Abstract
Background
Individuals suffering from mental as well as physical conditions often face stigma, which can adversely affect functioning, treatment seeking, and emotional health. We compared levels of stigma experienced by individuals with depression and/or chronic pain, to contrast the perception of stigma experienced by the sufferers with that of individuals who have never experienced these conditions, and to determine whether depression is related to greater experience of stigma for chronic pain.
Methods
Four groups of participants (N=236) took part in the study: depression only, chronic pain only, comorbid depression and chronic pain, and healthy controls. Participants underwent a clinical interview and completed a stigma measure that assessed general self-stigma, public stigma, treatment stigma, secrecy, and stigmatizing experiences.
Results
Healthy controls largely underestimated the stigma experienced by individuals with depression, but were not inaccurate in estimating stigma experienced by individuals with chronic pain. Further, individuals with chronic pain only generally perceived less stigma for their condition than did those with depression only. However, comorbid individuals perceived worse stigma of chronic pain compared to individuals with chronic pain alone, suggesting that depression may affect the stigma felt by sufferers of conditions other than depression.
Limitations
Social desirability may have influenced stigma scores. Comparing several groups required adapting a standardized instrument.
Conclusions
Results suggest that depression may play a role in the social experience of having a health condition, as well as indicate that the general public continues to fail to appreciate the negative social pressures experienced by individuals with mental health conditions.
Keywords: mental health stigma, mood disorders, comorbidity, depression stigma
Introduction
Stigma has been defined as “the situation of the individual who is disqualified from full social acceptance” (Goffman, 1963). A stigmatized trait “is deeply discrediting” to the bearer and degrades them “from a whole and usual person to a tainted, discounted one” (Goffman, 1963). Link and Phelan (2001) conceptualize stigma as the convergence of a number of components:
the distinguishing and labelling of human differences
the association of human difference with negative attributes
the separation of “us” from “them”
status loss and discrimination
As they note, though many human differences, such as the color of one’s hair, are generally overlooked and inconsequential, some differences can identify individuals as ‘other’ and lead to social consequences. This occurs when social, economic, and political power allows for the identification and labeling of the ‘other’ and the implementation of disapproval, rejection, exclusion, and discrimination.
Both mental health diagnoses such as major depression (Barney, Griffiths, Jorm, & Christensen, 2006; Bharadwaj, Pai, & Suziedelyte, 2015; Gaudiano & Miller, 2012; Kanter, Rusch, & Brondino, 2008; Latalova et. al., 2014; Oakley, Kanter, Taylor, & Duguid, 2011; Rusch, Kanter, Manos, & Weeks, 2008), and physical health conditions, like chronic pain (Holloway, Sofaer-Bennett, & Walker, 2007; Marbach, Lennon, Link, & Dohrenwend, 1990; Slade, Molloy, & Keating, 2009), are often associated with stigma. Experiencing stigma for having a particular health condition may increase the burden of that condition (Leventhal, Ethan, Horowitz, Leventhal, & Ozakinci, 2004), dissuade patients from accessing healthcare, and decrease overall quality of life (Earnshaw & Quinn, 2012).
Stigma associated with mental illnesses, including depression, can further exacerbate the mental health condition, and further harm an individual’s health. Depression stigma can discourage depressed individuals from seeking medical help (Barney et al., 2006; Clement et al., 2015), lead to social isolation (Crisp, Gelder, Rix, Meltzer, & Rowlands, 2000), decrease social opportunities (Corrigan, 2004), and decrease satisfaction with life (Markowitz, 1998).
Individuals suffering from chronic pain likewise experience stigma due to their condition. Stigma has been reported as coming from the general public, family and friends, and even from their treating healthcare professionals (Holloway et al., 2007; Marbach et al., 1990; Slade et al., 2009). In one representative study, individuals with chronic pain reported feeling disrespected and distrusted; they also reported being suspected of drug-seeking, and believing that their healthcare providers were dismissive of their symptoms (Upshur, Bacigalupe, & Luckmann, 2010). Stigmatization may have a negative effect on the attitudes and behaviors of individuals with chronic pain towards healthcare providers (Holloway et al., 2007). As De Ruddere and Craig (2016) note in their review of stigma and chronic pain, though there is ample evidence that patients with chronic pain experience stigma in all aspects of their lives—however, this stigma is still not well understood, particularly with regards to its determinants, underlying mechanisms, and impact on the patient.
Chronic pain and major depression are frequently comorbid (Arnow et al., 2006; Bair, Robinson, Katon, & Kroenke, 2003; Dworkin & Gitlin, 1991; Miller & Cano, 2009; Romano & Turner, 1985; Ruoff, 1996). We aim to better understand the subjective experience of these diseases and their social consequences given the high prevalence of depression and chronic pain, their economic burden, and the suffering these diseases cause. In the US, over 15 million adults are estimated to have depression (Center for Behavioral Health Statistics and Quality, 2015) and 100 million adults are estimated to have chronic pain (Institute of Medicine, 2011). Both depression and chronic pain are also costly; depression is estimated account for $210.5 billion in health costs and lost productivity (Greenberg, Fournier, Sisitsky, Pike, & Kessler, 2015), and chronic pain is estimated to account for $560 billion to $635 billion (Institute of Medicine, 2011). Both conditions are experienced most days for much of the day, and both interfere with one’s functioning. Both conditions may be chronic but non-progressive, that is, they may last a considerable amount of time, even decades, but their intensity does not inevitably worsen over time. The combination of these two disorders can exacerbate the experience of one’s health state. For example, in one study of patients who visited a primary care clinic, those with comorbid depression and disabling chronic pain reported poorer health-related quality of life and greater somatic symptom severity compared to other patients (Arnow et al., 2006). The combination of chronic pain and major depression may also affect the perception of stigma; however, the specific effect of the comorbidity on the experience of stigma is not yet known.
Given the high prevalence of depression and chronic pain, their economic burden, and the suffering these diseases cause, we aim to better understand the subjective experience of these diseases and their social consequences. Major decisions about the healthcare of individuals suffering from depression and pain are often made by policymakers, healthcare professionals, or even family members who have not experienced these health conditions. It is therefore important to understand whether the perceptions of health conditions and social sequelae such as stigma made by healthy individuals differs from those of the sufferers. Thus, the purpose of this investigation is to characterize the perception of stigma associated with depression and chronic pain among individuals diagnosed with depression, with chronic pain, with comorbid depression and pain, as well as among healthy individuals never affected by either condition. Because of the numerous studies that demonstrate the existence of stigma associated with depression and chronic pain and its impact, we hypothesized that healthy controls will underestimate the stigma associated with depression and chronic pain. However, less was known about the experience of stigma among patients with co-morbid depression and chronic pain – the information obtained from our study could help fill some of the gaps in our knowledge about chronic pain stigma (De Ruddere & Craig, 2016). A better understanding of stigma experiences and the differences of such experiences between the groups, as well as an understanding of the differences in stigma perceptions between those experiencing a disorder and those who do not would be helpful in educating providers and other stakeholders about the unique challenges of individuals struggling with these health conditions.
METHODS
Participants
Participants were recruited to a parent study that evaluated individuals’ decision-making regarding joining clinical trials (Leykin, Dunn, & Muñoz, 2017). Participants (N=236) were recruited to four groups: 61 participants were in the Depression group, 59 in the Chronic Pain group, 56 in the Comorbid (depression and pain) group, and 60 were healthy controls. For the Depression and Comorbid groups, the current diagnosis of primary major depression disorder (MDD) was determined by the SCID-IV-TR (First, Spitzer, Miriam, & Williams, 2001) administered as part of the study. For Chronic Pain and Comorbid groups, the diagnosis of current chronic pain was verified via an interview, and by participants’ report that chronic pain was an ongoing topic of conversation with the participants’ medical provider, and further confirmed with the Brief Pain Inventory (Cleeland, 1991) score of 5 or above on the item assessing worst pain in the past 24 hours. Additionally, single disorder groups (Depression and Chronic Pain) could not have any current or past experience with the other disorder (i.e., to be included in the Chronic Pain group, an individual could not have had a current or a past diagnosis of major depression). Individuals in the Healthy Control group could not have any current or past chronic pain or major depression. Additional inclusion criteria were: 21 years of age or older, proficient in the English language, no cognitive impairment as assessed by the Mini-Cog (Borson, Scanlan, Brush, Vitaliano, & Dokmak, 2000), no prior experience with clinical trial participation, and having access to medical or mental health care. Participants were recruited from local clinics, fliers, and through postings on Craigslist.org.
Measures
Demographics questionnaire
Demographics questionnaire was administered in a clinical interview format, and assessed participants’ age, gender, race, marital status, level of education, employment status, and several other demographic variables.
Structured Clinical Interview
Structured Clinical Interview for DSM-IV-TR (SCID; First et al., 2001) is a semi-structured diagnostic interview for psychiatric diagnoses based on the DSM-IV-TR (APA, 2000). The SCID was administered by advanced clinical psychology graduate students who had received thorough SCID training.
Mini-Cog
Mini-Cog (Borson et al., 2000) is a quick assessment of executive functioning widely used in primary care; Mini-Cog is reported to have a high degree of accuracy in detecting cognitive impairment (Steenland et al., 2008).
Brief Pain Inventory – Short Form
Brief Pain Inventory – Short Form (BPI; Cleeland, 1991) is a 9-item, well-validated measure of current pain. The instrument assesses the intensity of the pain (least, worst, and average in the past 24 hours and current pain), as well as the location of the pain and the degree of pain’s interference with everyday functioning. The pain intensity is assessed on a 10-point Likert-type scale, with scores of 5–6 indicative of moderate pain levels, and scores of 7–10 – of severe pain levels.
Depression Self-Stigma Scale
Depression Self-Stigma Scale (DSSS; Kanter et al., 2008, Oakley, Kanter, Taylor, & Duguid, 2011; Rusch, Kanter, Manos, & Weeks, 2008) is a self-report questionnaire that assesses perceived stigma related to one’s depression. The scale consists of 32 statements, with which a responder can agree or disagree, on a 7-point Likert-type scale. The points and verbal anchors are: 1 - “Completely disagree”, 2 - “Mostly disagree,” 3 - “Somewhat disagree,” 4 - “Neither agree nor disagree,” 5 - “Somewhat agree,” 6 - “Mostly agree,” and 7 - “Completely agree”. One of the items is reverse-coded. In addition to the Total score, five subscale scores are calculated:
General self-stigma – negative internalized beliefs about depression and depressed individuals.
Public stigma – negative attitudes about other individuals with depression.
Secrecy – desire to keep depression secret from others.
Treatment stigma – negative attitudes about receiving treatment for depression.
Stigmatizing experiences – lived experiences where stigma was perceived from others.
For all scores (total and subscales), higher scores reflect greater endorsement or perception of stigma. The Cronbach’s alpha for the Total score was .94, and the alphas for the subscales ranged from .78 to .91 (average: .85).
For Healthy Control participants, the questionnaire was reformulated with hypothetical wording as necessary (e.g., “I would work hard to keep my depression a secret” instead of “I work hard to keep my depression a secret”); the “Healthy Control” version of the questionnaire excluded Stigmatizing experiences subscale as well as several questions from the General self-stigma subscale as these questions required actual experiences with the disorder. For the Healthy Control version, the Cronbach’s alpha for the Total score was .84, and the alphas for the subscales ranged from .80 to .90 (average: .85).
Pain Self-Stigma Scale (PSSS)
To ensure more direct comparability between pain and depression in terms of self-stigma, the Depression Self-Sigma Scale was adapted for pain by replacing depression-related words (e.g., “depression”, “depressed”) with corresponding pain analogues. The Cronbach’s alpha for the Total score was .95, and the alphas for the subscales ranged from .78 to .92 (average: .88). Similarly to above, the questionnaire was reformulated with hypotheticals for Healthy Control participants (e.g., “I would work hard to keep my pain a secret” instead of “I work hard to keep my pain a secret”). Additionally, as with above, for Healthy Control participants, the Stigmatizing experiences subscale as well as several questions from the General self-stigma subscale were removed as these questions required actual experiences with the disorder. For the Healthy Control version, the Cronbach’s alpha for the Total score was .90, and the alphas for the subscales ranged from .80 to .90 (average: .86).
Participants also completed other questionnaires and tasks that are not relevant to the current report.
Procedures
Participants were briefly screened via phone, to determine initial eligibility (access to a provider, English proficiency, whether they are currently experiencing depression and/or pain, and whether they had ever participated in a clinical trial). Those who passed the phone screen were invited for an in-person interview, conducted by clinical psychology graduate students. Informed consent was obtained by the interviewer, after a thorough explanation of study procedures. Once consented, participants were asked a series of demographic questions, followed by Mini-Cog, and (if Mini-Cog was passed) the SCID. Given that major depression and chronic pain were the primary foci of this investigation, aside from the Screening module, all participants were administered the Major Depression section of Modules A and D, and Module G (to rule out chronic pain for psychogenic, rather than medical, reasons). Because MDD needed to be the primary psychiatric diagnosis for those in Depression and Comorbid groups, other modules of the SCID were used as needed, to rule out other primary diagnoses if participant screened positive for other psychiatric conditions or if the interview revealed that other mental health issues could be present.
At the conclusion of the clinical interview, the interviewer determined the participants’ group (i.e., Depression, Chronic Pain, Comorbid, Healthy Control, or disqualified). Those not disqualified completed a battery of self-report questionnaires, including the stigma questionnaires (DSSS and/or PSSS), and other study-related tasks. Depression and Chronic Pain participants completed the DSSS or the PSSS, respectively. Participants in the Comorbid group completed both the DSSS and the PSSS. Participants in the Healthy Control group completed the “control” versions (as described above, without the Stigmatizing experiences subscale, and with several items removed from the General self-stigma subscale) of both measures.
Participants were compensated US$50 for their participation. All study procedures were approved by the Institutional Review Board of the University of California, San Francisco. Analytical considerations.
ANCOVA models were used to compare the stigma scores between groups (Depression, Pain, Comorbid, and Healthy Controls). Aside from group, other predictors in the models were: gender, race (Caucasian/non-Caucasian), marital status (partnered/not-partnered), education level (high school or less/4 year college/graduate education), and age. For within-subject comparisons, repeated measures ANCOVAs were used, with the same controls as above.
The original DSSS uses sum scores for both total stigma scores and for subscale scores. However, in order to make comparisons with the Healthy Control group, which responded to a reduced number of items, we calculated the scores (total as well as subscale scores) as means, by dividing the sum of scores by the number of available items.
RESULTS
Participant characteristics
Chi-square tests and one-way ANOVAs were used to identify differences in demographic characteristics (age, gender, race, marital status, and education level) between the groups. The percentages and means (SDs) of these variables, by group, can be found in Table 1.
Table 1.
Patient characteristics by group
| Group % or mean (SD) |
||||
|---|---|---|---|---|
|
| ||||
| Depression only | Chronic Pain only | Comorbid | Healthy Control | |
| Age | 40.0 (13.6)(A) | 48.3 (13.6)(B) | 50.8 (11.7)(B) | 41.7 (15.0)(A) |
| Gender (% women) | 54.1 | 52.5 | 61.4 | 45.9 |
| Race (% white) | 63.9(A) | 37.3(B) | 42.9(B,C) | 56.7(A,C) |
| Marital status (% single) | 78.7 | 74.6 | 73.7 | 78.7 |
| Education level | ||||
| (% high school or less) | 13.1(A,B) | 15.3(A,B) | 21.1(B) | 4.9(A) |
| (% 4 year college) | 63.9(A,B,C) | 76.3(C) | 56.1(B) | 78.7(A,C) |
| (% graduate school) | 23.0(A) | 8.5(B) | 22.8(A) | 16.4(A,B) |
Note: For each row, different superscript letters indicate significant differences between groups. Statistically significant at p<0.05.
There were significant differences between groups based on race (X2(3,N=236) = 10.7, p = 0.01), education level (X2(6,N=236) = 13.5, p = 0.04), and age (F(3,234) = 8.60, p < 0.001). The Depression and Healthy Control groups were more likely to identify as Caucasian than the Chronic Pain group. Further, the Depression and Comorbid groups were more likely to report having attained an advanced degree than the Chronic Pain group. Those with depression alone tended to be younger than those with chronic pain or co-morbid depression and pain. There were no significant differences between groups based on gender (X2(3,N=236) = 2.89, p = 0.41), or marital status (X2(3,N=236) = 0.70, p = 0.87).
Do stigma ratings of healthy controls differ from those with depression and/or chronic pain?
Depression stigma (Figure 1)
Figure 1.
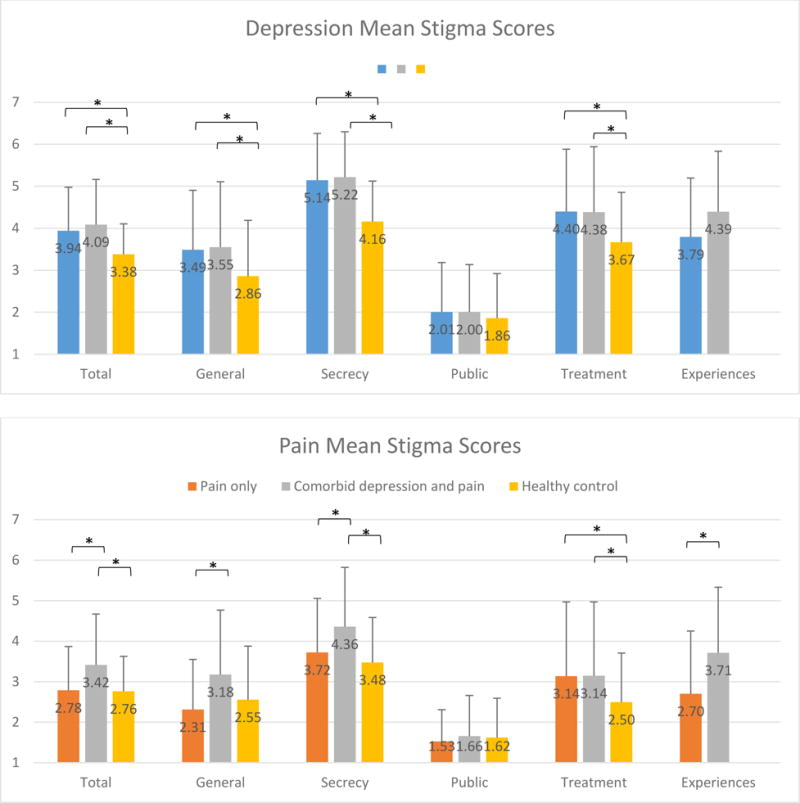
Note: Asterisk (*) indicates p<0.05. Higher scores reflect greater endorsement of stigma attitudes or experiences. Error bars represent standard deviations. Difference of 0.25 points represents a small effect size; difference of 0.63 points represents a medium effect size, difference of 1.01 points represents a large effect size.
ANCOVA models comparing ratings of Healthy Controls, Depression, and Comorbid groups (controlling for demographic characteristics as specified above) revealed significant differences between groups in ratings of total depression stigma score (F(2,168) = 9.48, partial η2 = 0.101, p < 0.001). Examining the estimated marginal means, compared to Healthy Controls, participants with depression and participants with co-morbid depression and chronic pain had significantly higher total stigma scores for depression (p = 0.002 and p < 0.001, respectively). Further analyses revealed significant differences between Healthy Controls, Depression, and Comorbid groups in stigma subscale scores, specifically General self-stigma (F(2,167) = 6.27, partial η2 = 0.070, p = 0.002), Secrecy (F(2,168) = 19.37, partial η2 = 0.187, p < 0.001), and Treatment stigma (F(2,168) = 5.72, partial η2 = 0.064, p = 0.004). Using pairwise comparisons, compared with Healthy Controls, both Depression and Comorbid groups had higher scores for General self-stigma (p = 0.02 and p = 0.001, respectively), Secrecy (p < 0.001 and p < 0.001, respectively), and Treatment stigma (p = 0.005 and p = 0.004, respectively). No differences in Public stigma were identified. Additionally, examining other predictors in the model, younger participants reported higher General self-stigma scores (F(1,167) = 5.58, partial η2 = 0.032, p = 0.019) as did married participants (F(1, 167) = 6.76, partial η2 = 0.039, p = 0.010); married participants also reported higher Treatment stigma score (F(1,168) = 5.02, partial η2 = 0.029, p = 0.026). Non-Caucasian participants reported higher Public stigma score (F(1,168) = 21.51, partial η2 = 0.114, p < 0.001).
Chronic pain stigma (Figure 1)
ANCOVA models comparing Healthy Controls, Pain, and Comorbid groups (controlling for demographic characteristics) revealed significant differences between groups in the total pain stigma score (F(2,166) = 7.00, partial η2 = 0.078, p = 0.001), with Comorbid participants reporting significantly higher total stigma scores compared to Healthy Controls (p=0.001). There were no significant differences in the total stigma scores between Healthy Controls and Chronic Pain participants (p=0.807). In regards to stigma subscales, there were differences between groups in General self-stigma (F(2,166) = 6.43, partial η2 = 0.072, p = 0.002), Secrecy (F(2,166) = 6.70, partial η2 = 0.075, p = 0.002), and Treatment stigma (F(2,166) = 4.09, partial η2 = 0.047, p = 0.018). Compared with healthy controls, the comorbid group reported greater General self- stigma (p=0.008), Secrecy (p<0.001), and Treatment stigma (p=0.011). Participants in the Chronic Pain group did not report higher stigma scores than Healthy Controls, with the exception of Treatment stigma (p=0.017). Of the other predictors, non-Caucasians reported higher Public stigma scores (F(1,166) = 7.89, partial η2 = 0.045, p = 0.006); no other significant differences were observed.
Do stigma scores of the Comorbid group differ from those with single disorders?
For this set of analyses, the Healthy Control group was excluded, to focus on the differences between the Comorbid group and individuals with only depression or only chronic pain.
Depression stigma (Figure 1)
ANCOVA models (controlling for demographic characteristics) revealed no statistically significant differences between Depression and Comorbid groups in either total stigma scores (F(1,109) = 1.56, partial η2 = 0.014, p = 0.211) or stigma subscales, with a possible exception of Stigmatizing experiences (F(1,109) = 3.05, η2 = 0.027, p=0.083), though the difference was small and did not reach statistical significance.
Chronic pain stigma (Figure 1)
The Comorbid group reported significantly higher total stigma scores compared with Chronic Pain group (F(1,107) = 9.07, partial η2 = 0.078, p=0.003), controlling for demographic characteristics. For subscales, compared to the Chronic Pain group, Comorbid group reported higher General self-stigma, (F(1,107) = 10.31, partial η2 = 0.088, p=0.002), Secrecy (F(1,107) = 6.37, partial η2 = 0.056, p=0.013), and Stigmatizing experiences (F(1,107) = 12.908, partial η2 = 0.108, p<0.001). No differences were observed in Public stigma (F(1,107) = 0.76, partial η2 = 0.007, p=0.386) or Treatment stigma (F(1,107) = 0.100, partial η2 = 0.001, p=0.752).
Comparing stigma scores for depression and pain among those with a single condition
Though Depression and Chronic Pain groups did not complete a single common stigma measure, given that the pain stigma scale was constructed from depression stigma scale by replacing references to “depression” with references to “pain”, it was possible to compare the stigma ratings between these two groups directly. Thus, in the following analyses that used the same ANCOVA models as above (controlling for demographic characteristics), the Depression group reported depression stigma, and Chronic Pain group reported chronic pain stigma.
Compared to the Chronic Pain group, Depression group reported higher total stigma scores (F(1,112) = 24.65, partial η2 = 0.18, p < 0.001). Additionally, married individuals and younger individuals reported higher total stigma scores (F(1,112) = 5.89, partial η2 = 0.017, p = 0.017, and F(1,112) = 8.53, partial η2 = 0.071, p = 0.004, respectively). The Depression group also reported higher scores for all subscales: General self-stigma (F(1,111) = 14.350, partial η2 = 0.114, p < 0.001), Secrecy (F(1,112) =25.263, partial η2 = 0.184, p < 0.001), Public stigma (F(1,112) = 9.748, partial η2 = 0.080, p = 0.002), Treatment stigma (F(1,112) = 12.001, partial η2 = 0.097, p = 0.001), and Stigmatizing experiences (F(1,112) = 11.751, partial η2 = 0.095, p = 0.001).
Within-subject comparisons
We also compared stigma scores for both depression and pain among respondents who had both disorders (Comorbid group) by testing within-subjects effects using Repeated Measures ANCOVAs, controlling for gender, age, marital status, education, and race. Participants with co-morbid depression and chronic pain were significantly more likely to give higher total stigma scores for depression than pain (F(1,49) = 10.11, partial η2 = 0.171, p = 0.003). Looking at specific stigma sub-scales, depression stigma scores were significantly higher than chronic pain stigma scores for General self-stigma (F(1,49) = 5.909, partial η2 = 0.108, p = 0.019), Secrecy (F(1,49) = 6.526, partial η2 = 0.118, p = 0.014), and Stigmatizing experiences (F(1,49) = 6.026, partial η2 = 0.110, p = 0.018), while there were no significant differences between depression stigma scores and chronic pain stigma scores for Public stigma (F(1, 49) = 0.098, η2 = 0.002, p = 0.756) or Treatment stigma (F(1, 49) = 1.854, η2 = 0.036, p = 0.180).
Finally, we used Repeated Measures ANCOVAs to compare perceived stigma associated with depression and pain among healthy controls by testing within-subjects effects. Once again, we controlled for gender, age, marital status, education, and race. Healthy controls reported significantly higher total stigma scores for depression compared to chronic pain (F(1,53) = 8.955, partial η2 = 0.145, p = 0.004). Looking at specific stigma sub-scales, healthy controls rated depression stigma higher only on the Secrecy sub-scale (F(1,53) = 12.735, partial η2 = 0.194, p = 0.001). There were no significant differences between Healthy Controls’ ratings of depression stigma and pain stigma in regards to General self-stigma (F(1,53) = 0.003, partial η2 < 0.001, p = 0.955), Public stigma (F(1,53) = 0.671, partial η2 = 0.012, p = 0.416), or Treatment stigma (F(1,53) = 3.413, partial η2 = 0.060, p = 0.070).
DISCUSSION
Depression and chronic pain are prevalent disorders that cause considerable personal and social challenges, with stigma being a particularly burdensome social challenge. In this investigation, we aimed to understand the differences in the perceptions of stigma of depression and chronic pain between those who suffer these conditions, as well as to contrast them with healthy individuals.
Compared to healthy participants, individuals with depression endorsed higher levels of perceived stigma. Specifically, depressed individuals perceived higher levels of general stigma, secrecy stigma, and treatment stigma, but not public stigma or stigmatizing experiences. Previous studies have found that healthy individuals tend to underestimate the burden of experiencing depression (Pyne et al., 2009). Our data show that healthy individuals likewise seem to underestimate negative social consequences, such as stigma, that those with depression face, specifically related to the burden of hiding one’s disease and undergoing treatment for depression. While this may partially be explained by social desirability effects, some research suggests that administering stigma-related questionnaires via a computer (rather than via an interview) reduces the effects of social desirability (Henderson et al., 2012). In our study, participants completed self-reported questionnaires on a tablet computer, and although an interviewer was present in the room, he or she could not see the responses.
Conversely, there was not a significant difference in chronic pain stigma scores between healthy controls and those with chronic pain only. For instance, the mean pain stigma total scores were 2.76 for healthy controls and 2.78 for individuals with chronic pain. This is in stark contrast with what was observed with depression, where healthy individuals tend to underestimate the amount of stigma depressed individuals perceive (3.38 vs 3.94). Thus, healthy individuals did not seem to over- or under-estimate the total amount of stigma those with chronic pain face, though they did seem to underestimate the degree of treatment-related stigma. Treatment stigma may be of considerable importance for those with chronic pain; a previous study has shown that individuals with chronic pain reported being suspected of drug-seeking, rather than seeking treatment for an actual illness (Upshur et al., 2010).
When comparing the perceived levels of stigma for depression and chronic pain directly, individuals perceived stigma of depression as greater than stigma of chronic pain. We compared stigma scores among those with depression only and pain only, as well as scores among those with co-morbid depression and chronic pain, and perceived stigma scores among healthy controls; in all comparisons, depression stigma scores were higher than those of chronic pain. Though a number of studies have shown that physical illnesses may be stigmatized (Hamann et al., 2014; Slade et al., 2009), it appears that societal impression of mental illness remains considerably more negative.
Importantly, the presence of depression appears to be associated with greater experience of non-depression-related stigma. Thus, individuals with co-morbid depression and chronic pain reported higher levels of chronic pain stigma compared to those with chronic pain alone. Studies have found that depression can contribute to pain-related disability (Hall et al., 2011; Velly et al., 2011). We have previously reported that individuals with comorbid depression and chronic pain seem to “dislike” their chronic pain more than individuals with chronic pain alone (Leykin, Dunn, & Muñoz, 2017), and this report extends these findings to stigma. One possible explanation for these results lies in the tendency of depression to produce more overall negativity in all aspects of an individual’s experience, which would suggest that all pain stigma scores ought to have been worse for comorbid individuals as compared to chronic pain only individuals. However, examining specific facets of stigma, it appears that the general negativity does not fully explain the difference in scores. Indeed, for two stigma subscales (Public stigma and Treatment stigma), the scores of comorbid individuals were no worse than those of chronic pain only individuals. Thus, the presence of depression increases the perception of general self-stigma among those with chronic pain, and also increases the perception of secrecy stigma, and stigmatizing experiences. Among those with co-morbid depression and chronic pain, the presence of depression may cause patients to feel a greater need to hide their chronic pain and also make them more likely to perceive experiences as stigmatizing.
In general, healthy controls tended to underestimate total stigma related to depression, particularly compared to those with co-morbid depression and chronic pain. However, a more nuanced picture appears when examining the categories of stigma that we studied: there were some patterns in the stigma sub-scores that healthy controls tended to rate similarly to those with the disease and other sub-scores they tended to underestimate. For both depression and pain, perception of public stigma were similar among those with the disease and the healthy controls. This may be because these questions ask patients about their feelings about other people with that disease (e.g. “Other people with depression are morally weak.” ”I do not want to live next door to another depressed person.”). There are a couple of explanations that may contribute to this observation: 1) Because these questions are about another person, rather than themselves, patients with the disease may respond more similarly to healthy controls. 2) Healthy controls do not want to appear prejudiced and thus answer in socially desirable ways. Meanwhile, for both depression and chronic pain, there were significant differences in perceptions of treatment stigma between those with the disease and healthy controls. Healthy controls underestimated the amount of stigma related to getting treatment that people with chronic pain, depression, or both perceive. Perhaps healthy people, who have not experienced depression or chronic pain, do not fully realize how receiving treatment for an illness can actually be a source of stigma for some patients. This is something healthcare providers should be aware of when managing patients with depression and/or chronic pain.
There are several limitations that need to be acknowledged. These data were from a larger interview-based study, and some individuals might be reluctant to disclose their thoughts about stigma in the presence of a live interviewer. When discussing topics like stigma, which have a moral association, it is possible that respondents feel compelled to respond in socially desirable ways; we attempted to minimize this effect by having participants answer the questions related to stigma on a computer, rather than as part of a live interview. The main instrument in this study was the Depression Self-Stigma Scale (Kanter et al., 2008), which we adapted to create a chronic pain self-stigma scale by replacing words such as “depression” with “chronic pain”. While this approach resulted in analogous scales for depression and chronic pain that enabled us to directly compare the experience of stigma related to each condition, it may also have introduced error. Further adaptation (removing questions) were needed to make the questionnaires interpretable by the healthy control group, which may have resulted in key questions being omitted; however, this only affected the overal score as well as one subscale (general self-stigma), and the pattern of these results were similar for scales that were untouched. Finally, our participants were recruited from a large, diverse, and largely progressive metropolitan area; the stigma experienced by our participants may not be representative of individuals from other communities.
The results of this study raise a number of additional questions. For instance, we have seen that healthy individuals tend to misperceive the amount of stigma that people with depression and/or chronic pain face. What specific effect does this misperception of the stigma have on the disease sufferers? While it is known that self-stigma can interfere with treatment seeking for depression (Barney et al., 2006; Schomerus et al., 2012; Vogel, Wade, & Haake, 2006), future research should examine whether the depression and the associated increase of self-stigma for physical illnesses such as chronic pain also affects treatment seeking for these illnesses. For example, our findings suggest that individuals with chronic pain who also suffer from depression may be prone to a vicious cycle in which they may be less likely to seek treatment for the pain, which could then result in greater duration and intensity of pain, leading to exacerbation of their depression. In our study, healthy controls did not significantly over- or under-estimate the stigma faced by those with chronic pain only, but they did underestimate the stigma faced by those with co-morbid pain and depression, identifying a population that may be at higher risk of poor outcomes due to stigma.
Highlights.
Healthy individuals underestimate stigma of depression, but not of chronic pain
Depression increases perception of stigma of chronic pain
Depression is associated with greater stigma than chronic pain
Acknowledgments
Funding for this work was provided by the National Institute of Mental Health grant 5K08MH091501 (Leykin, P.I.). We are grateful to the Center for Health and Community (Nancy Adler, Director) for providing office space and additional resources. We acknowledge and are grateful for the contributions of research assistants, clinical interviewers, and participants.
Role of Funding Source
Funding sources had no role in the study design, in the collection, analysis, or interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
Contributors
Nida Naushad analyzed the data and wrote much of the first draft of the manuscript. Laura B. Dunn and Ricardo F. Muñoz contributed to the design of the study and to the interpretation of the resulting data. Yan Leykin led the study, wrote the protocol, and oversaw data analyses. All authors contributed to and have approved the final manuscript
Conflict of Interest
The authors report no conflicts of interest.
References
- APA. Diagnostic and statistical manual of mental disorders. 4th. Washington DC: Author; 2000. Text Revision. [Google Scholar]
- Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, Hayward C. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68(2):262–268. doi: 10.1097/01.psy.0000204851.15499.fc. [DOI] [PubMed] [Google Scholar]
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Australian and New Zealand Journal of Psychiatry. 2006;40(1):51–54. doi: 10.1080/j.1440-1614.2006.01741.x. [DOI] [PubMed] [Google Scholar]
- Bharadwaj P, Pai MM, Suziedelyte A. Mental Health Stigma: NBER Working Paper No. 21240 2015 [Google Scholar]
- Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: A cognitive’vital signs’ measure for dementia screening in multi-lingual elderly. International journal of geriatric psychiatry. 2000;15(11):1021–1027. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (HHS Publication No. SMA 15-4927 & S. H-50).Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health N. 2015 (Eds.), Retrieved from http://www.samhsa.gov/data/
- Cleeland CS. Pain assessment in cancer. In: Osoba D, editor. Effect of cancer on quality of life. Boca Raton: CRC Press; 1991. pp. 293–305. [Google Scholar]
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological medicine. 2015;45(1):11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. Am Psychol. 2004;59(7):614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain. 2016;157(8):1607–1610. doi: 10.1097/j.pain.0000000000000512. [DOI] [PubMed] [Google Scholar]
- Dworkin RH, Gitlin MJ. Clinical aspects of depression in chronic pain patients. Clin J Pain. 1991;7(2):79–94. doi: 10.1097/00002508-199106000-00004. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17(2):157–168. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Miriam G, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Gaudiano BA, Miller IW. Self-stigma and attitudes about treatment in depressed patients in a hospital setting. International Journal of Social Psychiatry. 2012;59:586–591. doi: 10.1177/0020764012446404. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs: Prentiss Hall; 1963. [Google Scholar]
- Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) Journal of Clinical Psychiatry. 2015;76(2):155–162. doi: 10.4088/JCP.14m09298. [DOI] [PubMed] [Google Scholar]
- Hall AM, Kamper SJ, Maher CG, Latimer J, Ferreira ML, Nicholas MK. Symptoms of depression and stress mediate the effect of pain on disability. Pain. 2011;152(5):1044–1051. doi: 10.1016/j.pain.2011.01.014. [DOI] [PubMed] [Google Scholar]
- Hamann HA, Ostroff JS, Marks EG, Gerber DE, Schiller JH, Lee SJ. Stigma among patients with lung cancer: a patient-reported measurement model. Psychooncology. 2014;23(1):81–92. doi: 10.1002/pon.3371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson C, Evans-Lacko S, Flach C, Thornicroft G. Responses to mental health stigma questions: the importance of social desirability and data collection method. The Canadian Journal of Psychiatry. 2012;57:152–160. doi: 10.1177/070674371205700304. [DOI] [PubMed] [Google Scholar]
- Holloway I, Sofaer-Bennett B, Walker J. The stigmatisation of people with chronic back pain. Disabil Rehabil. 2007;29(18):1456–1464. doi: 10.1080/09638280601107260. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Kanter JW, Rusch LC, Brondino MJ. Depression Self-Stigma: A New Measure and Preliminary Findings. Journal of Nervous & Mental Disease. 2008;196(9):663. doi: 10.1097/NMD.0b013e318183f8af. [DOI] [PubMed] [Google Scholar]
- Latalova K, Kamaradova D, Prasko J. Perspectives on perceived stigma and self-stigma in adult male patients with depression. Neuropsychiatric disease and treatment. 2014;10:1399. doi: 10.2147/NDT.S54081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal H, Ethan H, Horowitz C, Leventhal E, Ozakinci G. Living with chronic illness: A contextualized, self-regulation approach. In: Sutton S, Baum A, Johnston M, editors. The SAGE handbook of health psychology. London: SAGE; 2004. [Google Scholar]
- Leykin Y, Dunn LB, Muñoz RF. The effect of depression on the decision to join a clinical trial. Journal of Consulting and Clinical Psychology. 2017;85:751–756. doi: 10.1037/ccp0000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual review of Sociology. 2001;27(1):363–385. [Google Scholar]
- Marbach JJ, Lennon MC, Link BG, Dohrenwend BP. Losing face: sources of stigma as perceived by chronic facial pain patients. J Behav Med. 1990;13(6):583–604. doi: 10.1007/BF00844736. [DOI] [PubMed] [Google Scholar]
- Markowitz FE. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav. 1998;39(4):335–347. [PubMed] [Google Scholar]
- Miller LR, Cano A. Comorbid chronic pain and depression: who is at risk? J Pain. 2009;10(6):619–627. doi: 10.1016/j.jpain.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Oakley LD, Kanter JW, Taylor JY, Duguid M. The self-stigma of depression for women. International Journal of Social Psychiatry. 2011;58:512–520. doi: 10.1177/0020764011409820. [DOI] [PubMed] [Google Scholar]
- Pyne JM, Fortney JC, Tripathi S, Feeny D, Ubel P, Brazier J. How bad is depression? Preference score estimates from depressed patients and the general population. Health Serv Res. 2009;44(4):1406–1423. doi: 10.1111/j.1475-6773.2009.00974.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano JM, Turner JA. Chronic pain and depression: does the evidence support a relationship? Psychol Bull. 1985;97(1):18–34. [PubMed] [Google Scholar]
- Ruoff GE. Depression in the patient with chronic pain. J Fam Pract. 1996;43(6 Suppl):S25–33. discussion S34. [PubMed] [Google Scholar]
- Rusch LC, Kanter JW, Manos RC, Weeks CE. Depression stigma in a predominantly low income African-American sample with elevated depressive symptoms. Journal of Nervous and Mental Disease. 2008;196:919–922. doi: 10.1097/NMD.0b013e31818ec5d9. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, Angermeyer MC. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. 2012;125(6):440–452. doi: 10.1111/j.1600-0447.2012.01826.x. [DOI] [PubMed] [Google Scholar]
- Slade SC, Molloy E, Keating JL. Stigma experienced by people with nonspecific chronic low back pain: a qualitative study. Pain Med. 2009;10(1):143–154. doi: 10.1111/j.1526-4637.2008.00540.x. [DOI] [PubMed] [Google Scholar]
- Steenland NK, Auman CM, Patel PM, Bartell SM, Goldstein FC, Levey AI, Lah JJ. Development of a rapid screening instrument for mild cognitive impairment and undiagnosed dementia. Journal of Alzheimer’s Disease. 2008;15(3):419–427. doi: 10.3233/jad-2008-15308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upshur CC, Bacigalupe G, Luckmann R. “They don’t want anything to do with you”: patient views of primary care management of chronic pain. Pain Med. 2010;11(12):1791–1798. doi: 10.1111/j.1526-4637.2010.00960.x. [DOI] [PubMed] [Google Scholar]
- Velly AM, Look JO, Carlson C, Lenton PA, Kang W, Holcroft CA, Fricton JR. The effect of catastrophizing and depression on chronic pain–a prospective cohort study of temporomandibular muscle and joint pain disorders. Pain. 2011;152(10):2377–2383. doi: 10.1016/j.pain.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, Haake S. Measuring the Self-Stigma Associated with Seeking Psychological Help. Journal of Counseling Psychology. 2006;53:325–337. [Google Scholar]
- Waugh OC, Byrne DG, Nicholas MK. Internalized stigma in people living with chronic pain. The Journal of Pain. 2014;15(5):550–e1. doi: 10.1016/j.jpain.2014.02.001. [DOI] [PubMed] [Google Scholar]


