Abstract
Objectives
Meaning-Centered Group Psychotherapy (MCGP) has been demonstrated to be an effective method for improving advanced cancer patients’ quality of life and reducing their depression, hopelessness, and desire for hastened death. To further understand MCGP, this study examined the mechanisms of change in MCGP on these outcomes via advanced cancer patients’ changes of sense of meaning and peace in life.
Methods
The sample data were from 2 randomized control trials that compared MCGP (n = 124) to supportive group psychotherapy (n = 94). Mediation effects of treatment status on outcomes (2 months after completion of treatment) via patients’ change in sense of meaning and peace (posttreatment minus pretreatment) were tested. The outcome variables used in these analyses were quality of life, depression, hopelessness, and desire for hastened death.
Results
Significant mediation effects via change in sense of meaning and peace on these outcomes were found. Consistent results were found using intention-to-treated statuses. Weaker, but still significant, mediation effects via change in sense of faith on these outcomes were also found.
Conclusions
Results supported the hypotheses that improvement due to MCGP is mediated by advanced cancer patients’ enhanced sense of meaning. These findings highlight the importance of interventions focused on enhancing sense of meaning, as this appears to be a viable route to improve quality of life and decrease psychological distress among patients with advanced cancer.
Keywords: advanced cancer, cancer, group psychotherapy, meaning-centered psychotherapy, mediation models, oncology, sense of meaning, spiritual well-being
1 | INTRODUCTION
An ever-growing research literature has identified a patient’s sense of meaning and purpose in life as one of most important influences on quality of life and psychological distress in patients with advanced cancer.1–4 However, identifying techniques to bolster a patient’s sense of meaning remains challenging, as mental health clinicians are often uncomfortable addressing issues of spirituality and meaning in the course of psychotherapy.5,6 To facilitate this process, we developed meaning-centered psychotherapy (MCP), a structured psychotherapeutic approach to enhancing patients’ sense of meaning as they confront terminal illness and death.7–11 Grounded in Viktor Frankl’s Logotherapy,12,13 originally conceived as a group psychotherapy, MCP has subsequently been adapted to an individualized format and adapted to a range of diverse cultures and settings.14
Like many other novel interventions, the effectiveness of MCP has been investigated by randomly assigning individuals with advanced cancer to either MCP or an alternative intervention (typically supportive psychotherapy). By comparing MCP to an alternative, “active” treatment, the magnitude of improvements due to MCP can be more reliably identified. However, what is less clear from the traditional randomized controlled trial (RCT) is whether the effect of MCP is indeed due to its intended impact on enhancing the patient’s sense of meaning or whether improvements represent a more general (ie, nonspecific) treatment effect.
As psychotherapy approaches proliferate, there has been increasing calling for systematic examination of the mechanism of change.15–17 Specifically, researchers question whether the purported rationale behind a psychotherapy approach is indeed the basis for its effectiveness. Yet few studies have addressed this important question in studying psychotherapies for cancer patients,18,19 and none have analyzed the mechanism of change in a psychotherapy grounded in their sense of meaning. The present study investigated the mechanism of change in Meaning-Centered Group Psychotherapy (MCGP) on patients’ quality of life, depression, hopelessness, and desire for hastened death via their improvements on sense of meaning. This question has particular relevance for understanding the extent to which MCGP indeed relies on enhanced meaning (the purported “mechanism of action” underlying the intervention) in achieving the positive results thus far identified. Moreover, identifying particularly helpful treatment components can help lead to even more effective integrative interventions that combine the most beneficial ingredients from multiple different approaches. We chose to contrast the mediation effects of meaning to those of religious faith, in large part because MCP focuses squarely on meaning rather than faith. However, an extensive literature has addressed the benefits of religious faith on physical health outcomes (eg, survival),20–22 albeit typically conceptualizing faith as a “static” (unchanging) variable, rather than one that might change over the course of illness. Thus, we anticipated little or no mediation effects for the patient’s religious faith.
To increase the validity of the findings about the mechanism of change in MCGP, we used a number of critical design elements and statistical analyses.23 First, we combined data from 2 RCTs comparing MCGP to a supportive group psychotherapy (SGP). Although these 2 studies were collected at different periods of time, the interventions and study design were almost identical (with the exception of some changes in study measures). Successful RCTs rule out the influence of potentially confounding pretreatment variables on any effects that result from the RCTs. Data collection at 2 different time periods also increases the generalizability of results. Second, we tested the hypothesized mediation effects of the RCTs (MCGP vs SGP) on patients’ outcomes (quality of life, depression, hopelessness, and desire for hastened death) via their improvements on sense of meaning and peace in life. Figure 1 shows the tested mediation models. We used a nonparametric bootstrapping method to produce the confidence intervals of the mediation effects.24,25 Third, we also tested the mediation effects via patients’ change of sense of faith. Because MCGP is not intended to directly effect this construct, its mediation effects are hypothesized to be negligible (no effects). Support for this hypothesis would rule out the mechanism of change due to an alternative but related construct (ie, religious faith). Finally, randomization to MCGP vs SGP temporally preceded the mediators, which in turn precede the study outcomes. This increases the causality of the mechanism of change.24,26 To sum, the present study aims to provide a rigorous test of the mechanism of change in MCGP using the data from 2 RCTs at different periods of time.
FIGURE 1.
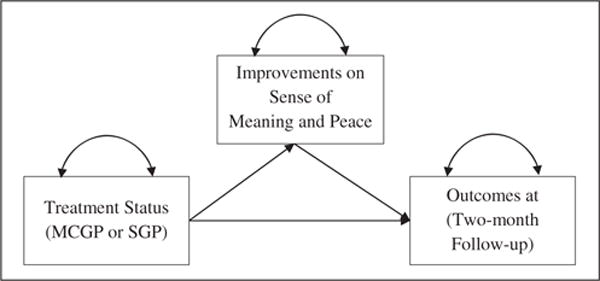
Path diagram of hypothesized medication model of the effect of Meaning-Centered Group Psychotherapy (MCGP) on patients’ outcomes (quality of life, depression, hopelessness, and desire for hastened death) via their improvements on sense of meaning and peace in life. SGP, supportive group psychotherapy
2 | METHOD
2.1 | Participants
Data for this study were drawn from 2 RCTs that compare MCGP and SGP on advanced cancer patients.7,8 Identical recruitment procedures and inclusion/exclusion criteria were used in these 2 studies. Patients with advanced cancer were recruited between July 2002 and September 2005 (study 1) and between August 2007 and May 2012 (study 2). Participants were recruited through multiple sources, including posted flyers, review of medical records, and physical referral from the outpatient clinics at Memorial Sloan Kettering Cancer Center. Eligibility criteria were stage IV cancer (or stage III cancer if diagnosed with poor-prognosis disease, such as pancreatic cancer or non-Hodgkin’s lymphoma), ambulatory, age 18 years or older, and English speaking. Exclusion criteria were significant cognitive impairment or psychotic symptoms (based on clinician assessment), or physical limitations that impeded participation in an outpatient group-based intervention. Potential participants were informed of the study risks and benefits and provided written informed consent. Both of the studies that provided data for these analyses were by the institutional review boards of Memorial Sloan Kettering Cancer Center and Fordham University. Both studies were also registered with the clinical trials registry (NCT00067288 and NCT00494910, respectively).
Of the 413 participants (160 in study 1 and 253 in study 2) who provided informed consent and were randomly assigned to MCGP or SGP, 262 patients (63.4%) began treatment. Typical reasons for this attrition were becoming too ill to participate and scheduling conflicts.7,8 Among these 262 patients, 142 (54.2%) were randomly assigned to MCGP and 120 (45.8%) were assigned to SGP. There were 104 MCGP participants (73.2%) and 78 SGP participants (65.0%) that completed the 8-week treatment and posttreatment assessment. As with pretreatment attrition, the typical reasons for attrition during treatment were worsening illness and scheduling conflicts. Two months after treatment, 82 MCGP participants (57.7%) and 58 SGP participants (48.3%) completed the follow-up assessment.
The present study only involved participants who attended at least 3 sessions of the assigned treatment, with 124 MCGP participants (56.9%) and 94 SGP participants (43.1%). Table 1 shows the participants’ demographic and clinical characteristics. There were 77 men (35.3%) and 141 women (64.7%), with an average age of 59.0 years old (SD = 11.2, range: 21-91) and 16.4 years of education completed (SD = 2.6). Most participants were Caucasians (83.1%) or African Americans (10.3%) and having some forms of faith (91.7%; 32.3% Catholic, 28.6% Jewish, 14.3% Christian, and 16.6% other). Common diagnosed cancers were breast cancers (22.5%), colon/rectal/prostate/testes cancers (19.3%), or pancreas/liver/stomach/kidney cancers (19.3%). Most participants (80.5%) had stage IV disease while 19.5% had stage III disease.
TABLE 1.
Participants’ demographic and clinical characteristics, and their differences between randomized groups (MCGP and SGP) and between randomized controlled trials (RCTs)
| Variables | Frequency, % | Mean (SD) | Difference Between RCTs | Difference Between MCGP and SGP |
|---|---|---|---|---|
| Age | 59.0 (11.2) | t216 = 1.57 | t216 = 0.07 | |
|
| ||||
| Years of education | 16.4 (2.6) | t212 = 1.73 | t212 = 0.70 | |
|
| ||||
| Gender | χ2 = 13.92** | χ2 = 0.84 | ||
| Male | 77 (35.3) | |||
| Female | 141 (64.7) | |||
|
| ||||
| Race | χ2 = 4.73 | χ2 = 0.29 | ||
| Caucasian | 177 (83.1) | |||
| African American | 22 (10.3) | |||
| Asian | 6 (2.8) | |||
| Other | 8 (3.8) | |||
|
| ||||
| Religion | χ2 = 4.91 | χ2 = 3.14 | ||
| Catholic | 70 (32.3) | |||
| Jewish | 62 (28.6) | |||
| Christian | 31 (14.3) | |||
| Other | 36 (16.6) | |||
| None | 18 (8.3) | |||
|
| ||||
| Cancer diagnosis | χ2 = 47.1** | χ2 = 2.07 | ||
| Breast | 49 (22.5) | |||
| Colon/rectal/prostate/testes | 42 (19.3) | |||
| Pancreas/liver/stomach/kidney | 42 (19.3) | |||
| Lung/bronchi | 32 (14.7) | |||
| Other | 53 (24.3) | |||
|
| ||||
| Stage of cancer | χ2 = 20.6** | χ2 = 1.21 | ||
| Stage IV | 173 (80.5) | |||
| Stage III | 42 (19.5) | |||
|
| ||||
| Current medical treatment | χ2 = 31.3** | χ2 = 5.80 | ||
| Chemotherapy | 150 (69.1) | |||
| Hormonal therapy | 13 (6.0) | |||
| Surgery | 5 (2.3) | |||
| Other | 49 (22.6) | |||
Abbreviations: MCGP, Meaning-Centered Group Psychotherapy; SGP, supportive group psychotherapy. χ2 test of independence with bootstrap P value was used for categorical variables. Independent-sample t test was used for continuous variables.
P < .05.
P < .01.
2.2 | Procedures
The 2 RCTs used identical procedures. Participants were randomized in groups of 8 to 10, and then groups were randomly assigned to MCGP or SGP. All participants completed a battery of self-report questionnaires before the first session of treatment (time 1, T1), and they were readministered with the same battery of questionnaires after the last session of the treatment (time 2, T2). Two months after the treatment, participants completed the same battery of questionnaires (time 3, T3).
This study used a subset of the measures completed by the participants in the assessment battery. Sense of meaning and peace as well as sense of faith were measured by the subscales of the Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale, which is composed of 2 subscales, one measuring sense of meaning and peace and a second measuring sense of faith (Meaning and Peace subscale: α = .88 [T1] and .89 [T2]; Faith subscale: α = .92 [T1] and .91 [T2]).27 Quality of life was measured by the McGill Quality of Life Questionnaire (α = .92 [T1] and .90 [T3]).28 Depression was measured by the Beck Depression Inventory (α = .90 [T1] and .88 [T3]).29 Hopelessness was measured by the Hopelessness Assessment in Illness Questionnaire (α = .86 [T1] and .86 [T3]).30 Desire for hastened death was measured by the Schedule of Attitudes Toward Hastened Death (α = .87 [T1] and .86 [T3]).31
2.2.1 | Meaning-Centered Group Psychotherapy
Developed by Breitbart and colleagues,7–11 MCGP is an 8-session manualized psychotherapy influenced by the work of Viktor Frankl.12,13 It uses didactics, discussion, and experiential exercises to develop or increase sense of meaning and purpose despite illness in patients with advanced cancer. Each session addresses specific themes related to exploration of the concepts and sources of meaning, the impact of cancer on sense of meaning and peace, and putting patient’s life in a historical and personal context.
2.2.2 | Supportive group psychotherapy
Supportive group psychotherapy is an 8-session manualized psychotherapy that focuses on discussing issues and themes that emerge for patients coping with cancer. In the sessions, patients are encouraged to share concerns related to the cancer diagnosis and treatment, describe their experiences, emotions, and problems, and offer support and advice to other group members. In the 2 RCTs, all group facilitators only conducted either MCGP or SGP to prevent “bleeding” across conditions.
2.3 | Statistical analysis
Several preliminary analyses were conducted to aid the mediation analyses. First, we calculated the intraclass correlations (ICCs) of participants within therapy groups for the analyzed variables. Small ICCs (≤0.15) suggest that this clustering effect can be ignored in all analyses. Second, we compared the differences between the 2 RCTs on participants’ demographic and clinical characteristics. When there were more than 5% of the variables showing significant differences between the 2 RCTs, we included an indicator of the 2 RCTs as a covariate in the mediation analyses. Third, we compared the differences between MCGP and SGP on participants’ demographic and clinical characteristics. Successful RCTs should have not more than 5% of the variables showing significant differences (when testing at α = .05). We also summarized the attrition analyses that were previously conducted for the 2 RCTs.8,9 In addition, we investigated whether any demographic and analyzed variables were significantly related to missing data patterns in the sample data. Variables with significant relationships would be included as covariates to account for the missing values in the data using maximum likelihood estimation.32
Mediation analyses were conducted using structural equation modeling using Mplus Version 7.2 (Figure 1).33 Treatment status was dummy coded (1 = MCGP, 0 = SGP). The mediator (improvement in meaning and peace/faith) was expressed as latent difference score (LDS) between T2 and T1.34 Contrary to the difference score (ie, subtraction of the measured scores between T2 and T1), LDS is an unobserved (latent) factor created by imposing model constraints on the path coefficients and residual variance of the scores at T2 and T1. One important advantage of the LDS over and above difference score is that LDS is measurement error free (ie, perfectly reliable).35 In addition, with the use of maximum likelihood estimation in the model estimation, LDS is advantageous in using the observed data from participants who completed the assessment in T1 but not T2. All outcomes were measured at T3. Each outcome (quality of life, depression, hopelessness, and desire for hastened death) was analyzed in a separate mediation model. The mediation effect is the product of the effect of treatment status to mediator and that of mediator to outcome, and it was tested using nonparametric bootstrapping method.25,26 No covariates were included for the effect of treatment status to mediator because of the successful randomization. Outcome measured at T1 was used as the covariate for the effect of mediator to outcome.
3 | RESULTS
3.1 | Preliminary analyses
First, the average therapy group size was 5.3. All analyzed variables had small ICCs of participants within therapy groups (mean = 0.06, range = 0.00-0.14).36 Therefore, we decided to ignore this clustering effect in subsequent analyses. Second, half (4 of 8) demographic and clinical characteristics in Table 1 showed significant differences between the 2 RCTs. We included a dummy variable of the 2 RCTs (0 = study 1, 1 = study 2) as a covariate in the mediation analyses to control for sample effects. Third, none of the demographic and clinical characteristics in Table 1 showed significant differences between MCGP and SGP, indicating that the randomization was successful.
3.2 | Attrition and completion
In study 1, there were no significant relationships between pretreatment attrition with patients’ demographic and clinical characteristics and whether patients were assigned to their preferred treatment. In addition, there were no significant differences between MCGP and SGP in terms of completing 8 sessions of treatment. In study 2, there were no group differences between MCGP and SGP participants on their attrition before treatment, number of attended sessions, or completing the 8 session treatment. In this sample, the missing data rate was 0.0%, 19.4%, and 35.9% at T1, T2, and T3, respectively. There were no significant differences between the missing data patterns of the 3 time points on patents’ treatment assignment, demographic and clinical characteristics, and the analyzed variables at T1. The results supported that the sample data are missing completely at random. No variables were used as covariates to account for the missing values using maximum likelihood estimation.
3.3 | Mediation effects via change in meaning and peace
Panel A in Table 2 shows the unstandardized path coefficients and mediation effects attributable to change in meaning and peace. There was a significant positive treatment effect for the mediator (b = 0.33, S.E. = 0.10, P < .01), indicating that MCGP resulted in significantly greater change in meaning and peace compared to SGP. In turn, change in the mediator led to significantly improved quality of life (b = 1.00, S.E. = 0.26, P < .01) and decreased depression (b = −0.21, S.E. = 0.05, P < .01), hopelessness (b = −0.12, S.E. = 0.06, P < .05), and desire for hastened death (b = −0.04, S.E. = 0.02, P < .05) at T3. The mediation effects were significant for quality of life and depression (P < .05), but not for hopelessness and desire for hastened death (P = .10).
TABLE 2.
Unstandardized path coefficients and mediation effects
| Outcome | Treatment to Outcome | Treatment to Mediator | Mediator to Outcome | Mediation Effect (95% CI) |
|---|---|---|---|---|
| A, Change in meaning and peace as mediator | ||||
| Quality of life | 0.25 (0.28) | 0.32 (0.10)** | 1.00 (0.26)** | .32 (.08 to .64) |
| Depression | −0.01 (0.05) | 0.33 (0.10)** | −0.21 (0.05)** | −.07 (−.14 to −.02) |
| Hopelessness | −0.11 (0.07) | 0.32 (0.10)** | −0.12 (0.06)* | −.04 (−.09 to .00) |
| Desire for hastened death | −0.03 (0.02) | 0.33 (0.10)** | −0.04 (0.02)* | −.01 (−.03 to .00) |
|
| ||||
| B, Change in faith as mediator | ||||
| Quality of life | 0.33 (0.28) | 0.30 (0.12)* | 0.65 (0.20)** | .19 (.02 to .43) |
| Depression | −0.03 (0.05) | 0.30 (0.12)* | −0.13 (0.03)** | −.04 (−.08 to −.01) |
| Hopelessness | −0.11 (0.07) | 0.31 (0.12)* | −0.10 (0.05)* | −.03 (−.08 to .00) |
| Desire for hastened death | −0.03 (0.02) | 0.31 (0.12)** | −0.04 (0.01)** | −.01 (−.02 to .00) |
All path coefficients and mediation effects are unstandardized. Coefficients represent b (S.E.). Mediation effect is the effect of treatment status to mediator and that of mediator to outcome. Numbers in parentheses are standard error estimates. Numbers in round brackets are the lower and upper limits of the 95% confidence intervals of the mediation effects. When the confidence interval does not include zero, the mediation effect is significant at P = .05.
P < .05.
P < .01.
A second set of mediation analyses was conducted that included all participants who were randomized assigned to MCGP or SGP regardless of how many treatment sessions were attended (ie, intention-to-treat analyses). Panel A in Table 3 shows the results for change of sense of meaning and peace. All results were consistent with the results described above.
TABLE 3.
Unstandardized path coefficients and mediation effects using intent-to-treat status
| Outcome | Treatment to Outcome | Treatment to Mediator | Mediator to Outcome | Mediation Effect (95% CI) |
|---|---|---|---|---|
| A, Change in meaning and peace as mediator | ||||
| Quality of life | 0.25 (0.28) | 0.29 (0.03)** | 1.00 (0.25)** | .29 (.07 to .59) |
| Depression | −0.01 (0.05) | 0.30 (0.10)** | −0.21 (0.05)** | −.06 (−.13 to −.02) |
| Hopelessness | −0.11 (0.07) | 0.28 (0.10)** | −0.12 (0.06) | −.03 (−.09 to .00) |
| Desire for hastened death | −0.03 (0.02) | 0.30 (0.10)** | −0.04 (0.02)* | −.01 (−.03 to .00) |
|
| ||||
| B, Change in faith as mediator | ||||
| Quality of life | 0.33 (0.28) | 0.34 (0.12)** | 0.65 (0.20)** | .22 (.03 to .47) |
| Depression | −0.03 (0.05) | 0.34 (0.12)** | −0.13 (0.03)** | −.04 (−.09 to −.01) |
| Hopelessness | −0.11 (0.07) | 0.35 (0.12)** | −0.10 (0.05)* | −.04 (−.09 to .00) |
| Desire for hastened death | −0.03 (0.02) | 0.35 (0.12)** | −0.04 (0.01)** | −.01 (−.03 to .00) |
All path coefficients and mediation effects are unstandardized. Mediation effect is the effect of treatment status to mediator and that of mediator to outcome. Numbers in parentheses are standard error estimates. Numbers in round brackets are the lower and upper limits of the 95% confidence intervals of the mediation effects. When the confidence interval does not include zero, the mediation effect is significant at P = .05.
P < .05.
P < .01.
3.4 | Mediation effects via change in faith
Panel B in Table 2 shows the unstandardized path coefficients and mediation effects via change of sense of faith. There was significant positive treatment effect to the mediator (b = 0.31, S.E. = 0.10, P < .05), indicating that MCGP resulted in significantly greater change in faith than did SGP. It was noted that the treatment effect attributable to the change in faith was smaller in magnitude than that to the change of sense of meaning and peace. In turn, change in the mediator corresponded to significantly improved quality of life (b = 0.65, S.E. = 0.20, P < .01) and decreased depression (b = −0.13, S.E. = 0.03, P < .01), hopelessness (b = −0.10, S.E. = 0.05, P < .05), and desire for hastened death (b = −0.04, S.E. = 0.01, P < .01) at T3. The mediation effects were significant for quality of life and depression (P = .05), but not for hopelessness and desire for hastened death (P = .10). The intention-to-treat analyses showed consistent results (panel B in Table 3).*
4 | DISCUSSION
A growing research base has supported the effectiveness of MCGP as a method of improving spiritual and psychological well-being in patients with advanced and terminal cancer. Indeed, interest in MCGP has rapidly spread across the globe, with many clinicians seeking and receiving training in this technique. Although our prior research has consistently demonstrated stronger effects for MCGP compared to supportive psychotherapy, this research has not addressed the extent to which the effectiveness of MCGP is due to its purported theoretical mechanism—improvement in a sense of meaning—is indeed the basis for the changes observed in clinical outcomes. The absence of research addressing this presumptive mechanism of change is particularly surprising given the long-standing interest in psychotherapies that target existential despair,37 as well as the recent growth in meaning-based interventions.38–40
The analyses reported here provide strong support for the theoretical foundation underlying MCGP that an enhanced sense of meaning and peace leads to decreased psychological distress. These findings, in which an improved sense of meaning and peace mediated improvement in distress more generally (improved quality of life and decreased depression, in particular), provide support for this purported mechanism of change. Indeed, change in the meaning and peace was a particularly powerful mediator of improved quality of life, the outcome variable that has consistently demonstrated the strongest MCGP treatment effects in our past research. Weaker mediation effects were observed for depression, and weaker still (and not significant) for hopelessness and desire for hastened death. These latter outcomes, which have also demonstrated significant treatment effects following MCGP, reflect much more serious levels of despair. It may be that improvement in hopelessness and desire for death follows a more complex mediation pathway, such as being mediated by changes in both depression and meaning, rather than only meaning. Nevertheless, it is noteworthy that the 4 outcome variables were highly correlated (r’s > 0.50). Further research exploring the interrelationships among these variables may help explain the mechanism by which MCGP impacts different aspects of psychological well-being among patients with advanced cancer.
Although we expected to find significant mediation effects for the meaning and peace subscale, we observed similar, albeit weaker, mediation effects for changes in the faith subscale. These 2 subscales of the Spiritual Well-Being scale are, of course, highly correlated with one another (r = 0.42 in the current study), and our past research has consistently demonstrated significant improvement in the faith subscale in response to MCGP. Hence, the findings from this study that changes in faith also significantly mediated change in the outcome variables are not surprising, and likely reflect the fact that, for many people, a sense of meaning and peace is interwoven with their religious faith. Given the prominence of meaning and peace (versus faith), both in terms of responsiveness to MCGP and its mediating effect on these study outcome variables, this finding does not diminish support for the proposed mechanism of change for MCGP.
There are, of course, a number of limitations in this study that should be acknowledged. First, the 2 RCTs that compose the sample data had high attrition rates throughout the recruitment, treatment, and follow-up stages. The most common reason of attrition was deteriorating heath, which is hardly unexpected for an intervention targeting patients with advanced cancer.5,6 Analysis of this attrition supported the assumption that this attrition would have little impact on biasing the study results. In addition, an appropriate statistical procedure (maximum likelihood estimation) was used to handle the missing values in the data and provide correct statistical inferences. Intent-to-treat analyses also showed consistent results, further supporting the conclusion that attrition did not significantly alter the study findings. In addition, change of sense of meaning (and faith) was operationalized only by the pretreatment and posttreatment measurements. Ideally, midtreatment assessments would have shown how patients’ sense of meaning (and faith) changes over the course of treatment. Further research using multiple (including midtreatment) time points may help further elucidate these mediating effects.
Despite the study limitations, this study provides one of the first attempts to examine the mechanism of change of a psychotherapeutic intervention (MCGP) specifically developed for advanced cancer patients. A growing research base has demonstrated the effectiveness of MCGP, but the extent to which these benefits are due to changes in meaning has not been previously demonstrated. Meaning-centered psychotherapy may have unique ingredients that are able to address existential suffering in advanced cancer patients in ways that more traditional psychotherapies do not directly target. Given the time-limited nature of the intervention and the many challenges advanced cancer patients face, this also highlights the effectiveness of targeting meaning as a powerful tool to cultivate change. Indeed, the integration of techniques focusing on enhancing meaning into other psychotherapeutic, or even psychoeducational approaches, may be worth consideration, as these findings demonstrate the potential importance of meaning, particularly for individuals confronting advanced or terminal illness. As psychotherapies continue to arise and be promoted, understanding the critical and unique elements of these psychotherapies will become increasingly important. Such research can help refine existing psychotherapies or even help create hybrid treatment approaches that integrate key elements from multiple interventions. This study represents one of the first such efforts along this important path.
Acknowledgments
This research was supported by funding from the National Center for Complementary and Alternative Medicine and the National Cancer Institute (grant numbers R21-AT/CA0103 and R01-AT001842; William Breitbart, P.I.).
Funding information
National Center for Complementary and Alternative Medicine and National Cancer Institute, Grant/Award Numbers: R01-AT001842 and R21-AT/CA0103
Footnotes
We have also conducted the mediation analyses where both mediators (change in meaning and peace and change in faith) were included in the models together. All the results were consistent with the findings in which they were analyzed separately, except that the mediation effect of (treatment → change in faith → quality of life) was not significant.
ORCID
Barry Rosenfeld, http://orcid.org/0000-0003-1399-2777
References
- 1.Field MJ, Cassel CK, editors. Approaching Death: Improving Care at the End of Life. Washington, DC: National Academies Press; 1997. [PubMed] [Google Scholar]
- 2.McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. The Lancet. 2003;361(9369):1603–1607. doi: 10.1016/S0140-6736(03)13310-7. [DOI] [PubMed] [Google Scholar]
- 3.Nelson CJ, Rosenfeld B, Breitbart W, Galietta M. Spirituality, religion, and depression in the terminally ill. Psychosomatics. 2002;43(3):213–220. doi: 10.1176/appi.psy.43.3.213. [DOI] [PubMed] [Google Scholar]
- 4.Breitbart W, Rosenfeld B, Pessin H, et al. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA. 2000;284(22):2907–2911. doi: 10.1001/jama.284.22.2907. [DOI] [PubMed] [Google Scholar]
- 5.Pargamet KI. Spirituality Integrated Psychotherapy: Understanding and Addressing the Sacred. New York, NY: Guilford Press; 2007. [Google Scholar]
- 6.Jenkins RA, Pargamet KI. Religion and spirituality as resources for coping with cancer. J Psychosoc Oncol. 1995;13(1–2):51–74. [Google Scholar]
- 7.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psychooncology. 2010;19(1):21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breitbart W, Rosenfeld B, Pessin H, Applebaum A, Kulikowski J, Lichtenthal WG. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Oncol. 2015;33(7):749–754. doi: 10.1200/JCO.2014.57.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenstein M, Breitbart W. Cancer and the experience of meaning: a group psychotherapy program for people with cancer. Am J Psychother. 2000;54(4):486–500. doi: 10.1176/appi.psychotherapy.2000.54.4.486. [DOI] [PubMed] [Google Scholar]
- 10.Breitbart W, Poppito S, Rosenfeld B, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol. 2012;30(12):1304–1309. doi: 10.1200/JCO.2011.36.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer. 2002;10(4):272–280. doi: 10.1007/s005200100289. [DOI] [PubMed] [Google Scholar]
- 12.Frankl VE. Man’s Search for Meaning. 4th. Boston, MA: Beacon Press; 1959. [Google Scholar]
- 13.Frankl VE. Expanded. New York, NY: Penguin Books; 1969. The Will to Meaning: Foundations and Applications of Logotherapy. [Google Scholar]
- 14.Breitbart W, editor. Meaning-Centered Psychotherapy in the Cancer Setting: Finding Meaning and Hope in the Face of Suffering. New York, NY: Oxford University Press; 2017. [Google Scholar]
- 15.Kazdin AE. Developing a research agenda for child and adolescent psychotherapy. Arch Gen Psychiatry. 2000;57(9):829–835. doi: 10.1001/archpsyc.57.9.829. [DOI] [PubMed] [Google Scholar]
- 16.Kazdin AE. Mechanisms of change in psychotherapy: advances, breakthroughs, and cutting-edge research (do not yet exist) In: Bootzin RR, McKnight PE, editors. Strengthening Research Methodology: Psychological Measurement and Evaluation. Vol. 2006. Washington, DC: American Psychological Association; pp. 77–101. [Google Scholar]
- 17.Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. 2007;3(1):1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- 18.Sherman KA, Heard G, Cavanagh KL. Psychological effects and mediators of a group multi-component program for breast cancer survivors. J Behav Med. 2010;33(5):378–391. doi: 10.1007/s10865-010-9265-9. [DOI] [PubMed] [Google Scholar]
- 19.Vallance JKH, Courneya KS, Plotnikoff RC, Mackey JR. Analyzing theoretical mechanisms of physical activity behavior change in breast cancer survivors: results from the activity promotion (ACTION) trial. Ann Behav Med. 2008;35(2):150–158. doi: 10.1007/s12160-008-9019-x. [DOI] [PubMed] [Google Scholar]
- 20.Powell LH, Shahabi L, Thoresen CE. Religion and spirituality: linkages to physical health. Am Psychol. 2003;58(1):36–53. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- 21.Schreiber JA, Brockopp DY. Twenty-five years later—what do we know about religion/spirituality and psychological well-being among breast cancer survivors? A systematic review. J Cancer Surviv. 2012;6(1):82–94. doi: 10.1007/s11764-011-0193-7. [DOI] [PubMed] [Google Scholar]
- 22.Jim HSL, Pustejovsky JE, Park CL, et al. Religion, spirituality and physical health in cancer patients: a meta-analysis. Cancer. 2015;121(21):3760–3768. doi: 10.1002/cncr.29353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Preacher KJ. Advances in mediation analysis: a survey and synthesis of new developments. Annu Rev Psychol. 2015;66(1):825–852. doi: 10.1146/annurev-psych-010814-015258. [DOI] [PubMed] [Google Scholar]
- 24.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58(1):593–637. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivar Behav Res. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Preacher KJ, Selig JP. Advantages of Monte Carlo confidence intervals for indirect effects. Commun Methods Meas. 2012;6(2):77–98. [Google Scholar]
- 27.Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D. A case for including spirituality in quality of life measurement in oncology. Psychooncology. 1999;8(5):417–428. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 28.Cohen SR, Mount BM, Strobel MG, Bui F. The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med. 1995;9(3):207–219. doi: 10.1177/026921639500900306. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Ward CH, Mendelson M. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 30.Rosenfeld B, Pessin H, Lewis C, et al. Assessing hopelessness in terminally ill cancer patients: development of the Hopelessness Assessment in Illness Questionnaire. Psychol Assess. 2011;23(2):325–336. doi: 10.1037/a0021767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosenfeld B, Breitbart W, Stein K, et al. Measuring desire for death among patients with HIV/AIDS: the schedule of attitudes toward hastened death. Am J Psychiatry. 1999;156(1):94–100. doi: 10.1176/ajp.156.1.94. [DOI] [PubMed] [Google Scholar]
- 32.Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Methods. 2001;6(4):330–351. [PubMed] [Google Scholar]
- 33.Muthén LK, Muthén BO. Mplus User’s Guide. 7th. Los Angeles, CA: Muthén & Muthén;; 1998. [Google Scholar]
- 34.McArdle JJ. A latent difference score approach to longitudinal dynamic structural analyses. In: Cudeck R, du Toit S, Sorbom D, editors. Structural Equation Modeling: Present and Future. Vol. 2001. Lincolnwood, IL: Scientific Software International; pp. 342–380. [Google Scholar]
- 35.Edwards JR. Ten difference score myths. Organ Res Meth. 2001;4(3):265–287. [Google Scholar]
- 36.Hedges LV, Hedberg EC. Intraclass correlations for planning group randomized experiments in rural education. J Res Rural Educ. 2007;22(10):1–15. [Google Scholar]
- 37.Yalom ID, Greaves C. Group therapy with the terminally ill. Am J Psychiatry. 1977;134(4):396–400. doi: 10.1176/ajp.134.4.396. [DOI] [PubMed] [Google Scholar]
- 38.Ando M, Morita T, Okamoto T, Ninosaka Y. One-week Short-Term Life Review interview can improve spiritual well-being of terminally ill cancer patients. Psychooncology. 2008;17(9):885–890. doi: 10.1002/pon.1299. [DOI] [PubMed] [Google Scholar]
- 39.LeMay K, Wilson KG. Treatment of existential distress in life threatening illness: a review of manualized interventions. Clin Psychol Rev. 2008;28(3):472–493. doi: 10.1016/j.cpr.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 40.Lo C, Hales S, Jung J, et al. Managing Cancer And Living Meaningfully (CALM): phase 2 trial of a brief individual psychotherapy for patients with advanced cancer. Palliat Med. 2014;28(3):234–242. doi: 10.1177/0269216313507757. [DOI] [PubMed] [Google Scholar]


