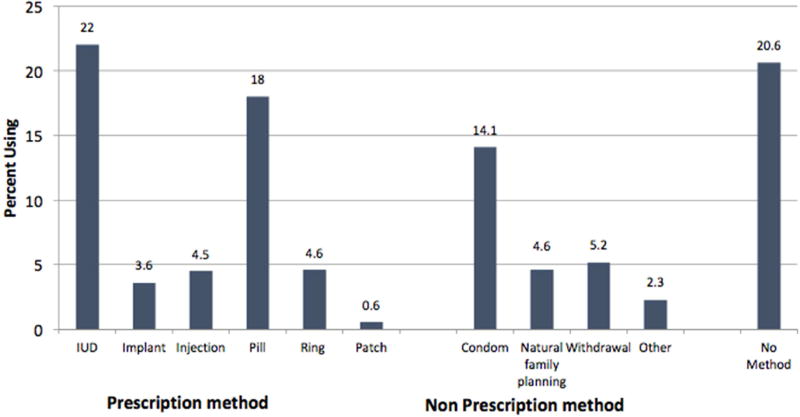
Sociodemographic characteristics of our study population are shown in Table 1. Briefly, 51% were non-Hispanic White, 28% were non-Hispanic Black, 13% were Hispanic, and 8% identified as “other” race. The majority of the women were between the ages of 30 to 39 (59%), were married or living with a partner (52%), had a college degree (53%), had an annual household income below $40,000 (54%), had children (60%), and served in the Army (50%). Overall, 79% of women used any method of contraception, and 53% used prescription contraception. The distribution of specific contraceptive methods is shown in Figure 1.
Table 1.
Demographic Characteristics of Study Sample
| Full Cohort N (%) |
|
|---|---|
| Age | |
| 20–29 | 332 (26.8) |
| 30–34 | 425 (34.2) |
| 35–39 | 306 (24.7) |
| 40–44 | 178 (14.3) |
| Race/ethnicity | |
| Non-Hispanic White | 631 (50.8) |
| Non-Hispanic Black | 349 (28.1) |
| Hispanic | 166 (13.4) |
| Other* | 95 (7.7) |
| Marital status | |
| Single | 276 (22.3) |
| Married/living with partner | 650 (52.4) |
| divorced/separated/widowed | 314 (25.3) |
| Education - college degree or above | |
| Yes | 659 (53.1) |
| Income | |
| <$20,000 | 259 (21.1) |
| $20,000– <$40,000 | 396 (32.3) |
| $40,000+ | 571 (46.6) |
| Parity | |
| 0 | 502 (40.5) |
| 1–2 | 621 (50.0) |
| 3+ | 118 (9.5) |
| Military branch | |
| Army | 616 (49.6) |
| Navy | 279 (22.5) |
| Marine Corps/ Coast Guard | 112 (9.0) |
| Air Force | 234 (18.9) |
| Experienced Military Sexual Trauma | |
| Yes | 663 (53.4) |
| Presence of Mental Health Condition | |
| Yes | 822 (66.2) |
| Presence of Medical Health Condition | |
| Yes | 649 (52.3) |
| Geographic Census Region | |
| Northeast | 105 (8.5) |
| Midwest | 220 (17.7) |
| South | 663 (53.4) |
| West | 253 (20.4) |
Other race includes 2.3% Asian, 0.7% Pacific Islander, 1.1% American Indian, 1.9% multiple race, etc.
Figure 1.
Factors associated with reproductive coercion are shown in Table 2. Women aged 20 to 29, 30 to 34 and 35 to 39 were more likely to report recent reproductive coercion compared to women aged 40 to 44 (15%, 10%, 12% vs. 6%, respectively; aOR: 3.93; 95% CI: 1.80–8.57, aOR: 2.41; 95% CI: 1.14–5.09, and aOR: 2.93; 95% CI: 1.38–6.24, respectively). Non-Hispanic Black women and women from “other” race groups were over twice as likely to report reproductive coercion compared to White women (18%, 19% vs. 7%; aOR: 2.69; 95% CI: 1.69–4.27 and aOR: 2.97; 95% CI: 1.54–5.71). Single and divorced/separated/widowed women were more likely to report reproductive coercion compared to married women (16%, 17% vs. 7%; aOR: 2.24; 95% CI: 1.33–3.78 and aOR: 2.39; 95% CI: 1.49–3.83). Finally, women who experienced MST were more likely to report reproductive coercion compared to women who did not (14% vs. 8%; aOR: 2.14; 95% CI: 1.40–3.27). There were no differences in likelihood of male partner reproductive coercion by parity, history of mental health condition, history of medical comorbidities, or geographic region.
Table 2.
Association between Demographic Characteristics and Past Year Reproductive Coercion
| n=1241 | Reproductive Coercion (%) 139 (11.2%) |
P value | Unadjusted OR (95%)CI |
Adjusted OR (95%)CI |
|---|---|---|---|---|
| Age | 0.04 | |||
| 20–29 | 48 (14.5) | 2.72 (1.34,5.53) | 3.93 (1.80,8.57) | |
| 30–34 | 44 (10.4) | 1.90 (0.93,3.87) | 2.41 (1.14,5.09) | |
| 35–39 | 36 (11.8) | 2.25 (1.09,4.66) | 2.93 (1.38,6.24) | |
| 40–44 | 11 (6.2) | ref | ref | |
| Race/ethnicity | <.0001 | |||
| Non-Hispanic White | 46 (7.3) | ref | ref | |
| Non-Hispanic Black | 64 (18.3) | 2.69 (1.79,4.05) | 2.69 (1.69,4.27) | |
| Hispanic | 11 (6.6) | 0.89 (0.45,1.75) | 0.84 (0.41,1.69) | |
| Other | 18 (18.9) | 2.79 (1.52,5.11) | 2.97 (1.54,5.71) | |
| Marital status | <.0001 | |||
| Single | 43 (15.6) | 2.58 (1.65,4.05) | 2.24 (1.33,3.78) | |
| Married/living with partner | 43 (6.6) | ref | ref | |
| Divorced/separated/widowed | 53 (16.9) | 2.62 (1.69,4.04) | 2.39 (1.49,3.83) | |
| Education - college degree or above | 0.02 | |||
| No | 78 (13.4) | 1.58 (1.10,2.27) | 1.35 (0.91,2.02) | |
| Yes | 61 (9.3) | ref | ref | |
| Income | 0.003 | |||
| <$20,000 | 36 (13.9) | ref | ref | |
| $20,000– <$40,000 | 55 (13.9) | 0.99 (0.63,1.56) | 1.21 (0.74,1.98) | |
| $40,000+ | 44 (7.7) | 0.52 (0.32,0.82) | 0.92 (0.53,1.60) | |
| Parity | 0.66 | |||
| 0 | 54 (10.8) | ref | ref | |
| 1–2 | 74 (11.9) | 1.07 (0.73,1.56) | 1.21 (0.79,1.84) | |
| 3+ | 11 (9.3) | 0.78 (0.38,1.58) | 0.82 (0.38,1.80) | |
| Military branch | 0.1783 | |||
| Army | 75 (12.2) | ref | ref | |
| Navy | 36 (12.9) | 1.01 (0.65,1.55) | 0.96 (0.60,1.52) | |
| Marine Corps/Coast Guard | 8 (7.1) | 0.56 (0.26,1.19) | 0.47 (0.21,1.05) | |
| Air Force | 20 (8.5) | 0.64 (0.38,1.08) | 0.70 (0.40,1.23) | |
| Experience Military Sexual Trauma | 0.0007 | |||
| No | 46 (8.0) | ref | ref | |
| Yes | 93 (14.0) | 1.79 1.23,2.61) | 2.14 (1.40,3.27) | |
| Mental Health Condition | 0.26 | |||
| No | 41 (9.8) | ref | ref | |
| Yes | 98 (11.9) | 1.23 (0.84,1.82) | 0.95 (0.60,1.49) | |
| Medical Health Condition | 0.04 | |||
| No | 55 (9.3) | ref | ref | |
| Yes | 84 (12.9) | 1.46 (1.01,2.10) | 1.46 (0.97,2.19) | |
| Geographic Census Region | 0.67 | |||
| Northeast | 10 (9.5) | ref | ref | |
| Midwest | 23 (10.5) | 1.10 (0.50,2.40) | 1.42 (0.62,3.28) | |
| South | 81 (12.2) | 1.28 (0.64,2.56) | 1.23 (0.58,2.59) | |
| West | 25 (9.9) | 1.00 (0.46,2.18) | 1.25 (0.55,2.86) |
Values in bold indicate statistical significance with a p-value < 0.05 using chi-squared tests
Associations between reproductive coercion and contraceptive use and pregnancy are shown in Table 3. In adjusted analyses controlling for age, race, marital status, education, income, medical comorbidities, and MST, compared to women who did not report coercion, those women who did were less likely to use any contraceptive method at last sex (76% vs. 80%; aOR: 0.61, 95% CI: 0.38–0.96), any prescription contraceptive method (43% vs. 55%; aOR: 0.62, 95% CI: 0.43–0.91), and their ideal method of contraception (35% vs. 45%; aOR: 0.63, 95% CI: 0.43–0.93). Those who reported coercion were more likely to have a pregnancy in the last year (14% vs. 10%; aOR: 2.07, 95% CI: 1.17–3.64) though were not significantly more likely to report unintended pregnancy (6% vs. 4%; aOR: 1.63, 95% CI: 0.71–3.76).
Table 3.
Associations of Reproductive Coercion with Contraceptive Use at Last Sex and Pregnancy in Last Year
| History of past year male partner reproductive coercion |
|||||
|---|---|---|---|---|---|
| N=1241 | No 1102 (88.8) |
Yes 139 (11.2) |
P value |
Unadjusted OR (95% CI) Coercion (yes vs. no) |
Adjusted OR* (95% CI) Coercion (yes vs. no) |
| Used any method of contraception | 879 (79.8) | 106 (76.3) | 0.33 | 0.82 (0.54, 1.24) | 0.61 (0.38, 0.96) |
| Used prescription contraception | 600 (54.5) | 60 (43.2) | 0.01 | 0.64 (0.45, 0.91) | 0.62 (0.43, 0.91) |
| Used ideal contraceptive method | 497 (45.1) | 49 (35.3) | 0.03 | 0.66 (0.46, 0.96) | 0.63 (0.43, 0.93) |
| Pregnancy in last year | 107 (9.7) | 20 (14.4) | 0.09 | 1.56 (0.94, 2.61) | 2.07 (1.17,3.64) |
| Unintended pregnancy in last year | 39 (3.5) | 8 (5.8) | 0.20 | 1.67 (0.76, 3.64) | 1.63 (0.71, 3.76) |
Model adjusted for factors associated with reproductive coercion at the p<0.10 level in bivariate analysis (Table 2), including age, race, marital status, education, income, medical illness, military branch, and MST Values in bold indicate statistical significance with a p-value < 0.05 using adjusted logistic regression
Comment
In this national survey of women veterans of reproductive age who use VA for health care, 11% reported experiencing male partner reproductive coercion in the past year. Black women, younger women, single women, and women who experienced MST were significantly more likely to report reproductive coercion. In addition, women who experienced recent reproductive coercion were less likely to use any method of contraception, prescription methods of contraception and their ideal method of contraception at last sex and more likely to experience pregnancy but not unintended pregnancy in the past year when controlling for age, race, marital status, education, income, medical illness, military branch, and MST.
The 2010 National Intimate Partner and Sexual Violence Survey, a nationally representative survey of US adults aged 18 and older, found that around 9% of women in the United States report ever experiencing reproductive coercion or control by an intimate partner in their lifetime.14 In other recent research, women aged 16 to 29 who attended family planning clinics for health services reported a lifetime prevalence of reproductive coercion of approximately 25%4 and an incidence of 5% to 13% in the past three months.2,3 Given that these studies used different temporal measures and questions to assess reproductive coercion, it is difficult to make direct comparisons to our study sample. However, the prevalence of reproductive coercion does appear to be higher among women veterans than the US adult general population, as 11% of veterans experienced coercion in the past year while 9% of US women experienced coercion in their lifetime.
Consistent with data from non-veteran populations,6,15 we found that Black women were much more likely than White women to report reproductive coercion and that reproductive coercion was more common in younger women and those who are single or divorced/widowed/separated.2,6 One new finding from our study is the association between MST and reproductive coercion. This is not entirely surprising as research has found that women who experience MST are more likely to experience IPV, a context in which reproductive coercion often occurs.3,5,16–18 Given that younger women, minority women, and women exposed to sexual violence are more likely to also experience reproductive coercion, efforts are needed to educate providers about the risks facing these particularly vulnerable subpopulations of veterans.
We found that women who report male partner reproductive coercion were less likely to use any method of contraception and were also less likely to use prescription methods of contraception. While overall contraceptive use was high in both groups, the majority of unintended pregnancies are known to occur among the small proportion of women who are sexually active but do not use a contraceptive method.19 A meta-analysis of 7 studies on the relationship between IPV and contraception use found that women who experience IPV have a reduced odds of using any contraception.20 Our study demonstrates that this association exists with reproductive coercion as well. In addition, we found that women who experience coercion are less likely to use their ideal method of contraception. One previous study reported that women who experience IPV were less likely to use their preferred methods of contraception; however this association did not remain significant after adjusting for confounders.21 Our study found that ideal contraceptive method use is low among all women in this sample. A number of factors such as access, medical contraindications, pregnancy intentions, knowledge of options, and cost all likely contribute to contraceptive use. Our findings offer another potential mechanism to consider in women veterans’ contraceptive decision making. Those who experienced reproductive coercion were less likely to use their ideal method compared to those not exposed. This may be because male partners may actively interfere in contraceptive choices, prevent women from attending health care appointments, sabotage contraceptive efforts, and/or pressure women not to use any contraception.6
We also found that the incidence of pregnancy in the past year was higher among women reporting reproductive coercion compared to those who did not report reproductive coercion. Over 14% of women reporting reproductive coercion had a pregnancy in the past year while less than 10% of women veterans who did not experience coercion experienced pregnancy. While we found no association between coercion and unintended pregnancy, the small numbers of unintended pregnancies in the past year likely limited our ability to detect statistically significant differences, as the study was powered to detect differences in contraceptive use, but not the rarer outcome of unintended pregnancy. In addition, reporting bias could impact the retrospective reporting of unintended pregnancy and coercion, as once her child is born, a woman may no longer view her pregnancy as unintended or report the reproductive coercion that caused it. However, associations between reproductive coercion and unintended pregnancy have been found in other research.2,4,5
VA providers should be made aware of the prevalence of and risk factors associated with reproductive coercion. Specifically, providers need to be aware that women are at risk for reproductive coercion if they are young, single and a racial/ethnic minority and veterans are at increased risk for coercion due to their exposure to sexual trauma. In addition to the demographic risk factors noted in this study, repeated testing for sexually transmitted infections, pregnancy testing, and/or use of emergency contraception may be indicators of exposure to reproductive coercion.3,22 One means to identify patients who may be experiencing reproductive coercion is to integrate targeted assessment of reproductive coercion for veterans with risk factors or clinical red flags during routine clinical visits and visits for reproductive health services.23 To assess for reproductive coercion, the American College of Obstetricians and Gynecologists suggests providers ask questions such as: “has your partner ever forced you to do something sexually that you did not want to do or refused your request to use condoms?” and “has your partner ever tampered with your birth control or tried to get you pregnant when you didn’t want to be?”23,24 Given our findings around ideal versus used method mismatches, providers could also ask their patients about their ideal method of contraception as a means to prompt discussion about any potential method mismatch and encourage shared decision making among women and providers to optimize selection of contraceptive methods. One potential strategy to reduce harm (i.e., undesired pregnancy) related to reproductive coercion is through the use of contraceptive methods that are more discreet and thus less vulnerable to partner interference such as IUDs, implants and contraceptive injections.23 In fact, the American College of Obstetricians and Gynecologists recommends that providers specifically offer these methods of contraception to patients experiencing reproductive coercion.23 Providers are also well-positioned to connect their patients exposed to reproductive coercion to victim service supports and resources both within and outside the VA (such as victim service advocates, counseling, hotlines, and support groups).23
There are several limitations of our study that are important to consider. First, this is a cross sectional study and we cannot establish the temporal relationship of reproductive coercion to pregnancy. Second, contraceptive decision-making is complex and we could not control for all potential confounders, but our findings do suggest that male partner reproductive coercion also influences contraceptive use. Third, the findings from our study cannot necessarily be generalized to women in the general US population or even women veterans who do not use VA. Compared to these other populations, women VA-users have a higher burden of both mental health conditions and medical comorbidities and have a lower socioeconomic status.25,26 Fourth, the survey did not assess IPV, and reproductive coercion is often associated with partner violence; however, research has found that reproductive coercion commonly occurs in the absence of physical violence in a relationship.2,3 Finally, reproductive coercion includes a set of behaviors by male partners in heterosexual relationships which include not only attempts to get a woman pregnant through birth control sabotage, condom manipulation, and pressure to get pregnant, but also behaviors that contribute to termination or continuation of a pregnancy against a woman’s wishes.5,6,23 For this study, consistent with other studies on reproductive coercion and unintended pregnancy2,4,15 as well as nationally representative data,14 we focused on measuring behaviors related to becoming pregnant only given our interest in contraceptive use patterns, thus we did not assess partner influence on decisions related to continuation or termination of pregnancies.
In conclusion, more than 1 in 10 reproductive aged women with male partners in our sample of veterans experience male partner reproductive coercion, which may impact their use of contraception and ability to prevent pregnancy. This study adds to a growing body of literature on the impact of male reproductive coercion on women’s reproductive health. Further research is necessary to understand the relationship between sexual trauma experienced during military service and subsequent reproductive coercion among women veterans. Effort is needed to ensure that providers within the VA healthcare system routinely assess for and address reproductive coercion during reproductive health care visits.
Acknowledgments
This study was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, VA Merit Award IIR 12–124 (PI: Sonya Borrero). The views and opinions of authors expressed herein do not necessarily state or reflect those of the Department of Veterans Affairs or the United States Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: The authors report no conflict of interest
References
- 1.Frayne SM, Phibbs C, Saechao F, et al. Sociodemographics, Utilization, Costs of Care, and Health Profile. Women’s Health Evaluation Initiative, Women’s Health Services, Veterans Health Administration, Department of Veterans Affairs; Washington DC: 2014. Sourcebook: Women Veterans in the Veterans Health Administration. Volume 3. [Google Scholar]
- 2.Miller E, McCauley HL, Tancredi DJ, Decker MR, Anderson H, Silverman JG. Recent reproductive coercion and unintended pregnancy among female family planning clients. Contraception. 2014;89(2):122–128. doi: 10.1016/j.contraception.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kazmerski T, McCauley HL, Jones K, et al. Use of reproductive and sexual health services among female family planning clinic clients exposed to partner violence and reproductive coercion. Matern Child Health J. 2015;19(7):1490–1496. doi: 10.1007/s10995-014-1653-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller E, Decker MR, McCauley HL, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception. 2010;81(4):316–322. doi: 10.1016/j.contraception.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller E, Jordan B, Levenson R, Silverman JG. Reproductive coercion: connecting the dots between partner violence and unintended pregnancy. Contraception. 2010;81(6):457. doi: 10.1016/j.contraception.2010.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grace KT, Anderson JC. Reproductive coercion a systematic review. Trauma Violence Abuse. 2016 doi: 10.1177/1524838016663935. 1524838016663935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerber MR, Iverson KM, Dichter ME, Klap R, Latta RE. Women veterans and intimate partner violence: Current state of knowledge and future directions. J Womens Health. 2014;23(4):302–309. doi: 10.1089/jwh.2013.4513. [DOI] [PubMed] [Google Scholar]
- 8.Turchik JA, Wilson SM. Sexual assault in the US military: A review of the literature and recommendations for the future. Aggress Violent Behav. 2010;15(4):267–277. [Google Scholar]
- 9.Borrero S, Callegari L, Zhao X, et al. Unintended pregnancy and contraceptive use among women Veterans: The ECUUN study. J Gen Intern Med. 2017:1–9. doi: 10.1007/s11606-017-4049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Callegari LS, Zhao X, Schwarz EB, Rosenfeld E, Mor MK, Borrero S. Racial/ethnic differences in contraceptive preferences, beliefs, and self-efficacy among women veterans. Am J Obstet Gynecol. 2017;216(5):504–e1. doi: 10.1016/j.ajog.2016.12.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kimerling R, Gima K, Smith MW, Street A, Frayne S. The Veterans Health Administration and military sexual trauma. Am J Public Health. 2007;97(12):2160–2166. doi: 10.2105/AJPH.2006.092999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Department of Reproductive Health, World Health Organization. Medical eligibility criteria for contraceptive use, 4th edition. 4. Geneva, Switzerland: WHO Press; 2010. [Google Scholar]
- 13.Sonfield A, Kost K, Gold RB, Finer LB. The public costs of births resulting from unintended pregnancies: national and state-level estimates. Perspect Sex Reprod Health. 2011;43(2):94–102. doi: 10.1363/4309411. [DOI] [PubMed] [Google Scholar]
- 14.Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. National intimate partner and sexual violence survey (NISVS): 2010 Summary Report. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 15.Holliday CN, McCauley HL, Silverman JG, Ricci E, Decker MR, Tancredi DJ, et al. Racial/Ethnic differences in women's experiences of reproductive coercion, intimate partner violence, and unintended pregnancy. J Womens Health. 2017 doi: 10.1089/jwh.2016.5996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iverson KM, Mercado R, Carpenter SL, Street AE. Intimate partner violence among women veterans: Previous interpersonal violence as a risk factor. J Traum Stress. 2013;26(6):767–771. doi: 10.1002/jts.21867. [DOI] [PubMed] [Google Scholar]
- 17.Silverman JG, Raj A, Clements K. Dating violence and associated sexual risk and pregnancy among adolescent girls in the United States. Pediatrics. 2004;114(2):e220–e225. doi: 10.1542/peds.114.2.e220. [DOI] [PubMed] [Google Scholar]
- 18.Dichter ME, Marcus SC. Intimate partner violence victimization among women veterans: health, health care service use, and opportunities for intervention. Mil Behav Health. 2013;1(2):107–113. [Google Scholar]
- 19.Sonfield A, Hasstedt K, Gold RB. Moving Forward, Family Planning in the Era of Health Reform. New York: Guttmacher Institute; 2014. [Google Scholar]
- 20.Maxwell L, Devries K, Zionts D, Alhusen JL, Campbell J. Estimating the effect of intimate partner violence on women’s use of contraception: a systematic review and meta-analysis. PLoS One. 2015;10(2) doi: 10.1371/journal.pone.0118234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams CM, Larsen U, McCloskey LA. Intimate partner violence and women's contraceptive use. Violence against women. 2008;14(12):1382–1396. doi: 10.1177/1077801208325187. [DOI] [PubMed] [Google Scholar]
- 22.Nikolajski C, Miller E, McCauley HL, et al. Race and reproductive coercion: A qualitative assessment. Women's Health Issues. 2015;25(3):216–223. doi: 10.1016/j.whi.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American College of Obstetricians Gynecologists. Reproductive and sexual coercion. Committee opinion No. 554. Obstet Gynecol. 2013;121:441–445. doi: 10.1097/01.AOG.0000426427.79586.3b. [DOI] [PubMed] [Google Scholar]
- 24.American College of Obstetricians Gynecologists. Intimate partner violence. Committee opinion no. 518. Obstet Gynecol. 2012;119(2):412–417. doi: 10.1097/AOG.0b013e318249ff74. [DOI] [PubMed] [Google Scholar]
- 25.Washington DL, Yano EM, Simon B, Sun S. To use or not to use. J Gen Intern Med. 2006;21:S11–S18. doi: 10.1111/j.1525-1497.2006.00369.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker?: A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252–3257. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]